Abstract
Background
Few standards exist for reporting VCUG results.
Objective
To assess the variation in reporting of VCUG findings from different facilities using a standardized assessment tool.
Materials and Methods
VCUG reports were evaluated for demographic, technical, anatomic, and functional information. Reports were categorized by age, gender, indication, and VUR status. Institutions were classified as a free-standing pediatric hospital (FSPH, n=3), pediatric ‘hospital within a hospital’ (PHWH, n=11), or non-pediatric facility (NPF, n=24) and reports as having been read by a pediatric radiologist or not. Each category of outside reports (n=152) was randomly matched with a twice larger group of Hospital A reports from the same category (n=304). Multivariate linear regression was used to analyze the association between the primary outcome (percentage of items described in dictated VCUG report) and the type of radiologist and institution.
Results
Of the 456 studies, 66% were in females, 56% were in those <12 months old, and the indication was UTI in 81%. The mean percentage of items reported was 67±14%: 74±7% at FSPH, 61±10% at PHWH, and 48±11% at NPF. In multivariate analysis, VCUG reports generated at NPF had 17% fewer items included (95% CI: 14.5 – 19.7%, p<0.0001), and PHWH had 9% fewer items included (5.9 – 12.5%, p<0.0001), compared to FSPH. Reports read by a pediatric radiologist had 12% more items included (9.1–15.3%, p<0.0001), compared to those read by a non-pediatric radiologist.
Conclusion
More complete VCUG reports were observed when generated at FSPH and when interpreted by a pediatric radiologist.
MeSH Keywords: vesicoureteral reflux, radiology, fluoroscopy, quality improvement
Introduction
A voiding cystourethrogram (VCUG) is often part of the imaging evaluation for children with urinary tract infection (UTI) or prenatal hydronephrosis. The VCUG has the potential to provide a tremendous amount of information about the anatomic and functional status of the urinary tract, including identification of vesicoureteral reflux (VUR). One might expect that certain elements of the report would be consistently reported in all cases. However, our clinical experience has been that there is substantial variability both within and between institutions, which suggests that there is little standardization of the information documented in these reports.
Inconsistent reporting of findings is a common problem in radiology - reports are not all “created equal.” Studies have demonstrated wide variation in reporting standards for procedures as diverse as chest radiography, abdominal CT, mammography, and ultrasound [1–4]. Variations occur in description of the technique, clinical findings, terminology, final interpretations, and recommendations for patient management or further imaging. Itemized reports or templates have been proposed to address such inconsistencies[5,6], including a VCUG report template put forth by the Radiological Society of North America (RSNA)[7]. However, the use of such tools, and the consistency of VCUG reports in clinical practice has not been investigated.
In this study we sought to assess the completeness of VCUG reports arising from one of three types of institutions: free-standing pediatric hospitals (FSPH), pediatric hospitals within a hospital (PHWH), or non-pediatric facilities (NPF). Every report was assessed against a set of standard demographic, technical, anatomic, and functional parameters that should ideally be components of every VCUG report. We hypothesized that there would be significant variation in the completeness of VCUG reports comparing free-standing pediatric hospitals (FSPH) to other institutions.
Materials and Methods
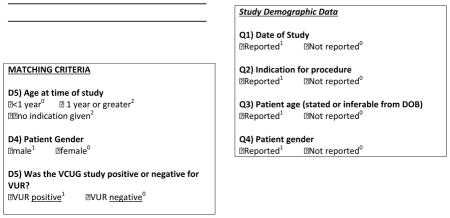
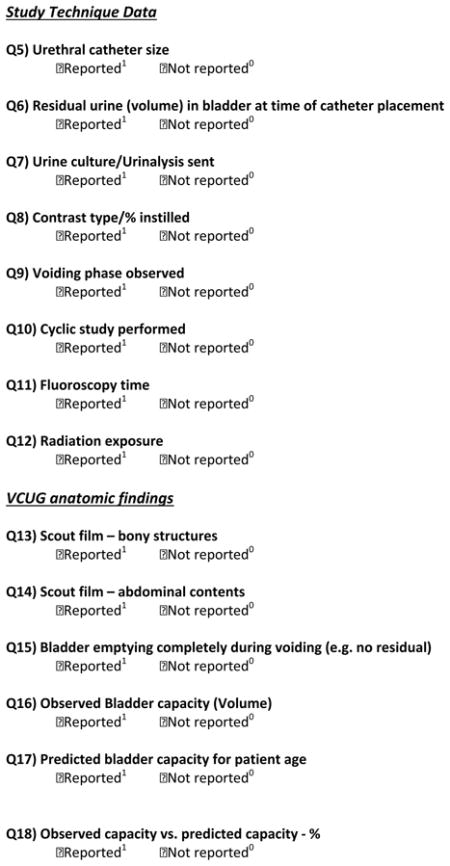
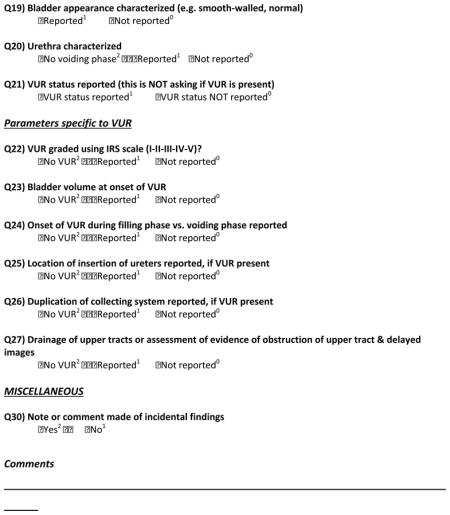
Standardized Assessment Tool
Pediatric radiologist and urologists from Hospital A created a standardized assessment tool used to measure the completeness of VCUG reports. This instrument incorporated 26 different variables related to demographic (e.g. age, gender, study indication), technical (e.g. catheterization technique with or without subsequent urine culture, single or multiple voiding phases), anatomic (e.g. bladder capacity, International Reflux Study (IRS) reflux grade, renal collecting system duplication), and functional (e.g. bladder emptying) information (see appendix). Reports from all facilities were compared to this idealized standard.
Selection of Cases and Controls
The aim of this study was to compare the documentation of VCUG report findings between free-standing pediatric hospitals, pediatric hospitals within a larger general hospital (PHWH), and non-pediatric facilities (NPF) using our assessment tool. Our hospital (Hospital A, a freestanding pediatric hospital with a dedicated pediatric genitourinary radiology team) was used as the control group. We determined a priori that the study period was 1/1/07–12/31/11. After IRB approval, reports of VCUGs performed at outside institutions during the study period, among patients referred to Hospital A for care, were identified through a HIPPA compliant retrospective review of medical records and our VUR and prenatal hydronephrosis databases. We similarly used radiology billing and medical records to identify all VCUG studies performed at Hospital A during the same period. A matched cohort was identified to control for specific patient characteristics and study findings that impact VCUG technique and subsequent reporting, as the prevalence of such factors may differ systematically between institutions. Age (<12 or ≥12 months) was matched because infants often have cyclic VCUGs [8], which increases the complexity of VCUG reporting. We also matched on gender (due to differences in urethral anatomy), study indication (UTI vs. prenatal hydronephrosis), and presence or absence of VUR (reports from studies with VUR will obviously include information that does not appear in studies without VUR e.g. VUR grade). After categorizing the reports according to these criteria, each group of outside VCUG reports was then matched with a twice larger group of internal (Hospital A) VCUG reports randomly selected from all internal reports with similar values for matching criteria. There were 152 outside VCUG reports and 304 internal (Hospital A) VCUG reports for analysis (total: 456 reports).
Categorization of Institutions and Radiologists
The Children’s Hospital Association (CHA) website was used to categorize the hospital where each VCUG originated as a free standing pediatric hospital (FSPH, n=3), a pediatric specialty hospital or a pediatric hospital within a larger general hospital (PHWH, n=11) [9]. If an institution was not present on the CHA website, it was classified as an NPF (n=24). Another potentially significant contributor to the VCUG report quality is whether the report was issued by a pediatric radiologist or non-pediatric radiologist. The Check Board Certification tool within the American Board of Radiology’s website was used to identify if the attending radiologist had pediatric subspecialty certification[10], in which case they were classified as a pediatric radiologist. For those without pediatric subspecialty certification or those not identified by the ABR’s tool, the website of the radiologist’s employer was searched to identify if they had completed a pediatric radiology fellowship, or if their research and/or clinical focus was dedicated solely to pediatric radiology. This ensured that radiologists who may be exempt from pediatric subspecialty certification by a ‘grandfather clause’ are classified appropriately.
Statistical Analysis
Each VCUG report was assessed with standardized assessment tool. The reports were abstracted by a single reviewer for consistency. For quality control a 10% subset of reports was reviewed by a second reviewer and the results compared; concordance was identified for over 99% of items. Using the quality measurement tool, one point was assigned for each item on the tool, for a maximum total of 26 points (20 points for those reports for which VUR was not seen). Each item was given equal weight. A score was assigned by dividing the number of points achieved for each report by the total number of possible points (20 or 26). This score represented the percent of variables assessed in each VCUG report and was the primary outcome.
Descriptive statistics were used to display relationships between significant hospital and provider characteristics and the percent of variables assessed. A multivariate linear regression was developed to analyze the association between the outcome and the type of institution where the report was generated and whether the report was read by a pediatric radiologist. Matching characteristics were controlled for in the model. Generalized estimating equations were used to account for correlations among reports generated within the same institution. The functional form of the outcome was investigated, and diagnostic checks and sensitivity to outliers of the fitted model were performed to verify model assumptions. All statistical tests were two-sided, and a significance level of p<0.05 was considered to indicate significance. SAS™ software v9.2 (SAS Institute Inc., Cary, NC, USA) was used for the analysis.
Results
Table 1 displays the characteristics of the 152 outside hospital and 304 internal (Hospital A) VCUG reports, each categorized according to hospital type.
Table 1.
Characteristics of VCUG studies
| Matching characteristic | All studies (n=456) | Source of VCUG report | ||
|---|---|---|---|---|
| FSPH (n=306 ) | PHWH (n=51) | NPF (n=99) | ||
| No. (%) | No. (%) | No. (%) | No. (%) | |
| Indication for VCUG | ||||
| Hydronephrosis | 87 (19) | 58 (19) | 17 (33) | 12 (12) |
| UTI | 369 (81) | 248 (81) | 34 (67) | 87 (88) |
|
| ||||
| VUR status | ||||
| Present | 354 (78) | 238 (78) | 42 (82) | 74 (75) |
| Absent | 102 (22) | 68 (22) | 9 (18) | 25 (25) |
|
| ||||
| Gender of patient | ||||
| Male | 153 (34) | 102 (33) | 19 (37) | 32 (32) |
| Female | 303 (66) | 204 (67) | 32 (63) | 67 (68) |
|
| ||||
| Age of patient | ||||
| <1 year | 255 (56) | 171 (56) | 34 (67) | 50 (51) |
| ≥1 year | 201 (44) | 135 (44) | 17 (33) | 49 (49) |
FSPH free-standing pediatric hospital, PHWH pediatric hospital within a larger general hospital NPF non-pediatric facility
There was wide variation in assessing specific VCUG report items (Table 2). No report assessed all items. Overall, the mean (SD) percentage of items assessed was 67 +/− 14%. Demographic characteristics were universally reported, but a number of other items were reported very infrequently, including clinical factors like collecting system duplication status and whether the VUR occurred during the filling and/or voiding phases of micturition. Although current protocols are stressing the importance of minimizing radiation exposure [11], less than half of all VCUGs (58% of FSPH, 14% of PHWH, and 2% of NPF) reported the radiation exposure associated with the procedure.
Table 2.
How frequently was each element of the VCUG assessed and reported?
| Item | All Hospitals (n=456) | Source of VCUG report | ||
|---|---|---|---|---|
| FSPH (n=306) | PHWH (n=51) | NPF (n=99) | ||
| No. (%) | No. (%) | No. (%) | No. (%) | |
| Date of study | 456 (100) | 306 (100) | 51 (100) | 99 (100) |
|
| ||||
| Indication for procedure | 456 (100) | 306 (100) | 51 (100) | 99 (100) |
|
| ||||
| Patient age | 454 (99.6) | 305 (99.7) | 51 (100) | 98 (99) |
|
| ||||
| Patient gender | 422 (93) | 303 (99) | 48 (94) | 71 (72) |
|
| ||||
| Urethral catheter size | 72 (16) | 8 (3) | 26 (51) | 38 (38) |
|
| ||||
| Residual urine (volume) in bladder at time of catheter placement | 312 (68) | 295 (96) | 13 (25) | 4 (4) |
|
| ||||
| Urine culture/urinalysis sent | 305 (67) | 275 (90) | 19 (37) | 11 (11) |
|
| ||||
| Contrast type/% instilled | 362 (79) | 252 (82) | 42 (82) | 68 (69) |
|
| ||||
| Voiding phase observed | 427 (94) | 294 (96) | 47 (92) | 86 (87) |
|
| ||||
| Cyclic study performed | 161 (35) | 136 (44) | 11 (22) | 14 (14) |
|
| ||||
| Fluoroscopy time | 226 (50) | 178 (58) | 20 (39) | 28 (28) |
|
| ||||
| Radiation exposure | 186 (41) | 177 (58) | 7 (14) | 2 (2) |
|
| ||||
| Scout film – bony structures | 321 (70) | 253 (83) | 36 (71) | 32 (32) |
|
| ||||
| Scout film – abdominal structures | 337 (74) | 274 (90) | 37 (73) | 26 (26) |
|
| ||||
| Bladder emptying completely during voiding (e.g., no residual) | 127 (28) | 38 (12) | 34 (67) | 55 (56) |
|
| ||||
| Observed bladder capacity | 380 (83) | 304 (99.3) | 39 (76) | 37 (37) |
|
| ||||
| Predicted bladder capacity | 297 (65) | 281 (92) | 12 (24) | 4 (4) |
|
| ||||
| Bladder appearance characterized (e.g. smooth-walled, normal) | 416 (91) | 299 (98) | 46 (90) | 71 (72) |
|
| ||||
| Urethra characterizeda | 396 (92) | 282 (95) | 45 (90) | 69 (78) |
|
| ||||
| VUR status reported | 456 (100) | 306 (100) | 51 (100) | 99 (100) |
|
| ||||
| VUR graded using IRS scaleb | 333 (95) | 232 (98) | 37 (88) | 64 (86) |
|
| ||||
| Bladder volume at onset of VURb | 12 (3) | 2 (0.01) | 3 (7) | 7 (9) |
|
| ||||
| Onset of VUR during filling phase vs. voiding phaseb | 63 (18) | 9 (4) | 14 (33) | 40 (54) |
|
| ||||
| Location of insertion of ureters reportedb | 235 (67) | 203 (86) | 13 (31) | 19 (26) |
|
| ||||
| Duplication of collecting system reportedb | 18 (5) | 10 (4) | 5 (12) | 3 (4) |
|
| ||||
| Drainage of upper tracts or assessment of evidence of obstruction of upper tract & delayed imagesb | 224 (64) | 197 (83) | 11 (26) | 16 (22) |
FSPH free-standing pediatric hospital, PHWH pediatric hospital within a larger general hospital, NPF non-pediatric facility, VCUG voiding cystourethrogram, VUR vesicoureteral reflux
Voiding phase was not observed in 10 FSPH, 1 PHWH and 10 NPF reports
These items were only assessed among the 352 reports (236 FSPH, 42 PHWH and 74 NPF) with vesicoureteral reflux
In univariate analyses, a substantial difference in VCUG report quality among institutions was observed; FSPH assessed 74 +/− 7% of items compared to PHWH, which assessed 61 +/− 10% of items (p<0.0001), and NPF, which assessed 48 +/− 11% of items (p<0.0001). The average number of variables assessed by a pediatric radiologist was 72 +/− 9% compared to 46 +/− 10% when the report was read by a non-pediatric radiologist, p=0.02 (Table 3). After controlling for the type of radiologist reading the report, gender, study indication, age at time of VCUG, and whether the report was positive or negative for VUR, a report generated at an NPF compared to one generated at a FSPH had on average 17% (95% CI: 14.5–19.7%) fewer variables assessed, p<0.0001 (Table 4). Similarly, a report generated at a PHWH compared to one generated at a FSPH had on average 9% (95% CI: 6–12.5%) fewer variables assessed, p<0.0001. Finally, a report that was read by a pediatric radiologist compared to one read by a non-pediatric radiologist had on average 12.1% (95% CI: 9.1–15.3%) more variables assessed, p<0.0001.
Table 3.
Univariate associations between percentage of items assessed in VCUG reports and the type of hospital and report characteristics
| Characteristic | Mean percentage (SD) of items assessed | Difference in percentage of variables assessed in VCUG report (95% CI) | P-value |
|---|---|---|---|
| Overall study sample | 67±4 | -- | -- |
|
| |||
| Institution where study performed | |||
| Non-pediatric Facility | 48±1 | −25.9 (−29.0, −22.7) | <0.0001 |
| Pediatric hospital within a hospital | 61±0 | −13.3 (−18.4, −8.15) | <0.0001 |
| Free-standing pediatric hospital | 74±7 | Ref | -- |
|
| |||
| Report signed by pediatric radiologist | |||
| Yes | 72±9 | 11.7 (2.1, 21.4) | 0.02 |
| No | 46±10 | Ref | -- |
|
| |||
| Study indication | |||
| Hydronephrosis | 72±12 | 4.3 (3.2, 5.3) | <0.0001 |
| UTI | 66±14 | Ref | -- |
|
| |||
| Age at time of study | |||
| >1 year | 65±13 | −1.7 (−2.7, −0.1) | 0.003 |
| ≤1 year | 68±14 | Ref | -- |
|
| |||
| Patient gender | |||
| Male | 69±13 | 1.8 (0.1, 3.1) | 0.004 |
| Female | 66±14 | Ref | -- |
|
| |||
| Vesicoureteral reflux present | |||
| Yes | 65±13 | −9.0 (−10.0, −8.0) | <0.0001 |
| No | 74±14 | Ref | -- |
CI confidence interval, SD standard deviation, UTI urinary tract infection, VCUG voiding cystourethrogram
Table 4.
Multivariate analysis of the association between the percentage of items assessed in VCUG reports and the type of hospital and report characteristics.
| Characteristic | Difference in percentage of variables assessed in VCUG report (95% CI) | P-value |
|---|---|---|
| Institution where study performed | ||
| Non-pediatric facility | −17.2 (−19.8, −14.5) | <0.0001 |
| Pediatric hospital within a hospital | −9.2 (−12.5, −5.9) | <0.0001 |
| Free-standing pediatric hospital | Ref | -- |
|
| ||
| Report signed by pediatric radiologist | ||
| Yes | 12.1 (9.1, 15.3) | <0.0001 |
| No | Ref | -- |
|
| ||
| Study indication | ||
| Hydronephrosis | 1.2 (0, 2.7) | 0.12 |
| UTI | Ref | -- |
|
| ||
| Age at time of study | ||
| >1 year | −0.1 (−2.4, 0.1) | 0.24 |
| ≤1 year | Ref | -- |
|
| ||
| Patient gender | ||
| Male | −0.1 (−3.1, 1.7) | 0.59 |
| Female | Ref | -- |
|
| ||
| Vesicoureteral reflux present | ||
| Yes | −9.4 (−11.0, −7.8) | <0.0001 |
| No | Ref | -- |
UTI urinary tract infection, VCUG voiding cystourethrogram
Discussion
In this study we observed great variation among facilities in the completeness of VCUG reports, with more complete reports being observed at pediatric specialty centers. If the primary aim of the VCUG is simply to assess for the presence or absence of VUR, all centers performed exceedingly well with 100% reporting of this parameter. However, the VCUG is a study that is able to assess much more than the presence or absence of VUR. If assessed and subsequently reported in the VCUG, a ‘Christmas tree’ shaped bladder with bladder diverticula, a low bladder capacity, and a funneled urethra could indicate a neurogenic bladder. Similarly, a dilated prostatic urethra could suggest posterior urethral valves as the reason for secondary vesicoureteral reflux. In cases where VUR is identified, important information such as the reflux grade, the bladder volume at the onset of reflux, whether the reflux occurred during the filling or voiding phases of the study, and an assessment of the presence or absence of periureteral diverticula provide important prognostic information to guide the clinician’s counseling and management plan [12–15]. Here we show that a significant number of all VCUG reports lack these important anatomic and functional assessments, but that reports generated at FSPH or PHWH had more complete reports than those generated at non-pediatric institutions, as did those that were read by a pediatric radiologist.
There are several reasons that could explain the large variation in VCUG reporting. Multidisciplinary conferences at pediatric tertiary centers may facilitate communication and collaboration between pediatric radiologists and pediatric urologists, thus helping radiologists understand the type of information of greatest importance to other clinicians. Moreover, these hospitals likely have a higher volume of these procedures, which increases the radiologists’ familiarity with the technique and the important non-reflux-related anatomic and functional components of the VCUG report.
The frequency of omissions in key components of the VCUG at FSPH, PHWH, and non-pediatric institutions demonstrates that there is room for improvement at all institutions. Items consistently omitted from reports include whether a cyclic study was performed, which can improve the diagnostic accuracy of a VCUG [8], and whether the VUR occurred during the filling or voiding phase, which can help prognostication [14]. Another potential target for improved reporting at all institutions is the description of the collecting system as single or duplicated (among patients with VUR). Should definitive management be necessary, knowing whether the collecting system is duplicated has implications for the pediatric urologist’s surgical approach. Even in cases where a cyclic study was performed, or the phase at which VUR first occurred was noted, or the duplication status was assessed, failure to include these details explicitly in the report forces the clinician to guess as to whether the omission means that the finding was not present, or was not assessed at all. This is a clear opportunity for quality improvement.
These findings are relevant within the broader context of the health care system because payers such as insurance companies increasingly treat radiology as a commodity. This is based on the premise that, for a particular diagnostic study, comparable reports can be generated at any facility. Payers therefore incentivize patients to undergo diagnostic imaging at lower-cost general radiology facilities instead of specialized tertiary care centers [16,17]. The current findings suggest that, given the wide variation in reporting, the decline in quality associated with such a strategy is measureable, and may be substantial. The completeness of VCUG reports as measured by content was significantly higher at pediatric hospitals, and when pediatric radiologists generated the reports. Thus, the adoption and promulgation of standardized reporting templates, in addition to advancing knowledge in the nuances of pediatric radiology techniques at non-pediatric facilities, could improve the quality of VCUG reports and possibly the quality of the study itself. Until these measures are undertaken, pediatric patients may benefit from having studies performed at high-volume specialized pediatric centers.
The low rate of radiation exposure level reporting is concerning for a number of reasons. Medical radiation exposure among pediatric patients is increasingly recognized as a significant public health issue [18,19]. There is evidence that simply reporting exposure levels during diagnostic imaging procedures may result in lowering of subsequent exposure levels [20], perhaps related to a so-called “Hawthorne effect” wherein the act of measuring the parameter leads to changes in behavior among the observed[21]. Although in this study we measured only the reporting of radiation exposure, and not the levels themselves, other investigators have found that imaging equipment at general adult and even some pediatric facilities may not be routinely adjusted for pediatric patients or different pediatric age groups, resulting in higher-than-necessary exposure levels [22,18,19,23].
Furthermore, an incomplete VCUG report may lead to increased radiation exposure by requiring repeat imaging. Unlike CT scans and MRI studies in which all of the imaging data is recorded (and all images can be reexamined or reinterpreted), most radiology departments only store a few representative VCUG images at study completion. The report is therefore the only opportunity for complete documentation of the observed findings, other than the selected saved images themselves. For example, if a VCUG report for a male infant does not include a statement regarding the urethra, and urethral images were not saved, then a repeat study may be required, thereby exposing the child to unnecessary radiation. Thus, strategies to improve the completeness of VCUG reports could not only help the radiographic assessment of the child with VUR, but also improve the quality of the report and reduce the harm from diagnostic radiation in these children.
The results of this study should be interpreted in light of its limitations. Most significant among these is the relatively selective nature of the VCUG reports that were available for review. The great majority of pediatric hospital reports came from our own facility, while the outside reports came from a more diverse set of facilities. This raises issues of selection, particularly if the outside studies are more likely to have certain characteristics, such as presence of VUR. We attempted to address this by explicitly matching for several characteristics that appeared to be differentially distributed between outside and internal (Hospital A) reports and by using generalized estimating equations to account for the correlation in reports generated at particular hospitals. Another limitation is that the 26-item quality assessment tool was devised by our own pediatric radiologists and pediatric urologists, based on technical and clinical factors that we thought important in a VGUG report. The choice of items therefore reflects the clinical biases and preferences of the study authors and their colleagues. While these decisions were somewhat subjective, the included items were not chosen simply because they were routinely reported at our institution; indeed, it turns out that our institution performed poorly for several items, including catheter size, bladder emptying during voiding, and the phase of VUR onset (filling or voiding), as well as other items). Also, in requiring key items not included in the RSNA template[7], the tool used in this study is more stringent. For example, our tool assessed whether the IRS VUR grade, the phase of VUR onset (filling or voiding), and upper tract drainage after voiding were reported, among others. Even given these differences in report measurement tools, the discrepancies in reporting between FSPH and non-pediatric institutions are of such large magnitude that changes in the quality assessment tool are not likely to substantially change the results. Although inclusion of items queried in our study may lead to a longer VCUG report, it is our opinion that they also produce a report that provides a more complete picture of the anatomic and functional characteristics of the upper and lower urinary tracts. The aim of this study was not to devise an ideal VCUG report template, but rather to highlight the variation in VCUG reporting between institutions. Such a task should be left to a consensus decision among key stakeholders from the radiologic, nephrourologic, and general pediatric communities. Finally, this study focused on the content of the VCUG report itself, not on the accuracy or reliability of the clinical findings. We cannot state whether the findings of the diagnostic study (e.g. VUR grade) were more or less accurate at certain facilities compared to others. However, clinical accuracy has been studied extensively within the radiology literature, and substantial variation has been observed among institutions in numerous settings [24–27]; there is little reason to expect different results in the VCUG context.
Conclusion
Documentation of VCUG findings varies significantly, with more complete reports observed at pediatric centers. Quality improvement strategies such as template-driven VCUG reports may improve the completeness of VCUG reports, regardless of facility. In the absence of such systematic change, our findings suggest that the quality and completeness of VCUG reports is significantly dependent on both the interpreting radiologist and the center at which the study is performed.
Abbreviations
- VUR
Vesicoureteral Reflux
- VCUG
Voiding Cystourethrogram
- FSPH
Free-standing Pediatric Hospital
- PHWH
Pediatric Hospital within a Hospital
- NPF
Non-pediatric Facility
- RSNA
Radiological Society of North America
- IRS
International Reflux Study
- ABR
American Board of Radiology
APPENDIX: Form generated by Hospital A urologist and pediatric radiologists and used to systematically analyzed all VCUG reports

Footnotes
COI Statement:
All authors of this manuscript have NO affiliations with or involvement in any organization or entity for which a financial or non-financial interest exist for the material in this manuscript.
References
- 1.Houssami N, Boyages J, Stuart K, Brennan M. Quality of breast imaging reports falls short of recommended standards. Breast. 2007;16 (3):271–279. doi: 10.1016/j.breast.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Lee R, Cohen MD, Jennings GS. A new method of evaluating the quality of radiology reports. Acad Radiol. 2006;13 (2):241–248. doi: 10.1016/j.acra.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz LH, Panicek DM, Berk AR, Li Y, Hricak H. Improving communication of diagnostic radiology findings through structured reporting. Radiology. 2011;260 (1):174–181. doi: 10.1148/radiol.11101913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Le T, Fayadh RA, Menard C, Hicks-Boucher W, Faught W, Hopkins L, Fung-Kee-Fung M. Variations in ultrasound reporting on patients referred for investigation of ovarian masses. J Obstet Gynaecol Can. 2008;30 (10):902–906. doi: 10.1016/S1701-2163(16)32970-X. [DOI] [PubMed] [Google Scholar]
- 5.Sistrom CL, Langlotz CP. A framework for improving radiology reporting. J Am Coll Radiol. 2005;2 (2):159–167. doi: 10.1016/j.jacr.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 6.Bosmans JM, Weyler JJ, De Schepper AM, Parizel PM. The radiology report as seen by radiologists and referring clinicians: results of the COVER and ROVER surveys. Radiology. 2011;259 (1):184–195. doi: 10.1148/radiol.10101045. [DOI] [PubMed] [Google Scholar]
- 7.Meyer J. [Accessed September 30 2013];Radiological Society of North America Radiology Reporting Templates. 2012 http://www.radreport.org/template/0000110.
- 8.Papadopoulou F, Efremidis SC, Oiconomou A, Badouraki M, Panteleli M, Papachristou F, Soteriou I. Cyclic voiding cystourethrography: is vesicoureteral reflux missed with standard voiding cystourethrography? Eur Radiol. 2002;12 (3):666–670. doi: 10.1007/s003300101108. [DOI] [PubMed] [Google Scholar]
- 9.Children’s Hospital Association-Find a Children’s Hospital. [Accessed October 1 2012];2012 http://www.childrenshospitals.net.
- 10.American Board of Radiology-Check Board Certification. [Accessed January 30 2014];2014 http://www.theabr.org.
- 11.Frush DP, Donnelly LF, Rosen NS. Computed tomography and radiation risks: what pediatric health care providers should know. Pediatrics. 2003;112 (4):951–957. doi: 10.1542/peds.112.4.951. [DOI] [PubMed] [Google Scholar]
- 12.Knudson MJ, Austin JC, McMillan ZM, Hawtrey CE, Cooper CS. Predictive factors of early spontaneous resolution in children with primary vesicoureteral reflux. J Urol. 2007;178 (4 Pt 2):1684–1688. doi: 10.1016/j.juro.2007.03.161. [DOI] [PubMed] [Google Scholar]
- 13.Barrett DM, Malek RS, Kelalis PP. Observations on vesical diverticulum in childhood. J Urol. 1976;116 (2):234–236. doi: 10.1016/s0022-5347(17)58760-1. [DOI] [PubMed] [Google Scholar]
- 14.Arsanjani A, Alagiri M. Identification of filling versus voiding reflux as predictor of clinical outcome. Urology. 2007;70 (2):351–354. doi: 10.1016/j.urology.2007.03.031. [DOI] [PubMed] [Google Scholar]
- 15.Estrada CR, Jr, Passerotti CC, Graham DA, Peters CA, Bauer SB, Diamond DA, Cilento BG, Jr, Borer JG, Cendron M, Nelson CP, Lee RS, Zhou J, Retik AB, Nguyen HT. Nomograms for predicting annual resolution rate of primary vesicoureteral reflux: results from 2,462 children. J Urol. 2009;182 (4):1535–1541. doi: 10.1016/j.juro.2009.06.053. [DOI] [PubMed] [Google Scholar]
- 16.Tynan A, Berenson RA, Christianson JB. Health plans target advanced imaging services: cost, quality and safety concerns prompt renewed oversight. Issue Brief Cent Stud Health Syst Change. 2008;(118):1–4. [PubMed] [Google Scholar]
- 17.Andrews M. Some Insurers Paying Patients Who Agree To Get Cheaper Care. [Accessed December 15 2012];Kaiser Health News. 2012 http://www.kaiserhealthnews.org/Features/Insuring-Your-Health/2012/Cash-Rewards-For-Cheaper-Care-Michelle-Andrews-032712.aspx.
- 18.Goske MJ, Applegate KE, Bulas D, Butler PF, Callahan MJ, Coley BD, Don S, Frush DP, Hernanz-Schulman M, Kaste SC, Morrison G, Sidhu M, Strauss KJ, Treves ST. Image Gently: progress and challenges in CT education and advocacy. Pediatr Radiol. 2011;41(Suppl 2):461–466. doi: 10.1007/s00247-011-2133-0. [DOI] [PubMed] [Google Scholar]
- 19.Sidhu M, Goske MJ, Connolly B, Racadio J, Yoshizumi TT, Strauss KJ, Coley BD, Utley T. Image Gently, Step Lightly: promoting radiation safety in pediatric interventional radiology. AJR Am J Roentgenol. 2010;195 (4):W299–301. doi: 10.2214/AJR.09.3938. [DOI] [PubMed] [Google Scholar]
- 20.Darling S, Sammer M, Chapman T, Parisi MT. Physician documentation of fluoroscopy time in voiding cystourethrography reports correlates with lower fluoroscopy times: a surrogate marker of patient radiation exposure. AJR Am J Roentgenol. 2011;196 (6):W777–780. doi: 10.2214/AJR.10.5827. [DOI] [PubMed] [Google Scholar]
- 21.Mayo E. The human problems of an industrial civilization. 2. Vol. 3. MacMillan; New York, NY: 1993. [Google Scholar]
- 22.Paterson A, Frush DP, Donnelly LF. Helical CT of the body: are settings adjusted for pediatric patients? AJR Am J Roentgenol. 2001;176 (2):297–301. doi: 10.2214/ajr.176.2.1760297. [DOI] [PubMed] [Google Scholar]
- 23.Hollingsworth C, Frush DP, Cross M, Lucaya J. Helical CT of the body: a survey of techniques used for pediatric patients. AJR Am J Roentgenol. 2003;180 (2):401–406. doi: 10.2214/ajr.180.2.1800401. [DOI] [PubMed] [Google Scholar]
- 24.Eakins C, Ellis WD, Pruthi S, Johnson DP, Hernanz-Schulman M, Yu C, Kan JH. Second opinion interpretations by specialty radiologists at a pediatric hospital: rate of disagreement and clinical implications. AJR Am J Roentgenol. 2012;199 (4):916–920. doi: 10.2214/AJR.11.7662. [DOI] [PubMed] [Google Scholar]
- 25.Gollub MJ, Panicek DM, Bach AM, Penalver A, Castellino RA. Clinical importance of reinterpretation of body CT scans obtained elsewhere in patients referred for care at a tertiary cancer center. Radiology. 1999;210 (1):109–112. doi: 10.1148/radiology.210.1.r99ja47109. [DOI] [PubMed] [Google Scholar]
- 26.Sung JC, Sodickson A, Ledbetter S. Outside CT imaging among emergency department transfer patients. J Am Coll Radiol. 2009;6 (9):626–632. doi: 10.1016/j.jacr.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 27.Loevner LA, Sonners AI, Schulman BJ, Slawek K, Weber RS, Rosenthal DI, Moonis G, Chalian AA. Reinterpretation of cross-sectional images in patients with head and neck cancer in the setting of a multidisciplinary cancer center. AJNR Am J Neuroradiol. 2002;23 (10):1622–1626. [PMC free article] [PubMed] [Google Scholar]


