Abstract
Objective
A large body of factor analytic research supports the idea that common mental disorders are organized along correlated latent dimensions termed internalizing and externalizing. Eating disorders (EDs) have been associated with both internalizing (mood and anxiety disorders) and externalizing (substance use, antisocial personality disorder) forms of psychopathology. Previous studies found that EDs are best classified as internalizing disorders. However, no previous factor analytic studies of EDs and the internalizing/externalizing dimensions have evaluated if the EDs align with these spectra similarly for men and women. We examined the location of anorexia nervosa (AN), bulimia nervosa (BN) and binge eating disorder (BED) symptoms within this model of psychopathology among a sample of veterans, a population traditionally understudied in EDs.
Method
Data were from two studies of veterans and their intimate partners (N = 453 men and 307 women). Participants were administered the Structured Clinical Interview for DSM-IV without skip-outs. Lifetime symptom severity scores were used in confirmatory factor analytic models.
Results
A model with AN, BN, and BED symptoms loading onto the distress sub-factor of the internalizing domain fit the data best in the full sample and the male and female subsamples. This model was statistically equivalent for men and women.
Discussion
All three EDs loaded onto distress, indicating that these conditions overlap with psychopathology characterized by negative affect. Investigating latent dimensions of psychopathology is one approach to identifying common factors that partially account for patterns of comorbidity among psychiatric disorders which may aid in translating research findings into clinical practice.
Keywords: eating disorders, internalizing, externalizing, gender, comorbidity
Eating disorders (EDs) are pernicious, multi-factorial conditions whose complexity is further compounded by their high rate of comorbidity with many other psychiatric disorders,1,2 especially depression, anxiety, personality, and substance use disorders. In the National Comorbidity Study-Replication, 47.9% of individuals with a history of anorexia nervosa (AN) had a history of an anxiety disorder, and 42.1% had a history of a depressive disorder. Among those with a history of bulimia nervosa (BN) these rates were 80.6% and 70.7%, respectively, and in individuals with a history of binge eating disorder (BED), 65.1% and 46.4%, respectively. The prevalence of a substance use disorder among individuals with AN, BN, and BED was 27.0%, 36.8%, and 23.3%2.
One of the more influential contemporary models of psychiatric comorbidity is the internalizing/externalizing model, which organizes diagnoses on the basis of their associations with underlying liabilities. These higher-order liability factors, termed “internalizing,” representing mood and anxiety psychopathology, and “externalizing,” representing substance use disorders, antisociality, and conduct disorders, may account for a large proportion of the covariation among mental disorders3,4.
Factor analytic studies generally have supported the hypothesis that common psychiatric disorders load onto either a latent internalizing or externalizing factor. For example, Krueger et al.4 found evidence for a two factor model among both women and men: major depression, panic disorder, simple phobia, and social phobia loaded onto the internalizing factor; and alcohol dependence, cannabis dependence, drug dependence, and adult antisocial behavior loaded onto the externalizing latent factor. This basic structure has been replicated in many factor analytic investigations, although in some models, the internalizing factor is bifurcated into two correlated subfactors: fear (panic disorder, simple phobia, and social phobia) and distress or anxious/misery (major depression, dysthymia, and generalized anxiety disorder). A recent examination of a model in which common psychiatric disorders loaded onto distress/anxious misery, fear, and externalizing found that this model was invariant for women and men, suggesting that the structure of psychiatric comorbidity may be equivalent across genders3.
Until recently, factor analytic models of internalizing and externalizing dimensions of psychopathology have not included eating disorders. Forbush and colleagues5, in a sample of female twins, estimated a series of models to determine the location of eating pathology along the internalizing-externalizing dimension. They used a combined BN and BED variable and AN as indicators of a latent ED variable. The model with latent factors representing distress, fear, and EDs loading on a higher-order internalizing factor fit the data better than models in which the EDs loaded onto externalizing, or cross-loaded onto both latent variables. Forbush and Watson6 replicated this finding in an expanded internalizing/externalizing model that included both common and uncommon mental health diagnoses in a nationally representative sample of men and women.
The underlying association between the internalizing and externalizing dimensions and EDs is of particular relevance to the study of gender in the etiology of EDs. It has long been thought that EDs affect women at much higher rates compared to men. However, population-based studies have shown that men comprise a higher percentage of ED cases than previously believed2. Further, men and women have fairly comparable rates of binge eating and BED7,8. In general, men have a higher prevalence of externalizing disorders, such as substance use disorders, while women have a higher prevalence of internalizing disorders, including depression and anxiety3,9,10. Thus, there may be important gender differences in patterns of comorbidity across the EDs and other disorders that reflect the influence of these latent dimensions.
One population that has been understudied with respect to EDs is veterans. Preliminary findings suggest that rates of these conditions among military and veteran samples are comparable to those in the general population, if not higher11. The high overall rates of psychiatric morbidity among veterans, including depression and substance use disorders12,13, suggest the need to further evaluate the EDs in this predominantly male population.
To date, few extant studies have included EDs in comprehensive models of internalizing/externalizing, and none have examined measurement invariance across women and men5,6. This study estimated a series of models, including the four tested by Forbush et al.,5 of mood, anxiety, substance use disorders, and ED symptom severity, among a sample of male and female veterans and civilians to determine the location of the ED symptoms along the internalizing and externalizing dimensions. Analyses were conducted on data from a study originally collected to evaluate the latent structure of PTSD comorbidity in trauma-exposed veterans and their intimate partners. Because of the selected nature of this sample, and high prevalence of PTSD, PTSD was not included in the models of psychiatric comorbidity, and the final model controlled for lifetime trauma exposure, as described below. Based on previous research14, we hypothesized that AN, BN, and BED would load onto the internalizing latent factor. In addition, we hypothesized that although mean symptom levels of disorders would differ significantly for men and women (termed scalar non-invariance), the overall factor structure and association between these EDs and the latent psychopathology dimensions would be similar among men and women (termed metric invariance).
Method
Participants
Participants were U.S. military veterans and their intimate partners (N = 852), who enrolled in one of two studies with near overlapping procedures at a large urban Northeastern Veterans Affairs (VA) Medical Center or a large Southwestern VA Medical Center. As described previously15, one study recruited male and female veterans who reported exposure to a traumatic event consistent with DSM-IV PTSD Criterion A. Intimate partners with whom the veterans had been cohabitating for ≥ 12 months prior to the study were recruited as well. The second study recruited trauma-exposed male and female veterans who exceeded the cutoff on the PTSD Checklist-Civilian Version (PCL-C)16 indicating probable PTSD.
From the original sample, participants were excluded from the current analyses for the following reasons: 44 had completed both studies (data were entered only once), and 48 did not complete at least one interview or were terminated due to problems conforming their behavior to protocol expectations (e.g., repeatedly falling asleep during the interview). Thus, the current analyses included 760 participants (N = 307 women and 453 men); 513 were veterans.
Procedure
Participants were recruited via flyers, mailings, clinician referrals, and from a research participant database. Eligibility criteria included age of > 18 years and able to read and speak English. Participants meeting these criteria provided informed consent and were administered interviews by advanced psychology graduate students, postdoctoral-level clinical psychology trainees, or licensed clinical psychologists. Intimate partners underwent identical assessment procedures as veterans. All interviews were videotaped for the purposes of evaluating diagnostic reliability and preventing rater drift. Approximately 25% of the videotapes were subsequently viewed by a second rater to determine inter-rater reliability. The local Institutional Review Boards approved all study procedures.
Measures
Structured Clinical Interview for the DSM-IV (SCID)
The SCID17 was used to assess lifetime Axis I disorders. Consistent with a dimensional conceptualization of psychopathology (Watson, 2005), SCID skip-outs were ignored so that each item was administered in each module, and items were summed to create severity scores. Because of this, the wording of some items was changed very slightly to accommodate the lack of skip-outs. For example, the first AN item is “Have you ever had a time when you weighed much less than other people thought you ought to weigh?” For participants who said no (and would normally skip the second item), rather than asking “at that time were you very afraid you could become fat?” they were asked “Have you ever been very afraid that you could become fat?” In this way, all items were administered in a manner that was relevant for all participants, regardless of whether the typical skip-out items were endorsed. In addition, the interviewers assessed whether symptoms for a given disorder were anchored together in time.
Lifetime severity of AN, BN, BED, major depression, generalized anxiety disorder, panic disorder, agoraphobia, specific phobia, and obsessive-compulsive disorder were included. Current severity of dysthymia was included, as the SCID does not assess lifetime dysthymia. Because men could not endorse the amenorrhea criterion for AN, resulting in a lower possible range of scores, z-scores were computed separately for men and women and used in the models. In addition, abuse and dependence severity scores were summed for alcohol, cannabis, and cocaine use disorders. These three disorders were selected, as they were the most commonly endorsed substance use disorders in this sample. Due to the high prevalence of PTSD (55.6%), this disorder was not included in the models. Intraclass correlations (ICCs) were calculated to determine inter-rater reliability for lifetime BN (.94), BED (.97), and major depressive disorder (.96) severity scores. ICCs for the other SCID-based lifetime severity scores ranged from .88 for obsessive-compulsive disorder severity to .97 for panic disorder severity18.
Adult Antisociality
Adult antisociality was assessed using two different measures. The International Personality Disorder Examination (IPDE)19 was administered in the veteranonly study, and the SCID-II20 was administered in the study which enrolled veterans and their partners. We created a single adult antisocial scale by standardizing matching items across the two measures so as to place the items on the same metric and then summed these items to create a total score. The ICC for adult antisocial features was .95.
Traumatic Life Events Questionnaire (TLEQ)
The TLEQ is a self-report measure of exposure to a range of potentially traumatic events. This instrument, which has been validated among demographically diverse adult samples, has adequate test-retest reliability and content validity (Kubany et al., 2000). The number of different lifetime trauma types was used as a covariate in the final model, as described below.
Statistical Analysis
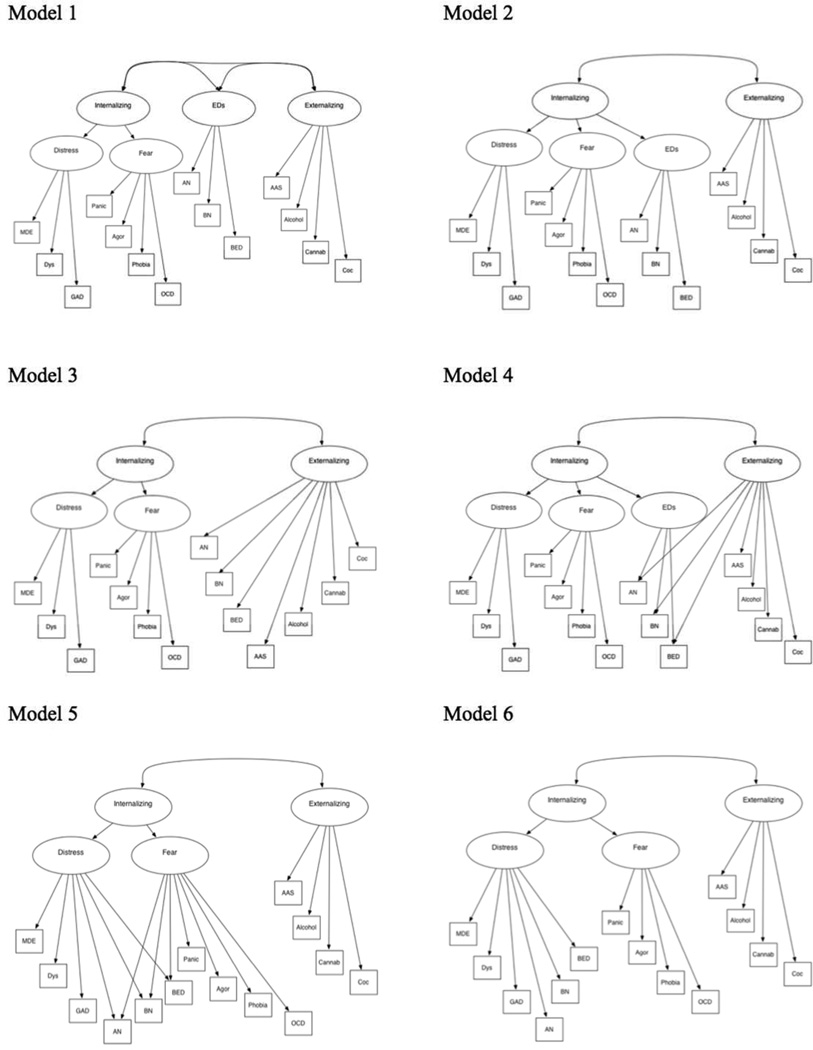
Descriptive statistics were computed using PASW Statistics 18.021. Confirmatory factor analyses were estimated using Mplus version 7.1122. The cluster option was used to account for the correlated nature of the data for couples. The residual variances of cocaine abuse/dependence and cannabis abuse/dependence were correlated in the models to account for their shared method variance (i.e., they are assessed using the same questions in the SCID). We first replicated the models tested by Forbush et al.5: 1) a model with a latent ED variable (with AN, BN, and BED severity indicators, which was free to correlate with the internalizing and externalizing factors, 2) a model with second-order distress, fear, and ED factors which loaded on a higher-order internalizing factor, 3) a model with AN, BN, and BED severity as indicators of the externalizing factor which was correlated with a higher-order internalizing variable, and 4) a model with AN, BN, and BED indicators cross-loading on a lower-order ED factor and externalizing and with the ED factor loading on a higher-order internalizing variable (see Figure 1). We used the Bayesian Information Criterion (BIC) to select the best-fitting model; the model with the lowest BIC is preferred23.
Figure 1. Theoretical models.
Note: Models 1–4 are from Forbush et al.5 MDE=major depressive episode, Dys=dysthymia, GAD=generalized anxiety disorder, AN=anorexia nervosa, BN=bulimia nervosa, BED=binge eating disorder, Panic=panic disorder, Agor=agoraphobia, phobia=specific phobia, OCD=obsessive compulsive disorder, AAS=adult antisociality, Alcohol=alcohol abuse/dependence, Cannab=cannabis abuse/dependence, Coc=cocaine abuse/dependence. All measured variables are continuous, lifetime severity scores.
We also tested two additional models that did not include EDs as a separate latent factor in order to determine whether AN, BN, and BED severity variables would load directly onto the distress or fear latent variables. In addition to wanting to explore whether EDs were most closely related to distress or fear disorders, we also hypothesized that EDs may have loaded onto a separate ED latent variable in the Forbush et al.5,6 papers because they share method variance. Specifically, the same two items in the SCID are used to assess binge eating and loss of control for both BN and BED. Thus, we correlated the residual variances of these two severity scores and compared: 5) a model with all three ED indicators loading onto both distress and fear, and 6) a model with all three ED indicators loading onto distress only. Models 5 and 6 were compared using the BIC; the best-fitting model was then compared to the best-fitting model from Forbush et al5.
The best-fitting model was then estimated separately for the male and female subsamples in order to compare the pattern of results by gender. In addition, multigroup model comparisons were conducted to assess whether the model was statistically equivalent (i.e., invariant) across genders. A model with the same parameters estimated freely for men and women (i.e., equal form), respectively, was compared to a model with factor loadings constrained to be equal across groups. If full or partial measurement invariance is established, then it is possible to test scalar invariance, or equivalence of indicator intercepts. At least partial measurement invariance and scalar invariance is required to conduct additional tests of measurement invariance, e.g., latent factor means and item residuals24. The BIC was used to compare models; a higher BIC for the model with parameters equated, compared to the model with parameters estimating freely in both samples, indicates that the parameters are not equivalent. In addition, the chi-square difference test was used to compare models; a significant chi-square indicates that the parameters are not invariant. The Satorra-Bentler scaled chi-square difference test was used to compare nested models22.
Robust maximum likelihood (MLR) was used, as this method of estimation is robust to non-normality and non-independence of data. The comparative fit index (CFI), Tucker Lewis index (TLI), standardize root mean square residual (SRMR) and root mean squared error of approximation (RMSEA) were used to examine omnibus fit for all models.
Results
Descriptives
Participants’ mean age was 51.43 (SD = 10.91). The majority (66.6%) were married, 9.9% were single or never married, 14.2% were divorced/separated, 8.0% were cohabitating, and .9% were widowed. Nearly half (49%) had incomes ≤ $30,000; 10.6% had less than a high school education, and 15.3% had a high school diploma or high school equivalency credential. The majority (67.7%) had at least some college. Regarding race and ethnicity, 81.3% were Caucasian, 15.0% were Hispanic/Latino/a, 11.8% were African American, 1.1% were Asian, 8.7% were Native American or Alaskan Native, .5% were Hawaiian or Pacific Islander, and 5.5% reported that their race was unknown (categories are not mutually exclusive).
Five women met lifetime criteria for AN (1.6%), five (1.6%) met criteria for BN, and 10 (3.3%) met criteria for BED. None of the men met criteria for lifetime AN. Two men (.4%) met criteria for lifetime BN, and 15 (3.3%) met criteria for BED; evaluation of diagnostic prevalence followed standard SCID scoring rules. See Table 1 for rates of Axis I and II diagnoses in the full sample and within the male, female, veteran, and intimate partner subsamples.
Table 1.
Lifetime diagnoses in the total sample and veteran, intimate partner, and female and male subsamples
| Lifetime Diagnoses | Total Sample (N = 760) |
Study 1 Veterans (n = 225) |
Study 2 Veterans (n = 283) |
Study 2 Partners (n = 294) |
Women (n = 307) |
Men (n = 453) |
|---|---|---|---|---|---|---|
| Anorexia nervosa | 5 (0.7) | 2 (1.0) | 0 | 3 (1.1) | 5 (1.6) | 0 |
| Bulimia nervosa | 7 (0.9) | 1 (0.5) | 1 (0.4) | 5 (1.8) | 5 (1.6) | 2 (0.4) |
| Binge eating disorder | 25 (3.3) | 5 (2.4) | 13 (4.8) | 7 (2.5) | 10 (3.3) | 15 (3.3) |
| Major depressive episode | 382 (50.3) | 103 (49.3) | 149 (55.2) | 130 (46.3) | 159 (51.8) | 223 (49.2) |
| Dysthymia | 115 (15.1) | 44 (21.1) | 46 (17.0) | 25 (8.9) | 35 (11.4) | 80 (17.7) |
| Generalized anxiety disorder | 78 (10.3) | 22 (10.5) | 30 (11.1) | 26 (9.3) | 34 (11.1) | 44 (9.7) |
| Panic disorder | 112 (14.7) | 47 (22.5) | 38 (14.1) | 27 (9.6) | 42 (13.7) | 70 (15.5) |
| Agoraphobia | 95 (12.5) | 36 (17.2) | 36 (13.3) | 23 (8.2) | 33 (10.7) | 62 (13.7) |
| Specific phobia | 90 (11.8) | 19 (9.1) | 27 (10.0) | 44 (15.7) | 49 (16.0) | 41 (9.1) |
| Obsessive-compulsive disorder | 28 (3.7) | 6 (2.9) | 11 (4.1) | 11 (3.9) | 13 (4.2) | 15 (3.3) |
| Alcohol abuse disorder | 382 (50.3) | 143 (68.4) | 164 (60.7) | 75 (26.7) | 91 (29.6) | 291 (64.2) |
| Alcohol dependence disorder | 299 (39.3) | 114 (54.5) | 134 (49.6) | 51 (18.1) | 63 (20.5) | 236 (52.1) |
| Cocaine abuse disorder | 36 (4.7) | 13 (6.2) | 13 (4.8) | 10 (3.6) | 11 (3.6) | 25 (5.5) |
| Cocaine dependence disorder | 93 (12.2) | 49 (23.4) | 31 (11.5) | 13 (4.6) | 21 (6.8) | 72 (15.9) |
| Cannabis abuse disorder | 80 (10.5) | 30 (14.4) | 33 (12.2) | 17 (6.0) | 20 (6.5) | 60 (13.2) |
| Cannabis dependence disorder | 77 (10.1) | 44 (21.1) | 21 (7.8) | 12 (4.3) | 12 (3.9) | 65 (14.3) |
| Antisocial personality disorder | 44 (5.8) | 18 (8.6) | 18 (6.7) | 8 (2.8) | 10 (3.3) | 34 (7.5) |
Note: Dysthymia is current, not lifetime.
Confirmatory Factor Analysis Models
Correlations, means, standard deviations, and ranges are presented for the full sample and male and female subsamples in Tables 2 and 3. We first tested the four Forbush models, as described above. All models fit the data well (see Table 4). All factor loadings were significant in Models 1, 2, and 3. However, in Model 4, the cross-loadings of AN (β = .01, t = 0.18, p = .86) and BN (β = −.09, t = −1.55, p = .12) onto externalizing were nonsignificant; the cross-loading of BED onto externalizing was small and negative (β = −.14), t = −2.33, p = .02). The BIC for Model 2, which included a latent ED variable loading onto a higher order internalizing factor, was the lowest, indicating that this was the best-fitting model of the four. Thus, as in Forbush et al.5, ED symptoms loaded onto the latent internalizing factor.
Table 2.
Correlations, means, standard deviations, and ranges for lifetime severity variables for the total sample
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. MDE | -- | |||||||||||||
| 2. AN | .16** | -- | ||||||||||||
| 3. BN | .22** | .16** | -- | |||||||||||
| 4. BED | .18** | .10** | .80** | -- | ||||||||||
| 5. Dysthymia | .36** | .09* | .24** | .21** | -- | |||||||||
| 6. GAD | .40** | .12* | .26** | .28** | .40** | -- | ||||||||
| 7. Panic | .36** | .12** | .22** | .22** | .38** | .41** | -- | |||||||
| 8. Phobia | .13** | .07 | .14** | .15** | .11** | .18** | .27** | -- | ||||||
| 9. OCD | .21** | .09* | .11** | .12** | .26** | .23** | .23** | .19** | -- | |||||
| 10. Agor | .23** | .09* | .16** | .18** | .26** | .28** | .58** | .26** | .23** | -- | ||||
| 11. AAS | .24** | .03 | .07 | .03 | .23** | .21** | .19** | .07 | .06 | .13** | -- | |||
| 12. Cocaine | .16** | .04 | .10** | .03 | .17** | .09* | .16** | .01 | .07 | .09* | .41** | -- | ||
| 13. Alcohol | .21** | .02 | .06 | .04 | .21** | .14** | .23** | .01 | .09* | .12** | .50** | .33** | -- | |
| 14. Cannabis | .14** | .07 | .07 | .03 | .12** | .07 | .11** | −.02 | .04 | .04 | .37** | .42** | .36** | -- |
| Mean | 9.72 | .28 | 1.41 | 2.33 | 4.76 | 5.63 | 10.62 | 3.48 | 1.02 | .78 | 3.12 | 1.68 | 7.64 | 1.22 |
| SD | 5.84 | .99 | 2.23 | 4.04 | 4.59 | 5.20 | 9.99 | 3.92 | 2.68 | 1.53 | 3.56 | 3.97 | 7.78 | 2.56 |
| Range | 0–18 | 0–8 | 0–10 | 0–18 | 0–14 | 0–16 | 0–32 | 0–10 | 0–14 | 0–4 | 0–16 | 0–22 | 0–24 | 0–14 |
|
Possible Range |
0–18 | 0–8 | 0–10 | 0–18 | 0–14 | 0–16 | 0–32 | 0–8 | 0–14 | 0–4 | 0–40 | 0–24 | 0–24 | 0–24 |
Note: Dysthymia is current, not lifetime. Raw AN scores are presented in order to show the mean and range; however, z-scores were used in the models. MDE=major depressive episode, AN=anorexia nervosa, BN=bulimia nervosa, BED=binge eating disorder, GAD=generalized anxiety disorder, Panic=panic disorder, phobia=specific phobia, OCD=obsessive compulsive disorder, Agor=agoraphobia, AAS=adult antisociality, Cocaine=cocaine abuse/dependence, Alcohol=alcohol abuse/dependence, Cannab=cannabis abuse/dependence.
p < .05
p < .01
Table 3.
Correlations, means, standard deviations, and ranges for lifetime severity variables for the female and male subsamples
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. MDE | -- | .12* | .15** | .14** | .33** | .41** | .35** | .12* | .19** | .20** | .26** | .15** | .21** | .13** |
| 2. AN | .20** | -- | .14** | .08 | .07 | .07 | .00 | .02 | .16** | .02 | −.02 | −.02 | .01 | .03 |
| 3. BN | .30** | .16** | -- | .79** | .18** | .27** | .20** | .18** | .09 | .17** | .07 | .07 | .03 | .10* |
| 4. BED | .22** | .10 | .80** | -- | .18** | .28** | .19** | .19** | .14** | .24** | .03 | .01 | .03 | .06 |
| 5. Dysthymia | .41** | .16** | .35** | .28** | -- | .36** | .31** | .12* | .23** | .19** | .13** | .13** | .14** | .10* |
| 6. GAD | .38** | .18** | .26** | .28** | .47** | -- | .39** | .16** | .18** | .28** | .21** | .10 | .18** | .08 |
| 7. Panic | .38** | .23** | .26** | .26** | .48** | .45** | -- | .24** | .22** | .59** | .12* | .16** | .19** | .09 |
| 8. Phobia | .13* | .08 | .09 | .10 | .13* | .21** | .34** | -- | .17** | .27** | .11* | .02 | .04 | −.02 |
| 9. OCD | .25** | .07 | .14* | .11* | .32** | .30** | .25** | .21** | -- | .26** | .01 | .07 | .10* | .05 |
| 10. Agor | .27** | .20** | .18** | .13* | .38** | .28** | .59** | .27** | .19** | -- | .09 | .07 | .07 | .01 |
| 11. AAS | .26** | .18** | .16** | .10 | .36** | .24** | .31** | .08 | .15** | .18** | -- | .34** | .39** | .32** |
| 12. Cocaine | .20** | .18** | .21** | .10 | .22** | .09 | .16** | .03 | .08 | .09 | .51** | -- | .28** | .39** |
| 13. Alcohol | .27** | .20** | .23** | .17** | .28** | .11 | .29** | .06 | .09 | .13* | .56** | .37** | -- | .33** |
| 14. Cannabis | .17** | .22** | .08 | .03 | .13* | .05 | .13* | .04 | .04 | .06 | .40** | .45** | .31** | -- |
| Women | ||||||||||||||
| Mean | 9.85 | .52 | 1.71 | 2.73 | 4.20 | 5.68 | 9.98 | 3.91 | 1.02 | .62 | 1.99 | .97 | 4.01 | .65 |
| SD | 5.74 | 1.38 | 2.53 | 4.38 | 4.39 | 5.10 | 9.76 | 4.14 | 2.64 | 1.39 | 3.02 | 3.11 | 6.20 | 1.92 |
| Range | 0–18 | 0–8 | 0–10 | 0–18 | 0–14 | 0–16 | 0–31 | 0–10 | 0–14 | 0–4 | 0–14 | 0–14 | 0–24 | 0–14 |
|
Possible Range |
0–18 | 0–8 | 0–10 | 0–18 | 0–14 | 0–16 | 0–32 | 0–8 | 0–14 | 0–4 | 0–40 | 0–24 | 0–24 | 0–24 |
| Men | ||||||||||||||
| Mean | 9.63 | .12 | 1.20 | 2.05 | 5.13 | 5.59 | 11.07 | 3.18 | 1.03 | .89 | 3.90 | 2.17 | 10.14 | 1.60 |
| SD | 5.90 | .53 | 1.97 | 3.76 | 4.69 | 5.27 | 9.96 | 3.74 | 2.72 | 1.62 | 3.70 | 4.41 | 7.78 | 2.85 |
| Range | 0–18 | 0–5 | 0–10 | 0–18 | 0–14 | 0–16 | 0–32 | 0–10 | 0–14 | 0–4 | 0–16 | 0–22 | 0–24 | 0–12 |
|
Possible Range |
0–18 | 0–6 | 0–10 | 0–18 | 0–14 | 0–16 | 0–32 | 0–8 | 0–14 | 0–4 | 0–40 | 0–24 | 0–24 | 0–24 |
Note: Correlations for women are presented below the diagonal; correlations for men are presented above the diagonal. Dysthymia is current, not lifetime. Raw AN scores are presented in order to show the mean and range; however, z-scores were used in the models. MDE=major depressive episode, AN=anorexia nervosa, BN=bulimia nervosa, BED=binge eating disorder, GAD=generalized anxiety disorder, Panic=panic disorder, phobia=specific phobia, OCD=obsessive compulsive disorder, Agor=agoraphobia, AAS=adult antisociality, Cocaine=cocaine abuse/dependence, Alcohol=alcohol abuse/dependence, Cannab=cannabis abuse/dependence.
p < .05
p < .01
Table 4.
Fit statistics for confirmatory factor analysis models
| Model | χ2 | Df | CFI | TLI | RMSEA | RMSEA 90% CI |
SRMR | AIC | BIC |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 114.140 | 72 | .98 | .97 | .03 | .02, .04 | .04 | 52178.07 | 52395.33 |
| 2 | 117.633 | 73 | .98 | .97 | .03 | .02, .04 | .04 | 52180.43 | 52393.08 |
| 3 | 762.721 | 74 | .64 | .56 | .11 | .10, .12 | .09 | 52948.12 | 53156.15 |
| 4 | 107.187 | 70 | .98 | .98 | .03 | .02, .04 | .03 | 52174.51 | 52401.02 |
| 5 | 105.443 | 70 | .98 | .98 | .03 | .02, .04 | .03 | 52174.22 | 52400.74 |
| 6* | 108.503 | 73 | .98 | .98 | .03 | .01, .04 | .03 | 52171.36 | 52384.01 |
| Equal form | 184.647 | 146 | .98 | .98 | .03 | .01, .04 | .04 | 51836.49 | 52261.78 |
| Metric invariance 1 | 205.954 | 158 | .98 | .97 | .03 | .02, .04 | .05 | 51841.09 | 52210.91 |
| Metric invariance 2** | 206.371 | 159 | .98 | .97 | .03 | .02, .04 | .05 | 51839.14 | 52204.34 |
| Scalar invariance | 361.036 | 173 | .90 | .90 | .05 | .05, .06 | .08 | 51990.99 | 52291.47 |
Note: χ2 = chi square; df=degrees of freedom; Comparative Fit Index; Tucker Lewis Index (TLI); RMSEA=Root Mean Square Error of Approximation; CI=confidence interval; SRMR=standardized root mean square residual; AIC=Akaike's Information Criterion; BIC=Bayesian Information Criterion.
Model 6 was the best-fitting model according to the BIC.
A model with first and second-order factor loadings equated for men and women provided the best fit to the data.
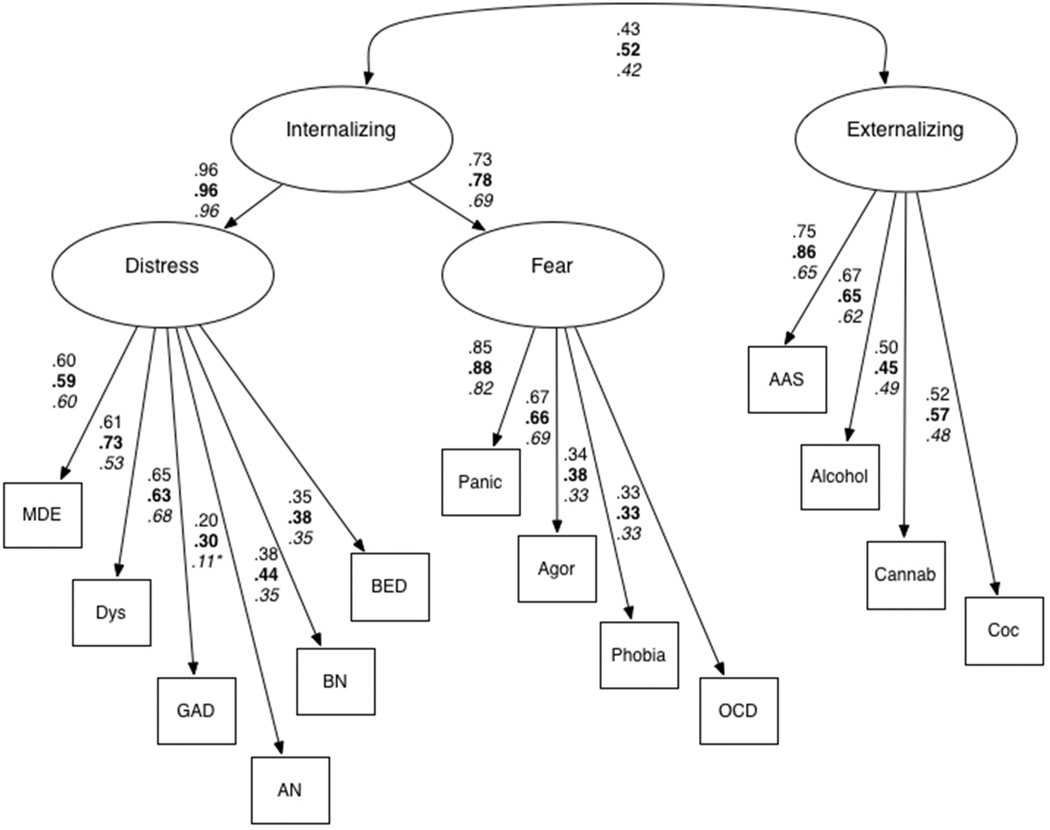
A second set of models investigated whether AN, BN, and BED severity loaded directly onto 5) both distress and fear, or 6) distress only. The externalizing factor was also included in these models for completeness. Model 5 fit the data well and had a slightly lower BIC value than did Model 2. Model 6, in which the ED severity indicators loaded directly onto latent distress, fit the data well; factor loadings representing relationships between distress and AN, BN, and BED symptoms were positive and significant. Model 6, which also had a lower BIC value than did Model 2 or 5, was therefore retained as the best-fitting model (see Figure 2).
Figure 2. Final model.
Note: coefficients are presented for the total sample, women (bold) and men (italicized). MDE=major depressive episode, Dys=dysthymia, GAD=generalized anxiety disorder, AN=anorexia nervosa, BN=bulimia nervosa, BED=binge eating disorder, Panic=panic disorder, Agor=agoraphobia, phobia=specific phobia, OCD=obsessive compulsive disorder, AAS=adult antisociality, Alcohol=alcohol abuse/dependence, Cannab=cannabis abuse/dependence, Coc=cocaine abuse/dependence. All measured variables are continuous, lifetime severity scores.
*all factor loadings except the one from distress to AN among men were significant at p < .05
Because many participants (all veterans in the sample) were selected based upon their trauma history, Model 6 was re-estimated covarying for the number of lifetime traumatic events on each indicator. Results were very similar to the model without trauma. Some factor loadings shifted slightly in magnitude, but all remained significant. Similarly, Model 6 was estimated in the veteran-only subsample, and results very closely followed the pattern of findings in the full sample (results available upon request).
Comparison of Models by Gender
Model 6 was estimated separately among men and women. As shown by the path coefficients in Figure 2, a similar pattern of results was observed in the male and female subsamples compared to the full sample. A multigroup analysis was performed in order to determine whether Model 6 was statistically equivalent for men and women. A model with all parameters freely estimated for both genders fit the data well, establishing equal form of the model. We compared this to a model with all first order factor loadings (i.e., those between factors and indicators) constrained to be equivalent across genders. As shown in Table 4, the BIC value for the constrained model was lower than the model with all parameters estimating freely. In addition, the chi-square difference test was non-significant (Δχ2 = 20.34, Δdf = 12, p = .06), indicating that the first order factor loadings were equivalent for men and women. Similarly, a model with the first and second order factor loadings, i.e., those from internalizing to distress and fear, constrained provided a better fit to the data, suggesting all factor loadings were equivalent (Δχ2 = .04, Δdf = 1, p = .83). With measurement invariance established, we then tested scalar invariance. Compared to the model with all factor loadings equal for men and women, constraining the item intercepts resulted in significantly worse model fit, as indicated by a higher BIC value and significant chi-square difference test (Δχ2 = 167.05, Δdf = 14, p < .001).* Thus, although the items (i.e., severity scores) had similar relations with the latent constructs in women and men, item intercepts were not equivalent. Because of this, no further measurement invariance analyses were conducted24.
Discussion
We hypothesized that AN, BN, and BED symptoms would load onto the internalizing latent factor, as found in previous studies,5,6. Our findings supported this hypothesis; in addition, we found that AN, BN, and BED severity variables loaded primarily onto the distress subfactor of the internalizing domain. Despite their strong association with distress-mediated disorders, particularly depression, it is important to note that rates of externalizing (e.g., substance use) and fear (e.g., phobias) disorders have been shown to be elevated among individuals with EDs2 as well. BN has been associated with high rates of substance use disorders2 as well as borderline personality disorder,25 which is considered to encompass both internalizing and externalizing facets of psychopathology.26 Nonetheless, our results and those of previous studies5,6 suggest that EDs may be most strongly associated with disorders characterized primarily by negative affect, worry, and rumination. Taken together, extant results underscore the importance of the role that depressive symptomatology, and affect regulation more generally28,29, may play in the development and maintenance of disordered eating.
Our findings aligned well with previous studies of internalizing/externalizing and EDs among women5 and a combined sample of men and women6. Of the four Forbush et al. models,5 we found that a model with the ED latent factor loading onto internalizing fit the data best. However, a model without a latent ED factor, and AN, BN, and BED symptoms loading onto the distress factor, provided a better fit. The best fitting model in this study was not evaluated by Forbush et al. The latent ED factor described by Forbush et al. may represent shared method variance, as some items assessing BN and BED overlap. In addition, the model with the latent ED factor is somewhat less useful in explaining the comorbidity across AN, BN, and BED and other disorders. Specifically, the current results suggest that the EDs align more strongly with the distress factor than with a more general internalizing factor that is indicated by both distress and fear disorders.
To our knowledge, this was the first study to statistically compare a factor analytic model of EDs along the internalizing/externalizing spectrum between men and women. Women have higher rates of EDs than do men, although men have higher rates than previously recognized2. In addition, important differences across gender have emerged, including different body ideals and presenting symptoms.7,30 However, in the current study, when model comparisons were stratified by gender, the final model, with all three ED variables loading onto distress only, provided the best fit to the data in both subsamples, suggesting that for both men and women, the EDs primarily reflect tendencies toward negative emotionality and distress. In addition, this model was statistically equivalent for men and women, although there were differences in mean levels of symptom severity across genders. Taken together, these findings suggest that EDs are influenced by the same underlying psychopathology variables in men and women, although the prevalence of these disorders may differ by gender.
Several important limitations should be noted. First, this was not a nationally representative sample and was selected based on trauma history or PTSD symptoms. We did not include PTSD symptoms in the models for this reason. It is possible that sample selection may have influenced our results, given that PTSD has been found to load on the distress factor.31 However, it has also shown structural associations across the internalizing and externalizing domains32. Controlling for lifetime trauma history had little impact on the model parameter estimates, and our results were consistent with a previous study of a nationally representative sample of women and men,6 together suggesting that our results may generalize to more diverse samples. Second, it is possible that our sample included a subset of individuals for whom their eating symptoms were more consistent with externalizing psychopathology but that this was not detected in the models. Third, we were unable to include borderline personality disorder, which has a high degree of comorbidity with EDs, in the models, as this was not assessed in both studies. Nonetheless, this study has several strengths, most notably the use of semi-structured clinician-administered interviews with demonstrated strong inter-rater reliability and the use of dimensional indicators of each disorder. In addition, veterans and men remain understudied in the field of EDs, despite findings that these disorders are more prevalent in underserved populations than previously recognized2,7. Potential future areas of research include replication of this model among larger and more demographically diverse samples of men and women.
Findings from the current study have potentially important implications for studies of EDs and comorbid psychopathology. In particular, there has been much recent interest on research domains that cut across multiple disorders, in order to further the study of neurobiological and genetic elements of psychopathology as well as treatment of these disorders33. Investigating latent dimensions of psychopathology is one approach to identifying common factors that partially account for patterns of comorbidity among psychiatric disorders. This approach may ultimately aid in translating research findings into clinical practice.
Acknowledgements
Financial Support
Funding for this study was provided by R01MH079806 and by a VA CSR&D Merit Award (application # 5I01CX000431-02) to Mark W. Miller. Karen S. Mitchell’s contribution was supported by K01MH093750. Erika J. Wolf’s contribution to this project was supported by a VA CSR&D Career Development Award.
Footnotes
In order to further assess whether our sample composition influenced our results, we tested the invariance of the model without EDs, so that it was similar to Eaton et al.3 We found that the factor loadings were equivalent for men and women.
Conflict of Interest
None
References
- 1.Blinder BJ, Cumella EJ, Sanathara VA. Psychiatric comorbidities of female inpatients with eating disorders. Psychol Med. 2006;68:454–462. doi: 10.1097/01.psy.0000221254.77675.f5. [DOI] [PubMed] [Google Scholar]
- 2.Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eaton NR, Keyes KM, Krueger RF, Balsis S, Skodol AE, Markon KE, et al. An invariant dimensional liability model of gender differences in mental disorder prevalence: Evidence from a national sample. J Abnorm Psychol. 2012;121:282–288. doi: 10.1037/a0024780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krueger RF, McGue M, Iacono WG. The higher-order structure of common DSM mental disorders: Internalization, externalization, and their connections to personality. Personal Individ Differ. 2001;30:1245–1259. [Google Scholar]
- 5.Forbush KT, South SC, Krueger RF, Iacono WG, Clark LA, Keel PK, et al. Locating eating pathology within an empirical diagnostic taxonomy: Evidence from a community-based sample. J Abnorm Psychol. 2010;119:282–292. doi: 10.1037/a0019189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forbush KT, Watson D. The structure of common and uncommon mental disorders. Psychol Med. 2013;43:97–108. doi: 10.1017/S0033291712001092. [DOI] [PubMed] [Google Scholar]
- 7.Mitchison D, Mond J, Slewa-Younan S, Hay P. Sex differences in health-related quality of life impairment associated with eating disorder features: A general population study. Int J Eat Disord. 2013;46:375–380. doi: 10.1002/eat.22097. [DOI] [PubMed] [Google Scholar]
- 8.Striegel-Moore RH, Rosselli F, Perrin N, DeBar L, Wilson GT, May A, et al. Gender difference in the prevalence of eating disorder symptoms. Int J Eat Disord. 2009;42:471–474. doi: 10.1002/eat.20625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen H-U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012;21:169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jacobson IG, Smith TC, Smith B, Keel PK, Amoroso PJ, Wells TS, et al. Disordered eating and weight changes after deployment: Longitudinal assessment of a large US military cohort. Am J Epidemiol. 2009;169:415–427. doi: 10.1093/aje/kwn366. [DOI] [PubMed] [Google Scholar]
- 12.Jordan BK, Schlenger WE, Hough R, Kulka RA, Weiss D, Fairbank JA, et al. Lifetime and current prevalence of specific psychiatric disorders among Vietnam veterans and controls. Arch Gen Psychiatry. 1991;48:207–215. doi: 10.1001/archpsyc.1991.01810270019002. [DOI] [PubMed] [Google Scholar]
- 13.Maguen S, Ren L, Bosch JO, Marmar CR, Seal KH. Gender differences in mental health diagnoses among Iraq and Afghanistan veterans enrolled in veterans affairs health care. Am J Public Health. 2010;100:2450–2456. doi: 10.2105/AJPH.2009.166165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adambegan M, Wagner G, Nader IW, Fernandez-Aranda F, Treasure J, Karwautz A. Internalizing and externalizing behaviour problems in childhood contribute to the development of anorexia and bulimia nervosa: A study comparing sister pairs. Eur Eat Disord Rev. 2012;20:116–120. doi: 10.1002/erv.1152. [DOI] [PubMed] [Google Scholar]
- 15.Logue MW, Baldwin C, Guffanti G, Melista E, Wolf EJ, Reardon AF, et al. A genomewide association study of post-traumatic stress disorder identifies the retinoid-related orphan receptor alpha (RORA) gene as a significant risk locus. Mol Psychiatry. 2013;18:937–942. doi: 10.1038/mp.2012.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weathers FW. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. 1993 [Google Scholar]
- 17.First M, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-IV (SCID) New York: Biometrics Research Department, New York State Psychiatric Institute; 1994. [Google Scholar]
- 18.Miller MW, Wolf EJ, Logue M, Baldwin C. The retinoid-related orphan receptor alpha (RORA) gene and anxiety disorder comorbidity. J Affect Disord. doi: 10.1016/j.jad.2013.07.022. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Loranger AW. International Personality Disorder Examination: DSM-IV and ICD-10 interviews. Lutz, FL: Psychological Assessment Resources, Inc; 1999. [Google Scholar]
- 20.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). Part I: Description. J Personal Disord. 1995;9:83–91. [Google Scholar]
- 21.SPSS Inc. Released 2009. SPSS for Windows, version 18.0. Chicago: SPSS Inc.; 2009. [Google Scholar]
- 22.Muthén LK, Muthén BO. Mplus User’s Guide. Seventh Edition. Los Angeles, CA: Muthén & Muthén; 1998. [Google Scholar]
- 23.Raftery AE. Bayesian model selection in social research. Socioloical Methodol. 1995;25:111–163. [Google Scholar]
- 24.Brown TA. Confirmatory factor analysis for applied research. New York: Guilford Press; 2006. [Google Scholar]
- 25.Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychol Bull. 2004;130:19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- 26.Mitchell KS, Mazzeo SE. Binge eating and psychological distress in ethnically diverse undergraduate men and women. Eat Behav. 2004;5:157–169. doi: 10.1016/j.eatbeh.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 27.Ouwens MA, van Strien T, van Leeuwe JFJ, van der Staak CPF. The dual pathway model of overeating: Replication and extension with actual food consumption. Appetite. 2009;52:234–237. doi: 10.1016/j.appet.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 28.Stice E. A prospective test of the dual-pathway model of bulimic pathology: Mediating effects of dieting and negative affect. J Abnorm Psychol. 2001;110:124–135. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- 29.Sansone RA, Levitt JL, Sansone LA. The prevalence of personality disorders among those with eating disorders. Eat Disord. 2005;13:7–21. doi: 10.1080/10640260590893593. [DOI] [PubMed] [Google Scholar]
- 30.Hudson JI, Zanarini MC, Mitchell KS, Choi-Kain L, Gunderson JG. The contribution of familial internalizing and externalizing liability factors to borderline personality disorder. Psychol Med. doi: 10.1017/S0033291713003140. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Corstorphine E, Mountford V, Tomlinson S, Waller G, Meyer C. Distress tolerance in the eating disorders. Eat Behav. 2007;8:91–97. doi: 10.1016/j.eatbeh.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 33.Svaldi J, Griepenstroh J, Tuschen-Caffier B, Ehring T. Emotion regulation deficits in eating disorders: A marker of eating pathology or general psychopathology? Psychiatry Res. 2012;197:103–111. doi: 10.1016/j.psychres.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 34.Strother E, Lemberg R, Stanford SC, Turberville D. Eating disorders in men: Underdiagnosed, undertreated, and misunderstood. Eat Disord. 2012;20:346–355. doi: 10.1080/10640266.2012.715512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller MW, Fogler JM, Wolf EJ, Kaloupek DG, Keane TM. The internalizing and externalizing structure of psychiatric comorbidity in combat veterans. J Trauma Stress. 2008;21:58–65. doi: 10.1002/jts.20303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wolf EJ, Miller MW, Krueger RF, Lyons MJ, Tsuang MT, Koenen KC. Posttraumatic stress disorder and the Genetic Structure of comorbidity. J Abnorm Psychol. 2010;119:320–330. doi: 10.1037/a0019035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]