Abstract
Objectives
For dual source cardiac CTs without heart rate control, the influence of body habitus on quality is uncertain. We evaluated study quality across a range of heart rates (HR) and body size.
Methods
160 subjects were randomly selected for four HR groups [<70, 70-79, 80-89, ≥90 beats per minute (bpm)] from 703 subjects who underwent cardiac CT without premedication. Coronary visualization quality was scored on a 3 point scale (1=non-diagnostic, 2=diagnostic, 3=excellent).
Results
99% of coronaries were diagnostic quality. Six vessels were non-diagnostic, mostly due to motion. Nondiagnostic or diagnostic scores (<3) were greatest in the HR ≥90 bpm group. All normal weight subjects had excellent quality but 6% of vessels in overweight and 17% in obese subjects had diagnostic scores <3. Mean effective dose was 11.4 mSv and correlated with body size.
Conclusions
Diagnostic quality cardiac CT exams can be obtained without premedication regardless of body size.
Keywords: Cardiac CT, heart rate, beta-blockers, body mass index, image quality
Introduction
Cardiac computed tomography (CT) is an established non-invasive method for rapid and accurate evaluation of the coronary arteries.1-3 In clinical practice, cardiac CT examinations can be used as a first-line diagnostic test for the exclusion of significant coronary artery disease in patients with chest pain and low to intermediate pre-test probability of disease.4-7
Traditionally, high quality cardiac CT examinations require a low heart rate to minimize motion blurring due to limited scanner temporal resolution. Premedication with beta-blockers to achieve a target heart rate of less than 65 beats per minute (bpm) is considered current standard of care.8 Premedication with beta-blockers may be unavailable, however, in 5-11% of patients due to contraindications, the most common of which is reactive airway disease.8 In addition, adequate heart rate reduction cannot be achieved despite attempted beta blockade in 25-30% of subjects.8 Finally, achieving beta-blockade is time consuming and delays the time to scan acquisition and subsequent patient disposition in the emergency room setting.
The introduction of dual-source CT scanner technology, which combines data simultaneously acquired from two X-ray tubes to double temporal resolution to 75 msec, has greatly reduced motion artifacts during cardiac exams.9,10 Several groups have recently shown that high quality, accurate examinations can be obtained using dual-source CT over a range of heart rates without beta-blockade.11-13 Several studies have focused on technical factors related to imaging at high heart rates, identifying the most optimal image reconstruction intervals in the cardiac cycle for diagnostic exams.14-17 Less is known, however, about the influence of patient-related factors on image quality at high heart rates.
Obesity can have a negative impact on image quality due to a number of factors including increased noise and reduced peak contrast opacification. These factors would suggest that imaging at high heart rates may be more challenging in obese patients. Indeed, previous studies on first generation dual-source CT scanners saw decreased image quality with elevated body mass index (BMI), although no reduction in diagnostic accuracy.18,19 Recently introduced second generation dual-source CT scanners have the advantage of improved temporal resolution and generator power over first generation scanners, potentially reduce both motion and noise artifacts in larger patients.20 Accordingly, the goal of our current examination was to evaluate the diagnostic quality of second-generation dual-source coronary CT examinations performed in a cohort of mostly overweight and obese subjects with no beta-blocker premedication.
Materials and Methods
Study population
Participants were selected from the larger ongoing Genetic Study of Atherosclerosis Risk (GeneSTAR), a prospective study of 4000 individuals designed to characterize genetic and biological factors associated with cardiovascular disease phenotypes in 883 families with early-onset coronary heart disease. Recruitment protocols for the GeneSTAR study have been previously described in detail.21 Consecutive subjects (n=703) who received coronary CT examinations between July 2009 and January 2012 constituted the study group. Retrospective review of these examinations was performed for each subject to identify the heart rate during the coronary CT angiography portion of the examination from DICOM headers. Subjects were separated into four heart rate groups: <70 bpm (n=447), 70-79 bpm (n=150), 80-89 bpm (n=64), and ≥90 bpm (n=42). 40 subjects were randomly selected from each group for analysis (total of 160 subjects). In all but the ≥90 bpm group, the study sample included 20 males and 20 females. Due to smaller number of female subjects in the >90 bpm group, 26 males and 14 females were selected. Participants underwent a comprehensive risk factor screening following a 12-hour overnight fast. Medical history and current medication use were elicited, and a physical exam was performed by a study cardiologist. Anthropometric measures included height determined using a fixed stadiometer and weight measured on a balance scale with the subject wearing light clothing and no shoes. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Current cigarette smoking behavior was assessed by self-report and verified by expired carbon monoxide (CO) levels of ≥8 ppm. Blood pressure was measured according to the American Heart Association guidelines three times over the course of the day and the average of the three measurements was used to characterize blood pressure; hypertension was defined as an average blood pressure ≥140 mmHg systolic, or ≥90 mmHg diastolic, and/or use of an antihypertensive drug. Blood was taken for measurement of lipid and glucose levels. Total cholesterol, high-density lipoprotein (HDL) cholesterol, and triglyceride levels were measured using the United States Centers for Disease Control standardized methods.22 Low-density lipoprotein (LDL) cholesterol was estimated using the Friedewald formula23 for persons with triglyceride levels up to 400 mg/dl. Glucose concentration was measured using the glucose oxidase method;24 type 2 diabetes was defined as a physician diagnosed history, a fasting glucose level ≥6.99 mmol/l (126 mg/dl), and/or use of prescribed hypoglycemic medications.
Coronary CT technique
Coronary CT examinations were performed on a second generation dual-source CT scanner (Definition FLASH, Siemens, Erlangen, Germany). Initially, a standard ECG-gated non-contrast calcium scoring sequence was performed. Agaston score was calculated from dedicated software and recorded on a per vessel and per subject basis. Coronary CT angiography was performed with retrospective ECG-gating. Automated dose modulation was used to reduce radiation dose, with the tube current reduced to 5% of maximal current during portions of the cardiac cycle outside of the diagnostic imaging window. In subjects with low (<70 bpm) steady heart rates, an imaging window centered on 70% of the RR interval with 10% padding was used. In subjects with elevated (>70 bpm) heart rate or variable heart rhythm, the imaging window was increased to 30-80% of the RR interval. Subjects with BMI ≥25 kg/m2 were imaged at 120 kV. Subjects with BMI <25 kg/m2 were imaged at 100 kV. 80 mL of iodinated contrast was injected at 4-7 mL/sec followed by a 20 mL saline flush. Automated tube current modulation (CareDose 4D, Siemens) was used with a reference mAs value set at 320 mAS. Dose length product (DLP) in mGy·cm for each study was recorded both for the CT angiographic phase only and for the total examination (inclusive of pre-monitoring images and calcium score). Estimated effective radiation dose was calculated using DLP multiplied by a standard thoracic conversion factor, k = 0.014 mSv × (mGy × cm)−1.25
Image evaluation
Coronary CT examinations were reviewed in consensus by two radiologists (SLZ, EKF) with 4 and >20 years of experience reading coronary CT, respectively. All imaging review was performed on a dedicated 3D workstation (Siemens MMWP, Siemens, Erlangen, Germany and HipGraphics, Baltimore, MD) running InSpace software. The highest quality imaging phase (best diastolic or best systolic phase, depending on heart rate) predetermined by scanner hardware was used for initial review. Image quality was evaluated on a per-vessel basis with coronary arteries scored for diagnostic quality on a three-point scale. Coronary artery segments <1.5 mm were not evaluated. Coronary arteries that were completely evaluated with no artifacts and a high diagnostic confidence were scored with a 3. Coronary arteries that had minor artifacts, such as increased noise or mild motion blurring, that did not prevent diagnostic evaluation were scored with a 2. Any coronary artery that contained portions of the vessel that were non-diagnostically evaluated was scored with a 1. For any examination receiving a score of 1 or 2, reasons for reduced quality were recorded. Multiphase datasets were available at the time of review. Additional reconstructed phases (every 5% of the RR interval) were reviewed for any vessels demonstrating less than excellent quality for all segments. Coronary artery quality was considered excellent if all segments were of excellent quality either if available on a single phase or through combined evaluation of more than one phase. Any studies that required multiphase evaluation were recorded.
Statistical analysis
Mean and standard deviations were calculated for continuous variables. Differences between groups were compared using either student's t-test for two groups or one-way analysis of variance (ANOVA) for more than two groups. Associations between continuous variables were tested with Pearson's correlation coefficient. A p-value less than 0.05 was considered significant.
Results
Demographics
The initial study population consisted of 160 subjects. Four subjects were excluded from analysis (3 had only calcium scoring exams performed, one had missing images). Of the excluded exams, one had subject HR 70-79, one with HR 80-89, and two with HR >90 bpm. The final cohort was 154 subjects. Mean age was 49.9 ± 10.7 years. 53.5% of subjects were female. The average BMI for the cohort was 31.4 ± 6.8 kg/m2. 5.7% of subjects were taking beta blocking medications at the time of examination. Population demographics and coronary artery disease (CAD) risk factors are shown in Table 1.
Table 1.
Subject demographic data and cardiac risk factors.
| Characteristic | Mean ± SD |
|---|---|
| Age, years | 49.9 ± 10.7 |
| Weight, kg | 89.1 ± 19.4 |
| Body Mass Index, kg/m2 | 31.4 ± 6.8 |
| Beta-blocker, % | 5.7 |
| Female sex, % | 53.5 |
| African American race, % | 35.1 |
| Hypertension, % | 50.3 |
| Diabetic, % | 11.5 |
| Current smoker, % | 15.3 |
| LDL cholesterol, mg/dL | 115.2 ± 36.0 |
| HDL cholesterol, mg/dL | 54.1 ± 15.9 |
| Triglycerides, mg/dL | 122.6 ± 67.8 |
| Any coronary plaque, % | 45.9 |
Overall image quality
On a per subject basis, diagnostic image quality for all three coronary arteries was achieved in 97% of examinations (151/156 exams). The most common non-diagnostic vessel was the RCA (n=4), followed by the LAD and circumflex coronary arteries (n=1 for each, both in the same subject). For non-diagnostic RCA cases, limited quality was attributed to cardiac motion in three cases and respiratory motion in the fourth case. For the subject with non-diagnostic visualization of the circumflex and LAD, both cardiac motion and noise contributed to non-diagnostic quality. There was no study for which left main coronary artery visualization was considered non-diagnostic. On a per-vessel basis, 88.9% (555/624) of coronary arteries were considered of excellent quality, 10.1% (63/624) of diagnostic quality, and 1.0% (6/624) of non-diagnostic quality. The most common reasons for diagnostic (grade 2) quality were image noise in 57.1% (36/63), cardiac motion in 17.4% (11/63), respiratory motion in 3.2% (2/63), and inadequate contrast in one subject (1.6%, 1/63). No specific reason for grade 2 image quality was provided for 13 subjects. There were no significant differences in calcium score between studies grouped according to image quality. Representative examples of image quality scores at various heart rates are provided in Figures 1-3.
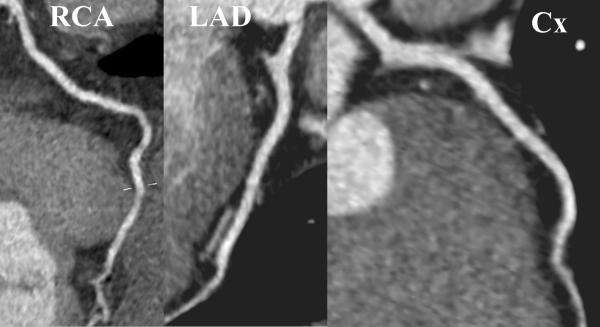
Figure 1.
Example of excellent image quality (score 3) for a 30 year old woman with body mass index of 46.9 kg/m2 and heart rate of 98 beats per minute. (RCA = right coronary artery, LAD = left anterior descending coronary artery, Cx = circumflex coronary artery).
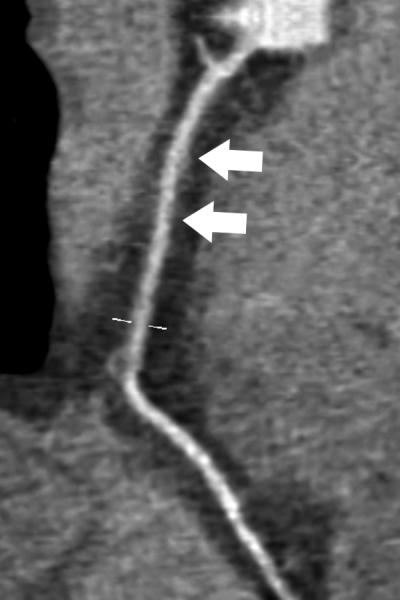
Figure 3.
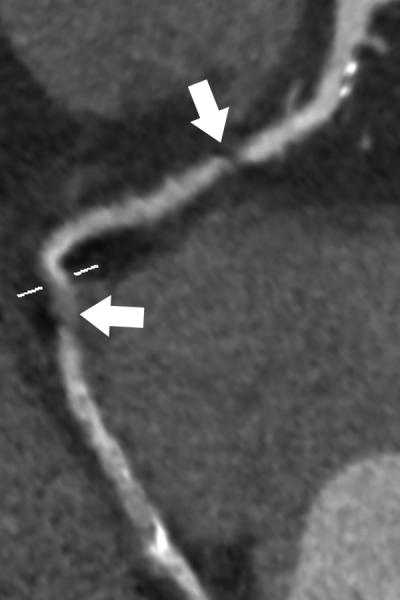
Example of non-diagnostic image quality (score 1) for the right coronary artery (RCA) in a 70 year old male with body mass index of 34.7 kg/m2 and heart rate of 108 beats per minute. There is focal non-visualization of two areas of the RCA (arrows) that did not resolve on multiphase images.
Image quality versus heart rate
The majority of non-diagnostic quality coronary arteries occurred in subjects with heart rate ≥90 bpm (80%, 4/5). A single study in the low heart rate group (<70 bpm) was scored non-diagnostic in quality due to cardiac motion artifacts, likely secondary to arrhythmia. Distribution of scan quality according to the coronary vessel and heart rate category is detailed in Table 2. Overall, on a per-vessel basis, the number of coronary arteries scored as excellent quality was similar between the first three heart rate categories (88.1% for HR <70 bpm, 91.7% for HR 70-79 bpm, 92.3% for HR 80-89). There was a significant decrease in the number of excellent quality coronary arteries in the highest heart rate category (HR ≥90 bpm, 73.7%, p=0.001). This trend was similar for all specific epicardial coronary arteries (p<0.05 for all). The RCA had the lowest rate of excellent quality scores in the highest heart rate category at 68.4%, compared to 79.0% for the left main, 73.7% for the LAD, and 73.7% for the circumflex coronary artery. There was a significant increase in the use of multiple phases with increasing heart rate categories (p=0.01 for trend). In the lowest heart rate category (<70 bpm), multiphase was used in 15.0% of exams, compared to 25.5% for heart rates 70-79 bpm, 28.2% for heart rates 80-89 bpm, and 47.9% for heart rates ≥ 90 bpm.
Table 2.
Distribution of scan quality rating by coronary vessel and heart rate category. (RCA = right coronary artery, LM = left main coronary artery, LAD = left anterior descending coronary artery, CX = circumflex coronary artery)
| Scan Heart Rate (beats per minute) | |||||
|---|---|---|---|---|---|
| Vessel | Scan Quality | <70 N=40 | 70 to 79 N=39 | 80 to 89 N=39 | ≥90 N=38 |
| RCA | Non-diagnostic N=4 |
n=1 2.5% |
n=0 0% |
n=0 0% |
n=3 7.9% |
| Diagnostic N=20 |
n=3 7.5% |
n=4 10.3% |
n=4 10.3% |
n=9 23.7% |
|
| Excellent N=132 |
n=36 90.0% |
n=35 89.7% |
n=35 89.7% |
n=26 68.4% |
|
| LM | Non-diagnostic N=0 |
n=0 0% |
n=0 0% |
n=0 0% |
n=0 0% |
| Diagnostic N=12 |
n=1 2.5% |
n=1 2.6% |
n=2 5.1% |
n=8 21.1% |
|
| Excellent N=144 |
n=39 97.5% |
n=38 97.4% |
n=37 94.9% |
n=30 79.0% |
|
| LAD | Non-diagnostic N=1 |
n=0 0% |
n=0 0% |
n=0 0% |
n=1 2.6% |
| Diagnostic N=17 |
n=1 2.5% |
n=4 10.3% |
n=3 7.7% |
n=9 23.7% |
|
| Excellent N=138 |
n=39 97.5% |
n=35 89.7% |
n=36 92.3% |
n=28 73.7% |
|
| CX | Non-diagnostic N=1 |
n=0 0% |
n=0 0% |
n=0 0% |
n=1 2.6% |
| Diagnostic N=17 |
n=1 2.5% |
n=4 10.3% |
n=3 7.7% |
n=9 23.7% |
|
| Excellent N=138 |
n=39 97.5% |
n=35 89.7% |
n=36 92.3% |
n=28 73.7% |
|
| Total | Non-diagnostic N=6 |
n=1 0.1% |
n=0 0% |
n=0 0% |
n=5 3.3% |
| Diagnostic N=66 |
n=6 3.8% |
n=13 8.3% |
n=12 7.7% |
n=35 23.0% |
|
| Excellent N=552 |
n=153 88.1% |
n=143 91.7% |
n=144 92.3% |
n=112 73.7% |
|
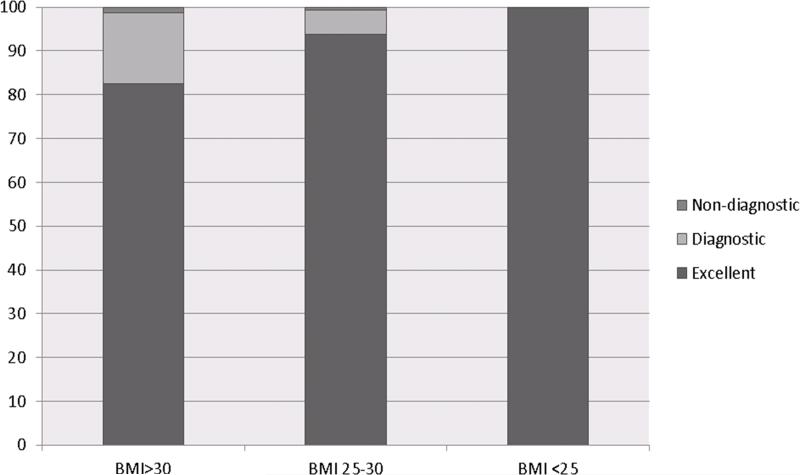
Image quality versus body size
There was a trend to higher mean BMI for the five subjects with non-diagnostic image quality (35.7 ± 9.1 kg/m2) compared to the remaining subjects with either diagnostic or excellent quality (31.2 ± 6.6 kg/m2), although this did not reach statistical significance (p=0.14). However, there was a significant difference in mean BMI when comparing image quality categories on a per-vessel basis, with diagnostic quality vessels (score 2) showing significantly higher BMI compared to the excellent quality group (Table 3). Per-vessel image quality scores stratified by BMI grouped into normal, overweight, and obese categories are detailed in Table 4. Overall study quality for each BMI group is shown in Figure 4. Among normal weight subjects, 100% of coronary arteries were scored as excellent quality. The rate of diagnostic quality vessels (score 2) increased for overweight (16.1%) and obese (5.4%) subjects. There was a significant positive correlation of BMI with heart rate (r=0.19, p=0.02).
Table 3.
Body mass index (BMI, kg/m2) by per-vessel image quality. Data expressed as mean BMI ± standard deviation (kg/m2). (RCA = right coronary artery, LM = left main coronary artery, LAD = left anterior descending coronary artery, CX = circumflex coronary artery)
| Vessel | Non-diagnostic | Diagnostic | Excellent | ANOVA p-value |
|---|---|---|---|---|
| RCA | 31.8 ± 3.4 | 37.6 ± 7.9 | 30.3 ± 6.1 | <0.0001 |
| LM | N/A | 38.7 ± 8.5 | 30.7 ± 6.2 | <0.0001 |
| LAD | 51.0 (n=1) | 37.5 ± 6.8 | 30.4 ± 6.1 | <0.0001 |
| CX | 51.0 (n=1) | 38.4 ± 6.9 | 30.5 ± 6.1 | <0.0001 |
Table 4.
Per-vessel coronary artery quality stratified by body mass index (BMI). Data expressed as number of exams (percentage). (RCA = right coronary artery, LM = left main coronary artery, LAD = left anterior descending coronary artery, CX = circumflex coronary artery)
| Coronary Artery Quality versus BMI (kg/m2) | |||
|---|---|---|---|
| Excellent (%) | Diagnostic (%) | Non-diagnostic (%) | |
| Obese (BMI>30 kg/m2), n=76 | |||
| RCA | 59 (78) | 15 (20) | 2 (3) |
| LM | 67 (88) | 9 (12) | 0 (0) |
| LAD | 61 (80) | 14 (18) | 1 (1) |
| CX | 64 (84) | 11 (15) | 1 (1) |
| Total | 251 (83) | 49 (16) | 4 (1) |
| Overweight (BMI 25-30 kg/m2), n=65 | |||
| RCA | 58 (89) | 5 (8) | 2 (3) |
| LM | 62 (95) | 3 (5) | 0 |
| LAD | 62 (95) | 3 (5) | 0 |
| CX | 62 (95) | 3 (5) | 0 |
| Total | 244 (94) | 14 (5) | 2 (1) |
| Normal weight (BMI <25 kg/m2), n =15 | |||
| RCA | 15 (100) | 0 | 0 |
| LM | 15 (100) | 0 | 0 |
| LAD | 15 (100) | 0 | 0 |
| CX | 15 (100) | 0 | 0 |
| Total | 60 (100) | 0 | 0 |
Figure 4.
Percent of studies in each image quality category stratified by body mass index (kg/m2). Overall exam quality was considered non-diagnostic or diagnostic if any vessel received quality score of 1 and diagnostic if any vessel received a quality score of 2.
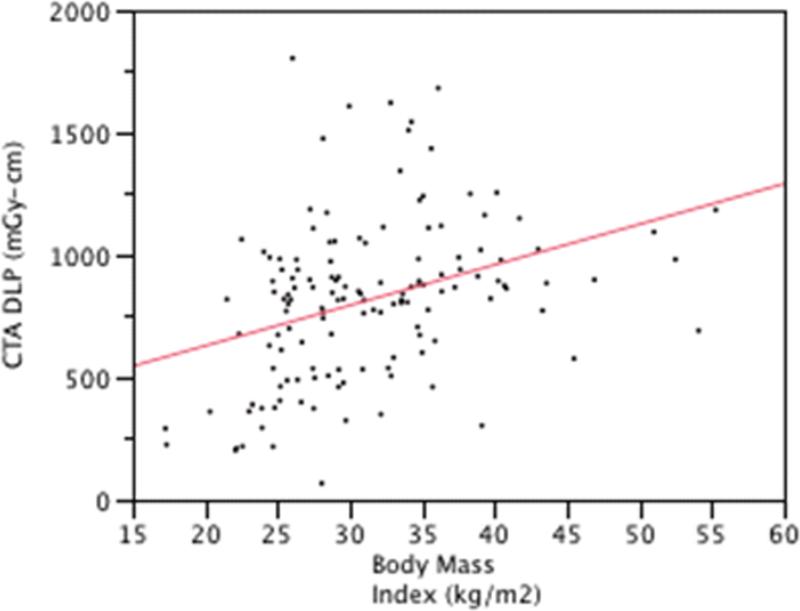
Radiation dose
Dose information was not available in 17 subjects. Mean total examination DLP was 977.5 ± 613.8 mGy•cm. Mean DLP for the only the CT angiographic portion of the examination, exclusive of monitoring scans and calcium scoring sequence, was 818.3 ± 325.2 mGy•cm. Mean total examination estimated effective dose was 13.7 ± 8.6 mSv. Mean effective dose for the CT angiographic portion of the exam was 11.5 ± 4.6 mSv. There was a significant positive correlation between both total examination and CT angiographic DLPs to BMI (r=0.35 and 0.46, respectively, both p<0.0001), Figure 5. Total examination and CT angiographic DLP were not significantly correlated to heart rate (r=0.14, p=0.09 and r=0.07, p=0.44, respectively)
Figure 5.
Association of CT angiographic DLP (dose-length product) with body mass index (R = 0.35, p<0.0001).
Discussion
The primary finding of this study is that high quality dual-source cardiac CT exams were reliably obtained in a population of mostly obese and overweight subjects without heart rate control. The majority of exams in the current study were of excellent quality, even in larger subjects. These results have important clinical implications for centers with access to dual-source technology. In this setting, cardiac CT exams can be confidently performed in subjects with elevated heart rates and contraindications to beta-blockade, regardless of body size, with potential to increase patient throughput.
In our study, we found that image quality varied with heart rate. Vessel visualization was considered excellent in 90% or greater of coronary arteries performed in the lowest and middle heart rate groups (<70 bpm, 70-79 bpm, and 80-89 bpm). However, subjects in the highest heart rate group (>90 bpm) had lower rates of excellent quality vessel visualization, ranging from 68-79%, depending upon the vessel. The RCA had the lowest rate of excellent quality visualization in this group, while the left main was the highest. Importantly, however, the rate of diagnostic quality vessel visualization was high in all heart rate groups. Only 6 coronary arteries in 5 subjects were considered of non-diagnostic quality, equating to a diagnostic study rate of 97% on a per-subject basis and 99% on per-vessel basis. Prior studies have demonstrated some variability in the frequency of diagnostic quality exams at high heart rates. Studies on first generation dual source technology without heart rate control have reported a rate of non-diagnostic coronary visualization ranging from 1-10%.12-14,26-28 Differences in diagnostic scan rate among these studies are likely at least in part due to inter-center variation in qualitative thresholds for defining diagnostic quality scans and population differences. More recent reports have evaluated second generation dual-source technology that was used in the current study, which has the advantage of higher temporal resolution (75 msec) compared to first generation technology (83 msec), resulting in decreased motion artifact for any given heart rate. These studies report consistently high rates of diagnostic coronary visualization (≥ 98%)29-31, very similar to our results.
In contrast to prior studies, however, the subject population of the current study was comprised of mostly overweight and obese individuals (mean BMI 31.4 ± 6.8 kg/m2, range 17-55). The majority of previous studies reported average subject BMI <30 kg/m2,12,13,26,27,31,32 whereas other studies did not provide BMI information.11,17,28,29 It is well known that image quality is negatively affected by subject size. Increased subcutaneous soft tissue in larger subjects will result in greater photon attenuation, increasing image noise. Larger subjects will have decreased peak vascular contrast enhancement, due to larger blood distribution volume. We also found that in our cohort resting heart rates increased linearly with BMI, reinforcing the need for high temporal resolution scanning in larger subjects. The current cohort was comprised of subjects more reflective of the North American population that has been gradually increasing in size year by year, with 34% of U.S. adults meeting the threshold for obesity in a 2011 survey.33
Overall, we found that the majority of subjects had excellent quality coronary artery visualization in all subject size groups, ranging from 100% in normal weight, 94% in overweight, to 83% in obese subjects. The number of coronary arteries scored as only of diagnostic quality, ie: with some artifact but still adequate for diagnosis, increased with subject size, to a maximum of 16% of exams in the obese group. The most common causes for reduced exam quality were image noise and cardiac motion. However, importantly, the number of non-diagnostic coronary arteries was very small in all groups, only 1% each in the obese and overweight groups and zero in the normal weight group. Therefore, although there is a greater chance of some compromise in image quality at higher BMI, our data indicate that at least diagnostic quality examinations can be expected in 99% of subjects regardless of size.
The association between BMI and cardiac CT image quality has been investigated by previous authors using first generation dual-source scanners. In the study by Alkadhi et al.,18 larger subjects showed decreased in rate of diagnostic coronary segments (2.4% vs. 1.4% for subjects above and below 26.0 kg/m2, respectively),18 but no decrease in diagnostic accuracy. Unlike the current study, however, this study had relatively few obese and severely obese subjects, and no subjects with BMI >40 kg/m2. The study by Brodoefel et al. showed decreased image quality in obese subjects and similarly saw no reduction in diagnostic accuracy.19 However, the majority (74%) of these subjects were on beta-blockers at the time of the examination. Other studies have evaluated the use of adjustable temporal resolution protocols with first-generation scanners that trade-off improved image noise for reduced temporal resolution. 30,31 These have the disadvantage of increased artifacts due to cardiac motion, which necessitates beta blocker administration. Our results would suggest that adjustable temporal resolution protocols are unnecessary using second generation dual-source technology.
Radiation dose is an important limitation of cardiac CT examinations. The mean estimated effective dose for the CT angiographic portion of the current study was 11.4 mSv, which is similar to the 12 mSv mean effective dose reported for the multicenter PROTECTION I trial (Prospective Multicenter Study On Radiation Dose Estimates Of Cardiac CT Angiography In Daily Practice), a cross-sectional multicenter study evaluating coronary CT dose in 1965 subjects from 50 sites.25 Total examination estimated effective dose in the current study, inclusive of calcium scoring and monitoring scans, was 13.7 mSv. As expected, radiation dose was positively correlated with BMI. Given the large average body size of our cohort, we were unable to use 100 kV tube potential in the majority of our exams, which was limited to subjects with BMI <25 kg/m2. In normal weight subjects, this could be expected to further reduce dose by approximately 31%.34 All exams in the current study were performed with retrospective gating and dose modulation to limit radiation exposure outside the diagnostic imaging window. The use of prospective gating would have further reduced radiation dose in our population, however, this was not used given concerns over reduced image quality from heart rate variability and cardiac motion at elevated heart rates. Several recent studies on dual-source scanners have confirmed, however, that prospectively gated studies are feasible with dual source CT in the absence of heart rate control.29,35,36 It is important to note that protocols should be adjusted to a wider acquisition window for optimal quality in these subjects. The prior work by Srichai et al. showed that prospectively gated studies at heart rates >80 bpm require a wide reconstruction window in late systole (30-50% of the RR interval) for diagnostic coronary visualization.14 Similarly, we found that the use of multiple reconstructed phases became more critical with high heart rates. Among the ≥90 bpm group, multiple phases were necessary for diagnostic quality evaluation of all coronaries in 48% of studies, as compared to only 15% in the lowest heart rate group (≤70 bpm). These findings lend further support to the use of beta-blockade in subjects without contraindications to permit a narrower acquisition window and reduced radiation dose.
There are several limitations in this study. First, we could not evaluate accuracy of coronary CT in this population as the majority of subjects did not undergo subsequent coronary artery catheterization. Second, our study was performed with retrospective ECG-gating. In many centers, prospective gating is the protocol of choice due to reduced radiation exposure. We suspect the current results would translate well to prospectively gated exams, however, further work is necessary for confirmation. We did not perform noise measurements for quantitative analysis of image quality, choosing rather to focus on assessment of diagnostic quality by expert reviewers, which we believe has greater clinical relevance. Finally, we did not evaluate the use of iterative reconstruction, which has been recently shown to increase image quality in obese subjects on a single-source scanner.37 We suspect that the use of iterative reconstruction would not significantly change the number of non-diagnostic coronary arteries, given that these were quite rare in the current study. However, it is likely that the use of iterative reconstruction may have upgraded the quality of some diagnostic (score 2) exams which were limited by noise.
In conclusion, we have found that the high quality dual-source CTA examinations can be obtained in subjects with normal or elevated heart rates across a wide range of body sizes. These findings indicate that coronary CT exams can be confidently performed in subjects without premedication.
Figure 2.
Example of diagnostic image quality (score 2) for the right coronary artery (RCA) in a 39 year old woman with body mass index of 38.2 kg/m2 and heart rate of 109 beats per minute. There is increased noise, particularly in the mid-RCA (arrows) which results in some blurring of the vessel wall but does not prevent diagnostic evaluation.
Acknowledgments
Funding sources: This work was supported by grants from the National Heart, Lung, and Blood Institute (Grants RC1HL099747 and K23HL094747).
Footnotes
Author conflicts of interest: SLZ: none; BGK: none ; EKF: none
References
- 1.Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52:1724–32. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 2.Salavati A, Radmanesh F, Heidari K, et al. Dual-source computed tomography angiography for diagnosis and assessment of coronary artery disease: systematic review and meta-analysis. J Cardiovasc Comput Tomogr. 2012;6:78–90. doi: 10.1016/j.jcct.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 3.Miller JM, Rochitte CE, Dewey M, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008;359:2324–36. doi: 10.1056/NEJMoa0806576. [DOI] [PubMed] [Google Scholar]
- 4.Mark DB, Berman DS, Budoff MJ, et al. ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Catheter Cardiovasc Interv. 2010;76:E1–42. doi: 10.1002/ccd.22495. [DOI] [PubMed] [Google Scholar]
- 5.Litt HI, Gatsonis C, Snyder B, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med. 2012;366:1393–403. doi: 10.1056/NEJMoa1201163. [DOI] [PubMed] [Google Scholar]
- 6.Hoffmann U, Truong QA, Schoenfeld DA, et al. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012;367:299–308. doi: 10.1056/NEJMoa1201161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor AJ, Cerqueira M, Hodgson JM, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate Use Criteria for Cardiac Computed Tomography A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2010;56:1864–1894. doi: 10.1016/j.jacc.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 8.Mahabadi AA, Achenbach S, Burgstahler C, et al. Safety, efficacy, and indications of beta-adrenergic receptor blockade to reduce heart rate prior to coronary CT angiography. Radiology. 2010;257:614–23. doi: 10.1148/radiol.10100140. [DOI] [PubMed] [Google Scholar]
- 9.Baumuller S, Leschka S, Desbiolles L, et al. Dual-source versus 64-section CT coronary angiography at lower heart rates: comparison of accuracy and radiation dose. Radiology. 2009;253:56–64. doi: 10.1148/radiol.2531090065. [DOI] [PubMed] [Google Scholar]
- 10.Achenbach S, Ropers U, Kuettner A, et al. Randomized comparison of 64-slice single-and dual-source computed tomography coronary angiography for the detection of coronary artery disease. JACC Cardiovasc Imaging. 2008;1:177–86. doi: 10.1016/j.jcmg.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Brodoefel H, Burgstahler C, Tsiflikas I, et al. Dual-source CT: effect of heart rate, heart rate variability, and calcification on image quality and diagnostic accuracy. Radiology. 2008;247:346–55. doi: 10.1148/radiol.2472070906. [DOI] [PubMed] [Google Scholar]
- 12.Ropers U, Ropers D, Pflederer T, et al. Influence of heart rate on the diagnostic accuracy of dual-source computed tomography coronary angiography. J Am Coll Cardiol. 2007;50:2393–8. doi: 10.1016/j.jacc.2007.09.017. [DOI] [PubMed] [Google Scholar]
- 13.Scheffel H, Alkadhi H, Plass A, et al. Accuracy of dual-source CT coronary angiography: First experience in a high pre-test probability population without heart rate control. Eur Radiol. 2006;16:2739–47. doi: 10.1007/s00330-006-0474-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Srichai MB, Hecht EM, Kim D, et al. Dual-source computed tomography angiography image quality in patients with fast heart rates. J Cardiovasc Comput Tomogr. 2009;3:300–9. doi: 10.1016/j.jcct.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 15.Araoz PA, Kirsch J, Primak AN, et al. Optimal image reconstruction phase at low and high heart rates in dual-source CT coronary angiography. Int J Cardiovasc Imaging. 2009;25:837–45. doi: 10.1007/s10554-009-9489-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weustink AC, Mollet NR, Pugliese F, et al. Optimal electrocardiographic pulsing windows and heart rate: effect on image quality and radiation exposure at dual-source coronary CT angiography. Radiology. 2008;248:792–8. doi: 10.1148/radiol.2483072098. [DOI] [PubMed] [Google Scholar]
- 17.Seifarth H, Wienbeck S, Pusken M, et al. Optimal systolic and diastolic reconstruction windows for coronary CT angiography using dual-source CT. AJR Am J Roentgenol. 2007;189:1317–23. doi: 10.2214/AJR.07.2711. [DOI] [PubMed] [Google Scholar]
- 18.Alkadhi H, Scheffel H, Desbiolles L, et al. Dual-source computed tomography coronary angiography: influence of obesity, calcium load, and heart rate on diagnostic accuracy. Eur Heart J. 2008;29:766–76. doi: 10.1093/eurheartj/ehn044. [DOI] [PubMed] [Google Scholar]
- 19.Brodoefel H, Tsiflikas I, Burgstahler C, et al. Cardiac dual-source computed tomography: effect of body mass index on image quality and diagnostic accuracy. Invest Radiol. 2008;43:712–8. doi: 10.1097/RLI.0b013e318180bae1. [DOI] [PubMed] [Google Scholar]
- 20.Chen MY, Shanbhag SM, Arai AE. Submillisievert median radiation dose for coronary angiography with a second-generation 320-detector row CT scanner in 107 consecutive patients. Radiology. 2013;267:76–85. doi: 10.1148/radiol.13122621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kral BG, Nyquist P, Vaidya D, et al. Relation of subclinical coronary artery atherosclerosis to cerebral white matter disease in healthy subjects from families with early-onset coronary artery disease. Am J Cardiol. 2013;112:747–52. doi: 10.1016/j.amjcard.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myers GL, Kimberly MM, Waymack PP, et al. A reference method laboratory network for cholesterol: a model for standardization and improvement of clinical laboratory measurements. Clin Chem. 2000;46:1762–72. [PubMed] [Google Scholar]
- 23.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 24.Pesce AJ, Kaplan LA. Methods in clinical chemistry. St. Louis: Mosby. 1987 [Google Scholar]
- 25.Hausleiter J, Meyer T, Hermann F, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301:500–7. doi: 10.1001/jama.2009.54. [DOI] [PubMed] [Google Scholar]
- 26.Leschka S, Scheffel H, Desbiolles L, et al. Image quality and reconstruction intervals of dual-source CT coronary angiography: recommendations for ECG-pulsing windowing. Invest Radiol. 2007;42:543–9. doi: 10.1097/RLI.0b013e31803b93cf. [DOI] [PubMed] [Google Scholar]
- 27.Matt D, Scheffel H, Leschka S, et al. Dual-source CT coronary angiography: image quality, mean heart rate, and heart rate variability. AJR Am J Roentgenol. 2007;189:567–73. doi: 10.2214/AJR.07.2078. [DOI] [PubMed] [Google Scholar]
- 28.Adler G, Meille L, Rohnean A, et al. Robustness of end-systolic reconstructions in coronary dual-source CT angiography for high heart rate patients. Eur Radiol. 2010;20:1118–23. doi: 10.1007/s00330-009-1642-9. [DOI] [PubMed] [Google Scholar]
- 29.Paul JF, Amato A, Rohnean A. Low-dose coronary-CT angiography using step and shoot at any heart rate: comparison of image quality at systole for high heart rate and diastole for low heart rate with a 128-slice dual-source machine. Int J Cardiovasc Imaging. 2013;29:651–7. doi: 10.1007/s10554-012-0110-9. [DOI] [PubMed] [Google Scholar]
- 30.Srichai MB, Barreto M, Lim RP, et al. Prospective-triggered sequential dual-source endsystolic coronary CT angiography for patients with atrial fibrillation: a feasibility study. J Cardiovasc Comput Tomogr. 2013;7:102–9. doi: 10.1016/j.jcct.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 31.Feuchtner G, Goetti R, Plass A, et al. Dual-step prospective ECG-triggered 128-slice dual-source CT for evaluation of coronary arteries and cardiac function without heart rate control: a technical note. Eur Radiol. 2010;20:2092–9. doi: 10.1007/s00330-010-1794-7. [DOI] [PubMed] [Google Scholar]
- 32.Weustink AC, Neefjes LA, Kyrzopoulos S, et al. Impact of heart rate frequency and variability on radiation exposure, image quality, and diagnostic performance in dual-source spiral CT coronary angiography. Radiology. 2009;253:672–80. doi: 10.1148/radiol.2533090358. [DOI] [PubMed] [Google Scholar]
- 33.McGuire S, Shields M, Carroll MD, Ogden CL. Adv Nutr. Vol. 2. National Center for Health Statistics; Hyattsville, MD: 2011. 2011. adult obesity prevalence in Canada and the United States. pp. 368–9. NCHS data brief no. 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hausleiter J, Martinoff S, Hadamitzky M, et al. Image quality and radiation exposure with a low tube voltage protocol for coronary CT angiography results of the PROTECTION II Trial. JACC Cardiovasc Imaging. 2010;3:1113–23. doi: 10.1016/j.jcmg.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 35.Xu L, Yang L, Zhang Z, et al. Low-dose adaptive sequential scan for dual-source CT coronary angiography in patients with high heart rate: comparison with retrospective ECG gating. Eur J Radiol. 2010;76:183–7. doi: 10.1016/j.ejrad.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 36.Goetti R, Feuchtner G, Stolzmann P, et al. High-pitch dual-source CT coronary angiography: systolic data acquisition at high heart rates. Eur Radiol. 2010;20:2565–71. doi: 10.1007/s00330-010-1838-z. [DOI] [PubMed] [Google Scholar]
- 37.Gebhard C, Fuchs TA, Fiechter M, et al. Image quality of low-dose CCTA in obese patients: impact of high-definition computed tomography and adaptive statistical iterative reconstruction. Int J Cardiovasc Imaging. 2013;29:1565–74. doi: 10.1007/s10554-013-0228-4. [DOI] [PubMed] [Google Scholar]