Abstract
We have learned over the last several decades that the brain is an important target for insulin action. Insulin in the central nervous system (CNS) affects feeding behavior and body energy stores, the metabolism of glucose and fats in the liver and adipose, and various aspects of memory and cognition. Insulin may even influence the development or progression of Alzheimer disease. Yet, a number of seemingly simple questions (e.g., What is the pathway for delivery of insulin to the brain? Is insulin’s delivery to the brain mediated by the insulin receptor and is it a regulated process? Is brain insulin delivery affected by insulin resistance?) are unanswered. Here we briefly review accumulated findings affirming the importance of insulin as a CNS regulatory peptide, examine the current understanding of how peripheral insulin is delivered to the brain, and identify key gaps in the current understanding of this process.
Introduction
Accumulating information suggests several significant roles for insulin action in the brain. Here, we briefly review selected studies that provoke exploration of this emerging field. More pointedly, we highlight seemingly serious deficiencies in our understanding of how insulin from the systemic circulation might actually get to the brain parenchyma, and suggest that addressing these deficiencies is requisite to both a basic understanding of insulin physiology and a rational consideration of therapeutics involving the delivery of insulin to the brain.
Brain Insulin Action
Because bulk brain glucose uptake is not affected by insulin in either rats (1) or humans (2,3), the brain had long been considered “insulin insensitive.” While there is evidence for the expression and activity of glucose transport with the insulin-sensitive GLUT4 in a few selected nuclei, glucose transport into most neurons is GLUT3 dependent, while the glia and brain endothelial cells depend on GLUT1 activity for glucose uptake from brain interstitial fluid (ISF) and plasma, respectively (4). As insulin is not required for GLUT1- or GLUT3-mediated glucose transport, insulin is not needed for glucose transport into most brain cells. Insulin does, however, play a role as a neuroregulatory peptide, and this role is slowly being unraveled (5). Early, provocative studies showed that chronic intracerebroventricular (ICV) insulin administration markedly decreased food intake and body weight in primates (6). In contrast, intravenous insulin administration to humans during an euglycemic clamp did not acutely affect food intake (7). However, chronic intranasal insulin administration, which allows more direct access to the cerebrospinal fluid (CSF) than systemic insulin administration, decreased food intake in fasting men and acutely affected postprandial selection of palatable food by women without causing hypoglycemia (8,9). In addition, the correlation between adiposity and basal plasma insulin level led to the hypothesis that insulin in the central nervous system (CNS) could, like leptin, be a chronic signal regulating or reporting on energy reserves, as opposed to an acute satiety signal (10). Consistent with an important role for CNS insulin action, neuron-specific knockout of the insulin receptor (NIRKO mouse) enhanced diet-induced obesity and provoked insulin resistance, hypertriglyceridemia, and reproductive dysfunction (11). Thus, insulin in the brain appears to be important for the regulation of feeding behavior and monitoring energy stores.
During the past decade, acute insulin action in the CNS has been reported to regulate whole-body metabolic function. Obici et al. (12) demonstrated that acute delivery of insulin via ICV injection suppressed hepatic glucose production (HGP) in conscious rats. Moreover, ICV-delivered antisense oligonucleotide knockdown of the insulin receptor (IR) blocked the ability of insulin to regulate HGP in rats (13). In addition, the ability of ICV insulin to regulate HGP is lost in NIRKO mice (11). The arcuate nucleus in the hypothalamus appears to be critical, as IR deletion in Agouti-related protein–expressing neurons from this area blunted the ability of both systemic and ICV insulin to inhibit HGP in mice (14). ICV insulin can also acutely regulate lipolysis in white adipose tissue (15). In contrast to these findings in rodents, studies in a canine model have convincingly demonstrated that insulin acts directly at the liver to suppress HGP, and, while insulin acting via the CNS can influence the expression of certain gluconeogenic enzymes, it adds little to the acute physiologic regulation of hepatic glucose metabolism (16–18). Species and significant methodological differences cloud the resolution of these disparate findings, and definitive addressing of the question in humans is technically beyond reach.
Beyond the CNS effects of insulin on nutrient intake and acute metabolic effects, there is tantalizing emerging data on the effects of insulin on memory and cognition (19,20). Recent work suggests that insulin has functional effects in multiple brain areas. Most particularly, insulin affects areas in the hippocampus that are active in reward recognition, as well as areas involved in more global cognitive and memory functions (21). These insights have arisen from studies using either ICV or nasal insulin delivery, circumventing the metabolic effects of peripherally delivered insulin that would limit such treatment to improve cognitive function. Indeed, clinical trials examining the effect of intranasal insulin as a potential therapy in early Alzheimer disease are ongoing (see www.clinicaltrials.gov/ct2/results?term=nasal+insulin).
Local Insulin Production Within the Brain
The effects of insulin in the CNS raise questions regarding how much circulating insulin reaches brain tissue and the route by which this may occur. Before addressing that, however, there is the recurring question of whether insulin is produced locally within the brain. In Drosophila, three of the seven circulating insulin-like peptides are secreted from the brain (22) to act locally on feeding behavior and systemically to regulate metabolism. While early work (23) suggested that immunoreactive insulin was present in rat brain at concentrations up to 100 times higher than that in plasma, subsequent studies did not confirm this (24), and definitive evidence for the brain synthesizing significant amounts of insulin is lacking. Furthermore, as insulin can clearly cross the blood-brain barrier (BBB) and may be concentrated in CNS tissues, simple immune detection will not provide definitive evidence for a brain insulin source. An early RT-PCR study (25) found very small amounts of rat insulin 2 (INS2) mRNA, but no rat insulin 1 (INS1) gene expression throughout the rat brain at all stages of development. This was confirmed in rabbit brain where RT-PCR revealed that the insulin gene was selectively expressed at low levels in olfactory bulbs and hippocampal neurons (26). Transcription of the INS2 gene, but not the INS1 gene, in the CNS was shown in mice (27,28). The INS2 gene is the rodent equivalent of the human INS gene, which is indeed expressed in several regions of the human brain (27). These studies did not provide any evidence for a specific function for insulin produced within the CNS. Very recently, Molnár et al. (29) reported detecting insulin mRNA in neurogliaform cells in the rat cortex using single-cell quantitative RT-PCR. Importantly, they also observed that the quantity of INS2 mRNA per cell was greater when the concentration of extracellular glucose was increased. The number of spontaneous excitatory postsynaptic potentials measured in cells neighboring neurogliaform cells was decreased when neurogliaform cells were subjected to increasing extracellular glucose concentrations. Interestingly, this effect was blocked when cells were treated with the IR blocker S961. A similar effect of insulin has been observed in mouse proopiomelanocortin neurons (30). These data obtained from cerebral cortical neuroglial cells provide the strongest evidence to date for locally produced insulin-regulating brain function as a neurotransmitter in a glucose-regulated manner (29). Clearly, this finding requires follow-up investigation.
Delivery of Insulin to the Brain
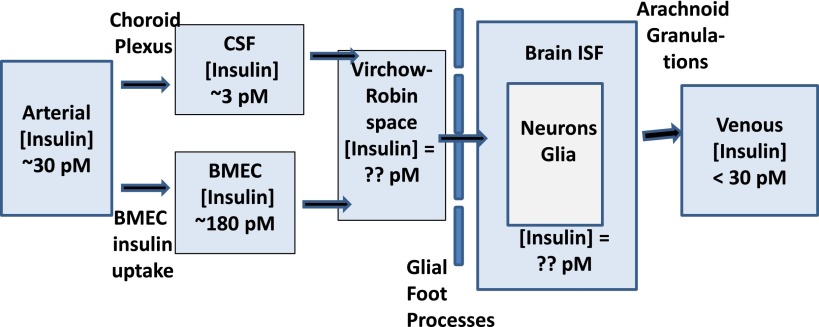
In multiple studies and several species (including humans), CSF has been used as a surrogate for brain ISF. Recent findings, however (vide infra), underscore that the composition of CSF measured in the cerebral ventricles or the subarachnoid space of the cisterna magna or lumbar spine is quite different from brain ISF. CSF contributes one component to brain ISF, and solute transport across the BBB provides another (Fig. 1). The relative contribution of these two potential routes for allowing peripherally produced insulin access to brain ISF is unknown. Studies in both experimental animals and humans uniformly indicate that a large gradient exists between plasma and CSF insulin concentrations in healthy individuals, with plasma concentrations being 10- to 20-fold higher (31–33) and this gradient being even greater in obese humans (33). Analogous findings are reported (34) for the leptin plasma/CSF gradient, suggesting that the transport of both proteins into CSF is quite restricted under healthy conditions and is further impaired by insulin resistance. Such findings raise the question of whether impaired systemic insulin delivery to CSF could contribute to impaired feeding behavior, dysregulation of hepatic and adipose tissue metabolism, and increase the risk for cognitive decline seen in type 2 diabetic and insulin-resistant patients (20). Clearly, this would only be the case if insulin delivery via CSF is a major contributor to the overall movement of insulin into brain ISF. The very low CSF insulin concentrations seen in healthy fasting humans (typically <10 pmol/L) are not sufficient to initiate significant IR activation, assuming that the IR in the CNS has kinetic properties similar to those found for IR in peripheral tissues. Equally striking in this regard are the results of kinetic studies in dogs (35) and humans (32) showing that the transit of insulin from plasma to CSF under hyperinsulinemic euglycemic clamp conditions is very slow. Even after 4 h of pharmacologic elevations in plasma insulin levels, CSF insulin concentrations remain below typical fasting plasma insulin levels (32). Such slow transport of insulin to the brain via the CSF circulation would render insulin an unlikely satiety signal.
Figure 1.
The potential pathways for insulin entry into brain ISF. The arterial and CSF insulin concentration is typical of that found in peripheral blood and in human lumbar CSF in postprandial healthy humans. The brain microvascular endothelial cell (BMEC) insulin concentration is estimated based on the observed ability of aortic endothelial cells to concentrate insulin (55).
Kinetic studies also demonstrate that insulin movement from plasma to CSF involves a saturable transport system (35) that is decreased in several insulin-resistant states (36–38). It is not known whether the IR is involved in moving insulin from blood to CSF during CSF formation by the choroid plexus, or whether the observed saturation results from the limited capacity of the more promiscuous transporter, megalin. This protein is known to mediate leptin transport across the choroid plexus (39) and can mediate insulin transport across the renal tubular epithelial cells (40). Mathematical modeling based on the transit time of radioactive insulin from plasma to the cisternal CSF in dogs suggests an intermediate compartment between plasma and cisternal CSF. Whether that compartment is between the blood-CSF barrier or simply reflects the mixing and flow through the ventricular system is unknown (41).
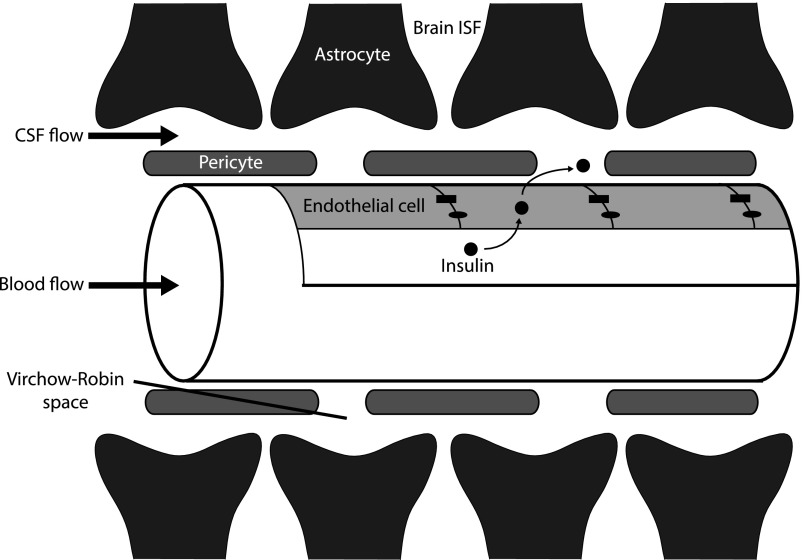
Given the above issues, it is important to consider recent data that clarifies the relationship between the CSF, as found in the cerebral ventricles or the subarachnoid space of the spinal cord, and the brain ISF. In an elegant study, Iliff et al. (42) injected several fluorescent markers of varying weight into the lateral ventricles of mice and traced their movement over time to examine their penetration into brain tissue. They identified a paravascular pathway involving the Virchow-Robin space, whereby CSF produced by the choroid plexus in the ventricles first passes through the third and fourth ventricles and eventually enters the cisterna magna (see Fig. 1 in Iliff et al. [42]). From there, it enters the subarachnoid space and subsequently accesses the Virchow-Robin space, and this para-arteriolar pathway brings CSF into contact with the blood vessel wall down to the level of the microvasculature. At this interface, water, nutrients (e.g., glucose, amino acids), electrolytes, and other solutes (e.g., possibly insulin) that cross the BBB now mix with CSF. The solutes from this admixture enter the ISF of the brain by passing through glial foot processes from astrocytes that line the Virchow-Robin space (Fig. 2). These foot processes act as filters that can restrict the entry of very large molecular weight solutes from brain ISF. Iliff et al. (43) suggest that the paravenous space also functions to clear waste from the brain interstitium, which is analogous to the lymphatic system in peripheral tissues. Insulin added to the CSF at the blood-CSF barrier in the choroid plexus will traverse the CSF circulation slowly as part of the bulk flow of CSF. In humans, CSF is made at a rate of ∼700 mL/24 h, with a total of ∼130 mL CSF being present in the brain at any time. Considering the relatively low insulin concentrations present in either the ventricular or lumbar subarachnoid CSF (see above), it can be estimated that the CSF circulation could only deliver insulin to the brain parenchyma (on a per gram of tissue basis) at a rate ∼1/600th the rate of delivery to skeletal muscle or adipose tissues and <1/30,000th the rate of delivery to the liver. This, of course, has implications for the body of work described above, in which insulin is infused into the CSF. Certainly, adding high doses of insulin to the CSF will greatly raise CSF and eventually brain ISF insulin levels, which may account for the reported effects of ICV-infused insulin on peripheral glucose and fat metabolism.
Figure 2.
Pathways for insulin delivery to brain ISF. This figure depicts a longitudinal section of a capillary, with blood and CSF flowing from left to right. The tight junctions (blocks) and adherens junctions (ovals) between endothelial cells in the brain vasculature prevent paracellular transport through the endothelial layer. Insulin is in CSF at concentrations 5–10% of those in plasma. Insulin transported across the endothelium would mix with the small amounts entering via CSF in the Virchow-Robin space, and the mixture could then enter brain ISF. The astrocytes act as the final sieve for insulin before entry into the brain ISF. The mechanisms regulating transendothelial insulin transport in brain microvasculature are unknown.
A few studies in rats have attempted to measure brain ISF insulin concentration using microdialysis. These studies detected very low fasting insulin concentrations in the hypothalamus, which increased significantly 30–60 min after a meal or peripheral insulin infusion, a rise more rapid than that seen in CSF (44,45). Whether these measurements truly reflect ISF or a combination of ISF, CSF, and vascular leakage in the region of the acutely placed microdialysis catheter is uncertain. These concerns, as well as the technical limitations that affect microdialysis measurements of large molecules (46), have limited the use of this method.
While the majority of work addressing insulin access to brain tissue has used CSF as a surrogate for brain ISF, some studies (47) have directly examined the “tissue content” of radiolabeled insulin in either brain sections or tissue samples as a function of time after intravenous injection in mice. These latter studies do not discriminate between insulin delivered via the choroid plexus (CSF circulation) and insulin delivered directly across the BBB to specific nuclei. In addition, these studies have not been conducted in a fashion that allows estimation of the brain ISF insulin concentration; rather, they report on radioactivity in specific regions. Such studies have indicated that intravenously administered insulin reaches many areas of the brain seemingly quickly, and appears to most readily penetrate the hypothalamus, the pons/medulla, and the hippocampus (48). Considering the possible direct movement of insulin across the BBB, investigators have also demonstrated that insulin binds to isolated brain microvessels with high affinity, which is consistent with participation by the IR (49) and that there is little, if any, degradation of insulin incubated with brain microvessels. Consequently, whether the rapid access of radiolabeled (125I) insulin to the brain parenchyma simply reflects insulin binding to endothelial cells in the brain microvasculature, its uptake by the endothelial cell, or its actual delivery to the brain ISF is not resolved by these studies. This notwithstanding, these findings with 125I-insulin suggest that transit across the BBB may be the preferred route of insulin entry into the brain. However, if this is the case, it appears fair to say that we know virtually nothing about the cell biology of this process and how it might—or might not—be regulated. This would appear to be an important area for future investigation. Whether the primary route for insulin transfer from the plasma to the brain ISF happens at the BBB throughout the brain, or is restricted to the choroid plexus and CSF, it is likely that the endothelium is involved.
We have been working to unravel aspects of the kinetics, cell biology, and regulation of insulin transport by endothelial cells from peripheral vessels (50). That transport appears to involve an insulin-regulated vesicular trafficking process requiring caveolae. It begins with insulin binding to its receptor (or at high insulin concentrations, the IGF-1 receptor) (51). In aortic endothelial cells, the IR is associated with caveolae, and the knockdown of caveolin-1 (the principal structural protein of caveolae) or chemical disruption of caveolae interferes with endothelial cell insulin transport (52). Likewise, interfering with insulin action in the endothelial cell by inhibiting signaling through the PI3 kinase, Src kinase, or MAP kinase pathway impedes endothelial cell insulin uptake (53). Perhaps importantly, transport activity appears negatively impacted by insulin resistance (54). It will be of great interest to see whether the brain endothelium behaves in a similar fashion.
In closing, it is interesting to consider that this question of how insulin reaches targets within the CNS may be part of a larger question of how a host of peptides synthesized in the periphery navigate this voyage. Peptides such as leptin, GLP-1, ghrelin, cholecystokinin, and others each act centrally, and must reach brain ISF to exert their specific effects. It will be fascinating to unravel just how this occurs for insulin and these other peptides.
Article Information
Funding. This work was supported by research grants from the National Institutes of Health (DK-057878 and DK-073059) and the American Diabetes Association (11-BS6) to E.J.B.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
References
- 1.Hom FG, Goodner CJ, Berrie MA. A [3H]2-deoxyglucose method for comparing rates of glucose metabolism and insulin responses among rat tissues in vivo. Validation of the model and the absence of an insulin effect on brain. Diabetes 1984;33:141–152 [DOI] [PubMed] [Google Scholar]
- 2.Hasselbalch SG, Knudsen GM, Videbaek C, et al. No effect of insulin on glucose blood-brain barrier transport and cerebral metabolism in humans. Diabetes 1999;48:1915–1921 [DOI] [PubMed] [Google Scholar]
- 3.Seaquist ER, Damberg GS, Tkac I, Gruetter R. The effect of insulin on in vivo cerebral glucose concentrations and rates of glucose transport/metabolism in humans. Diabetes 2001;50:2203–2209 [DOI] [PubMed] [Google Scholar]
- 4.McEwen BS, Reagan LP. Glucose transporter expression in the central nervous system: relationship to synaptic function. Eur J Pharmacol 2004;490:13–24 [DOI] [PubMed] [Google Scholar]
- 5.Ghasemi R, Haeri A, Dargahi L, Mohamed Z, Ahmadiani A. Insulin in the brain: sources, localization and functions. Mol Neurobiol 2013;47:145–171 [DOI] [PubMed] [Google Scholar]
- 6.Woods SC, Lotter EC, McKay LD, Porte D, Jr. Chronic intracerebroventricular infusion of insulin reduces food intake and body weight of baboons. Nature 1979;282:503–505 [DOI] [PubMed] [Google Scholar]
- 7.Chapman IM, Goble EA, Wittert GA, Morley JE, Horowitz M. Effect of intravenous glucose and euglycemic insulin infusions on short-term appetite and food intake. Am J Physiol 1998;274:R596–R603 [DOI] [PubMed] [Google Scholar]
- 8.Hallschmid M, Higgs S, Thienel M, Ott V, Lehnert H. Postprandial administration of intranasal insulin intensifies satiety and reduces intake of palatable snacks in women. Diabetes 2012;61:782–789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benedict C, Kern W, Schultes B, Born J, Hallschmid M. Differential sensitivity of men and women to anorexigenic and memory-improving effects of intranasal insulin. J Clin Endocrinol Metab 2008;93:1339–1344 [DOI] [PubMed] [Google Scholar]
- 10.Baskin DG, Figlewicz Lattemann D, Seeley RJ, Woods SC, Porte D, Jr, Schwartz MW. Insulin and leptin: dual adiposity signals to the brain for the regulation of food intake and body weight. Brain Res 1999;848:114–123 [DOI] [PubMed] [Google Scholar]
- 11.Brüning JC, Gautam D, Burks DJ, et al. Role of brain insulin receptor in control of body weight and reproduction. Science 2000;289:2122–2125 [DOI] [PubMed] [Google Scholar]
- 12.Obici S, Zhang BB, Karkanias G, Rossetti L. Hypothalamic insulin signaling is required for inhibition of glucose production. Nat Med 2002;8:1376–1382 [DOI] [PubMed] [Google Scholar]
- 13.Obici S, Feng Z, Karkanias G, Baskin DG, Rossetti L. Decreasing hypothalamic insulin receptors causes hyperphagia and insulin resistance in rats. Nat Neurosci 2002;5:566–572 [DOI] [PubMed] [Google Scholar]
- 14.Könner AC, Janoschek R, Plum L, et al. Insulin action in AgRP-expressing neurons is required for suppression of hepatic glucose production. Cell Metab 2007;5:438–449 [DOI] [PubMed] [Google Scholar]
- 15.Scherer T, O’Hare J, Diggs-Andrews K, et al. Brain insulin controls adipose tissue lipolysis and lipogenesis. Cell Metab 2011;13:183–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramnanan CJ, Kraft G, Smith MS, et al. Interaction between the central and peripheral effects of insulin in controlling hepatic glucose metabolism in the conscious dog. Diabetes 2013;62:74–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Edgerton DS, Lautz M, Scott M, et al. Insulin’s direct effects on the liver dominate the control of hepatic glucose production. J Clin Invest 2006;116:521–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramnanan CJ, Edgerton DS, Cherrington AD. Evidence against a physiologic role for acute changes in CNS insulin action in the rapid regulation of hepatic glucose production. Cell Metab 2012;15:656–664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Benedict C, Hallschmid M, Schultes B, Born J, Kern W. Intranasal insulin to improve memory function in humans. Neuroendocrinology 2007;86:136–142 [DOI] [PubMed] [Google Scholar]
- 20.Freiherr J, Hallschmid M, Frey WH, 2nd, et al. Intranasal insulin as a treatment for Alzheimer’s disease: a review of basic research and clinical evidence. CNS Drugs 2013;27:505–514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Craft S, Baker LD, Montine TJ, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: a pilot clinical trial. Arch Neurol 2012;69:29–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luo J, Becnel J, Nichols CD, Nässel DR. Insulin-producing cells in the brain of adult Drosophila are regulated by the serotonin 5-HT1A receptor. Cell Mol Life Sci 2012;69:471–484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Havrankova J, Schmechel D, Roth J, Brownstein M. Identification of insulin in rat brain. Proc Natl Acad Sci U S A 1978;75:5737–5741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baskin DG, Stein LJ, Ikeda H, et al. Genetically obese Zucker rats have abnormally low brain insulin content. Life Sci 1985;36:627–633 [DOI] [PubMed] [Google Scholar]
- 25.Devaskar SU, Singh BS, Carnaghi LR, Rajakumar PA, Giddings SJ. Insulin II gene expression in rat central nervous system. Regul Pept 1993;48:55–63 [DOI] [PubMed] [Google Scholar]
- 26.Devaskar SU, Giddings SJ, Rajakumar PA, Carnaghi LR, Menon RK, Zahm DS. Insulin gene expression and insulin synthesis in mammalian neuronal cells. J Biol Chem 1994;269:8445–8454 [PubMed] [Google Scholar]
- 27.Mehran AE, Templeman NM, Brigidi GS, et al. Hyperinsulinemia drives diet-induced obesity independently of brain insulin production. Cell Metab 2012;16:723–737 [DOI] [PubMed] [Google Scholar]
- 28.Deltour L, Leduque P, Blume N, et al. Differential expression of the two nonallelic proinsulin genes in the developing mouse embryo. Proc Natl Acad Sci U S A 1993;90:527–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Molnár G, Faragó N, Kocsis AK, et al. GABAergic neurogliaform cells represent local sources of insulin in the cerebral cortex. J Neurosci 2014;34:1133–1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams KW, Margatho LO, Lee CE, et al. Segregation of acute leptin and insulin effects in distinct populations of arcuate proopiomelanocortin neurons. J Neurosci 2010;30:2472–2479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Strubbe JH, Porte D, Jr, Woods SC. Insulin responses and glucose levels in plasma and cerebrospinal fluid during fasting and refeeding in the rat. Physiol Behav 1988;44:205–208 [DOI] [PubMed] [Google Scholar]
- 32.Wallum BJ, Taborsky GJ, Jr, Porte D, Jr, et al. Cerebrospinal fluid insulin levels increase during intravenous insulin infusions in man. J Clin Endocrinol Metab 1987;64:190–194 [DOI] [PubMed] [Google Scholar]
- 33.Kern W, Benedict C, Schultes B, et al. Low cerebrospinal fluid insulin levels in obese humans. Diabetologia 2006;49:2790–2792 [DOI] [PubMed] [Google Scholar]
- 34.Schwartz MW, Peskind E, Raskind M, Boyko EJ, Porte D, Jr. Cerebrospinal fluid leptin levels: relationship to plasma levels and to adiposity in humans. Nat Med 1996;2:589–593 [DOI] [PubMed] [Google Scholar]
- 35.Schwartz MW, Sipols A, Kahn SE, et al. Kinetics and specificity of insulin uptake from plasma into cerebrospinal fluid. Am J Physiol 1990;259:E378–E383 [DOI] [PubMed] [Google Scholar]
- 36.Begg DP, Mul JD, Liu M, et al. Reversal of diet-induced obesity increases insulin transport into cerebrospinal fluid and restores sensitivity to the anorexic action of central insulin in male rats. Endocrinology 2013;154:1047–1054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baura GD, Foster DM, Kaiyala K, Porte D, Jr, Kahn SE, Schwartz MW. Insulin transport from plasma into the central nervous system is inhibited by dexamethasone in dogs. Diabetes 1996;45:86–90 [DOI] [PubMed] [Google Scholar]
- 38.Kaiyala KJ, Prigeon RL, Kahn SE, Woods SC, Schwartz MW. Obesity induced by a high-fat diet is associated with reduced brain insulin transport in dogs. Diabetes 2000;49:1525–1533 [DOI] [PubMed] [Google Scholar]
- 39.Dietrich MO, Spuch C, Antequera D, et al. Megalin mediates the transport of leptin across the blood-CSF barrier. Neurobiol Aging 2008;29:902–912 [DOI] [PubMed] [Google Scholar]
- 40.Orlando RA, Rader K, Authier F, et al. Megalin is an endocytic receptor for insulin. J Am Soc Nephrol 1998;9:1759–1766 [DOI] [PubMed] [Google Scholar]
- 41.Schwartz MW, Bergman RN, Kahn SE, et al. Evidence for entry of plasma insulin into cerebrospinal fluid through an intermediate compartment in dogs. Quantitative aspects and implications for transport. J Clin Invest 1991;88:1272–1281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iliff JJ, Wang M, Liao Y, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Sci Transl Med 2012;4:147ra111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Iliff JJ, Lee H, Yu M, et al. Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J Clin Invest 2013;123:1299–1309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gerozissis K, Orosco M, Rouch C, Nicolaidis S. Insulin responses to a fat meal in hypothalamic microdialysates and plasma. Physiol Behav 1997;62:767–772 [DOI] [PubMed] [Google Scholar]
- 45.Orosco M, Gerozissis K, Rouch C, Nicolaïdis S. Feeding-related immunoreactive insulin changes in the PVN-VMH revealed by microdialysis. Brain Res 1995;671:149–158 [DOI] [PubMed] [Google Scholar]
- 46.Barrett EJ, Eringa EC. The vascular contribution to insulin resistance: promise, proof, and pitfalls. Diabetes 2012;61:3063–3065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Banks WA, Kastin AJ. Differential permeability of the blood-brain barrier to two pancreatic peptides: insulin and amylin. Peptides 1998;19:883–889 [DOI] [PubMed] [Google Scholar]
- 48.Banks WA, Kastin AJ, Huang W, Jaspan JB, Maness LM. Leptin enters the brain by a saturable system independent of insulin. Peptides 1996;17:305–311 [DOI] [PubMed] [Google Scholar]
- 49.Pardridge WM, Eisenberg J, Yang J. Human blood-brain barrier insulin receptor. J Neurochem 1985;44:1771–1778 [DOI] [PubMed] [Google Scholar]
- 50.Barrett EJ, Wang H, Upchurch CT, Liu Z. Insulin regulates its own delivery to skeletal muscle by feed-forward actions on the vasculature. Am J Physiol Endocrinol Metab 2011;301:E252–E263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang H, Liu Z, Li G, Barrett EJ. The vascular endothelial cell mediates insulin transport into skeletal muscle. Am J Physiol Endocrinol Metab 2006;291:E323–E332 [DOI] [PubMed] [Google Scholar]
- 52.Wang H, Wang AX, Barrett EJ. Caveolin-1 is required for vascular endothelial insulin uptake. Am J Physiol Endocrinol Metab 2011;300:E134–E144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang H, Wang AX, Liu Z, Barrett EJ. Insulin signaling stimulates insulin transport by bovine aortic endothelial cells. Diabetes 2008;57:540–547 [DOI] [PubMed] [Google Scholar]
- 54.Wang H, Wang AX, Aylor K, Barrett EJ. Nitric oxide directly promotes vascular endothelial insulin transport. Diabetes 2013;62:4030–4042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Genders AJ, Frison V, Abramson SR, Barrett EJ. Endothelial cells actively concentrate insulin during its transendothelial transport. Microcirculation 2013;20:434–439 [DOI] [PMC free article] [PubMed] [Google Scholar]