Many lines of evidence indicate that insulin resistance is a key component of the metabolic syndrome, a cluster of cardiovascular risk factors comprising glucose intolerance, dyslipidemia, hypertension, and obesity (1). Insulin resistance is also of central importance in the pathogenesis of type 2 diabetes, another major risk factor for atherosclerosis (1). However, the molecular mechanisms that precede the development of insulin resistance are only partially understood. Given the dramatic increases in the incidence of obesity and diabetes worldwide, the need to identify new therapies that might protect humans from the metabolic consequences of obesity and insulin resistance is urgent.
Macrophages, T cells, B cells, mast cells, and eosinophils accumulate in adipose tissue of obese mice. Each of these immune cells seems to contribute to the development of insulin resistance during diet-induced obesity (2). However, neutrophils—the most abundant circulating immune cell in both mice and humans—are generally the first cells to respond to an inflammatory challenge, although their role in insulin resistance has received much less attention. It is noteworthy that circulating neutrophil concentrations increase in obese mice (3). Moreover, neutrophils accumulate in murine adipose tissue after only 3 days of fat feeding (4). Importantly, recent studies have shown that fat-fed mice that are deficient in neutrophil elastase exhibit less adipose tissue inflammation and are more insulin sensitive than fat-fed controls. These observations suggest that inflammatory mediators derived from neutrophils might promote the development of obesity and its metabolic consequences (5).
The most abundant protein in human neutrophils is myeloperoxidase (MPO). Using hydrogen peroxide, this heme protein generates a wide array of reactive intermediates (6), although its best known product is hypochlorous acid (HOCl). This potent chlorinating intermediate is a unique product of MPO in mammals (7). Because it produces microbicidal oxidants such as HOCl, MPO has classically been considered an innate immune effector with a key role in host defense mechanisms during acute infection (6,7). However, the oxidizing molecular species generated by MPO during the inflammatory response can be indiscriminate because they can react with host, as well as pathogen, molecules (8). One important target may be lipoproteins, which become proatherogenic when oxidatively modified by MPO (9).
In this issue, Wang and colleagues (10) confirm previous findings that infiltration of white adipose tissue by neutrophils is an early and persistent event in the development of diet-induced obesity (4,5). Neutrophil actions, therefore, could be required for obesity-induced hyperglycemia and insulin resistance. Diet-induced obesity increased both adipose neutrophil infiltration and MPO activity in the absence of changes in MPO protein. These observations suggest a novel mechanism for the regulation of MPO activity in obesity and warrant further investigation.
Wang et al. (10) demonstrated that mice deficient in MPO were resistant to diet-induced obesity and insulin resistance. Fat-fed MPO-deficient mice exhibited elevated body temperature, increased concentrations of uncoupling protein-1, and higher mitochondrial oxygen consumption in brown adipose tissue compared with their fat-fed wild-type counterparts. MPO-deficient mice also showed improved insulin signaling in white adipose tissue. The reduced diet-induced obesity was associated with greater brown adipose uncoupling, which should lead to greater energy loss. Again, the underlying mechanisms are unclear, but increased energy expenditure is likely to be a key component of the improved metabolic state.
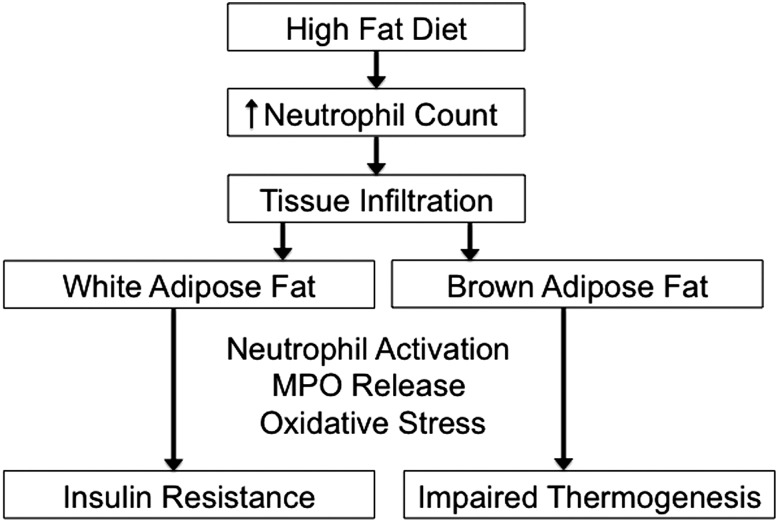
The investigators then asked whether HOCl—the product of MPO action—affected insulin signaling. In vitro studies of 3T3-L1 adipocytes demonstrated that HOCl inhibited insulin-stimulated phosphorylation of insulin receptor-β, insulin receptor substrate-1, and Akt. HOCl also inhibited insulin-induced binding of insulin receptor substrate-1 to P85, the regulatory subunit of phosphatidylinositide 3-kinase, a key enzyme during insulin signaling. Importantly, a nonspecific peroxidase inhibitor that blocked MPO activity in isolated neutrophils prevented diet-induced insulin resistance in obese wild-type mice. Taken together, these observations raise the exciting possibility that MPO is a major contributor to the development of inflammation-induced insulin resistance and metabolic disease. Wang et al. (10) propose that white and brown fat are targeted for damage by MPO and infiltrating neutrophils (Fig. 1). Testing this hypothesis in future studies will be important.
Figure 1.
Potential roles of neutrophil-derived MPO in insulin resistance and obesity. In this issue, Wang and colleagues (10) demonstrate that when mice consume a high-fat diet rich in calories, neutrophils infiltrate white and brown adipose tissue. Following activation by unknown mechanisms, the neutrophils release MPO, which uses hydrogen peroxide to generate a wide array of oxidizing intermediates. Oxidative damage of specific targets promotes insulin resistance and impairs thermogenesis, resulting in decreased energy expenditure, elevated glucose concentrations, further weight gain, and diabetes. Mice deficient in MPO are protected from diet-induced obesity and insulin resistance, raising the possibility that selective inhibitors of MPO might be able to prevent or treat insulin resistance in obese humans.
A key question is whether these observations in a mouse model of diet-induced obesity are relevant to humans. Human obesity and diabetes are known to associate strongly with leukocytosis (11–13). Moreover, elevated plasma concentrations of MPO were strongly associated with inflammation and a variety of other cardiovascular disease risk factors in a study of prepubertal obese children (14). Also, MPO has been implicated in the pathogenesis of human cardiovascular disease by a number of mechanisms, including lipoprotein oxidation (9) and the development of endothelial dysfunction (15), the latter an important early step in atherosclerosis. Weight loss in obese subjects decreased neutrophil and monocyte counts (4). The decrease in circulating leukocyte counts correlated with improved insulin sensitivity. Collectively, these observations suggest that neutrophils—and perhaps MPO—contribute to obesity-associated insulin resistance and cardiovascular disease in humans.
There is intense interest in developing therapies that could inhibit inflammatory pathways in obesity to prevent the onset of insulin resistance and its associated metabolic disorders. MPO can be readily inhibited by nonspecific peroxidase inhibitors (16), and its crystal structure is remarkably similar to that of cyclooxygenase (17), suggesting that it could be targeted for selective and specific inhibition. Moreover, nonspecific peroxidase inhibitors seem to be clinically safe, and several are currently used to treat hyperthyroidism (18). Importantly, although MPO-deficient mice are susceptible to bacterial and fungal infections, nondiabetic humans deficient in the heme protein do not seem to have impaired host defense mechanisms or increased risk of infection (19). Taken together, these observations suggest that selective inhibitors of MPO might be able to prevent or treat insulin resistance in obese humans. Moreover, such agents might also be useful for lowering the risk of cardiovascular disease by a number of other mechanisms, including blocking lipoprotein oxidation and preserving endothelial function in the coronary circulation.
To better understand the molecular targets of MPO and how the enzyme mediates insulin resistance, confirming and extending these observations in both human and animal models are important. This is crucial because although both mouse and human neutrophils express high concentrations of MPO, only human macrophages express the enzyme (8,20). Identifying biomarkers of MPO action also is critical, not only to determine whether elevated concentrations of such markers associate with insulin resistance or other proposed pathogenic mechanisms but also to establish whether potential selective MPO inhibitors are in fact active in vivo.
Article Information
Duality of Interest. J.W.H. is named by the U.S. Patent Office as a coinventor on patents on the use of HDL metrics to predict the risk of cardiovascular disease. No other conflicts of interest relevant to this article were reported.
Footnotes
See accompanying article, p. 4172.
References
- 1.Semenkovich CF. Insulin resistance and atherosclerosis. J Clin Invest 2006;116:1813–1822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glass CK, Olefsky JM. Inflammation and lipid signaling in the etiology of insulin resistance. Cell Metab 2012;15:635–645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagareddy PR, Kraakman M, Masters SL, et al. Adipose tissue macrophages promote myelopoiesis and monocytosis in obesity. Cell Metab 2014;19:821–835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elgazar-Carmon V, Rudich A, Hadad N, Levy R. Neutrophils transiently infiltrate intra-abdominal fat early in the course of high-fat feeding. J Lipid Res 2008;49:1894–1903 [DOI] [PubMed] [Google Scholar]
- 5.Talukdar S, Oh Y, Bandyopadhyay G, et al. Neutrophils mediate insulin resistance in mice fed a high-fat diet through secreted elastase. Nat Med 2012;18:1407–1412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klebanoff SJ, Kettle AJ, Rosen H, Winterbourn CC, Nauseef WM. Myeloperoxidase: a front-line defender against phagocytosed microorganisms. J Leukoc Biol 2013;93:185–198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaut JP, Yeh GC, Tran HD, et al. Neutrophils employ the myeloperoxidase system to generate antimicrobial brominating and chlorinating oxidants during sepsis. Proc Natl Acad Sci U S A 2001;98:11961–11966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daugherty A, Dunn JL, Rateri DL, Heinecke JW. Myeloperoxidase, a catalyst for lipoprotein oxidation, is expressed in human atherosclerotic lesions. J Clin Invest 1994;94:437–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shao B, Oda MN, Oram JF, Heinecke JW. Myeloperoxidase: an oxidative pathway for generating dysfunctional high-density lipoprotein. Chem Res Toxicol 2010;23:447–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Q, Xie Z, Zhang W, et al. Myeloperoxidase deletion prevents high-fat diet–induced obesity and insulin resistance. Diabetes 2014;63:4172–4185 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Schmidt MI, Duncan BB, Sharrett AR, et al. Markers of inflammation and prediction of diabetes mellitus in adults (Atherosclerosis Risk in Communities study): a cohort study. Lancet 1999;353:1649–1652 [DOI] [PubMed] [Google Scholar]
- 12.Ford ES. Leukocyte count, erythrocyte sedimentation rate, and diabetes incidence in a national sample of US adults. Am J Epidemiol 2002;155:57–64 [DOI] [PubMed] [Google Scholar]
- 13.Ohshita K, Yamane K, Hanafusa M, et al. Elevated white blood cell count in subjects with impaired glucose tolerance. Diabetes Care 2004;27:491–496 [DOI] [PubMed] [Google Scholar]
- 14.Olza J, Aguilera CM, Gil-Campos M, et al. Myeloperoxidase is an early biomarker of inflammation and cardiovascular risk in prepubertal obese children. Diabetes Care 2012;35:2373–2376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baldus S, Rudolph V, Roiss M, et al. Heparins increase endothelial nitric oxide bioavailability by liberating vessel-immobilized myeloperoxidase. Circulation 2006;113:1871–1878 [DOI] [PubMed] [Google Scholar]
- 16.Kazura JW, de Brito P, Rabbege J, Aikawa M. Role of granulocyte oxygen products in damage of Schistosoma mansoni eggs in vitro. J Clin Invest 1985;75:1297–1307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garavito RM, Mulichak AM. The structure of mammalian cyclooxygenases. Annu Rev Biophys Biomol Struct 2003;32:183–206 [DOI] [PubMed] [Google Scholar]
- 18.Nagasaka A, Hidaka H. Effect of antithyroid agents 6-propyl-2-thiouracil and 1-mehtyl-2-mercaptoimidazole on human thyroid iodine peroxidase. J Clin Endocrinol Metab 1976;43:152–158 [DOI] [PubMed] [Google Scholar]
- 19.Nauseef WM. Myeloperoxidase deficiency. Hematol Oncol Clin North Am 1988;2:135–158 [PubMed] [Google Scholar]
- 20.Sugiyama S, Okada Y, Sukhova GK, Virmani R, Heinecke JW, Libby P. Macrophage myeloperoxidase regulation by granulocyte macrophage colony-stimulating factor in human atherosclerosis and implications in acute coronary syndromes. Am J Pathol 2001;158:879–891 [DOI] [PMC free article] [PubMed] [Google Scholar]