Abstract
Objective:
The aim of this study was to compare the amount of root resorption after orthodontic treatment between the bidimensional and the Roth straight-wire techniques. Another objective was to compare the amount of root resorption in the whole sample studied and record the prevalence of root resorption.
Materials and Methods:
The sample consisted of 40 patients (age ranged between 11 and 18 years) with Angle Class II division 1 malocclusions, treated nonextraction. Twenty patients were treated with bidimensional technique and 20 with a 0.018-inch Roth straight-wire technique. Root lengths of the maxillary incisors were measured on pre- and post-treatment periapical radiographs.
Results:
The results demonstrated that the bidimensional and Roth straight-wire groups showed significant root resorption after treatment, 1.11 (0.17) and 0.86 (0.05), respectively, P < 0.001. When comparing the amount of root shortening between the bidimensional and Roth straight-wire groups, there was no significant difference between the mean change from pre- to post-treatment between bidimensional group (mean = 1.00 ± 1.34) and Roth straight-wire group (mean = 0.88 ± 0.86), P = 0.63. Considering the whole sample, there was no root resoprtion in 32.5% of the analysed teeth. There was only mild resorption in 56.2%, moderate in 8.8% and severe in only 2.5% of the teeth.
Conclusions:
Treatment with the bidimensional technique did not produce an increase in the amount of root resorption. The prevalence and amount of root resorption was similar between bidimensional and Roth straight-wire techniques.
Keywords: Bidimensional, orthodontic, root resorption, Roth, slot-size, straight-wire
INTRODUCTION
The field of orthodontics has been investigating the etiology of root resorption since 1927 when the relationship between orthodontic therapy and root resorption was recognized.[1,2] Unfortunately, even though this relationship has been known, little definitive conclusions have been reached as to the specific etiologic factors involved.[3] Brezniak addressed this issue when he noted that even though most root resorption studies attempt to determine the etiologic factors however, the causes remain obscure.[1,2]
The factors that have been proposed to induce root resorption are complex and include the following: Individual susceptibility, genetics, systemic factors, nutrition, chronological age, dental age, root shape, gender, history of resorption, previously traumatized teeth, endodontically treated teeth, density of alveolar bone, orthodontic therapy mechanics and duration of treatment.[1,4] This alludes to the difficulty in controlling confounding factors when performing a study. To help clarify this phenomenon much research has been performed to determine the process of root resorption during orthodontics.
The mechanism of action of orthodontic therapy is to place a force on the teeth that will induce a biological response in the supporting bone. The response must initiate resorption of bone on the side of compression, which allows the tooth to move in the direction of the force applied. Without this response orthodontics would not be possible. Unfortunately, the compressive force is also placed onto the root structure. Therefore, it is of no surprise that root structure often displays a certain amount of resorption after orthodontic therapy. Fortunately, the amount of resorption of the root is usually small and insignificant in determining the longevity of the involved teeth.[1,4,5] In general, the amount of root resorption is significantly less than the amount of bone resorption present. This allows one to suspect that the root is less susceptible to resorption than the bone.[4]
When studying root resorption, pre- and post-treatment cephalometric and panoramic radiographs have been used since they are routinely acquired in orthodontic treatment.[6,7,8,9] However, the most common type of radiograph used is a periapical type and until 1983 when Linge and Linge[10,11] standardized a magnification factor it was difficult to determine if the change in root length was a result of actual loss of tooth or positioning of the radiograph. Their method enabled the investigator to accurately compare root lengths of a pretreatment to a posttreatment radiograph by measuring the crown length, factoring in that the crown length would not be affected by orthodontic therapy.
The risk factors that lead to root resorption are vast and varied. To date it appears that much of this research is conflicting and generally inconclusive.
Schudy and Schudy[12] in 1975 introduced the concept of the bidimensional technique as the “bimetric system.” This was followed by the “bidimensional-wire technique,” as improved by Gianelly et al.[13] Later, it was modified as the “bidimensional technique”[14,15] which is a “bidimensional-slot” technique. In current literature, the application of the bidimensional technique has been reported,[15,16,17,18] but seldom has the bidimensional technique been compared with other techniques.
Therefore, the objective of this study was to compare the amount of root resorption after orthodontic treatment between the bidimensional technique and the Roth straight-wire System. Another objective was to compare the amount of root resorption in the whole sample studied and record the prevalence of root resorption.
MATERIALS AND METHODS
A total of 40 patients were studied. The sample consisted of two orthodontically treated groups: Bidimensional technique group (0.018-inch slot for the incisors and 0.022-inch slot for the canines, premolars and molars, GAC International, Bohemia, NY, USA) treated at a private practice and Roth straight-wire technique group (Roth 0.018-inch slot system, 3M unitek, Monrovia, CA, USA) treated at the Orthodontic Department, Faculty of Dentistry, King Abdulaziz, Saudi Arabia.
The inclusion criteria were: Class II division 1 malocclusion, overjet of 4 mm or more, nonextraction orthodontic treatment, good quality pre- and post-treatment clear periapical radiographs and a full complement of teeth (excluding third molars) with no supernumerary teeth. Exclusion criteria included: (1) Signs of apical root resorption at the beginning of treatment, (2) endodontically treated maxillary incisors, (3) poor quality radiographs, (4) incomplete orthodontic records and (5) history of previous orthodontic treatment. One investigator treated all cases. The study was reviewed and approved by the Faculty of Dentistry's Research Ethics Committee.
The bidimensional group consisted of 20 patients, 9 males and 11 females with a mean age of 13.95 years (age ranged between 11 and 18 years) at the start of treatment. The Roth straight-wire group consisted of 20 patients, 7 males and 13 females with a mean age was 14.85 years.
The research was a case controlled study and the data was collected from pretreatment and posttreatment periapical radiographs. Apical root resorption of the upper central incisors was measured on periapical radiographs using the Sirona Sidexis software (Sirona Dental Systems GmbH, Bensheim, Germany). Root length was defined as the length from the tooth's cementoenamel junction to its apex. This measurement was determined to the nearest 0.1 mm. The method of Linge and Linge[10,11] was used to account for changes in magnification of the radiographs from pre- to post-treatment and between the two periapical machines.
The amount of root resorption was defined as the difference from pretreatment to that of posttreatment.
One calibrated examiner who was blind with regards to the treatment technique performed all measurements using the Sirona Sidexis software. Reproducibility of the measurements was evaluated by assessing the root length of 12 randomly selected radiographs not involved in the study at two different occasions, at least 10 days apart. Intra-examiner reliability analysis was performed. The results showed significant intra-examiner reliability between measurements with intraclass correlation coefficient of 0.95, P < 0.001.
Statistical Analysis
Paired Student's t-tests were performed to determine intra-group pre- treatment to post-treatment differences. Independent sample Student's t-test was performed to determine inter-group difference between the bidimensional and the Roth straight-wire techniques. Mann-Whitney U-test was used for categorical data. Statistical analyses were performed using Statistical Package for the Social Sciences version 20.0 (IBM Corp., Released 2011. IBM SPSS Statistics for Mac, Armonk, NY: IBM Corp., USA).
RESULTS
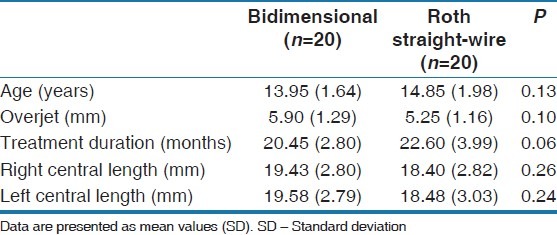
There were no significant differences found between the two treatment groups for age, amount of overjet, treatment duration, right or left central incisor root length at the beginning of treatment [Table 1]. Therefore, no significant inter-group differences were found between the bidimensional and Roth straight-wire technique for any of the variables.
Table 1.
Summary and comparisons of treatment variables at the beginning of treatment
The prevalence of root resorption is shown in Table 2. Based on the Mann–Whitney U-test there was no difference between the number of teeth exhibiting resoprtion (mild, moderate or severe) in both groups, P = 0.346.
Table 2.
Prevalence and percentage (%) of root resorption in the maxillary central incisors in the bidimensional and Roth straight-wire groups
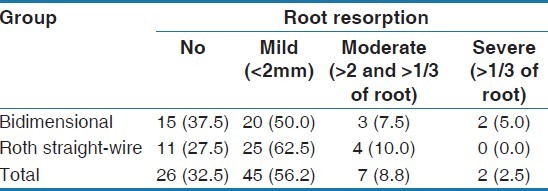
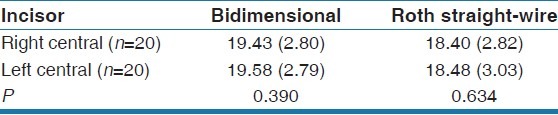
Table 3 shows that there were no significant differences in the pretreatment root lengths between right and left central incisors for both the bidimensional and Roth straight-wire groups. And because the sample size was small in each group, the measurements of the right and left root lengths were pooled as one variable rendering a sample size of 40 roots in each group.
Table 3.
Comparisons of the right and left amount of root resorption (mm) between the bidimensional and Roth straight-wire groups
There was a statistically significant amount of root resorption noted in both the bidimensional and Roth straight-wire groups from pretreatment to posttreatment [Table 4].
Table 4.
Bivariate comparisons of root resorption (mm) in both groups
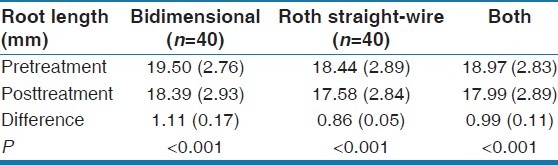
When comparing the amount of root shortening between the bidimensional and Roth straight-wire groups, the independent sample t-test showed that there was no significant difference between the mean change from pre- to post-treatment between bidimensional group (mean = 1.00 ± 1.34) and Roth Straight-wire group (mean = 0.88 ± 0.86), P = 0.63.
DISCUSSION
One of the major untoward effects of orthodontic treatment is loss of root structure. Currently, the etiologic factors of root resorption are still unpredictable. Several factors have been investigated and proposed as risk factors for apical root resorption, including gender, age, systemic factors, morphological characteristics of the dentition, previous trauma, certain malocclusions, type of mechanics and type of tooth movement and forces used.[2,3,7,10,11,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35]
Several studies have also demonstrated a link between the technique used during fixed appliance orthodontic therapy and the amount of root resorption noted. However, the results were conflicting.[2,7,9,36,37,38] Furthermore, none of these studies compared the effect of the bidimensional and Roth straight-wire techniques on roots.
In this study, it was found that both techniques produced a statistically significant amount of root resorption [Table 3]. The bidimensional technique group was found to have a mean value of 1.11 mm (±0.17) of root resorption and the Roth straight-wire technique group was found to have a mean value of 0.86 mm (±0.05). Moreover, the prevalence of root resorption was almost similar, 35% in the bidimensional group and 30% in the Roth straight-wire group. Fortunately, this amount of root resorption is considered clinical insignificance.[5]
The bidimensional technique utilizes different mechanics than the Roth straight-wire technique in order to correct a Class II malocclusion by applying heavier forces while the 0.018-inch slot Roth straight-wire technique utilizes lighter forces. In nonextraction therapy the bidimensional techniques typically begins treatment by distalizing of the upper molars into a Class I position. Then the canines followed by the anterior teeth are retracted bodily using Class I forces, while either Class II elastics or temporary anchorage mini-screws are used for anchorage. The majority of these mechanics are performed with 0.018 inch × 0.022 inch or 0.018 inch × 0.025 inch stainless steel arch-wires to facilitate bodily movement. Roth straight-wire technique on the other hand, utilizes 0.018-inch slot with Class II elastics to distalize the molars and retract the maxillary anterior teeth and simultaneously procline the mandibular anterior teeth. The majority of this treatment is performed on 0.016 × 0.022ss arch-wires and possibly producing a significant amount of proclination of the mandibular anterior teeth.
At present, the process of root resorption is under intense study. As mentioned before, a force on a tooth leads to areas of compression and areas of tension. It is well known that the areas of compression experience a bone resorption process and the areas of tension experience bone apposition. Often times, on the compression side, blood vessels are compressed and areas of hyalinization arise. This hyalinization must be removed in order for the tooth to move. The removal of this area occurs through resorbing cells.[20,39]
The loss of root structure is a serious issue in orthodontic treatment however, it is important to note that most often the resultant loss is miniscule and does not affect the longevity of the teeth involved.[40] Accordingly, Remington found that mild to moderate shortening of the root length as a result of orthodontic therapy had no clinical significance.[5]
The magnitude of force utilized has been implicated as contributing to root resorption. Once again the results of previous studies are conflicting. Vardimon[41] noted that the higher the force utilized the greater amount of root resorption was noted. In contrast, Owman-Moll et al.[33,34] failed to find a significant relationship between these two variables. The result of the present study is in concert with the findings of Owman-Moll et al.[33,34] The Bidimensional technique did not have an increased amount of root resorption when compared to the Roth straight-wire system.
CONCLUSION
Within the limitations of this study, no significant differences between the bidimensional and the Roth straight-wire techniques were found in the amount of root resorption.
The etiology of root resorption is complex with a common occurrence during orthodontic treatment and the cause is difficult to identify. Furthermore, it is challenging to predict when root resorption will occur. A great responsibility is placed upon orthodontists to closely monitor their patients. Continued research this area is warranted.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: Part 1. Literature review. Am J Orthod Dentofacial Orthop. 1993;103:62–6. doi: 10.1016/0889-5406(93)70106-X. [DOI] [PubMed] [Google Scholar]
- 2.Weltman B, Vig KW, Fields HW, Shanker S, Kaizar EE. Root resorption associated with orthodontic tooth movement: A systematic review. Am J Orthod Dentofacial Orthop. 2010;137:462–76. doi: 10.1016/j.ajodo.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 3.DeShields RW. A study of root resorption in treated Class II, Division I malocclusions. Angle Orthod. 1969;39:231–45. doi: 10.1043/0003-3219(1969)039<0231:ASORRI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: Part 2. Literature review. Am J Orthod Dentofacial Orthop. 1993;103:138–46. doi: 10.1016/S0889-5406(05)81763-9. [DOI] [PubMed] [Google Scholar]
- 5.Remington DN, Joondeph DR, Artun J, Riedel RA, Chapko MK. Long-term evaluation of root resorption occurring during orthodontic treatment. Am J Orthod Dentofacial Orthop. 1989;96:43–6. doi: 10.1016/0889-5406(89)90227-8. [DOI] [PubMed] [Google Scholar]
- 6.Alexander SA. Levels of root resorption associated with continuous arch and sectional arch mechanics. Am J Orthod Dentofacial Orthop. 1996;110:321–4. doi: 10.1016/s0889-5406(96)80017-5. [DOI] [PubMed] [Google Scholar]
- 7.Beck BW, Harris EF. Apical root resorption in orthodontically treated subjects: Analysis of edgewise and light wire mechanics. Am J Orthod Dentofacial Orthop. 1994;105:350–61. doi: 10.1016/S0889-5406(94)70129-6. [DOI] [PubMed] [Google Scholar]
- 8.Copeland S, Green LJ. Root resorption in maxillary central incisors following active orthodontic treatment. Am J Orthod. 1986;89:51–5. doi: 10.1016/0002-9416(86)90111-9. [DOI] [PubMed] [Google Scholar]
- 9.Parker RJ, Harris EF. Directions of orthodontic tooth movements associated with external apical root resorption of the maxillary central incisor. Am J Orthod Dentofacial Orthop. 1998;114:677–83. doi: 10.1016/s0889-5406(98)70200-8. [DOI] [PubMed] [Google Scholar]
- 10.Linge BO, Linge L. Apical root resorption in upper anterior teeth. Eur J Orthod. 1983;5:173–83. doi: 10.1093/ejo/5.3.173. [DOI] [PubMed] [Google Scholar]
- 11.Linge L, Linge BO. Patient characteristics and treatment variables associated with apical root resorption during orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991;99:35–43. doi: 10.1016/S0889-5406(05)81678-6. [DOI] [PubMed] [Google Scholar]
- 12.Schudy FF, Schudy GF. The bimetric system. Am J Orthod. 1975;67:57–91. doi: 10.1016/0002-9416(75)90129-3. [DOI] [PubMed] [Google Scholar]
- 13.Gianelly AA, Bednar JR, Dietz VS. A bidimensional edgewise technique. J Clin Orthod. 1985;19:418–21. [PubMed] [Google Scholar]
- 14.Giancotti A, Gianelly AA. Three-dimensional control in extraction cases using a bidimensional approach. World J Orthod. 2001;2:168–76. [Google Scholar]
- 15.Giancotti A, Greco M. Modified sliding mechanics in extraction cases with a bidimensional approach. Prog Orthod. 2010;11:157–65. doi: 10.1016/j.pio.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Aljhani A, Zawawi KH. The use of mini-implants in en masse retraction for the treatment of bimaxillary dentoalveolar protrusion. Saudi Dent J. 2010;22:35–9. doi: 10.1016/j.sdentj.2009.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aljhani AS, Zawawi KH. Nonextraction treatment of severe crowding with the aid of corticotomy-assisted orthodontics. Case Rep Dent. 2012;2012:694527. doi: 10.1155/2012/694527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greco M, Giancotti A. Sliding mechanics in extraction cases with a bidimensional approach. Prog Orthod. 2007;8:144–55. [PubMed] [Google Scholar]
- 19.Goldie RS, King GJ. Root resorption and tooth movement in orthodontically treated, calcium-deficient, and lactating rats. Am J Orthod. 1984;85:424–30. doi: 10.1016/0002-9416(84)90163-5. [DOI] [PubMed] [Google Scholar]
- 20.Engström C, Granström G, Thilander B. Effect of orthodontic force on periodontal tissue metabolism. A histologic and biochemical study in normal and hypocalcemic young rats. Am J Orthod Dentofacial Orthop. 1988;93:486–95. doi: 10.1016/0889-5406(88)90077-7. [DOI] [PubMed] [Google Scholar]
- 21.Davidovitch Z, Krishnan V. Role of basic biological sciences in clinical orthodontics: A case series. Am J Orthod Dentofacial Orthop. 2009;135:222–31. doi: 10.1016/j.ajodo.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 22.Jung YH, Cho BH. External root resorption after orthodontic treatment: A study of contributing factors. Imaging Sci Dent. 2011;41:17–21. doi: 10.5624/isd.2011.41.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Newman WG. Possible etiologic factors in external root resorption. Am J Orthod. 1975;67:522–39. doi: 10.1016/0002-9416(75)90298-5. [DOI] [PubMed] [Google Scholar]
- 24.Levander E, Malmgren O. Evaluation of the risk of root resorption during orthodontic treatment: A study of upper incisors. Eur J Orthod. 1988;10:30–8. doi: 10.1093/ejo/10.1.30. [DOI] [PubMed] [Google Scholar]
- 25.Kjaer I. Morphological characteristics of dentitions developing excessive root resorption during orthodontic treatment. Eur J Orthod. 1995;17:25–34. doi: 10.1093/ejo/17.1.25. [DOI] [PubMed] [Google Scholar]
- 26.Lee RY, Artun J, Alonzo TA. Are dental anomalies risk factors for apical root resorption in orthodontic patients.? Am J Orthod Dentofacial Orthop. 1999;116:187–95. doi: 10.1016/s0889-5406(99)70217-9. [DOI] [PubMed] [Google Scholar]
- 27.Sameshima GT, Sinclair PM. Predicting and preventing root resorption: Part II. Treatment factors. Am J Orthod Dentofacial Orthop. 2001;119:511–5. doi: 10.1067/mod.2001.113410. [DOI] [PubMed] [Google Scholar]
- 28.Sameshima GT, Sinclair PM. Predicting and preventing root resorption: Part I. Diagnostic factors. Am J Orthod Dentofacial Orthop. 2001;119:505–10. doi: 10.1067/mod.2001.113409. [DOI] [PubMed] [Google Scholar]
- 29.Malmgren O, Goldson L, Hill C, Orwin A, Petrini L, Lundberg M. Root resorption after orthodontic treatment of traumatized teeth. Am J Orthod. 1982;82:487–91. doi: 10.1016/0002-9416(82)90317-7. [DOI] [PubMed] [Google Scholar]
- 30.McFadden WM, Engstrom C, Engstrom H, Anholm JM. A study of the relationship between incisor intrusion and root shortening. Am J Orthod Dentofacial Orthop. 1989;96:390–6. doi: 10.1016/0889-5406(89)90323-5. [DOI] [PubMed] [Google Scholar]
- 31.Reitan K. Initial tissue behavior during apical root resorption. Angle Orthod. 1974;44:68–82. doi: 10.1043/0003-3219(1974)044<0068:ITBDAR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 32.Dermaut LR, De Munck A. Apical root resorption of upper incisors caused by intrusive tooth movement: A radiographic study. Am J Orthod Dentofacial Orthop. 1986;90:321–6. doi: 10.1016/0889-5406(86)90088-0. [DOI] [PubMed] [Google Scholar]
- 33.Owman-Moll P, Kurol J, Lundgren D. Effects of a doubled orthodontic force magnitude on tooth movement and root resorptions. An inter-individual study in adolescents. Eur J Orthod. 1996;18:141–50. doi: 10.1093/ejo/18.2.141. [DOI] [PubMed] [Google Scholar]
- 34.Owman-Moll P, Kurol J, Lundgren D. The effects of a four-fold increased orthodontic force magnitude on tooth movement and root resorptions. An intra-individual study in adolescents. Eur J Orthod. 1996;18:287–94. doi: 10.1093/ejo/18.3.287. [DOI] [PubMed] [Google Scholar]
- 35.Afify AR, Zawawi KH, Othman HI. External apical root resorption following cervical traction headgear. Life Sci J. 2014;2014:39–43. [Google Scholar]
- 36.Janson GR, De Luca Canto G, Martins DR, Henriques JF, De Freitas MR. A radiographic comparison of apical root resorption after orthodontic treatment with 3 different fixed appliance techniques. Am J Orthod Dentofacial Orthop. 2000;118:262–73. doi: 10.1067/mod.2000.99136. [DOI] [PubMed] [Google Scholar]
- 37.Mavragani M, Vergari A, Selliseth NJ, Bøe OE, Wisth PL. A radiographic comparison of apical root resorption after orthodontic treatment with a standard edgewise and a straight-wire edgewise technique. Eur J Orthod. 2000;22:665–74. doi: 10.1093/ejo/22.6.665. [DOI] [PubMed] [Google Scholar]
- 38.McNab S, Battistutta D, Taverne A, Symons AL. External apical root resorption following orthodontic treatment. Angle Orthod. 2000;70:227–32. doi: 10.1043/0003-3219(2000)070<0227:EARRFO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 39.Proffit WR, Fields HW, Sarver DM. Contemporary Orthodontics. 4th ed. St. Louis, Mo: Mosby Elsevier; 2007. [Google Scholar]
- 40.Hollender L, Rönnerman A, Thilander B. Root resorption, marginal bone support and clinical crown length in orthodontically treated patients. Eur J Orthod. 1980;2:197–205. doi: 10.1093/ejo/2.4.197-a. [DOI] [PubMed] [Google Scholar]
- 41.Vardimon AD, Graber TM, Voss LR, Lenke J. Determinants controlling iatrogenic external root resorption and repair during and after palatal expansion. Angle Orthod. 1991;61:113–22. doi: 10.1043/0003-3219(1991)061<0113:DCIERR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]


