Abstract
Objectives:
This study aimed to outline orthodontists’ perspectives at what stage they would initiate orthodontic treatment and also sought to assess the relationship between orthodontists’ views and their genders, types of practice, and experience levels.
Materials and Methods:
A questionnaire was sent electronically to 165 practicing orthodontists at different regions in Saudi Arabia. The orthodontists were asked to consider at what stage they would initiate orthodontic treatment for a child with one of 29 different types of occlusal deviations, functional problems, and temporomandibular disorders (TMDs) listed in the questionnaire as their main orthodontic problem. Frequency distributions of all the variables were derived, and comparisons were made using the Chi-square tests.
Results:
Fifty-two electronically completed questionnaires were returned (31.5% response rate). The majority of the respondents were males (63.5%). The majority of respondents (90%) reported that they would treat most of the occlusal deviations in the mixed dentition stage. Anterior cross-bite was the most frequent indication for treatment during the early mixed dentition stage (73.7%). Conditions rated as best treated during the late mixed, or the permanent dentition stages were; overjet > 6 mm with interdental spacing, maxillary midline diastema >2 mm and deep bite >5 mm without palatal impingement. The majority of respondents (86.6%) preferred to treat most of the functional problems in the deciduous or early mixed dentition stage. Orthodontists with more than 15 years of experience preferred to treat patients with TMDs, whereas those with <15 years of experience opted to refer such patients to TMD specialists.
Conclusions:
The findings of the present study suggest that orthodontists should consider many factors, such as the risks, benefits, duration, and costs of early and late intervention, when deciding the best timing to begin orthodontic treatment.
Keywords: Early, late, mixed dentition stage, one-phase treatment, orthodontic treatment, timing, two-phase
INTRODUCTION
Controversies about determining the appropriate timing of orthodontic treatment are significant among orthodontists. Many studies have investigated, discussed and compared early versus late treatment.[1,2,3] Moreover, the definition of early treatment is also controversial. Some clinicians consider treatment to be early if it is started in the primary or early mixed (permanent first molars and incisors present) dentition stage.[2,4] Others define treatment as early if it is started in the late mixed dentition stage (before the eruption of second bicuspids and permanent upper canines).[5,6] Part of the controversy is centered around whether to initiate treatment in the deciduous or early mixed dentition stage as a two-phase treatment or to start treatment in the late mixed dentition or permanent dentition stage as a one-phase treatment.
Some orthodontists advocate early orthodontic treatment in particular types of malocclusion, such as functional crossbite,[7,8] dental habits,[9,10] severe crowding with increased overjet,[7,8] and Class III malocclusion with maxillary deficiency.[9] Others prefer to start orthodontic treatment of some malocclusions, such as Class II, at the late mixed dentition stage as a one-phase of treatment.[10,11,12] Those orthodontists advocating early treatment believe that the early correction of specific dental and skeletal discrepancies at the deciduous or early mixed dentition stages has several benefits. First, this treatment method takes advantage of normal growth to modify skeletal growth and corrects the malocclusion;[13,14] it reduces the time needed for phase II treatment and the severity of the malocclusion;[8,15] it has better and more stable results;[1,14] it improves patient self-esteem and parental satisfaction; it reduces the potential for iatrogenic tooth damage, such as trauma to susceptible incisors, root resorption, and decalcification;[14] and finally, it is associated with greater patient compliance among preadolescent children, as they tend to be more adherent to treatment instructions.[16,17] Orthodontists who prefer late treatment have argued that early treatment at deciduous or early mixed dentition has no long-term benefits,[10] whereas the advantages of one-phase orthodontic treatment have been shown. One-phase treatment takes advantage of the sufficient remaining growth,[1] avoids patient/parent burnout due to lengthy two-phase treatment,[2,6] avoids unpredictable growth dynamics that can occur at the preadolescent ages,[17] and finally, one-phase is lower cost than two-phase treatment.[10]
Many orthodontists recommend that occlusion assessment be carried out before 7 years of age to determine whether to start the treatment early or later.[4] Kerosuo et al. 2008[18] recommended intervention in the early mixed dentition stage in cases of crossbite, increased overjet, deepbite with palatal impingement and severe crowding. Similar findings have been reported by many researchers.[7,8] The differences in the preferred timing of treatment for specific malocclusion have been reported among orthodontists in different countries as noted by Kiyak et al. 2004.[19] He studied orthodontists’ views on the timing of treatment for different skeletal and dental deviations in three countries: Italy, Turkey, and United States (US). Kiyak et al. found that orthodontists in Italy preferred two-phase treatment for increased overjets and severe crowding, as opposed to those in the US and Turkey, who recommended one-phase treatment. Most of the orthodontists in these three countries agreed that it was preferable to treat particular malocclusions, such as an anterior crossbite and severe arch constriction, during the primary or early mixed dentition stage.[19]
Researchers have not established the preferred timing of treatment for Class II malocclusions, and it remains an issue of controversy. Many orthodontists reported that Class II malocclusion with or without crowding can be treated successfully in only one phase during the late mixed dentition stage at puberty.[12,20,21] In contrast, Class II malocclusion is considered the most common indication for starting early orthodontic treatment in Finland.[4,8,22] When early orthodontic treatment is contemplated, every orthodontist should ask several questions: Do the benefits of early intervention justify the extra cost, time, and energy involved in two-phase treatment, and does early treatment eliminate or reduce the need for another orthodontic treatment at a later stage?
The purpose of the present study was to analyze the perspective of orthodontists practicing in Saudi Arabia regarding the ideal time to initiate treatment. This research also sought to assess the relationship between orthodontists’ views and their genders, types of practice, and years of experience.
MATERIALS AND METHODS
A cross-sectional survey was conducted by sending questionnaires electronically to 165 practicing orthodontists in different regions of Saudi Arabia. An explanation of the purpose of the study and the research procedure was included. The orthodontists were asked to voluntarily complete the anonymous questionnaire. The names of the orthodontists were obtained from the directory of the Saudi Dental Society and the Saudi Orthodontic Society. The first section recorded demographic details, including gender, length of time in practice, location of orthodontic training program attended, and the type of practice. In addition, the respondents were asked to report the proportion of patients of different ages treated (i.e. 6-8, 8-11, 12-18, and older than 18 years) and the proportion of conventional versus surgical orthodontic treatments rendered in their practices. The second section of the questionnaire comprised a list of 29 types of occlusal deviations, functional problems, and temporomandibular disorders (TMDs) [Appendix], which were selected from the previous questionnaire that was distributed to orthodontists throughout the US.[19]
The original questionnaire included a list of the most common malocclusions, which were obtained from the existing literature and textbooks. The list was revised and refined by three faculty members in the Department of Orthodontics at the University of Washington Dental School and four orthodontists in private practices around the country. The final list included 41 types of malocclusions; some of these distinguished between male and female patients and others specified the extent of deviation (e.g. different overjet) or described side-effects of the deviation (e.g. occurrence of attrition or periodontal concerns).[19] In the present study, the orthodontists were asked to consider at what stage they would most likely initiate orthodontic treatment for a child who had one of the types of occlusal deviations, functional problems, and TMDs listed in the questionnaire as their main orthodontic problem. They were also asked to rate their responses on a scale of X (no treatment needed) to 5 (treatment in the adult dentition) [Appendix]. Ethical approval of the study was obtained from the Ethical Committee of College of Dentistry Research Center at King Saud University. The survey was sent in May 2013 and the last response was received in August 2013.
Statistical Analysis
The data were tabulated and crosschecked. Data processing and analysis were carried out using the Statistical Package Software System (version 21, SPSS Inc., Chicago, IL, USA). Frequency distributions and descriptive statistics for gender, length of time in practice, type of practice, patient age range treated in the practice, and the treatment type was generated. In addition, the frequency of treatment for each occlusal deviation, functional problem, and TMDs at each specific stage was determined. Group comparisons (for gender, practice experience, and patient age range treated in the practice) were performed with Chi-square tests of association for each occlusal deviation, functional problem, and TMDs. Statistical significance was considered when P < 0.05.
RESULTS
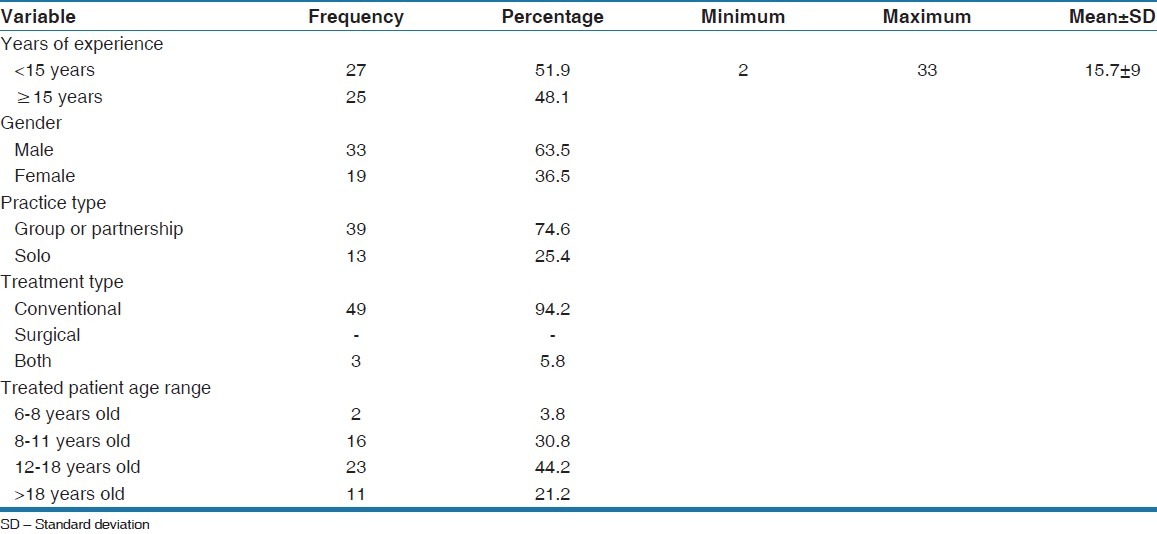
Fifty-two electronically completed questionnaires were returned (31.5% response rate). Thirty-three of the respondents were males (63.5%) working in group or partnership practices (74.6%) rather than solo practices (25.4%), and who were treating patients with conventional orthodontics (94.2%) rather than surgical orthodontics or both (5.8%). The percentage of orthodontists treating their patients in the adolescent age range (12-18-year-old) was higher (44.2%) than other age ranges, followed by children aged 8-11 (30.8%) and adults older than 18 years (21.2%). The lowest percentage was young children aged 6-8 (3.8%) [Table 1]. The mean years of experience among the respondents was 15.7 (±9), with a range of 2-33 years [Table 1]. The respondents represented different orthodontic programs throughout the US, Europe, and Saudi Arabia.
Table 1.
Frequency distributions and descriptive statistics for gender, length of time in practice, type of practice, patient age range treated in the practice, and the treatment type
The majority of respondents (90%) reported that they would treat most of the occlusal deviations in the mixed dentition stage. They preferred treatments of 13 conditions in the early mixed dentition stage, eight conditions in the late mixed dentition stage, and three conditions in either stage. Four conditions were rated as best treated in either the late mixed or the permanent dentition stage. These were overjet >6 mm with interdental spacing (44.2% in each stage); maxillary midline diastema >2 mm (36.5% and 57.7%, respectively); deepbite >5 mm without palatal impingement (54.2% and 36.2%, respectively); and congenitally missing permanent teeth (57.7 and 34.6%, respectively). Of the 29 occlusal deviations, the majority of orthodontists agreed that only one condition, that is, mandibular prognathism, was best treated during the adult dentition stage (55.8%). [Tables 2 and 3] respectively summarize the occlusal deviations rated as best treated in the early and late mixed dentition stages.
Table 2.
The most frequent occlusal deviations to be treated in the early mixed dentition stage (n=52)
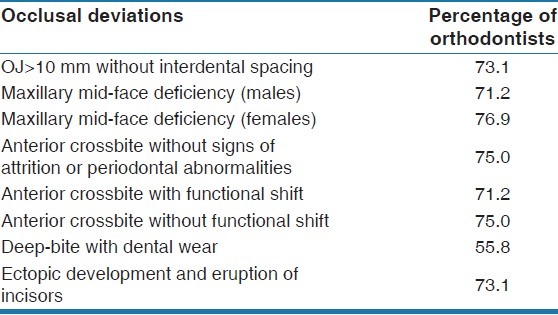
Table 3.
The most frequent occlusal deviations to be treated in the late mixed dentition stage (n=52)
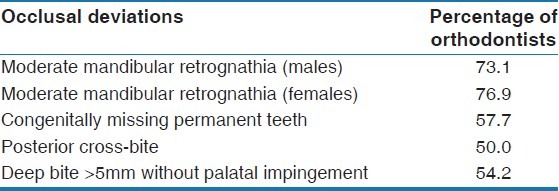
The condition of moderate mandibular retrognathia among males and females orthodontists was considered best treated during the late mixed dentition stage (73.1% and 76.9%, respectively). The majority of respondents stated that anterior crossbite (without obvious signs of attrition or periodontal abnormalities, with and without functional shift) was the most frequent indication for treatment during the early mixed dentition stage (75%, 71.2% and 75%, respectively). The conditions of posterior crossbite, obvious skeletal openbite >−1 mm, and severe crowding in maxillary or mandibular arch with significant esthetic concerns were most likely to be treated in either the early or late mixed dentition stage (46.2% and 50%, 48.1% in each stage; 51.9% and 48.1%, respectively). More than half of the respondents preferred to treat deepbite with dental wear and ectopic development and eruption of incisors in the early mixed dentition stage (55.8% and 73.1%, respectively).
The majority of respondents preferred to treat most of the functional problems in the deciduous or early mixed dentition stage (86.6%). Seventy-five percentage of orthodontists said they would treat thumb-sucking problems in the early mixed dentition stage whereas 23.1% would treat this condition in the deciduous dentition stage. Furthermore, any malocclusion leading to speech disorder would be treated in the early mixed dentition stage (55.8%) followed by the deciduous dentition stage (30.8%). More than half of the respondents selected to refer most TMD cases to specialists (53.8%). However, the remaining respondents preferred to treat TMDs problems in the permanent dentition stage (40.4%).
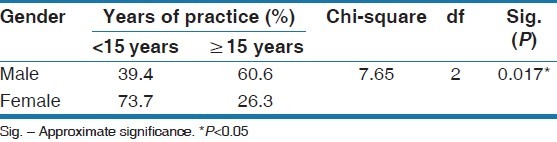
Chi-square analysis was performed to test the association of treatment timing with the participants’ genders, lengths of time in practice, and range of patients’ age treated in their respective practices. The results showed that there was a significant difference in the years of practice between male and female orthodontists where 60.6% of males had practiced more than 15 years compared with 26.3% of females (χ2 = 7.65; P < 0.05) [Table 4].
Table 4.
Chi-square test to compare between orthodontists’ gender and years of practice
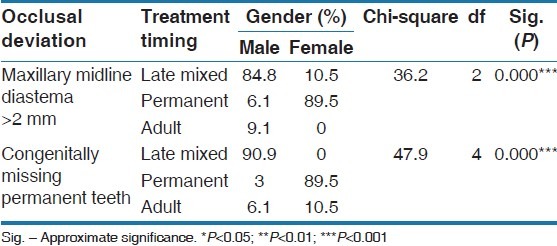
The result also indicated that, no significant difference between the years of practice among males and females and the proportion of patients of different ages treated in their practices (χ2df = 3 = 4.1; P = 0.25). In addition, there was no significant difference between the types of practices (solo or group practice) and the proportions of patients of different ages treated in the practices (χ2df = 6 = 9.8; P = 0.13). Chi-square tests also showed that orthodontists with more than 15 years of experience preferred to treat obvious skeletal openbite >−1 mm and severe crowding in maxillary or mandibular arch with significant esthetic concerns in the late mixed dentition stage, whereas less experienced orthodontists preferred to treat these two conditions in the early mixed dentition stage (χ2 = 40 and χ2 = 52, respectively; P ≤ 0.001) [Table 5]. Moreover, male orthodontists were more likely to initiate treatment of maxillary midline diastema > 2 mm and congenitally missing permanent teeth in the late mixed dentition, whereas female orthodontists preferred to treat these conditions in the permanent dentition stage (χ2 = 36.2 and χ2 = 47.9, respectively, P < 0.001) [Table 6].
Table 5.
Chi-square test of association for treatment timing of different occlusal deviations and orthodontists’ years of practice
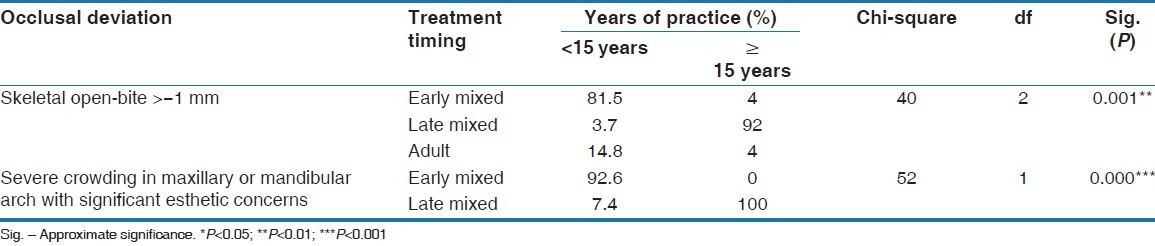
Table 6.
Chi-square test of association for treatment timing of different occlusal deviations and orthodontists’ gender
In cases with mandibular prognathism, the orthodontists with greater numbers of younger patients were more likely to treat this condition in the early mixed dentition stage. On the other hand, orthodontists with more adolescent patients preferred to initiate orthodontic treatment in the late mixed or permanent dentition stage (χ2df = 6 = 45, P < 0.001). Finally, orthodontists with <15 years of experience tended to refer patients with TMDs to specialists and on the other hand, orthodontists with more than 15 years of experience preferred to treat patients with deviations in opening (χ2df = 3 = 48, P < 0.001) or spontaneous pain in the temporomandibular joint area (χ2df = 6 = 39.3, P < 0.001).
DISCUSSION
There is scarce information regarding the ideal timing to start orthodontic treatment among Saudi professionals. The present study has shed important information about the opinion of orthodontist on when to initiate orthodontic treatment in Saudi Arabia. In orthodontics, the decision of early or late treatment is most frequently based on professional choices for each child according to his or her needs rather than on evidence from sound clinical research.[2,6,23] Furthermore, orthodontists should consider several factors when making their clinical decision for either early or late orthodontic intervention. These factors include the risks, benefits, duration, and costs. The ideal orthodontic treatment should achieve the best outcome in the shortest time with the lowest cost.
The orthodontists who responded to this survey worked in several sectors, including public health facilities, hospitals, universities, and private practices. In addition, some of the respondents had received their orthodontic training in Saudi Arabia, whereas others had studied abroad in the US, UK, and Norway. A wide variety of workplaces and training programs in the present study could have increased the variation in the timing of treatment. In this study, the majority of the respondents recommended early treatment for most of the occlusal deviations. This is consistent with results of previous studies.[4,17] All types of anterior crossbite disorders described in the questionnaire were most likely to be treated during early mixed dentition. The same results were also reported by many researchers.[4,8,19] According to the respondents, mandibular retrognathia and increased overjet with interdental spacing were most appropriately treated in the late mixed dentition. This could be related to the fact that the treatment of such conditions at this age could enhance the growth of a retrognathic mandible, allow for utilization of the leeway space, and shorten the treatment time. However, true mandibular prognathism was frequently selected during the adult dentition as most appropriately treated surgically after the completion of growth.
In the present study, orthodontists’ generally favored early treatment for most of the functional habits, such as thumb sucking, mouth breathing, and tongue thrusting, which can contribute to unfavorable growth of the jaws and protruded upper anterior teeth, possibly leading to trauma and speech problems. The preference of early intervention in cases with functional problems could be due to the benefits of early treatment, which include improved facial profile, smile, speech, and self-esteem. Early treatment also reduces or eliminates the time required for the second phase of treatment. The results showed that the orthodontists with more younger-age patients tended to recommend early intervention more often than did orthodontists with a greater number of adolescent patients; these respondents preferred late intervention. Moreover, more experienced orthodontists preferred to treat patients with TMDs, whereas those with fewer years of experience tended not to initiate orthodontic treatment for most patients with TMDs and prefer to refer them to TMD specialists. This difference might be explained by the greater clinical experience obtained among the former group of orthodontists.
The results of the present study must be interpreted cautiously due to the small sample size and the study's survey data-collection method. The questionnaire did not include details about each condition. This highlights the need for further investigation with a larger sample size. Further, future research should also investigate factors other than the length of time in practice, training program completed, and type of practice that could affect the treatment timing decision. Furthermore, a longitudinal study is required to test the impact of the orthodontists’ decisions to initiate early or late treatments based on outcomes and cost-effectiveness.
CONCLUSION
The majority of respondents preferred to treat most of the occlusal deviations in the mixed dentition stage
Anterior crossbite was the most frequent indication for treatment during the early mixed dentition stage
The majority of respondents favored treating most of the functional problems in the deciduous or early mixed dentition stage
Orthodontists with more years of experience preferred to treat obvious skeletal openbite and severe crowding in both arches with significant esthetic concerns in the late mixed dentition, whereas less experienced orthodontists favored treatment of the two conditions in the early mixed dentition stage
More experienced orthodontists preferred to treat patients with TMDs, whereas those with fewer years of experience tended not to initiate orthodontic treatment for most patients with TMDs or prefer to refer them to TMD specialists.
ACKNOWLEDGMENT
The author is grateful to the Saudi Dental Society and the Saudi Orthodontic Society for their cooperation and assistance sending the questionnaires electronically to all their members. The author would also like to thank all the orthodontists for participating in this study.
APPENDIX
For each condition below, please circle the number that represents the stage when you would most likely want to initiate orthodontic treatment for a child who has one of these conditions listed below as their primary orthodontic problem.
**Response scale for each question: X 1 2 3 4 5
Where: X=No treatment needed
1=Deciduous dentition (4-6 years).
2=Early mixed dentition
3=Late mixed dentition.
4=Permanent dentition
5=Adult dentition (16+years).
A. Occlusal deviations
-
Moderate mandibular retrognathia
-
MalesFemales
-
-
Overjet
-
(a)>6 mm with interdental spacing
-
(b)>10 mm without interdental spacing
-
(a)
-
Moderate maxillary retrognathia (Maxillary mid-face deficiency)
-
(a)Males
-
(b)Females
-
(a)
Mandibular prognathism
Maxillary midline diastema >2 mm
-
Anterior crossbite (at least one tooth in crossbite)
-
(a)Without obvious signs of attrition or periodontal abnormalities
-
(b)With functional shift
-
(c)Without functional shift
-
(a)
Severe upper arch constriction (with posterior crossbite)
Posterior crossbite (more than one tooth in crossbite)
Posterior scissor-bite (at least one tooth in reverse crossbite)
Midline discrepancies>2 mm (without posterior crossbite)
Obvious skeletal openbite >-1 mm
-
Apparent dental openbite >-1 mm
-
(a)Without oral habit
-
(b)With apparent contributing oral habit
-
(a)
-
Deepbite >5 mm
-
(a)Without palatal impingement
-
(b)With dental wear
-
(a)
Moderate crowding in maxillary or mandibular arch
-
Severe crowding in maxillary or mandibular arch
-
(a)Significant esthetic concerns
-
(b)Significant dental asymmetries
-
(c)Excessive gingival display with smiling
-
(a)
-
Missing permanent teeth
-
(a)Congenitally missing
-
(b)Ankylosed primary teeth with permanent teeth missing
-
(a)
Ectopic development and eruption (incisors)
Conditions with potential for resorption of roots of permanent teeth (e.g. central, lateral and cuspids)
Supernumerary teeth (found clinically or on X-ray)
B. Functional concerns
Faulty position of lower lip
Mouth breathing
Tongue posture abnormality and swallowing problems
Thumb/finger sucking
Speech disorders
C. Signs and symptoms of temporomandibular disorder
TMJ-sounds
Deviations in opening
Spontaneous pain in the TMJ area (reported by patient)
Limitation in maximal opening
Bruxism
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Jang JC, Fields HW, Vig KW, Beck FM. Controversies in the timing of orthodontic treatment. Semin Orthod. 2005;11:112–18. [Google Scholar]
- 2.Hsieh TJ, Pinskaya Y, Roberts WE. Assessment of orthodontic treatment outcomes: Early treatment versus late treatment. Angle Orthod. 2005;75:162–70. doi: 10.1043/0003-3219(2005)075<0158:AOOTOE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Pietilä I, Pietilä T, Svedström-Oristo AL, Varrela J, Alanen P. Acceptability of adolescents’ occlusion in Finnish municipal health centres with differing timing of orthodontic treatment. Eur J Orthod. 2010;32:186–92. doi: 10.1093/ejo/cjp085. [DOI] [PubMed] [Google Scholar]
- 4.Pietilä I, Pietilä T, Pirttiniemi P, Varrela J, Alanen P. Orthodontists’ views on indications for and timing of orthodontic treatment in Finnish public oral health care. Eur J Orthod. 2008;30:46–51. doi: 10.1093/ejo/cjm085. [DOI] [PubMed] [Google Scholar]
- 5.Ghafari J, Shofer FS, Jacobsson-Hunt U, Markowitz DL, Laster LL. Headgear versus function regulator in the early treatment of Class II, division 1 malocclusion: A randomized clinical trial. Am J Orthod Dentofacial Orthop. 1998;113:51–61. doi: 10.1016/s0889-5406(98)70276-8. [DOI] [PubMed] [Google Scholar]
- 6.Tulloch JF, Proffit WR, Phillips C. Outcomes in a 2-phase randomized clinical trial of early Class II treatment. Am J Orthod Dentofacial Orthop. 2004;125:657–67. doi: 10.1016/j.ajodo.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Tausche E, Luck O, Harzer W. Prevalence of malocclusions in the early mixed dentition and orthodontic treatment need. Eur J Orthod. 2004;26:237–44. doi: 10.1093/ejo/26.3.237. [DOI] [PubMed] [Google Scholar]
- 8.Väkiparta MK, Kerosuo HM, Nyström ME, Heikinheimo KA. Orthodontic treatment need from eight to 12 years of age in an early treatment oriented public health care system: A prospective study. Angle Orthod. 2005;75:344–9. doi: 10.1043/0003-3219(2005)75[344:OTNFET]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Viazis AD. Efficient orthodontic treatment timing. Am J Orthod Dentofacial Orthop. 1995;108:560–1. doi: 10.1016/s0889-5406(95)70058-7. [DOI] [PubMed] [Google Scholar]
- 10.Gianelly AA. One-phase versus two-phase treatment. Am J Orthod Dentofacial Orthop. 1995;108:556–9. doi: 10.1016/s0889-5406(95)70057-9. [DOI] [PubMed] [Google Scholar]
- 11.von Bremen J, Pancherz H. Efficiency of early and late Class II Division 1 treatment. Am J Orthod Dentofacial Orthop. 2002;121:31–7. doi: 10.1067/mod.2002.120016. [DOI] [PubMed] [Google Scholar]
- 12.Franchi L, Pavoni C, Faltin K, Jr, McNamara JA, Jr, Cozza P. Re: Response to: Long-term skeletal and dental effects and treatment timing for functional appliances in Class II malocclusion. The Angle Orthodontist 2013 (2) 334-340. Angle Orthod. 2013;83:933. doi: 10.2319/052912-450.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moyers RE. Handbook of Orthodontics. 4th ed. Chicago: Year Book Medical Publisher; 1988. pp. 433–34.pp. 346–47. [Google Scholar]
- 14.Bishara SE, Justus R, Graber TM. Proceedings of the workshop discussions on early treatment. Am J Orthod Dentofacial Orthop. 1998;113:5–6. [Google Scholar]
- 15.Mirabelli JT, Huang GJ, Siu CH, King GJ, Omnell L. The effectiveness of phase I orthodontic treatment in a Medicaid population. Am J Orthod Dentofacial Orthop. 2005;127:592–8. doi: 10.1016/j.ajodo.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 16.Cureton SL, Regennitter FJ, Yancey JM. Clinical versus quantitative assessment of headgear compliance. Am J Orthod Dentofacial Orthop. 1993;104:277–84. doi: 10.1016/S0889-5406(05)81731-7. [DOI] [PubMed] [Google Scholar]
- 17.Yang EY, Kiyak HA. Orthodontic treatment timing: A survey of orthodontists. Am J Orthod Dentofacial Orthop. 1998;113:96–103. doi: 10.1016/S0889-5406(98)70281-1. [DOI] [PubMed] [Google Scholar]
- 18.Kerosuo H, Väkiparta M, Nyström M, Heikinheimo K. The seven-year outcome of an early orthodontic treatment strategy. J Dent Res. 2008;87:584–8. doi: 10.1177/154405910808700604. [DOI] [PubMed] [Google Scholar]
- 19.Kiyak HA, Haluk I, Miotti FA. Orthodontists’ perspectives regarding treatment timing: A cross-national study. World J Orthod. 2004;5:40–7. [PubMed] [Google Scholar]
- 20.Dolce C, McGorray SP, Brazeau L, King GJ, Wheeler TT. Timing of Class II treatment: Skeletal changes comparing 1-phase and 2-phase treatment. Am J Orthod Dentofacial Orthop. 2007;132:481–9. doi: 10.1016/j.ajodo.2005.08.046. [DOI] [PubMed] [Google Scholar]
- 21.Baccetti T, Franchi L, Kim LH. Effect of timing on the outcomes of 1-phase nonextraction therapy of Class II malocclusion. Am J Orthod Dentofacial Orthop. 2009;136:501–9. doi: 10.1016/j.ajodo.2007.08.029. [DOI] [PubMed] [Google Scholar]
- 22.Keski-Nisula K, Lehto R, Lusa V, Keski-Nisula L, Varrela J. Occurrence of malocclusion and need of orthodontic treatment in early mixed dentition. Am J Orthod Dentofacial Orthop. 2003;124:631–8. doi: 10.1016/j.ajodo.2003.02.001. [DOI] [PubMed] [Google Scholar]
- 23.Shaw WC, Turbill EA. In: Public health aspects of oral diseases and disorders – dentofacial irregularities. Pine C, Harris R, editors. Berlin: Community Oral Health Quintessence Publishing Co. Ltd; 2007. pp. 227–37. [Google Scholar]


