ABSTRACT
BACKGROUND
Little is known regarding the prevalence or risk factors for non-comprehension and non-compliance with discharge instructions among older adults.
OBJECTIVE
To quantify the prevalence of non-comprehension and non-compliance with discharge instructions and to identify associated patient characteristics.
RESEARCH DESIGN
Prospective cohort study.
SUBJECTS
Four hundred and fifty adults aged ≥ 65 admitted to medical and surgical units of a tertiary care facility and meeting inclusion criteria.
MEASURES
We collected information on demographics, psycho-social factors, discharge diagnoses, and medications using surveys and patient medical records. Domains within discharge instructions included medications, follow-up appointments, diet, and exercise. At 5 days post-discharge, we assessed comprehension by asking patients about their discharge instructions, and compared responses to written instructions from medical charts. We assessed compliance among patients who understood their instructions.
RESULTS
Prevalence of non-comprehension was 5 % for follow-up appointments, 27 % for medications, 48 % for exercise and 50 % for diet recommendations. Age was associated with non-comprehension of medication [odds ratio (OR) 1.07; 95 % confidence interval (CI) 1.04, 1.12] and follow-up appointment (OR 1.08; 95 % CI 1.00, 1.17) instructions. Male sex was associated with non-comprehension of diet instructions (OR 1.91; 95 % CI 1.10, 3.31). Social isolation was associated with non-comprehension of exercise instructions (OR 9.42; 95 % CI 1.50, 59.11) Depression was associated with non-compliance with medication (OR 2.29; 95 % CI 1.02, 5.10) and diet instructions (OR 3.30; 95 % CI 1.24, 8.83).
CONCLUSIONS
Non-comprehension of discharge instructions among older adults is prevalent, multi-factorial, and varies by domain.
KEY WORDS: hospital discharge instructions, older adults, comprehension, compliance
INTRODUCTION
Discharge instructions communicate important medical information to help patients manage their own care when they leave the hospital. Nonetheless, patients do not always understand these instructions.1–8 Non-comprehension of the discharge instructions is associated with decreased compliance and could lead to poor health outcomes.1,9
Previous studies that have assessed patient comprehension of the discharge instructions have been primarily conducted in emergency departments and have not focused on older adults, who represent a disproportionate share of healthcare users.3,4,6,9–11 Furthermore, increased complexity of the discharge instructions due to a greater burden of comorbid illnesses and higher prevalence of cognitive impairment among older adults may result in an elevated risk of non-comprehension.1,2,12–14
In this study, we determined the prevalence of non-comprehension of the discharge instructions and identified patient characteristics associated with non-comprehension among older adults discharged from the medical and surgical units of a large urban hospital. As a secondary analysis, we assessed the prevalence of non-compliance with the discharge instructions and analyzed factors associated with non-compliance among study participants who understood their discharge instructions.
METHODS
Study Design and Study Population
We conducted a prospective cohort study of community-dwelling adults aged 65 and older admitted to general medical and surgical services of the University of Maryland Medical Center (UMMC) between 1 July 2011 and 9 August 2012.15 UMMC is a 757-bed tertiary-care hospital in Baltimore, MD. Eligible patients were enrolled in their hospital rooms within 72 hours of hospital admission and followed up by telephone at 5 days post-hospital discharge. Patients admitted to psychiatric, obstetrical, and intensive care units, residing in a nursing home, unable to communicate in English, or with a Mini-Mental State Examination (MMSE) score of less than 15 were excluded from the study.16
Baseline Measures
We administered a baseline questionnaire to study participants within 72 hours of hospital admission. Along with demographic information, we measured depressive symptoms using the 15-item Geriatric Depression Scale (GDS), and defined clinically important depressive symptoms as a score of 6 or greater.17,18 This cut-point has been observed to have a sensitivity of 83 % and a specificity of 69 % to detect depression in elderly inpatients.18 We measured disability in Katz’s Activities of Daily Living (range 0–5 with 0 indicating highest functioning), cognitive impairment using the Mini-Mental State Examination (MMSE) (range 0–30), and social isolation with the six-item Lubben Social Network Scale (LSNS-6).17,19,20 A cut-point of less than 12 on the LSNS-6 has been suggested to define social isolation and was used in this study.20 Baseline interviews were conducted by two trained interviewers (J.S.A. and J.H.R.).
We collected data on admission and discharge diagnoses (including both the primary diagnosis and up to 15 comorbid medical conditions), number of medications prescribed at discharge, discharge instructions, and hospital readmissions to UMMC from patients’ medical charts. At UMMC, a nurse or doctor explains the written discharge instructions to the patient prior to hospital discharge. The patient is given the opportunity to ask questions, and then signs a copy of the written discharge instructions. This signed copy is maintained in the patient’s medical record and another copy is sent home with the patient. Patients who are discharged to a skilled nursing facility (SNF) don’t receive discharge instructions. Rather, the discharge summary is sent to the next location of care. In this study, we defined patient receipt of discharge instructions by the presence of a signed receipt of discharge instructions form in the patients’ charts.
We used the UMMC Clinical Data Repository (CDR) to collect data on the Charlson Comorbidity Index score, home medications, and new medications prescribed at discharge.21 Data in the CDR have been validated against patients’ paper medical charts and have demonstrated predictive values exceeding 99 %.22,23 To determine whether home medications were continued, we abstracted medication information from patient discharge summaries.
We created disease categories based on patient discharge diagnosis International Classification of Diseases, Ninth Revision (ICD-9) codes.24,25 The following categories, representing the most common discharge diagnoses, were created: cancer (140-208, 230-234), heart disease (391-392.0, 393,-398, 402, 404, 410-416, 420-429), diseases of the digestive system (520-579), diseases of the musculoskeletal system (710-739), and complications of surgical and medical care (996-999). The remaining diagnoses were grouped as ‘other.’
Assessment of Comprehension at 5 Days Post-Hospital Discharge
The Joint Commission on Accreditation of Healthcare Organizations recommends that hospitals provide written instructions covering six categories (activity, diet, weight, follow-up appointments, discharge medications, and worsening symptoms) to all patients with a diagnosis of heart failure, and many hospitals provide this information to all patients.26,27
We included four of these categories as domains in our discharge instructions outcome variable: medications, follow-up appointments, diet, and exercise. Weight and worsening symptoms were not included because they are conditional on changes in status that may not have occurred during the study period. Our focus was patient comprehension of the written discharge instructions; therefore, we included only patients to whom we spoke directly (no proxy responses) at the 5-day follow-up call and who had documented receipt of discharge instructions in the medical record. All follow-up calls were conducted by a single trained interviewer (J.S.A.). We used the written discharge instructions from patient medical records as the ‘gold standard’ against which patient responses were compared. Concordance with the written discharge instructions indicated comprehension. Patients not receiving written instructions in a particular domain were not evaluated for that domain.
To assess comprehension of medication instructions, we asked patients: 1) if they were prescribed any new medications at discharge, and 2) if they were told to continue taking medications they had been taking prior to hospitalization. Responses were yes/no. Patients were not prompted with names of medications, nor were they asked to provide specific information regarding medications. Patients who correctly answered both questions were considered to ‘comprehend’ the medication instructions. A single incorrect answer or not knowing about new or continued medications indicated non-comprehension.
To assess comprehension of follow-up appointment instructions, we asked patients: 1) if they were told to schedule a follow-up appointment post-hospital discharge, and 2) if the hospital scheduled a follow-up appointment for them. Responses were yes/no. Patients were not asked to identify the date or location of the follow-up appointment, but were considered to ‘comprehend’ if they correctly answered both questions. Diet comprehension was assessed by asking if patients were told to follow a specific diet at hospital discharge. Examples of recommended diets such as a diabetic, heart healthy, low salt, or low fat diet were provided to prompt patients. The response was yes/no, and patients were required to correctly answer to ‘comprehend’. We did not base comprehension on recall of the specific diet. Patients whose ‘regular’ diet was diabetic or another special type always received written diet instructions. Exercise comprehension was assessed by asking if patients were told to engage in any physical activity at hospital discharge. Prompts of physical therapy and walking were provided, but the response was yes/no. We did not ask about physical activity limitations. We did not base comprehension on recall of the specific type of exercise.
Assessment of Compliance at 5 Days Post-Hospital Discharge
In this study, only patients who reported receiving instructions in a particular domain were asked follow-up compliance questions. For example, if a patient responded that they were not given diet instructions, we did not ask about diet compliance. We assessed compliance only among study participants who understood their discharge instructions for each domain. Compliance measures were based on patient self-report. General medication compliance was assessed by asking about prescription fills, and by using the four-item Morisky Medication Adherence Scale.28 The Morisky Medication Adherence Scale measures medication adherence by asking the following questions: (thinking about all medication that you take) Do you ever forget to take your medicine?; Are you careless at times about taking your medicine?; When you feel better, do you sometimes stop taking your medicine?; When you feel worse, do you sometimes stop taking your medicine?.28 To be considered compliant, patients had to report filling new prescriptions and answer ‘no’ to three out of the four questions on the Morisky scale. Follow-up appointment compliance was based upon scheduling of and attendance at the appointment. Most participants who received instructions to schedule a follow-up appointment were told to follow up within two weeks; hence a patient who had not yet scheduled an appointment by 5-days post-discharge might still have been compliant. Therefore; in this study, participants who had not yet tried to schedule a follow-up appointment by the 5-day follow-up call were considered to be compliant. Compliance with diet instructions required following the diet every day, and compliance with exercise instructions required participating in the exercise at least three times per week.
Compliance information was not collected if a death or unplanned readmission event occurred prior to the 5-day follow-up call. Participants unable to communicate or who did not direct their own medical care (including medications, appointments, or diet) were excluded from these analyses.
Data Analysis
We assessed the association of demographic, clinical, and psychosocial covariates with both the comprehension and compliance measures in all domains using chi-square analysis or Fisher’s exact test for categorical covariates, and Student’s t-tests or the Wilcoxon Rank Sum test for continuous covariates. We used separate logistic regression models, including factors that were significantly associated with non-comprehension in any domain in bivariate analysis, to examine predictors of non-comprehension in each domain of the discharge instructions (i.e., four models). Each model included only study participants who received instructions in the domain being modeled. The final logistic regression models for non-comprehension included age, sex, two or more hospital admissions in the past six months, social isolation, discharge diagnosis, and Charlson comorbidity index score.
In this study, we explicitly separated comprehension of the discharge instructions from compliance so that we could look at factors associated only with compliance. We used separate logistic regression models, including factors that were significantly associated with non-compliance in any domain in bivariate analysis, to examine predictors of non-compliance with each domain of the discharge instructions among those who understood their discharge instructions for that domain. We could not analyze non-compliance with follow-up appointments due to small numbers of non-compliant patients (n = 1). The final logistic regression models for non-compliance included age, sex, more than one disability in ADLs, and history of depression. Statistical significance was defined as p < 0.05. All data analysis was performed with SAS version 9.2 (SAS Institute Inc., Cary, NC). This study was approved by the Institutional Review Board at the University of Maryland, Baltimore, and all participants provided signed informed consent.
RESULTS
Study Population
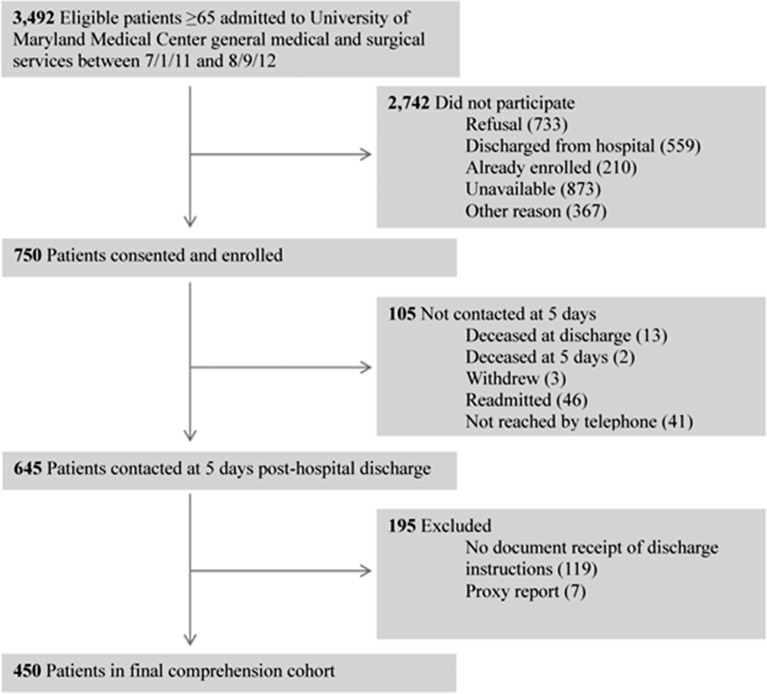
A total of 3,699 patients aged 65 and older were admitted to the general medical and surgical units at UMMC during the 13 month study period. (Fig. 1) Of these, 146 (4 %) were not competent to participate and 61 (2 %) did not speak English. Of the remaining 3,492, 750 (21 %) enrolled in the study. Among the 105 participants we were not able to contact at 5 days, thirteen (2 %) participants had died during the index hospitalization, three (< 1 %) had withdrawn from the study, two (< 1 %) were deceased, 46 (6 %) were readmitted to the hospital, and 41 (6 %) were not reached after five telephone attempts. Among the 645 participants contacted at 5 days, 119 (16 %) did not have documented receipt of the discharge instructions and we ascertained hospital readmission information through proxy report on 76 (10 %). There were 450 participants in our final study sample.
Figure 1.
Flow diagram of study participants.
Characteristics of the Study Participants
Mean age was 72.5 years [standard deviation (s.d.) 6.1] (Table 1). Length of the index hospital stay was skewed, with a median (interquartile range) of 3 (0,6) days. The most prevalent discharge diagnosis was heart disease (22 %). The ‘other’ category accounted for 36 % of discharge diagnoses and included (as a percentage of other): chronic kidney disease (17 %), non-specific symptoms (16 %), diseases of the respiratory system (13 %), stroke/transient ischemic attack (8 %), fractures (2 %), diseases of the nervous system (6 %), and septicemia (3 %).
Table 1.
Characteristics of Patients aged ≥ 65 at University of Maryland Medical Center Contacted at Five Days Post-Hospital Discharge, 2011–2012, n = 450
| Characteristic | Total |
|---|---|
| N = 450 | |
| Age in years, mean (sd) | 72.5 (6.1) |
| MMSE , mean (sd) | 28.1 (2.0) |
| Male sex, n (%) | 235 (52) |
| White race, n (%) | 335 (74) |
| Married, n (%) | 279 (62) |
| Disabilities in ADLS1 ≥ 1, n(%) | 59 (13) |
| ≥ High school education, n(%) | 390 (87) |
| ≥ 2 hospital admissions in last 6 months, n(%) | 98 (22) |
| Depressive Symptoms2, n(%) | 64 (14) |
| ≥ 2 falls in last 6 months, n(%) | 44 (10) |
| Social isolation3 risk, n(%) | 43 (10) |
| Number of medications at admission, median (IQR)4 | 3 (0,10) |
| Number of medications at discharge, mean (sd) | 10.1 (4.8) |
| Primary Discharge Diagnosis, n(%) | |
| Heart Disease | 99 (22) |
| Cancer | 51 (11) |
| Diseases of Digestive System | 61 (14) |
| Diseases of Musculoskeletal System | 30 (7) |
| Complications from Medical Care | 49 (11) |
| Other | 160 (36) |
| Charlson Comorbidity Index Score, mean (sd) | 2.4 (2.2) |
| Length of Hospital Stay in days, median (IQR)4 | 3 (0,6) |
1 Katz’s Activities of Daily Living, 2 15-item Geriatric Depression Scale ≥ 6, 3 6-item Lubben Social Network Scale <12, 4 Inter-quartile range
Who Received Discharge Instructions
One hundred percent of participants were prescribed medications at discharge (may have been new or continued), 99 % were told to follow up with a hospital, clinic or private physician, 58 % received diet instructions, and 19 % received exercise instructions (Table 2).
Table 2.
Prevalence of Non-Comprehension of the Hospital Discharge Instructions at 5 days Post-Discharge Among Adults ≥ 65 who Received Written Discharge Instructions, n = 450
| Discharge Instruction Domain | Instructions Given | Non-Comprehension |
|---|---|---|
| Medication, n (%) | 450 (100) | 120 (27) |
| Follow-Up Appointments, n (%) | 445 (99) | 22 (5) |
| Diet Recommendations, n (%) | 260 (58) | 131 (50) |
| Exercise Recommendations, n (%) | 87 (19) | 42 (48) |
Discharge diagnosis was associated with the receipt of discharge instructions concerning diet (Chi-square p < 0.001, df = 5) and exercise (Chi-square p < 0.001, df = 5). Patients with a discharge diagnosis of heart disease were most likely to receive diet instructions (91 %), while patients with a discharge diagnosis of cancer were least likely (41 %). Patients with a discharge diagnosis of musculoskeletal disease were most likely to receive exercise instructions (67 %), while patients with a discharge diagnosis of cancer (8 %) or heart disease (12 %) were least likely.
Non-Comprehension at 5 Days Post Discharge
Non-comprehension of the discharge instructions was 5 % for follow-up appointments, 27 % for medications, 48 % for exercise, and 50 % for diet recommendations (Table 2). Heart disease was chosen as the reference group for disease categories in regression analyses, because it was the most common discharge diagnosis.
In adjusted logistic regression models, increasing age [odds ratio (OR) 1.07; 95 % confidence interval (CI) 1.04, 1.12] was significantly associated with non-comprehension of medication instructions (Table 3). Compared to a discharge diagnosis of heart failure, complications from medical care (OR 3.11; 95 % CI 1.33, 7.25) and ‘other’ (OR 2.82; 95 % CI 1.45, 5.46) were significantly associated with non-comprehension of medication instructions. Increasing age (OR 1.08; 95 % CI 1.01, 1.17) was also associated with non-comprehension of follow-up appointment instructions. Compared to a discharge diagnosis of heart failure, complications from medical care (OR 11.12; 95 % CI 1.04, 119.61) and ‘other’ (OR 12.55; 95 % CI 1.46, 107.84) were significantly associated with non-comprehension of follow-up appointment instructions.
Table 3.
Adjusted Odds Ratios [95 % Confidence Intervals (CI)] of Non-Comprehension of the Hospital Discharge Instructions at 5 days Post-Discharge among Adults ≥ 651
| Medications | Follow-up Appointments | Diet | Exercise | |
|---|---|---|---|---|
| N = 450 | N = 445 | N = 260 | N = 87 | |
| Age | 1.07 (1.04, 1.12) | 1.08 (1.01, 1.17) | 1.03 (0.98, 1.08) | 1.04 (0.95, 1.14) |
| Male sex | 1.11 (0.71, 1.73) | 1.57 (0.60, 4.07) | 1.91 (1.10, 3.31) | 0.77 (0.26, 2.26) |
| ≥ 2 hospital admissions last 6 months | 1.31 (0.78, 2.23) | 0.57 (0.16, 2.07) | 0.52 (0.27, 1.02) | 1.31 (0.36, 4.75) |
| Social isolation2 | 0.54 (0.23, 1.26) | 2.85 (0.85, 9.60) | 2.15 (0.78, 5.89) | 9.42 (1.50, 59.11) |
| Primary discharge diagnosis | ||||
| Heart disease | Reference | Reference | Reference | Reference |
| Cancer | 2.17 (0.90, 5.24) | 2.32 (0.12, 43.64) | 0.46 (0.13, 1.61) | 0.25 (0.01, 9.66) |
| Digestive disease | 1.30 (0.55, 3.04) | 7.58 (0.73, 78.26) | 0.78 (0.32, 1.87) | 3.04 (0.52, 17.61) |
| Musculoskeletal disease | 2.17 (0.76, 6.21) | 5.05 (0.28, 90.30) | 6.54 (1.31, 32.78) | 0.55 (0.08, 3.73) |
| Complications from medical care | 3.11 (1.33, 7.25) | 11.12 (1.04, 119.61) | 5.96 (1.91, 18.62) | 0.47 (0.06, 3.72) |
| Other | 2.82 (1.45, 5.46) | 12.55 (1.46, 107.84) | 1.65 (0.79, 3.17) | 2.06 (0.42, 10.04) |
| Charlson comorbidity index score | 1.08 (0.96, 1.20) | 1.10 (0.89, 1.37) | 0.92 (0.79, 1.07) | 1.22 (0.83, 1.80) |
1 who received written discharge instructions; 2 6-item Lubben Social Network Scale < 12
Male sex was associated with non-comprehension of diet instructions (OR 1.91; 95 % CI 1.10, 3.1). Compared with a discharge diagnosis of heart failure, musculoskeletal disease (OR 6.54; 95 % CI 1.31, 32.78) and complications from medical care (OR 5.96; 95 % CI 1.91, 18.62) were significantly associated with non-comprehension of diet instructions. Social isolation (OR 9.42; 95 % CI 1.50, 59.11) was significantly associated with non-comprehension of the exercise instructions.
Non-Compliance at 5 Days Post Discharge
We examined non-compliance with the discharge instructions among those who understood their instructions (n = 330 for medications, n = 423 for follow-up appointments, n = 129 for diet, and n = 45 for exercise). Non-compliance was 10 % for medications, 0.2 % for follow-up appointments, 20 % for diet, and 51 % for exercise instructions. In adjusted logistic regression models, one or more ADL disabilities (OR 3.44; 95 % CI 1.44, 8.24) and self-reported history of diagnosed depression (OR 2.29; 95 % CI 1.02, 8.83) were significantly associated with non-compliance with medication instructions (Table 4). Self-reported history of depression (OR 3.30; 95 % CI 1.24, 8.83) was significantly associated with non-compliance with diet instructions. Increasing age (OR 1.06; 95 % CI 0.99, 1.15) was associated with non-compliance with diet instructions; however, this association did not reach statistical significance. No other significant associations were observed.
Table 4.
Adjusted Odds Ratios [95 % Confidence Intervals (CI)] of Non-Compliance with the Hospital Discharge Instructions at 5 Days Post-Discharge Among Adults ≥ 65 who Understood their Discharge Instructions
| Medications | Diet | Exercise | |
|---|---|---|---|
| N = 330 | N = 129 | N = 45 | |
| Age in years | 0.96 (0.90, 1.03) | 1.06 (0.99, 1.15) | 0.97 (0.86, 1.10) |
| Male sex | 0.67 (0.32, 1.49) | 1.42 (0.56, 3.65) | 1.02 (0.27, 3.80) |
| Disabilities in ADLS1 ≥ 1 | 3.44 (1.44, 8.24) | 0.38 (0.09, 1.57) | 0.70 (0.11, 4.33) |
| History of depression2 | 2.29 (1.02, 5.10) | 3.30 (1.24, 8.83) | 1.01 (0.25, 4.08) |
1Katz’s Activities of Daily Living; 2Self-reported history of diagnosed depression
DISCUSSION
In this prospective study of older adults, prevalence of non-comprehension of the discharge instructions varied by domain, and ranged from 5 % for follow-up appointments to 50 % for diet. Older age was associated with non-comprehension of medication and follow-up appointment instructions. Other factors associated with non-comprehension included male sex, social isolation, and discharge diagnosis. These results suggest a complex scenario in which patient factors contribute differentially to non-comprehension of distinct domains within the discharge instructions.
The prevalence of non-comprehension of the discharge instructions reported here is consistent with prior, smaller studies (range 16–78 %).2,6,7,29 Non-comprehension has also been observed to vary across domains of the discharge instructions.29 Social isolation was strongly associated with non-comprehension of the exercise instructions in this study, adding to prior reports of social isolation as a predictor of non-compliance.30–32 Cognition and high school education were not associated with non-comprehension in any domain of the discharge instructions, although health literacy has been previously identified as a barrier to comprehension.1,2,6,8
Factors associated with non-comprehension may help identify patients at greater risk, but do not provide a rationale for non-comprehension. Comprehension was defined in this study as accurately reporting the written discharge instructions; therefore, the patient may have ‘remembered’ instructions they perceived to be more important. Health behavior models suggest that patients react to symptoms.33 If no symptoms are present, patients may be less likely to ‘remember’ their instructions. Medications at discharge, stress related to the recent hospitalization, and related ongoing medical problems may also impact recall and/or comprehension of the discharge instructions.
Our reported estimates of non-compliance with the discharge instructions are lower than prior estimates (medication range: 29–58 %; follow-up appointment range: 22–44 %; diet range: 24–52 %; exercise range: 76–81 %), likely due to our requirement that patients understand the instructions.34–37 Our study design allowed examination of predictors of compliance without confounding by non-comprehension, in contrast with recent studies conducted among hospital inpatients.1,29 Our results suggest that increased comprehension may not improve compliance for all patients. Among patients who understood their discharge instructions and consistent with prior research, depression was associated with non-compliance with medication and diet instructions.35,36,38,39
Research on patient comprehension and compliance with discharge instructions is limited by a lack of uniform measures that leads to difficulty making comparisons with prior studies. As emphasis on discharge instructions is increased, there will be a need for consistent assessment methods. Patients with an MMSE score of 15 or less and those with limited English proficiency were excluded from this study, which may have resulted in an overestimation of comprehension. Poor English language proficiency has been previously correlated with non-comprehension of the discharge instructions.8 Furthermore, we asked about filled prescriptions but did not ask about medication names or dosing, which also may have resulted in an overestimation of comprehension. Prior studies have reported an association between non-comprehension and poor health literacy, which was not assessed in this study.1,2,6,8 However; cognition and high school education, which are correlated with health literacy, were not associated with non-comprehension in any domain of the discharge instructions. In this study, we did not assess verbal instructions; however, they are likely to be quickly forgotten and current guidelines call for written instructions.26,27 Future research with this instrument should incorporate patient education, an essential component of the discharge instructions. Outcomes of non-comprehension, such as hospital readmission, should be analyzed to determine if increased comprehension results in better patient outcomes.
The high prevalence of non-comprehension of the discharge instructions reported here highlights needs to improve patient understanding and possibly to revise the current discharge process. Patient comprehension is addressed in interventions that many hospitals are adopting, but current practice is a long way from where it needs to be.40 Furthermore, a narrow focus on comprehension may ignore the provider’s responsibility to improve delivery of discharge instructions. Results from this study will aid in developing an understanding of non-comprehension and non-compliance with the discharge instructions that will ultimately help patients get well sooner.
Acknowledgements
This work was supported by Agency for Healthcare Research and Quality grant R36HS021068-01 (J.S.A), National Institutes of Health grants T32AG000262-14 (J.S.A.), K01AI071015-05 (J.P.F.), National Heart, Lung, & Blood Institute grant R01 HL085706 (A.L.G.-B.).
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Coleman EA, Chugh A, Williams MV et al. Understanding and Execution of Discharge Instructions. Am J Med Qual. 2013;28(5):383–391 [DOI] [PubMed]
- 2.Chugh A, Williams MV, Grigsby J, et al. Better Transitions: Improving Comprehension of Discharge Instructions. Front Health Serv Manag. 2009;25:3. [PubMed] [Google Scholar]
- 3.Engel K, Heisler M, Smith D, et al. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand? Ann Emerg Med. 2009;53:454–461.e15. doi: 10.1016/j.annemergmed.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 4.James T, Smith P, Brice J. Self-reported discharge instruction adherence among different racial groups seen in the emergency department. J Natl Med Assoc. 2010;102:931–936. doi: 10.1016/s0027-9684(15)30712-4. [DOI] [PubMed] [Google Scholar]
- 5.Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80(8):991–994. doi: 10.4065/80.8.991. [DOI] [PubMed] [Google Scholar]
- 6.Spandorfer JM, Karras DJ, Hughes LA, et al. Comprehension of discharge instructions by patients in an urban emergency department. Ann Emerg Med. 1995;25:71–74. doi: 10.1016/S0196-0644(95)70358-6. [DOI] [PubMed] [Google Scholar]
- 7.Hastings SN, Barrett A, Weinberger M, et al. Older patients’ understanding of emergency department discharge information and Its relationship with adverse outcomes. J Patient Saf. 2011;7:19–25. doi: 10.1097/PTS.0b013e31820c7678. [DOI] [PubMed] [Google Scholar]
- 8.Karliner LS, Auerbach A, Napoles A, et al. Language barriers and understanding of hospital discharge instructions. Med Care. 2012;50:283–289. doi: 10.1097/MLR.0b013e318249c949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clarke C, Friedman SM, Shi K, et al. Emergency department discharge instructions comprehension and compliance study. CJEM. 2005;7(1):5–11. doi: 10.1017/s1481803500012860. [DOI] [PubMed] [Google Scholar]
- 10.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare Fee-for-Service Program. JAMA. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 11.Stanton MW, Rutherford MK. The high concentration of U.S. health care expenditures. Rockville (MD): Agency for Healthcare Research and Quality; 2005. Research in Action Issue 19. AHRQ Pub. No. 06-0060.
- 12.Boustani M, Baker MS, Campbell N, et al. Impact and recognition of cognitive impairment among hospitalized elders. J Hosp Med. 2010;5(2):69–75. doi: 10.1002/jhm.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forster AJ, Murff HJ, Peterson JF, et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–7. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 14.Coleman E. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51:549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 15.Albrecht JS, Gruber-Baldini AL, Hirshon JM, Brown CH, Goldberg R, Rosenberg JH, Comer AC, Furuno JP. Depressive symptoms and hospital readmission in older adults. J Am Geriatr Soc. 2014;62(3):495–9. doi: 10.1111/jgs.12686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 17.Sheikh VI, Yesavage VA. Geriatric depression scale (GDS): Recent evidence and development of a shorter version. In: Brink TL, editor. Clinical Gerontology: A Guide to Assessment and Intervention. New York: Hawthorn Press; 1986. p. 165. [Google Scholar]
- 18.Lesher E, Berryhill J. Validation of the geriatric depression scale—short-form among inpatients. J Clin Psychol. 1994;50:256–260. doi: 10.1002/1097-4679(199403)50:2<256::AID-JCLP2270500218>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 19.Katz S, Ford AB, Moscowitz RW, et al. Studies of illness in the aged: The index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 20.Lubben J, Blozik E, Gillmann G, et al. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist. 2006;46:503–513. doi: 10.1093/geront/46.4.503. [DOI] [PubMed] [Google Scholar]
- 21.Charlson M, Szatrowski T, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 22.Harris A, Furuno J, Roghmann M, et al. Targeted surveillance of methicillin-resistant Staphylococcus aureus and its potential use to guide empiric antibiotic therapy. Antimicrob Agents Chemother. 2010;54:3143–3148. doi: 10.1128/AAC.01590-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Furuno J, McGregor J, Harris A, et al. Identifying groups at high risk for carriage of antibiotic-resistant bacteria. Arch Intern Med. 2006;166:580–585. doi: 10.1001/archinte.166.5.580. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Medicare & Medicaid Services. Chronic Conditions Warehouse. Available at: http://www.ccwdata.org/chronic-conditions/index.htm. Accessed 5/30/14.
- 25.Buie VC, Owings MF, DeFrances CJ, Golosinskiy A. National Hospital Discharge Survey: 2006 summary. Vital Health Stat 13(168) 2010. Washington, DC: National Center for Health Statistics; 2010;13. Available from: http://www.cdc.gov/nchs/data /series/sr_13/sr13_168.pdf. Accessed 5/30/14 [PubMed]
- 26.Centers for Medicare and Medicaid Services. Revision to State Operation Manual, Hospital Appendix A, Interpretive Guidelines for 42 CFR 48243, Discharge Planning. May, 2013. Available at: http://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Policy-and-Memos-to-States-and-Regions-Items/Survey-and-Cert-Letter-13-32.html. Accessed 5/30/14.
- 27.Joint Commission on Accreditation of Healthcare Organizations. Specifications manual for national implementation of hospital core measures Available at: http://www.jointcommission.org/national_hospital_quality_measures_-_icu/. Accessed 5/30/14.
- 28.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Inter Med. 2013;173(18):1715–22. doi: 10.1001/jamainternmed.2013.9318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cameron C. Patient compliance: recognition of factors involved and suggestions for promoting compliance with therapeutic regimens. J Adv Nursmg. 1996;24:244–250. doi: 10.1046/j.1365-2648.1996.01993.x. [DOI] [PubMed] [Google Scholar]
- 31.Cruess DG, Localio AR, Platt AB, et al. Patient attitudinal and behavioral factors associated with warfarin non-adherence at outpatient anticoagulation clinics. Int J Behav Med. 2010;17:33–42. doi: 10.1007/s12529-009-9052-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gonzalez JS, Penedo FJ, Antoni MH, et al. Social support, positive states of mind, and HIV treatment adherence in men and women living with HIV/AIDS. Health Psychol. 2004;23:413–418. doi: 10.1037/0278-6133.23.4.413. [DOI] [PubMed] [Google Scholar]
- 33.National Cancer Institute. Theory at a Glance: A Guide for Health Promotion Practice (Second Edition). 2005. U.S. Department of Health and Human Resources, National Institutes of Health. Available online at: http://www.cancer.gov/cancertopics/cancerlibrary/theory.pdf. Accessed 5/30/14.
- 34.Kravitz RL, Hays RD, Sherbourne CD, et al. Recall of recommendations and adherence to advice among patients with chronic medical conditions. Arch Intern Med. 1993;153:1869–1878. doi: 10.1001/archinte.1993.00410160029002. [DOI] [PubMed] [Google Scholar]
- 35.Benner J, Glynn R, Mogun H, et al. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288:455–461. doi: 10.1001/jama.288.4.455. [DOI] [PubMed] [Google Scholar]
- 36.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 37.Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv. 2000;51:885–889. doi: 10.1176/appi.ps.51.7.885. [DOI] [PubMed] [Google Scholar]
- 38.Grenard J, Munjas B, Adams J, et al. Depression and Medication Adherence in the Treatment of Chronic Diseases in the United States: A Meta-Analysis. J Gen Int Med. 2011;26(10):1175–1182. [DOI] [PMC free article] [PubMed]
- 39.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 40.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization a randomized trial. Ann Intern Med. 2009;150:178. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]