Abstract
Background
There is a natural assumption that quality and efficiency are optimized when providers consistently work together and share patients. Diversity in composition and recurrence of groups that provide face-to-face care to the same patients has not previously been studied.
Objective
Claims data enable identification of the constellation of providers caring for a single patient. To indirectly measure teamwork and provider collaboration, we measure recurrence of provider constellations and cohesion among providers.
Design
Retrospective analysis of commercial healthcare claims from a single insurer.
Participants
Patients with claims for office visits and their outpatient providers. To maximize capture of provider panels, the cohort was drawn from the four regions with the highest plan coverage. Regional outpatient provider networks were constructed with providers as nodes and number of shared patients as links.
Main Measures
Measures of cohesion and stability of provider constellations derived from the networks of providers to quantify patient sharing.
Results
For 10,325 providers and their 521,145 patients, there were 2,641,933 collaborative provider pairs sharing at least one patient. Fifty-four percent only shared a single patient, and 19 % shared two. Of 15,449,835 unique collaborative triads, 92 % shared one patient, 5 % shared two, and 0.2 % shared ten or more. Patient constellations had a median of four providers. Any precise constellation recurred rarely—89 % with exactly two providers shared just one patient and only 4 % shared over two; 97 % of constellations with exactly three providers shared just one patient. Four percent of constellations with 2+ providers were not at all cohesive, sharing only the hub patient. In the remaining constellations, a median of 93 % of provider pairs shared at least one additional patient beyond the hub patient.
Conclusion
Stunning variability in the constellations of providers caring for patients may challenge underlying assumptions about the current state of teamwork in healthcare.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-014-2964-0) contains supplementary material, which is available to authorized users.
Keywords: accountable care organizations, patient care team, physician’s practice patterns
Introduction
Don Berwick, as CMS Director, estimated that poor provider coordination annually costs the healthcare system $25-45 billion.1 A fundamental assumption of the Patient Protection and Affordable Care Act is that as accountable care organizations (ACOs) transition to bundled payments,2,3 they will improve care coordination by designing team-based incentives.4 But what is a team? The surgeon and operating room nurse, paired sometimes for decades on end, where protocol and interaction are perfectly rehearsed, anticipated, and executed, is a classic example of a tight-knit medical team. But are most patients cared for by providers working in such harmony? The constellation of providers that offers face-to-face care to each patient may range in size from just one to dozens. While some teams are deliberately assembled, other constellations often form haphazardly, with some providers added by other providers and some added by the patient or family member. As a result, a patient’s primary care physician and others who also provide care to the patient may not know who is in the constellation or when new additions occur. Doctors and other providers are continually reassembled into new constellations. The diversity in composition of constellations of providers, as well as frequency of their recurrence, has not previously been studied, yet has deep implications for the design of ACOs and patient-centered medical homes (PCMHs) and the associated costs and outcomes. We characterize provider collaboration by measuring the cohesion among providers and recurrence of provider constellations in regions densely covered by a common commercial insurer.
Methods
Design and Data
This is a retrospective analysis of commercial healthcare claims from the HealthCore Integrated Research Database (HIRDSM).5 The Institutional Review Board at HealthCore approved the study and the Committee on Clinical Investigation at Boston Children’s Hospital determined it exempt. The HIRD contains longitudinal data from health plans in 14 states. We identified regions where patients represented a substantial portion of the population to capture as large a proportion of a provider’s panel as possible. Data from 2008 to 2011 included beneficiaries from four distinct regions where the commercial health plans contributing to HIRD cover a large fraction of the market. These regions were identified by combining zip codes where (1) the HIRD population in the zip code area represented at least 30 % of the local 2010 US census, (2) the zip code was among the top 30 % of the state’s zip codes for HIRD enrollment size, (3) the zip code was surrounded by others meeting criteria 1 and 2 to avoid “holes” in the regions studied, and (4) a 50-mile buffer around the region did not extend into a state where the plan was not a major insurer. A total of 293 zip codes qualified, primarily in urban areas of four Midwest and Southern states. Over a half million (549,272) beneficiaries lived in one of these regions, but 28,127 (5 %) had no claims during the study period and were dropped. The total number of patients studied was 521,145: 19 % in Region 1, 40 % in Region 2, 21 % in Region 3, and 20 % in Region 4.
Provider data set
To include ambulatory care providers having face-to face encounters with the patient, we first identified all patients residing in our four regions and all of their providers. We dropped claims for procedures not involving direct care (Appendix 1, available online) and providers in specialties not associated with routine ambulatory care (e.g., pathology, anesthesia, radiology, emergency medicine). To select for providers with substantive participation in the health plan, those with less than 50 HIRD patients were excluded. For some analyses, family practice, general practice, internal medicine, and pediatric medicine were grouped as primary care. When a provider had a large number of patients (>2,000), we examined the name and location associated with the provider ID to determine whether it represented something other than an individual such as a group practice or generic default ID. Six provider IDs were dropped.
Patient data set
Then, to more completely account for shared patients, we looked at the providers’ full panels in the data set, regardless of where the patients lived. Most providers (77 %) had patients in only one of the four study regions. We identified a primary region for each of the 10,325 providers, and this region contained almost all of each provider’s panel [median 99.5 %, interquartile range (IQR) 98.6–100]. The remaining portion was from the area outside regional boundaries, and these patients were only used to calculate providers’ practice size and to count the number of patients shared by collaborative pairs and triads—sets of two or three providers that share patients with each other.
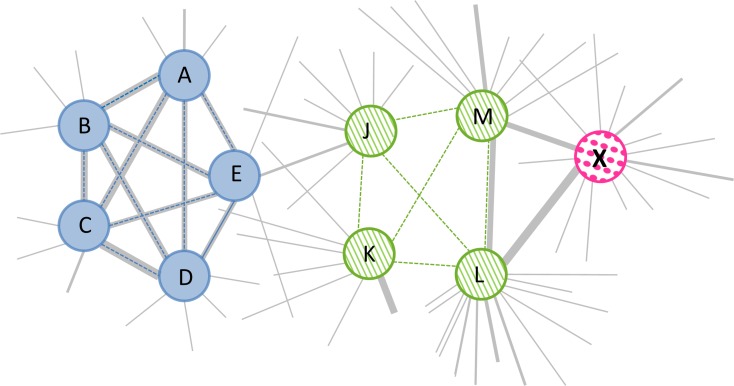
Regional provider networks were constructed for each region, with nodes denoting providers and links based on the total number of shared patients. The regional networks were used to derive variables describing relations among providers (Fig. 1 and Table 1).
Fig. 1.
An illustration of a subset of a regional provider network. In this illustrative network, providers are depicted as nodes and the number of shared patients between providers as links. Line thickness is proportional to the number of shared patients, and the shared hub patient in a constellation is indicated by a dotted line. On the left, a constellation of providers (A-E, colored blue) for Hub Patient 1 exhibits high cohesion. All the provider pairs in this constellation share other patients besides the hub patient (high constellation density). In fact, they share many patients as indicated by heavier lines for the links between them. These shared patients comprise large portions of the providers’ total patient panels. The remaining portions are illustrated by the thinner link lines to other providers whose nodes are not shown. In the middle is a constellation of four providers (J-M, colored green) for Hub Patient 2 that shows low cohesion. Only one of the six pairs in this constellation (L and M) shares other patients besides the hub (low constellation density). Further, each is linked to more other providers than the first team (higher personal network size). On the right is provider X (colored pink), who is the only provider for Hub Patient 3. This provider shares a moderate number of patients with provider L and M. If this patient needed to see another provider, L or M might be a good choice to add to the constellation for Patient 3 because they appear to collaborate more than other providers linked to X
Table 1.
Definition of terms and variables used in this study
| General terms | Definition |
|---|---|
| Cohesion | A concept that reflects the strength of bonds or links between providers. Measures include density and statistics regarding shared patients |
| Collaborative pair | Two providers (dyad) that share patients with each other. Dyads may be part of larger constellations as well |
| Collaborative triad | Three providers that share patients with each other. Triads may be part of larger constellations as well |
| Constellation | A subset of a regional network consisting only of providers who submitted claims for an individual patient |
| Density | Density (D) is the number of links observed (L) as a percent of all possible links (N*(N-1)) in a network. In an undirected network, D = 2 L/N(N-1) * 100. For example, in a network with 5 providers (A-E), if A shared patients with B, C, D, and E and C shared with D, the density score would be 50 % [((2*5) ÷ (5*4)) *100] |
| Hub patient | A patient who is shared by all members of a constellation |
| Provider personal network | A subset of a regional network that consists of a specific provider and all other providers with whom that one is linked |
| Regional provider network | Set of providers with patients in a region defined by zip codes. Providers in this study have at least 50 patients and are linked to each other when they shared at least one patient. Separate networks were constructed for each of the four study regions. No directionality was assumed for the links; thus, relations in the network were symmetric or undirected by design |
| Shared patients | Patients with claims submitted by two or more providers |
| Provider-centric variables | |
| Personal network density | The percent of collaborative pairs in the personal network of an individual provider |
| Personal network size | Number of providers in a region with whom one shares patients |
| Practice size | Number of patients with claims from an individual provider. Includes entire provider panel, regardless of where patients live |
| Personal network shared patients | Average and maximum number and percent of shared patients among collaborative pairs in a provider’s personal network |
| Patient-centric variables | |
| Constellation composition | Specialties of the providers in a constellation |
| Constellation density | The percent of all dyads in a constellation that share additional patients beyond the hub patient |
| Constellation size | Number of providers with claims for the hub patient |
| Other-patient sharing | Average and maximum number and percent of shared patients (excluding the hub patient) among pairs in a constellation |
A constellation is a group of providers sharing the same patient. Each provider has a provider personal network consisting of all other providers with whom she shares patients. Descriptive network variables define patterns of collaboration among providers.
Patient-centric metrics describe the size and composition and cohesion of constellations (Table 1). The number of shared patients is used to calculate variables related to the degree and extent of sharing. These variables include constellation density (the percent of dyads sharing other patients besides the hub patient) and average and maximum percent of patients shared. Provider-centric measures similarly describe cohesion among the group of providers with whom one is linked. This group is much larger in size than the set of providers in constellations. Greater cohesion would be indicated by greater density scores, but might be affected by network size.
Analysis
Summary measures (average and maximum number of shared patients) characterize the extent of patient sharing within a network. Descriptive analyses and t-tests or Kruskal-Wallis tests to compare groups were performed using SAS 9.3 (SAS Institute Inc., Cary, NC). The KW_MC macro6 implemented Dunn’s test for nonparametric post-hoc comparisons.
Results
Overall results are presented here in the text. Descriptive statistics and statistics by region are presented in Table 2. The specialties of collaborative provider pairs are presented in Appendix 2 (available online). And the extent of patient sharing among providers in precise constellations is presented in Table 3.
Table 2.
Patient, provider, and constellation characteristics by region
| Regions | Overall | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Providers | |||||
| Number with 50 or more patients, counted once in their primary region (area with majority of patients) | 2,103 | 4,043 | 2,408 | 1,771 | 10,325 |
| Practice size (number of patients*), median (IQR) | 153 (87–279) | 191 (100–191) | 198 (109–349) | 198 (101–389) | 185 (99–331) |
| Percent of patients that live in the provider’s primary region, median (IQR) | 99.2 (98–100) | 99.7 (99–100) | 98.9 (96–100) | 99.7 (99–100) | 99.5 (99–100) |
| Collaborative provider pairs | |||||
| Number of patients (combined practice size), median (IQR) | 509 (347–714) | 569 (399–781) | 638 (444–874) | 718 (482–1063) | 594 (408–836) |
| Number of patients shared by the pair, median (IQR) | 1 (1–2) | 1 (1–2) | 1 (1–2) | 2 (1–3) | 1 (1–3) |
| Collaborative provider triads | |||||
| Number of patients shared by the triad, median (IQR) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) |
| Provider personal networks | |||||
| Personal network size (number of providers with whom one shares patients), median (IQR) | 382 (235–592) | 411 (264–912) | 472 (292–782) | 492 (307–725) | 431 (268–662) |
| Personal network density (number of links as a percent of all possible links),† median (IQR) | 13 (8–19) | 7 (5–11) | 13 (8–21) | 26 (16–38) | 11 (6–19) |
| Average number of shared patients by provider pairs in personal network, median (IQR) | 1.8 (1.5–2.4) | 2.2 (1.7–3.1) | 2.3 (1.7–3.1) | 2.5 (1.8–3.6) | 2.1 (1.3–3.0) |
| Average percent shared patients from combined panels of pairs in personal network, median (IQR) | 0.4 (0.4–0.5) | 0.5 (0.4–0.6) | 0.4 (0.3–0.6) | 0.4 (0.4–0.5) | 0.4 (0.4–0.6) |
| Maximum number of shared patients by provider pairs in personal network, median (IQR) | 20 (10–47) | 28 (13–72) | 32 (14–74) | 32 (15–82) | 28 (13–68) |
| Maximum percent shared patients from combined panels of pairs in personal network, median (IQR) | 4.9 (2.6–11.3) | 6.3 (3.1–16.3) | 6.4 (2.9–15.1) | 5.7 (3.0–16.0) | 5.9 (3.0–14.9) |
| Patients | |||||
| Number with medical claims | 100,211 | 209,169 | 107,363 | 104,402 | 521,145 |
| Percent female | 56 | 54 | 55 | 57 | 55 |
| Age, mean (SD) | 40.4 (21.1) | 43.3 (22.1) | 47.8 (23.2) | 41.0 (20.2) | 43.2 (22.0) |
| Percent under 18 years old | 20 | 18 | 15 | 17 | 18 |
| Percent age 65 and older | 10 | 16 | 26 | 8 | 15 |
| Constellations | |||||
| Number of providers‡ median (IQR) | 3 (2–5) | 4 (2–6) | 4 (2–7) | 4 (3–7) | 4 (2–6) |
| Percent patients with a primary care provider§ | 88 | 92 | 89 | 94 | 91 |
| Percent female patients with an obstetrician/gynecologist | 42 | 49 | 42 | 50 | 46 |
| Percent patients with 2 or more providers in their constellation | 83 | 87 | 89 | 90 | 87 |
| Constellations with 2 or more providers | |||||
| Percent patients with 2+ providers | 83 | 87 | 89 | 90 | 87 |
| Number of providers in the constellation, median (IQR) | 4 (3–6) | 4 (3–6) | 5 (3–7) | 5 (3–7) | 4 (3–6) |
| Number of provider pairs in the constellation, median (IQR) | 6 (3–15) | 6 (3–15) | 10 (3–21) | 10 (3–21) | 6 (3–15) |
| Density (percent of pairs that share other patients besides the hub patient), median (IQR) | 86 (67–100) | 94 (70–100) | 90 (71–100) | 100 (83–100) | 93 (71–100) |
| Average number of other patients (besides hub) shared by pairs in a constellation, median (IQR) | 8 (4–21) | 14 (5–40) | 10 (5–27) | 25 (8–77) | 13 (5–39) |
| Average percent of pairs’ combined panels shared, median (IQR) | 1.2 (0.5–3.4) | 1.9 (0.7–5.9) | 1.3 (0.6–3.9) | 2.1 (0.8–6.1) | 1.6 (0.6–5.0) |
| Maximum number of other patients (besides hub) shared by at least one pair in a constellation, median (IQR) | 26 (7–87) | 56 (11–161) | 45 (11–136) | 132 (21–354) | 52 (11–169) |
| Maximum percent of pairs’ combined panels shared, median (IQR) | 3.7 (0.9–14.7) | 9.4 (1.4–24.1) | 6.4 (1.2–23.4) | 14.2 (1.8–25.4) | 8.1 (1.3–23.1) |
Abbreviations: SD = standard deviation, IQR = interquartile range
*Practice size was calculated by counting both patients who lived in the study regions and any other patients (not further studied) who lived outside the study regions
†To calculate, all possible links included all other providers in one’s primary region and any other provider with a patient in that same region
‡Providers were counted only if they had at least 50 patients in this study
§Primary care was defined as one of the following specialties: family practice, general practice, internal medicine, or pediatrics
Table 3.
Number of shared patients by size of precise constellation
| Constellation size: number of providers (# constellations at this size) | Number of shared patients | Constellations | |
|---|---|---|---|
| Number | Percent | ||
| 2 | 1 | 59,541 | 88.9 |
| (66,947) | 2 | 4,580 | 6.8 |
| 3+ | 2,826 | 4.2 | |
| 3 | 1 | 75,771 | 97.2 |
| (77,932) | 2 | 1,386 | 1.8 |
| 3+ | 775 | 1.0 | |
| 4+ | 1 | 280,609 | 99.5 |
| (281,920) | 2 | 913 | 0.3 |
| 3+ | 398 | 0.1 | |
Providers
The 10,325 providers studied had a median practice size of 185 HIRD patients. Primary care providers had larger practices (median 238 [IQR 127–386]) than obstetricians/gynecologists (median 206 [118–313], p < 0.05) and other specialists (median 155, [87–288], p < 0.05). The most common provider specialties were family practice (15 %), internal medicine (11 %), obstetrics and gynecology (8 %), pediatrics (8 %), orthopedic surgery (5 %), and cardiology (5 %). Half of all providers had one of these specialties, and no other specialty included more than 3.7 % of the providers.
Collaborative pairs
There were 2,641,933 unique collaborative pairs of providers who shared a median of one patient. This was 0.3 % [0.2–0.5] of the total number of patients in the providers’ panels combined. Of these collaborative pairs, 54 % shared only a single patient and 19 % shared two. The specialty of at least one provider in the pair was a primary care specialty (family practice, general practice, internal medicine, or pediatric medicine) in half of the unique pairs, and 15 % had at least one provider whose specialty was obstetrics/gynecology. The top 50 specialty pairs are shown in Appendix 2 (available online). The most frequently occurring were two primary care providers (6.3 %) and primary care-obstetrics/gynecology (5.4 %).
Collaborative Triads
There were 15,449,835 unique collaborative triads. Ninety-two percent shared just one patient, 5 % shared two, and only 0.2 % shared ten or more; 60 % of the triads included at least one primary care provider. When triads shared just one patient, 2 % contained three primary care providers. When triads shared at least ten patients, 38 % contained three primary care providers.
Provider personal networks
Providers were linked to a median of 431 other providers (personal network size) in their primary region (region with majority of patients), which was 11 % of the possible links (personal network density). This varied by provider specialty (p < 0.001), and each group differed from all others (p < 0.05 for all comparisons). Personal network size was smallest for primary care providers (median 364, [217–545]), followed by other specialties (median 471, [299–736]) and obstetrics/gynecology (median 486, [304–708]).
The median of the average number of patients shared by provider pairs in personal networks was 2.1 patients, representing 0.4 % of the collaborative pairs’ panels combined. The median of the maximum shared was 28 patients, which was 6 % of the combined panels across the collaborative pair.
Patients
A total of 521,145 patients were enrolled for a median of 1.9 years [0.9–2.7]. Fifty-five percent were female, and they were somewhat older (mean 43.9 years, SD 22.0) than male patients (42.3 years, SD 21.8, p < 0.001). Eighteen percent of patients were under 18 years old ,and 15 % were over 65.
Constellations
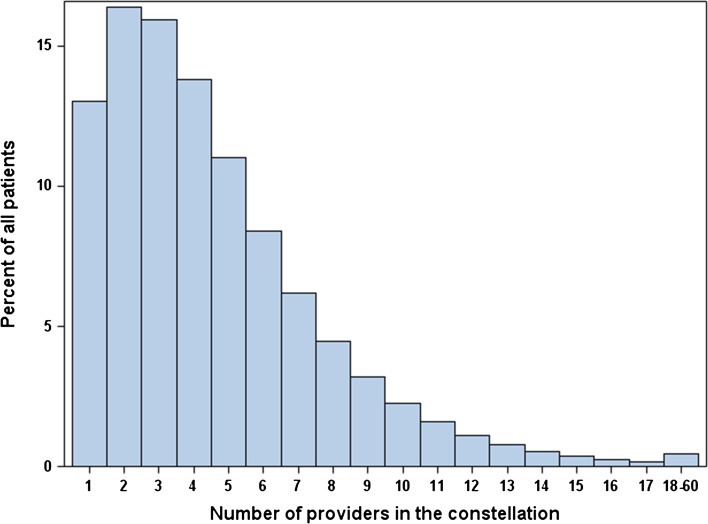
Patients had from 1 to 60 providers (median 4) in their constellation. Figure 2 shows the distribution of constellation size. Thirteen percent had just one provider, and 5 % had more than ten. Females had more providers (4 [3–7]) than males (3 [2–5], p < 0.001). Any precise constellation recurred rarely (Table 3). Constellations with exactly two providers (N = 66,947) usually shared just one patient (89 %), and only 4 % shared more than two. Of constellations with exactly three providers (N = 77,932), 97 % shared just one patient. When constellation size was above three, they almost always (99.5 %) shared just a single patient. Constellations with more than eight providers never shared more than two patients. The constellation composition of 91 % of the patients included at least one provider with a primary care specialty, and 46 % of female patients had an obstetrician/gynecologist. For constellation size of two or more, 94 % included a primary care provider, and 30 % included an obstetrician/gynecologist.
Fig. 2.
Percent of patients with constellations of different sizes
Constellation cohesion
Greater cohesion is indicated by both greater density (extent to which other patients are shared) and greater numbers of shared patients; 453,336 constellations included at least one collaborative pair, but 4 % of them only shared the hub patient.
For the remaining patients, 93 % of the pairs in their constellation shared at least one additional patient beyond the hub patient (constellation density). The median of the average number shared (excluding the hub) was 13 other patients, which was 1.6 % of the pairs’ combined panels. Some pairs in a constellation shared more patients than others. The median of the maximum number shared was 52 patients, which was 8 % of the combined panels.
Discussion
Insurance claims readily identify collaborative groups of physicians sharing patients, as well as the constellation of providers around each patient. There is stunning variability in the constellations of providers caring for patients, and the upper bound on collaboration among providers at the system level is disappointingly low. Nearly nine out of ten constellations with exactly two providers share only one patient within this health plan. Only 3% of constellations with exactly three providers shared more than one patient. We also describe dyads and triads—groups of two and three providers who may be parts of multiple constellations of varying sizes. Nearly three quarters of provider pairs who do share patients only share one or two. Nearly nine out of ten provider triads sharing patients only share one.
Cohesion among providers is not the norm. Instead, the often ad hoc constellations of providers caring for patients are not persistent teams. Yet as PCMHs and ACOs are formed, cross-organizational teams are expected to become increasingly foundational to standard practice. Re-design of healthcare around the PCMH and the ACO is predicated, in large part, on improving communication and collaboration among providers who share responsibility and financial risk for the health of the patient. A real team is a “small number of people with complementary skills who are equally committed to a common purpose, goals, and working approach for which they hold themselves mutually accountable.”7 Teamwork improves both primary care8 and chronic disease management;9 teams evaluated in these studies were generally proactively formed within specific organizational contexts, and often in inpatient settings.10 In patients with congestive heart failure, Pollock showed that when a patient’s providers shared more patients, both outpatient and inpatient costs tended to be lower.11
Our findings reveal not only that real teams are not prevalent in healthcare, but even recurrent constellations of providers—who may not be coordinating care at all—are exceedingly rare. Though it was uncommon for all providers in a constellation to regroup together in the exact same configuration and share additional patients, nonetheless, constellation density was high (93 %), indicating that most of the individual pairs did share some other patients besides the hub patient (median 13), just not necessarily the same other patients. Some of the collaborative provider pairs shared more patients than others; the median maximum shared was 52. So while constellations appear to be relatively unique, there is often some degree of patient sharing within the constellation; some pairs within the constellation might function more cohesively.
Other investigators have begun to examine health system properties that are apparent from claims-based analyses of networks constructed around shared patients between pairs of physicians. Landon et al. demonstrated that these shared patients define networks that vary in structure by region.12 Physicians with shared patients were more often located geographically close or based at the same hospital. Further, they suggest that regions with strong community networks—defined by the number of shared patients between any two physicians—might form the basis of a well-functioning ACO.13 Pollock showed that membership in a network of shared patients is indicative of practice pattern; prostatectomy rates varied across distinct subgroups of regional networks of urologists.14
Our study has some limitations. The regions studied may not be representative of all US practice, and our data include patients in just one commercial health plan. Other studies examining networks of providers defined by shared patients have used Medicare claims as a single data source.12,13,15,16 Like those studies, we miss shared patients, collaborative pairs, and constellations around patients covered by other payors. To mitigate this limitation, we chose regions with substantial market penetration by health plan. And from a health plan perspective, this data set represents all beneficiaries and affiliated providers. Nonetheless, we are clearly missing some additional shared patients who are covered by other payors or who do not have insurance. We have mitigated this limitation by selecting regions of high market share for the health plan. The median primary care practice size observed in our data is smaller than national averages, which reflects the single payor data source. Our study uses patients with commercial insurance and therefore patients are younger, but, as with prior studies in the literature, provider panels are a subset of their total. It appears that in our densely populated markets we capture a more complete network of providers; we found that primary care physicians are linked to 364 other providers, while in a survey-based study of Medicare patients, Pham showed 229 links per primary care provider.17 Some of the constellations likely represent cross-covering providers in the same practice, as claims data do not completely capture group practice designations. Hence, our results may have overestimated the number of shared patients across sites of care. Of course collaborative care may be no less important in these intra-institutional constellations.
Our data span 3 years. Additional linkages among providers might become apparent over a longer interval. The data set enabled identification of a primary specialty only, and some providers may have had a second specialty as well. Further, of the 12 % of dyads with the same specialty, we suspect that some were in the same practice.
Promoting a healthcare ecosystem based on stable, cohesive, and efficient constellations of providers will require substantial social engineering. A hypothetical example (Fig. 1) illustrates how team-based care may benefit from network statistics. Providers might be preferably selected based on prior collaboration. Our fundamental assumption, which remains to be tested, is that larger numbers of shared patients among providers may be indicative of cohesive practice and efficiencies in care delivery. These findings suggest that the current state is one of constant rearrangement of providers and that persistent teams in healthcare are far less common than assumed.
Electronic supplementary material
(DOCX 19 kb)
Acknowledgments
Supported by grant R21GM107645 from the National Institute of General Medical Sciences and G08LM009778 from the National Library of Medicine, NIH. We would like to thank Aurel Cami for his careful reading of and comments on the manuscript.
Conflict of interest
The authors declare that they do not have a conflict of interest.
References
- 1.Berwick D, Hackbarth A. Eliminating waste in US health care. JAMA: The Journal of the American Medical Association. 2012;307:1513–1516. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 2.Schroeder SA, Frist W. Phasing out fee-for-service payment. N Engl J Med 2013. [DOI] [PubMed]
- 3.Berwick DM. Launching accountable care organizations–the proposed rule for the Medicare Shared Savings Program. N Engl J Med. 2011;364:e32. doi: 10.1056/NEJMp1103602. [DOI] [PubMed] [Google Scholar]
- 4.Blumenthal DM, Song Z, Jena AB, Ferris TG. Guidance for structuring team-based incentives in healthcare. Am J Manag Care. 2013;19:e64–e70. [PMC free article] [PubMed] [Google Scholar]
- 5.About us. 2012. (Accessed June 17, 2014, at http://healthcore.com/home/research_enviro.php?page=Research.
- 6.Elliott AC, Hynan LS. A SAS((R)) macro implementation of a multiple comparison post hoc test for a Kruskal-Wallis analysis. Computer methods and programs in biomedicine. 2011;102:75–80. doi: 10.1016/j.cmpb.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Katzenbach J, Smith D. The Wisdom of Teams: Creating the High-performance Organization. New York: Harper Business; 2006. [Google Scholar]
- 8.Carter BL, Bosworth HB, Green BB. The hypertension team: the role of the pharmacist, nurse, and teamwork in hypertension therapy. J Clin Hypertens (Greenwich) 2012;14:51–65. doi: 10.1111/j.1751-7176.2011.00542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grumbach K, Bodenheimer T. Can health care teams improve primary care practice? Jama. 2004;291:1246–1251. doi: 10.1001/jama.291.10.1246. [DOI] [PubMed] [Google Scholar]
- 10.Manser T. Teamwork and patient safety in dynamic domains of healthcare: a review of the literature. Acta Anaesthesiol Scand. 2009;53:143–151. doi: 10.1111/j.1399-6576.2008.01717.x. [DOI] [PubMed] [Google Scholar]
- 11.Pollack CE, Weissman GE, Lemke KW, Hussey PS, Weiner JP. Patient sharing among physicians and costs of care: a network analytic approach to care coordination using claims data. J Gen Intern Med. 2013;28:459–465. doi: 10.1007/s11606-012-2104-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Landon BE, Keating NL, Barnett ML, et al. Variation in patient-sharing networks of physicians across the United States. JAMA: The Journal of the American Medical Association. 2012;308:265–273. doi: 10.1001/jama.2012.7615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Landon BE, Onnela JP, Keating NL, et al. Using administrative data to identify naturally occurring networks of physicians. Med Care. 2013;51:715–721. doi: 10.1097/MLR.0b013e3182977991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pollack CE, Weissman G, Bekelman J, Liao K, Armstrong K. Physician social networks and variation in prostate cancer treatment in three cities. Health Serv Res. 2012;47:380–403. doi: 10.1111/j.1475-6773.2011.01331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnett ML, Landon BE, O’Malley AJ, Keating NL, Christakis NA. Mapping physician networks with self-reported and administrative data. Health Serv Res. 2011;46:1592–1609. doi: 10.1111/j.1475-6773.2011.01262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnett ML, Christakis NA, O’Malley J, Onnela J-P, Keating NL, Landon BE. Physician patient-sharing networks and the cost and intensity of care in US hospitals. Med Care. 2012;50:152–160. doi: 10.1097/MLR.0b013e31822dcef7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pham HH, O’Malley AS, Bach PB, Saiontz-Martinez C, Schrag D. Primary care physicians' links to other physicians through Medicare patients: the scope of care coordination. Annals of internal medicine. 2009;150:236–242. doi: 10.7326/0003-4819-150-4-200902170-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 19 kb)