Abstract
Anabolic-androgenic steroid (AAS) use is associated with medical and psychiatric complications; however, despite the identification of psychosocial correlates of AAS use, comprehensive models have rarely been assessed. Thus, AAS use as a function of self-perceived weight status, victimization, and depressive symptoms was examined via simultaneous multiple mediation with non-parametric bootstrapping. Data from the 2009 National Youth Risk Behavior Survey (YRBS) was utilized. The target population consisted of all public, Catholic, and other private school students in grades 9 through 12 in the United States. The sample comprised 8,065 adolescent high school males. The global and individual indirect effects of self-perceived underweight status to AAS use through depressive symptoms and victimization were significant. However, the victimization pathway was revealed to be stronger in magnitude than the depressive pathway. Depressive symptoms and victimization are two pathways in which self-perceived underweight status predicts AAS use among adolescent boys.
Keywords: Anabolic-androgenic steroids, adolescent boys, depression, victimization, underweight
Anabolic-androgenic steroids (AAS) are a set of drugs which include testosterone and synthetic derivatives that serve to increase the synthesis of protein and promote the development of secondary male sex characteristics (Pope & Brower, 2009) and are typically taken to enhance strength, performance, and muscularity (Ip, Barnett, Tenerowicz, & Perry, 2011). Although the short-term negative outcomes of AAS use are perhaps not as pronounced as other drugs of abuse, there is emerging evidence that long-term consequences may include cardiovascular, endocrine, and psychiatric complications (Achar, Rostamian, & Narayan, 2010; Kanayama, Hudson, & Pope, 2008). Additionally, AAS use is not uncommon among adolescents (1% to 5.4%; Irving, Wall, Neumark-Sztainer, & Story, 2002; Ricciardelli & McCabe, 2004) and roughly one quarter of AAS using men report initial use during adolescence (Parkinson & Evans, 2006). Further, AAS users who initiate use in adolescence use AAS for more weeks than those who initiate in adulthood (controlling for age), and greater weeks using AAS is associated with more severe long-term consequences (H. Pope, personal communication, February 1, 2013; for a review see Lumia & McGinnis, 2010). Thus, it would seem plausible that identifying correlates of use in adolescence has the potential to aid in preventing the long-term consequences of AAS abuse.
One of the strongest correlates of AAS use among males is negative body image (e.g., Parent & Moradi, 2011; Ricciardelli & McCabe, 2004). Muscular mesomorphic bodies are often desired by adolescent boys (Ricciardelli & McCabe, 2004), perhaps due to perceptions that muscularity is an outward marker of one’s masculinity (Powlishta, Watterson, Blashill, & Kinnucan, 2008; Wienke, 1998). Indeed, muscularity and masculinity appear to be closely linked (Blashill, 2011; McCreary, Saucier, & Courtenay, 2005). AAS use is one strategy that adolescent boys may engage in to achieve a muscular body, and it would be expected that AAS use may be particularly salient for boys who view themselves as underweight, as this group may possess a desire to increase muscularity and body mass (Neumark-Sztainer, Story, Falker, Beuhring, & Resnick, 1999).
Although some studies have found an association between perceptions of being underweight and AAS use (e.g., Neumark-Sztainer, et al., 1999), to date, the mechanisms that explain this relationship remain largely unknown. Two possible pathways in this association may be elevated depressive symptoms and victimization (e.g., being threatened, bullied, or teased). Boys who perceive themselves as underweight tend to report elevated levels of depression (Atlantis & Ball, 2008; Eaton, Lowry, Brener, Galuska, & Crosby, 2005; ter Bogt et al., 2006; Whetstone, Morrissey, & Cummings, 2007) and victimization (e.g., Wang, Iannotti, & Luk, 2010). Regarding victimization, boys who perceive themselves as underweight may be vulnerable due to perpetrators also perceiving them as underweight, and thus, weak and easy targets (Wang et al., 2010). Boys who view themselves as underweight are also likely at increased risk for depression given the discordance between how they view their current body type and the idealized mesomorphic physique. Additionally, depression (Irving et al., 2002; Smolak, Murnen, & Thompson, 2005) and victimization (Ip et al., 2011; Irving et al., 2002; Pedersen, Wichstom, & Blekesaune, 2001; Pope, Phillips, & Olivardia, 2000; Smolak et al, 2005) have been associated with AAS use. Boys who are victimized may use AAS as one means of reducing bullying behavior, as larger, muscular boys tend not to be as frequent targets of victimization compared to their less muscular counterparts (Wang et al., 2010). They may also use AAS to cope with elevated depression that may be the result of negative body image (Ricciardelli & McCabe, 2004).
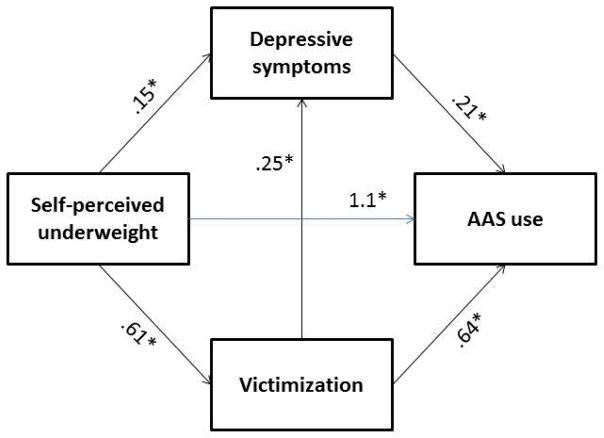
The literature to date has revealed several covariates of AAS use among adolescent boys; yet, few studies have explored these variables within a cohesive model, leaving the interrelationships among these constructs unidentified. For example, depression, victimization, and self-perceptions of shape/weight have independently been linked to AAS use. Yet, understanding the interrelationships among these variables is largely unknown. Accordingly, identifying and testing the various mediational (i.e., indirect) pathways between relevant variables and AAS use is of importance not just for advancing theory, but also to illuminate possible points of prevention and intervention (MacKinnon & Luecken, 2008). Given the literature reviewed above, it was hypothesized that boys who perceived themselves as underweight would endorse higher levels of depressive symptoms and victimization compared to their peers who perceived their bodies as non-underweight. Subsequently, these links were expected to be associated with AAS use (see Figure 1).
Figure 1.
Dual Pathway Model of AAS Use
Note. Unstandardized regression coefficients. Direct effect of self-perceived underweight to AAS use (B = .53, Odds Ratio = 1.7, SE = .25, z = 2.1, p = .04). Global indirect effect: self-perceived underweight—(victimization & depressive symptoms)—AAS use (B = .45, SE = .09, 95% BC CI [.27, .63]. Indirect effect: self-perceived underweight—depressive symptoms—AAS use (B = .03, SE = .02, 95% BC CI [.01, .07]). Indirect effect: self-perceived underweight—victimization—AAS use (B = .39, SE = .08, 95% BC CI [.23, .55]). Contrast of victimization indirect effect-depressive symptoms indirect effect (Bcontrast = .36, SE = .08, 95% BC CI [.19, .52].
Method
Participants and Procedure
Data were obtained from the 2009 national Youth Risk Behavior Survey (YRBS; CDC, 2004; Eaton et al., 2010). The YRBS is a nationally representative survey that monitors the health behaviors among U.S. high school students, and used a three-stage cluster sample design that yielded a representative sample of 9th through 12th grade students. Students included all public, Catholic, and other private school students enrolled in grades 9 through 12. Student participation in the study was voluntary and anonymous. In 2009, the survey included 98 items and the CDC’s IRB approved the national YRBS. A total of 16,410 students responded to the survey (88% return rate), from 158 schools (81% return rate). For the purposes of the current study, only participants who indicated their sex was male were included (N = 8,065). Additional information regarding the methodology and validity of the YRBS is discussed in detail elsewhere (see CDC, 2004).
Measures
Self-perceived weight status
Perceived weight status was assessed with the following item, “How do you describe your weight?” The response options were “very underweight,” “slightly underweight,” “about the right weight,” “slightly overweight,” and “very overweight.” These responses were bifurcated to create a yes/no item of very underweight status.
Victimization
Victimization was assessed via eight individual items, which included feeling unsafe, being threatened, and getting into fights at school, along with items that assessed intimate partner violence, sexual abuse, bullying and teasing. Most of these items included yes/no response options. For those that were assessed continuously, responses were dichotomized as “none/1 or more.” Next, a total victimization score was calculated based on the sum of the eight individual items, resulting in a possible range of 0 to 8, with higher scores denoting increased victimization. Internal consistency for the current sample was Kuder-Richardson Formula-20 (KR-20) = .70. KR-20 is an appropriate measure of internal consistency when individual items are responded to via dichotomous choices, and is analogous to Cronbach’s alpha.
Depressive symptoms
Symptoms of depression were assessed via four individual items, which included feeling sad or hopelessness nearly every day for a two-week period, as well as items assessing suicidal ideation, plans, and attempts over the previous 12 months. All but the latter item (regarding suicide attempts) were responded to via yes/no. The suicide attempts item was dichotomized into “none/ 1 or more”, and a total depressive symptoms score was calculated on the sum of the four individual items, resulting in a possible range of 0 to 4, with higher scores denoting increased depressive symptoms. Internal consistency for the current sample was KR-20 = .76.
AAS use
Lifetime AAS use was assessed with the following item, “During your life, how many times have you taken steroid pills or shots without a doctor’s prescription?” The response options for this item included, “0 times,” “1 or 2 times”, “3 to 9 times,” “10 to 19 times,” “20 to 39 times,” or “40 or more times.” A dichotomous variable—lifetime use of AAS: yes/no—was created via bifurcation of the response options.
Statistical analyses
Simultaneous multiple mediation (SMM) was conducted according to the bootstrapping strategy recommended by Preacher and Hayes (2008). SMM allows researchers to determine not only whether an individual variable meets criteria for mediation conditionally on the presence of other variables in the model, but also whether the combination of two or more variables meets criteria for mediation. One can also determine the relative magnitude of the indirect effects, in essence, comparing mediator variables’ unique ability to mediate, above and beyond other mediators in the model (Preacher & Hayes, 2008).
Bootstrapping is a non-parametric statistical approach in which cases from the original data set are randomly re-sampled (n = 2,000) with replacement, to re-estimate the sampling distribution. An indirect effect is considered to be “significant” if zero is not contained between the lower and upper 95% confidence intervals. Bootstrapping is generally preferred over traditional methods of studying mediation (i.e., the Causal Steps Approach and the Product-of-Coefficients Approach; Shrout & Bolger, 2002). One important advantage of this approach is that it does not require variables to conform to normal distributions. In the current study, SMM with 95% bias-corrected confidence intervals (BC CI) was conducted via PROCESS, a statistical program compatible with SPSS (Hayes, 2012).
Results
Preliminary analyses
The demographic characteristics of the sample (N = 8,065) included: 59.2% non-Hispanic white, 13.6% non-Hispanic black, 17.7% Hispanic, and 9.5% other race/ethnicity. There were fewer participants in higher grades than lower (28.6% in 9th grade, 26.3% in 10th grade, 23.1% in 11th grade, and 21.6% in 12th grade). See Table 1 for addition descriptive statistics.
Table 1.
Descriptive Statistics
| Variable | Frequency | % |
|---|---|---|
| AAS Use | 347 | 4.3 |
| Very Underweight | 226 | 2.8 |
|
|
||
| Mean | SD | |
|
|
||
| Depression | .42 | .88 |
| Victimization | .96 | 1.3 |
| Age | 16.1 | 1.2 |
Note. SD = standard deviation. Depression range: 0 to 4. Victimization range: 0 to 8.
Primary analyses
The total effect of self-perceived underweight status on AAS use was significant, B = 1.1, Odds Ratio = 3.0, SE = .21, z = 5.1, p < .00001. Self-perceived underweight status was significantly associated with increased victimization, B = .61, SE = .09, t = 7.1, p < .00001 and increased depressive symptoms, B = .15, SE = .06, t = 2.7, p = .007. Similarly, increased victimization was significantly associated with increased depressive symptoms, B = .25, SE = .007, t = 34.9, p < .00001, and increased AAS use, B = .64, Odds Ratio = 1.9, SE = .03, z = 18.6, p < .00001. Elevated depressive symptoms were also significantly related to AAS use, B = .21, Odds Ratio = 1.2, SE = .05, z = 4.2, p < .00001. When victimization and depressive symptoms were controlled, the direct effect of self-perceived underweight on AAS use remained significant, but dropped, B = .53, Odds Ratio = 1.7, SE = .25, z = 2.1, p = .04.
To quantify the difference between the total and direct effects, indirect effects of self-perceived underweight to AAS use were tested. The global indirect effect of self-perceived underweight to AAS use through depressive symptoms and victimization was significant, B = .45, SE = .09, 95% BC CI [.27, .63]. Both the depressive (B = .03, SE = .02, 95% BC CI [.01, .07]), and the victimization (B = .39, SE = .08, 95% BC CI [.23, .55]) pathways emerged as significant. However, the victimization pathway was revealed to have a stronger magnitude than the depressive pathway, Bcontrast = .36, SE = .08, 95% BC CI [.19, .52].
Discussion
Previous studies have explored the association between self-perceived underweight status and AAS use among adolescent boys; however, the current study was the first known to have assessed possible mechanisms in this relationship. Results indicated that both depressive symptoms and victimization appear to be possible mediators in the relationship between self-perceived underweight status and AAS use; however, victimization proved to be stronger in magnitude compared to depression. Thus, adolescent boys who view themselves as underweight are more likely to experience depressive symptoms and victimization compared to their peers. Perhaps these maladaptive outcomes are a function of perceptions of failing to meet cultural expectations for male norms, vis-a-vis the lack of a mesomorphic physique. Indeed, these boys may have responded to increased depressive symptoms and victimization by using AAS as a means to increase their muscularity in the context of conforming to masculine expectations (e.g., Kanayama, Barry, Hudson, & Pope, 2006). Theoretically, if underweight boys were to achieve a muscular, and hence, masculine appearance, then they may subsequently believe that their experience of depressive symptoms and victimization would be assuaged.
Clinical implications
On an individual level, clinicians working with depressed adolescent boys, particularly those who perceive themselves as underweight, should pay attention to the propensity for AAS use. For boys who have already initiated AAS use, perhaps an integrated intervention that specifically addresses depression and AAS use could be efficient and effective. To date, no known individual interventions have been published on AAS use among adolescent boys. However, based on the treatment recommendations of Kanayama, Brower, Wood, Hudson, and Pope (2010), simultaneously addressing body image concerns may prove useful. Cognitive behavioral therapy for body image disturbance has proven to be an efficacious treatment (Cash, 2008), and employing techniques from this intervention may also be helpful by indirectly targeting AAS use among boys (also see Parent, 2013, for techniques that address maladaptive masculine norms). To directly address AAS use, motivational interviewing techniques may be a useful first step, as they aim to increase awareness and motivation to change (Miller & Rollnick, 2002).
Limitations
Despite the additions the current study presents for both theory building and prevention/intervention, it is not without limitations. The nature of the cross-sectional data precludes temporal interpretation. Thus, causality cannot be inferred, as it is possible that the directionality of the pathways could be reversed, or bidirectional pathways may exist. Future research employing prospective designs, with three or more time points, are needed to assess the temporal prediction of the variables in the dual pathway model of AAS use. Further, the assessment of some of the variables in the study was limited. The internal consistency of the victimization variable was somewhat low (i.e., KR-20 = .70), thus, some caution should be made when interpreting results, and future research may benefit from careful selection of psychometrically sound measures. Weight status was based on participants’ self-perception, thus, it is possible that self-perceived weight may differ from objective measures of weight. Future research should incorporate both self-perceived and objective measures of weight to examine possible discrepancies and how this could alter pathways in the model of AAS use. It is also possible that AAS use was overestimated in the current study, given that some participants may have interpreted the question to include non-AAS, such as glucocorticoids. In addition, the depressive symptoms variable included items that measured sadness, hopelessness, and suicidality; however, the full range of possible depressive symptoms was not assessed, and thus likely limits the validity of this variable. Yet still, research has supported the validity of the suicide items from the YRBS, including strong correlations with a valid measure of depression (May & Klonsky, 2011). Lastly, the results from the current study should not be generalized to adults, as there may be important differences in correlates of AAS between boys and men (Parkinson & Evans, 2006).
Conclusions
In sum, self-perceived underweight status among adolescent boys is associated with both increased victimization and depressive symptoms. In turn, both are associated with AAS use, providing support for the dual pathway model. However, when these indirect effects were contrasted, the magnitude of the victimization pathway was stronger than the depressive pathway. Individual-based interventions that combine treatment for depression, body image concerns, and AAS use, via motivational interviewing, cognitive behavioral therapy, and gender-based intervention may prove effective.
Acknowledgments
Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under Award Number K23MH096647, awarded to Dr. Blashill.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Achar S, Rostamian A, Narayan SM. Cardiac and metabolic effects of anabolic-androgenic steroid abuse on lipids, blood pressure, left ventricular dimensions, and rhythm. American Journal of Cardiology. 2010;106:893–901. doi: 10.1016/j.amjcard.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atlantis E, Ball K. Association between weight perception and psychological distress. International Journal of Obesity. 2008;32:715–721. doi: 10.1038/sj.ijo.0803762. [DOI] [PubMed] [Google Scholar]
- Blashill AJ. Gender roles, eating pathology, and body dissatisfaction in men: A meta-analysis. Body Image. 2011;8:1–11. doi: 10.1016/j.bodyim.2010.09.002. [DOI] [PubMed] [Google Scholar]
- Cash TF. The body image workbook: An 8-step program for learning to like your looks. 2. Oakland, CA: New Harbinger Publications; 2008. [Google Scholar]
- Centers for Disease Control and Prevention. Methodology of the Youth Risk Behavior Surveillance System. MMWR. 2004;53:RR-12. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5312a1.htm. [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J Centers for Disease Control and Prevention. Youth risk behavior surveillance-United States, 2009. MMWR. 2010;59:1–142. Retrieved from http://www.cdc.gov/MMWR/preview/mmwrhtml/ss5905a1.htm. [PubMed] [Google Scholar]
- Eaton DK, Lowry R, Brener ND, Galuska DA, Crosby AE. Associations of body mass index and perceived weight with suicide ideation and suicide attempts among US high school students. Archives of Pediatric & Adolescent Medicine. 2005;159:513–519. doi: 10.1001/archpedi.159.6.513. [DOI] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper] 2012 Retrieved from http://www.afhayes.com/public/process2012.pdf.
- Ip EJ, Barnett MJ, Tenerowicz MJ, Perry PJ. The Anabolic 500 survey: Characteristics of male users versus nonusers of anabolic-androgenic steroids for strength training. Pharmacotherapy. 2011;31:757–766. doi: 10.1592/phco.31.8.757. [DOI] [PubMed] [Google Scholar]
- Irving LM, Wall M, Neumark-Sztainer D, Story M. Steroid use among adolescents: Findings from Project EAT. Journal of Adolescent Health. 2002;30:243–252. doi: 10.1016/S1054-139X(01)00414-1. [DOI] [PubMed] [Google Scholar]
- Kanayama G, Barry S, Hudson J, Pope H. Body image and attitudes toward male roles in anabolic-androgenic steroid users. American Journal of Psychiatry. 2006;163:697–703. doi: 10.1176/ajp.2006.163.4.697. Retrieved from http://ajp.psychiatryonline.org/data/Journals/AJP/3765/06AJ0697.PDF. [DOI] [PubMed] [Google Scholar]
- Kanayama G, Brower KJ, Wood RI, Hudson JI, Pope HG. Treatment of anabolic-androgenic steroid dependence: Emerging evidence and its implications. Drug & Alcohol Dependence. 2010;109:6–13. doi: 10.1016/j.drugalcdep.2010.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanayama G, Hudson JI, Pope HG. Long-term psychiatric and medical consequences of anabolic-androgenic steroid abuse: A looming public health concern? Drug & Alcohol Dependence. 2008;98:1–12. doi: 10.1016/j.drugalcdep.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumia AR, McGinnis MY. Impact of anabolic androgenic steroids on adolescent males. Physiology & Behavior. 2010;100:199–204. doi: 10.1016/j.physbeh.2010.01.007. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Luecken LJ. How and for whom? Mediation and moderation in health psychology. Health Psychology. 2008;27:S99–S100. doi: 10.1037/0278-6133.27.2(Suppl.).S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May A, Klonsky ED. Validity of suicidality items from the Youth Risk Behavior Survey in a high school sample. Assessment. 2011;18:379–381. doi: 10.1177/1073191110374285. [DOI] [PubMed] [Google Scholar]
- McCreary DR, Saucier DM, Courtenay WH. The drive for muscularity and masculinity: Testing the associations among gender-role traits, behaviors, attitudes, and conflict. Psychology of Men & Masculinity. 2005;6:83–94. doi: 10.1037/1524-9220.6.2.83. [DOI] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. Guilford Press; New York: 2002. [Google Scholar]
- Neumark-Sztainer D, Story M, Falkner NH, Beuhring T, Resnick MD. Sociodemographic and personal characteristics of adolescents engaged in weight loss and weight/muscle gain behaviors: Who is doing what? Preventive Medicine. 1999;28:40–50. doi: 10.1006/pmed.1998.0373. [DOI] [PubMed] [Google Scholar]
- Parent MC. Clinical considerations in etiology, assessment, and treatment of men’s muscularity-focused body image disturbance. Psychology of Men & Masculinity. 2013;14:88–100. doi: 10.1037/a0025644. [DOI] [Google Scholar]
- Parent MC, Moradi B. His biceps become him: A test of objectification theory’s application to drive for muscularity and propensity for steroid use in college men. Journal of Counseling Psychology. 2011;58:246–256. doi: 10.1037/a0021398. [DOI] [PubMed] [Google Scholar]
- Parkinson AB, Evans NA. Anabolic androgenic steroids: A survey of 500 users. Medicine and Science in Sports & Exercise. 2006;38:644–651. doi: 10.1249/01.mss.0000210194.56834.5d. [DOI] [PubMed] [Google Scholar]
- Pedersen W, Wichstom L, Blekesaune M. Violent behaviors, violent victimization, and doping agents. Journal of Interpersonal Violence. 2001;16:808–832. doi: 10.1177/088626001016008005. [DOI] [Google Scholar]
- Pope HG, Brower KJ. Anabolic-androgenic steroid-related disorders. In: Sadock B, Sadock V, editors. Comprehensive textbook of psychiatry. Philadelphia, PA: Lippincott Williams & Wilkins; 2009. pp. 1419–1431. [Google Scholar]
- Pope HG, Phillips KA, Olivardia R. The adonis complex: The secret crisis of male body obsession. New York: NY: Free Press; 2000. [Google Scholar]
- Powlishta K, Watterson E, Blashill A, Kinnucan C. Physical or appearance-related gender stereotypes. Poster presented at the Gender Development Research Conference; San Francisco, CA. 2008. Apr, [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Ressearch Methods. 2008;40:879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Ricciardelli LA, McCabe MP. A biopsychosocial model of disordered eating and the pursuit of muscularity in adolescent boys. Psychological Bulletin. 2004;130:179–205. doi: 10.1037/0033-2909.130.2.179. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. doi: 10.1037/1082-989X.7.4.422. [DOI] [PubMed] [Google Scholar]
- Smolak L, Murnen S, Thompson JK. Sociocultural influences and muscle building in adolescent boys. Psychology of Men & Masculinity. 2005;6:227–239. doi: 10.1037/1524-9220.6.4.227. [DOI] [Google Scholar]
- ter Bogt TF, van Dorsselaer SA, Monshouwer K, Verdurmen JE, Engels RC, Vollebergh WA. Body mass index and body weight perception as risk factors for internalizing and externalizing problem behavior among adolescents. Journal of Adolescent Health. 2006;39:27–34. doi: 10.1016/j.jadohealth.2005.09.007. [DOI] [PubMed] [Google Scholar]
- Wang J, Iannotti RJ, Luk JW. Bullying victimization among underweight and overweight U.S. youth: Differential associations for boys and girls. Journal of Adolescent Health. 2010;47:99–101. doi: 10.1016/j.jadohealth.2009.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whetstone LM, Morrissey SL, Cummings DM. Children at risk: The association between perceived weight status and suicidal thoughts and attempts in middle school youth. Journal of School Health. 2007;77:59–66. doi: 10.1111/j.1746-1561.2007.00168.x. [DOI] [PubMed] [Google Scholar]
- Wienke C. Negotiating the male body: Men, masculinity, and cultural ideals. Journal of Men’s Studies. 1998;6:255–282. Retrieved from http://mensstudies.metapress.com/content/c5qp785w06h01380/ [Google Scholar]