Abstract
The purpose of our study was to determine the safety and tolerability of early oral hydration (EOH) compared with delayed oral hydration (DOH) after general anesthesia. One thousand anesthesiology (ASA) I to III adult patients undergoing non-gastrointestinal surgery with general anesthesia were randomized assigned into two groups: DOH (n=500, patients were given water 4 h after general anesthesia), EOH (n=500, patients were given 0.5 ml/kg water once recovered from general anesthesia.) in the postanesthesia care unit (PACU). Patients were evaluated for nausea, vomiting, drink desire, thirsty scale, oropharyngeal discomfort scale, and satisfaction scale. Statistical analysis was performed with Student’s t and Chi-Square tests. Complete data were available for 983 patients (EOH=488, DOH=495). Twenty minutes after receiving water the incidence of vomiting in EOH group was very low. And there was no significant difference between the two groups at the same time point (p > 0.05). Compared with DOH group, after receiving water there was a significant decrease of patients’ thirsty scales (p < 0.0001) and oropharyngeal discomfort scales (p < 0.0001) in EOH group. Significantly more patients’ satisfaction were reported in EOH group (p < 0.001). No serious adverse effects were reported during the study period. For patients undergoing non-gastrointestinal surgery, early oral hydration after recovery from general anesthesia was safe, with lower thirsty scale and oropharyngeal discomfort scales, and higher satisfaction.
Keywords: General anesthesia, oral intake, postoperative nausea and vomit
Introduction
The number of general anesthesia procedures performed each year is increasing all around the world. Post-anesthesia care of these patients is important and demands attention. Now there is insufficient literature to evaluate the benefit of hydration status of patients in the post anesthesia care unit (PACU) [1]. Traditionally, postoperative oral hydration after general anesthesia (non-gastrointestinal surgery) has been withheld for about 4-6 hours for safety, in order to avoid vomiting, nausea because of residual anesthetics and incomplete emergence [2,3]. Sato [4] et al showed intraoperative fentanyl and remifentanil would delay the time of oral intake. However, many studies have shown the benefit and safety of oral fluid after general anesthesia [5-10]. The advantages include rapid return to normal diet, early ambulation, early bowl movement, reduced thirsty and increased satisfaction. Also there is little information about the timing of oral intake. Some studies [8,9] suggested water could be given 1 h after emergence from anesthesia for children under minor surgery. We hypothesized that oral hydration can be safely initiated immediately after recovery from general anesthesia for adult undergoing non-gastrointestinal surgery. The aim of this study was to determine whether, when compared with delayed oral hydration (DOH), early oral hydration (EOH) following general anesthesia is safe and has the potential to reduce thirst, as well as to increase patients’ satisfaction. The impact of this policy on nausea and vomit has also been observed.
Materials and methods
Sample
This prospective, randomized, controlled trial was approved by the West China Hospital, Sichuan University, China, and Institution Review Board. Patients were prospectively randomized with a computer-generated random number list. One thousand American Society of Anesthesiology (ASA) status I-III patients treated in the post anesthesia care unit (PACU) following general anesthesia were enrolled between July 2012 and Dec 2012. Exclusion criteria included conditions inducing delayed gastric empting time and pre-existing gastrointestinal disorders (such as peptic ulcer, hiatus hernia, irritable bowel syndrome, or esophagitis) facial, oropharyngeal and laryngeal surgery, impaired mental status, dysphagia, gastrointestinal surgery, neurosurgery, and thoracic surgery.
Overview of design
After taking a detailed medical history and administering the preoperative anesthesia evaluation, we explained the study procedures (details of the early oral hydration regimen, the thirst score, the satisfaction score, and follow-up) to the patient. Patients were also warned about possible complications (i.e., nausea, vomiting) that might be observed with the EOH regimen. Written, informed consent to participate was then obtained. When the patients were sent to PACU after their surgery, standard monitoring including electrocardiograph, pulse oximeter, capnograph and noninvasive blood pressure monitoring were applied. All patients received intravenous fluids. The thirst score used a verbal numeric scale (0 represented no thirst at all, and 100 meant strongest thirst ever experienced). The oropharyngeal discomfort scale also used a 0-100 verbal numeric scale (0 represented comfortable, and 100 meant most extreme discomfort ever experienced). On the first postoperative day, patients’ satisfaction pertaining to the oral intake regimen was recorded using a verbal numerical scale from 0 to 100, with 0 meaning not satisfied to 100 being most satisfied.
The patients were randomly assigned using a computer-generated random number assignment to two groups: Delayed oral hydration group (DOH, n=500), and early oral hydration group (EOH, n=500). The EOH group was treated as follows: trained PACU doctors and nurses evaluated the recovery from general anesthesia based on good mental status, muscle recovery to degree V, cough and swallowing reflex recovery, and stable vital signs. Muscle recovery degree was assessed by acceleromyography measurement of evoked responses to train-of four stimuli at the adductor pollicis using a TOF-GuardTM neuromuscular transmission monitor. The patients were then instructed to drink water (volume restricted to 0.5 ml/kg). After this single fluid intake patients in the EOH group received no additional fluid until 4-6 h after general anesthesia, by which time patients had been transferred from the PACU to the ward (to allow ward nurses to be blinded to patient group). The DOH group received oral water only 4 h after general anesthesia, as usual. The thirst and discomfort scores were administered in the PACU immediately after recovery from general anesthesia, and again 20 minutes later (20 minutes after the EOH group received early oral hydration or at the comparable time point for the DOH group) Patients were also asked about gastrointestinal symptoms such as nausea and vomiting at this 20 minutes time point, and again 20 minutes after receiving water in the ward at the 4 h time point. The number of patients expressing a desire to drink water was also obtained immediately after recovery from general anesthesia and 20 minutes later. These patients were observed in the PACU for 2 hours and then sent to the ward. On admission to the ward, the ward nurses were blinded to the policy. All patients will get water as traditional practice. Anesthesiologists and surgeons were also blinded to the study protocol.
The primary outcome measures were the time between arrival in the PACU to first drink, thirst scale, oropharyngeal discomfort scale, presence of nausea and vomiting, and patients’ satisfaction scale. Data was also collected about operation type, drugs used during anesthesia, and general medical data.
Statistical analysis
All data were expressed as mean±SD. Data was analyzed with SPSS Version 18.0 (SPSS Inc., Chicago, IL). Student’s t-Test was used for comparing continuous variables. Chi-Square analysis with Fisher’s test was used for categorical variables. P < 0.05 was considered statistically significant.
Results
There were 1000 patients enrolled in this trial, and complete data were available for 983 patients. Three patients were excluded because they refused to drink after general anesthesia, and 14 patients were unavailable for follow-up and excluded from the study (Figure 1). The demographic characteristics and surgical procedures of the remaining 983 patients are summarized in Table 1. There were no significant differences in the age, gender distribution, weight, ASA status, and surgical procedure between the two groups. Drugs used during general anesthesia are shown in Table 2, and there were no significant differences between the two groups. As expected, there was a significantly shorter time to the first drink in the EOH group (p < 0.05, EOH 0.29±0.14 h vs. 4 h respectively).
Figure 1.
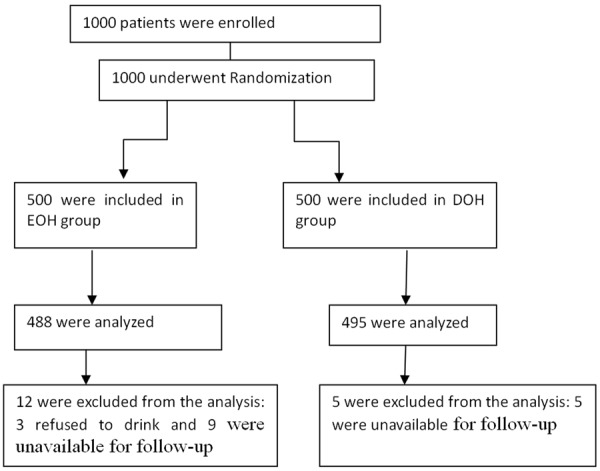
Randomization, treatment, and inclusion in analysis. EOH group: early oral hydration group; DOH group: delayed oral hydration group.
Table 1.
Characteristics of the patient population and the surgical procedures performed
| Characteristic and surgical procedure | Early oral hydration group (n=488) | Delayed oral hydration group (n=495) | P |
|---|---|---|---|
| Age (y) | 40.36±11.05 | 40.74±11.39 | 0.59 |
| Sex (%) | |||
| male | 116 (23.8) | 121 (24.4) | 0.82 |
| female | 372 (76.2) | 374 (75.6) | |
| Weight (kg) | 58.37±9.59 | 58.61±9.81 | 0.69 |
| ASA (%) | 0.21 | ||
| I | 57 (11.7) | 45 (9.1) | |
| II | 416 (84.6) | 430 (86.9) | |
| III | 18 (3.7) | 20 (4.0) | |
| Surgical procedures (%) | 0.72 | ||
| eye surgery | 32 (6.6) | 35 (7.1) | |
| breast surgery | 253 (51.8) | 265 (53.5) | |
| non-facial plastic surgery | 48 (9.8) | 55 (11.1) | |
| extremity surgery | 42 (8.6) | 43 (8.7) | |
| ear surgery | 113 (23.2) | 97 (19.6) |
Table 2.
Drugs used during general anesthesia
| Early oral hydration group (n=488) | Delayed oral hydration group (n=495) | P | |
|---|---|---|---|
| Atropine (%) | 315 (64.5) | 304 (61.4) | 0.32 |
| Fentanyl (%) | 26 (5.3) | 21 (4.2) | 0.46 |
| Sulfentanil (%) | 447 (91.6) | 457 (92.3) | 0.73 |
| Remifentanil (%) | 298 (61.1) | 285 (57.6) | 0.27 |
| Sevoflurane (%) | 362 (74.2) | 358 (72.3) | 0.52 |
| Tramadol (%) | 185 (37.9) | 177 (35.8) | 0.51 |
| Midazolam (%) | 433 (88.7) | 433 (87.5) | 0.56 |
| Propofol (%) | 452 (92.6) | 444 (89.7) | 0.11 |
| Neostigmine (%) | 174 (35.7) | 153 (30.9) | 0.12 |
| Antiemetic (%) | 327 (67.0) | 338 (68.3) | 0.68 |
There were no differences in incidence of nausea or vomiting after the first oral hydration. Twenty minutes after the first drink in the PACU, 1 patient (0.2%) experienced vomiting in EOH group, and 2 patients (0.4%) reported vomiting in the DOH group at the corresponding time without receiving water (Table 3). After the patients returned to the ward, there were also some patients who experienced vomiting before drinking at the 4 h post anesthesia time point: 7 (1.4%) in the EOH group vs. 5 (1.0%) in the DOH group). After they drank, there were 22 patients (4.5%) with vomiting in the EOH group compared to 20 (4.1%) in the DOH group (p > 0.05) (Table 3). Differences in vomiting incidence between the 2 groups were not significant at any of these time points. No serious adverse effects were reported during the study period.
Table 3.
Incidence of the postoperative nausea and vomiting in PACU and ward
| Early oral hydration group (n=488) | Delayed oral hydration group (n=495) | P | |
|---|---|---|---|
| PACU Vomiting within 20 minutes of first drink (EOH) or of recovery from anesthesia (DOH) | 1 (0.2) | 2 (0.4) | 1.0 |
| Ward 4 h post anesthesia Nausea before drinking | 12 (2.5) | 13 (2.6) | 1.0 |
| Vomiting before drinking | 7 (1.4) | 5 (1.0) | 0.58 |
| Nausea after drinking (%) | 37 (7.6) | 32 (6.5) | 0.53 |
| Vomiting after drinking (%) | 22 (4.5) | 20 (4.1) | 0.75 |
*Scales were administered just after recovery from anesthesia; the first drink was then administered to the EOH group only, and the scales were administered to both groups again 20 minutes later.
Regarding the thirst scale score just after recovery from anesthesia and before any oral hydration, it was similar between two groups (EOH 62.63±20.74 vs. DOH 60.42±20.09 respectively, p=0.09). But 20 minutes after the EOH group received the first drink, a significantly lower score was observed in (EOH 46.27±20.03 vs. DOH 61.09±20.11, P < 0.0001). There was a similar effect in the oropharyngeal discomfort scales (p < 0.0001). Also, patients’ satisfaction as reported on the following day was significantly higher in the EOH group (P < 0.001) (Table 4).
Table 4.
Thirsty scales, oropharyngeal discomfort scales in PACU and satisfaction scales
| Early oral hydration group (n=488) | Delayed oral hydration group (n=495) | P | |
|---|---|---|---|
| Thirsty scale before first drink* | 62.63±20.74 | 60.42±20.09 | 0.09 |
| Thirsty scale 20 minutes after first drink | 46.27±20.03 | 61.09±20.11 | 0.0001 |
| oropharyngeal discomfort scale before first drink | 26.76±25.16 | 27.40±26.12 | 0.70 |
| oropharyngeal discomfort scales 20 minutes after drink | 22.68±22.73 | 26.86±25.14 | 0.0001 |
| Number desiring a drink | |||
| Before drink | 488 (100%) | 495 (100%) | 1.00 |
| 20 minutes after drink | 347 (71.1%) | 469 (94.7%) | 0.001 |
| Satisfaction scale (postoperative day 1) | 98.31±3.59 | 96.94±5.47 | 0.001 |
Scales were administered just after recovery from anesthesia; the first drink was then administered to the EOH group only, and the scales were administered to both groups again 20 minutes later.
Discussion
The finding of this randomized study showed that early oral hydration for patients immediately after undergoing non-gastrointestinal surgery under general anesthesia, was not only safe and well tolerated, but also significantly reduced patients’ thirst and oropharyngeal discomfort, and increased patients’ satisfaction than delayed oral hydration.
This study included 983 patients who underwent non-gastrointestinal surgery under general anesthesia and were randomized to early or delayed oral hydration after surgery. Oral hydration immediately after recovery from anesthesia was not correlated with significant gastrointestinal or postoperative complications. Early intake of liquid decreased thirst and increased patients’ satisfaction.
Restriction of liquid has been a commonly accepted practice involving the gastrointestinal tract after general anesthesia because EOH may result in abdominal distension, postoperative nausea, and vomiting. However for non-gastrointestinal surgery, patients’ gastric activity returns its baseline level in a short time and it may be expected that hydration following emergence from anesthesia would not cause too much nausea and vomiting. Schreiner [10] et al. revealed that the incidence of vomiting increased in children who were required to drink before they were discharged home as compared with children for whom drinking was elective. Al-Takroni [5] et al enrolled 207 patients with caesarean section under general anesthesia, and the data showed eight per cent in the early hydration group and 7% in the control group had mild abdominal distension and nausea, and no vomiting. In our study, the incidence of nausea and vomiting was similar between EOH and DOH group both in PACU and in the ward. And the incidence of vomit and nausea of the non-gastrointestinal adult patients was lower than the previous study. So the effects of drinking on PONV may be caused by different surgical procedures, rather than by drinking fluids [11].
While discussion the timing of oral intake after general anesthesia, Cheng [9] et al reported that gastric motility has returned to normal 1 h after emergence from anesthesia in children who had undergone non-abdominal surgery. Mercan et al [8] showed a first oral intake in children 1 h after emergence from anesthesia for minor surgery did not cause increased incidence of vomiting. In our study, the first oral hydration time was 0.29±0.14 h. It is shorter than the previous studies because the incidence of vomiting is higher in pediatric patients than in adults [2].
When patients recovered from anesthesia, patients always complain with thirst and oropharyngeal discomfort which decrease patients’ comfort (thirsty scale: EOH 62.63±20.74 and DOH 60.42±20.09; oropharyngeal discomfort scale: EOH 26.76±25.16 and DOH 27.40±26.12). Most patients would like to drink or eat earlier after recovery from anesthesia than is usually permitted. Patients after non-gastrointestinal surgery can easily be allowed early hydration after careful evaluation and under strict vigilance. Reintroducing early drinking postoperatively was not associated with increased nausea. So water should not be withheld. A previous study showed that patients were thirsty after general anesthesia, and after receiving water, the incidence of vomiting was 1.4% [10]. This is comparable to our study. Jin et al showed neither drinking nor nondrinking worsened postoperative nausea or vomiting or prolonged hospital stays for 726 adults after ambulatory surgery. Therefore, we allowed patients 0.5 ml/kg water to decrease patients’ thirst and oropharyngeal discomfort. Patients in EOH group had lower thirsty ratings and less oropharyngeal discomfort.
Jin [12] et al showed early oral intake would increase patients’ satisfaction. Our study also showed giving patients water immediately after recovery from general anesthesia was safe and satisfactory. Although previous studies [3-7] showed the feasibility of early oral intake, thirst scales and oropharyngeal discomfort scales were not evaluated. Patients in our study evaluated thirst scales before and after oral hydration. This showed that patients in group EOH had significantly decreased thirst scales after hydration.
Finally, although our results proved the safety of early oral hydration after general anesthesia under non-gastrointestinal surgery, the regimen must be carefully weighed against potential serious complications, especially in PACU. In our study, we trained the anesthesia nurses to monitor the patients for safety.
There were several limitations to our study. First, the verbal numeric scale was used to describe the thirst, oropharyngeal discomfort and satisfaction. In PACU, the patients in both groups are so near to each other and at least the trend of the scores is somehow interrupted. Secondly, the patients received only a small amount of water. A larger study is needed to confirm our results and to evaluate whether larger amounts of water are also safe and tolerable.
Conclusion
In conclusion, this prospective randomized trial showed early oral hydration starting immediately after recovery from general anesthesia is safe and well tolerated in patients undergoing non-gastrointestinal surgery. EOH may increase patients’ satisfaction. Therefore, we believe patients should be allowed to choose drinking water immediately after general anesthesia for non-gastrointestinal surgery.
Acknowledgements
This work was supported in part by National Natural Science Foundation of China (81200865), the funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. All authors have no potential conflicts of interest for this work.
References
- 1.Apfelbaum JL, Silverstein JH, Chung FF, Connis RT, Fillmore RB, Hunt SE, Nickinovich DG, Schreiner MS, Silverstein JH, Apfelbaum JL, Barlow JC, Chung FF, Connis RT, Fillmore RB, Hunt SE, Joas TA, Nickinovich DG, Schreiner MS American Society of Anesthesiologists Task Force on Postanesthetic Care. Practice guidelines for postanesthetic care: an updated report by the american society of anesthesiologists task force on postanesthetic care. Anesthesiology. 2013;118:291–307. doi: 10.1097/ALN.0b013e31827773e9. [DOI] [PubMed] [Google Scholar]
- 2.Watcha MF, White PF. Postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthesiology. 1992;77:162–84. doi: 10.1097/00000542-199207000-00023. [DOI] [PubMed] [Google Scholar]
- 3.Horowitz IR, Rock JA. Post-anaesthesia and post operative care. In: Thomson JD, Rock JA, editors. Te Linde’s Operative Gynecology. 7th edition. Philadelphia, JB: Lippincott Company; 1992. [Google Scholar]
- 4.Sato C, Toraiwa S, Kobayashi T, Onodera N, Nakamura S. Influence of intraoperative fentanyl and remifentanil infusion on early postoperative oral intake after general anesthesia. Masui. 2012;61:1018–22. [PubMed] [Google Scholar]
- 5.Al-Takroni AM, Parvathi CK, Mendis KB, Hassan S, Qunaibi AM. Early oral intake after caesarean section (CS) performed under general anaesthesia. J Obstet Gynaecol. 1999;19:34–7. doi: 10.1080/01443619965921. [DOI] [PubMed] [Google Scholar]
- 6.Steed HL, Capstick V, Flood C, Schepansky A, Schulz J, Mayes DC. A randomized controlled trial of early versus “traditional” postoperative oral intake after major abdominal gynecologic surgery. Am J Obstet Gynecol. 2002;186:861–5. doi: 10.1067/mob.2002.123057. [DOI] [PubMed] [Google Scholar]
- 7.Mangesi L, Hofmeyr GJ. Early compared with delayed oral fluids and food after caesarean section. Cochrane Database Syst Rev. 2002;3:CD003516. doi: 10.1002/14651858.CD003516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mercan A, El-Kerdawy H, Bhavsaar B, Bakhamees HS. The effect of timing and temperature of oral fluids ingested after minor surgery in preschool children on vomiting: a prospective, randomized, clinical study. Paediatr Anaesth. 2011;21:1066–70. doi: 10.1111/j.1460-9592.2011.03626.x. [DOI] [PubMed] [Google Scholar]
- 9.Cheng BW, Chow B, Tam PK. Electrogastrographic changes in children who undergo day-surgery anesthesia. J Pediatr Surg. 1999;34:1336–1338. doi: 10.1016/s0022-3468(99)90006-4. [DOI] [PubMed] [Google Scholar]
- 10.Schreiner MS, Nicolson SC, Martin T, Whitney L. Should children drink before discharge from day surgery? Anesthesiology. 1992;76:528–533. doi: 10.1097/00000542-199204000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Larsson S, Lundberg D. A prospective survey of postoperative nausea and vomiting with special regard to incidence and relation to patient characteristics, anesthetic routines and surgical procedures. Acta Anaesthesiol Stand. 1995;39:539–45. doi: 10.1111/j.1399-6576.1995.tb04115.x. [DOI] [PubMed] [Google Scholar]
- 12.Jin F, Norris A, Chung F, Ganeshram T. Should adult patients drink before discharge from ambulatory surgery? Anesth Analg. 1998;87:306–11. doi: 10.1097/00000539-199808000-00013. [DOI] [PubMed] [Google Scholar]


