Abstract
Objective: The aim of this study was to evaluate change in the sagittal position of point A due to orthodontic treatment by orthodontic community-cone beam computed tomography (CBCT). Materials and methods: 40 subjects (22 males and 18 females) who had Class II division 2 malocclusion were recruited, and 40 subjects (23 males and 17 females) who had minor crowding in the beginning of the treatment and required no or minimal maxillary anterior tooth movement were served as control. The changes in maxillary incisor inclination, sagittal position of point A, SNA angle, and movement of incisor root apex and incisal edge were calculated before and after CBCT treatment. Results: Maxillary incisors were significantly proclined in the study group but not in the control group. This proclination resulted in 2.95 mm backward movement of the root apex and 6.23 mm forward movement of the incisal edge of maxillary incisors. Point A moved 1.24 mm and 0.18 mm backward in the study and control groups, respectively. Incisor root apex and incisal edge almost remained stable in the control group. No significant change was observed in the SNA angle in both the study and control groups. However, the change in SNA between the two groups was found to be significant. Conclusions: Proclination of maxillary incisors with backward movement of incisor root apex caused posterior movement of point A. This posterior movement significantly affects the SNA angle.
Keywords: Class II division 2, point A, maxillary incisor proclination
Introduction
Points A was the most commonly used as skeletal landmarks to reflect the sagittal relationship between maxilla and mandibular [1,2]. However, point A has also been considered as an unreliable anatomic landmark which may be influenced by growth and dentoalveolar remodeling during the orthodontic treatment [3]. It is important to assess whether there was a relationship between anterior tooth movement and position of point A.
However, there were still few studies investigated the effects of anterior tooth movement on the position changed of point A in previous literatures [4-11]. An earlier study [10] demonstrated that labial inclination of the incisor will be result in significant forward the point A. In recent study [5] further believed that 10 degrees to 14 degrees proclination of upper incisors resulted in 0.6 mm or great statistically significant change in point A, which was similar to the results of other studies [7,10].
Whilst study designs of previous works on the change of the Point A often appear to be defective. First, in order to evaluate the effect of any tooth movement on skeletal structures, the studies should be performed on subjects at the similar age because the skeletal response may be different in growing or grown patients. However, previous studies evaluating the relationship between the incisor inclination and movement of point A were performed on subjects with a wide range of ages, which may affect the response of point A to maxillary incisor movement. In addition, it is better to perform a control group in an attempt to account for growth. However, in the orthodontic literature, almost all previous studies evaluating the effect of maxillary incisor inclination on the position of point A lack a control group [4-11].
Furthermore, cephalometric studies are subject to error, and reports often indicate small changes caused by treatment. Many studies have looked at the reliability of lateral cephalograms and have found them to be reproducible. Few studies, however, have attempted to assess the accuracy of cephalometric measurements as applied three-dimensionally because of known intrinsic limitations of these images, such as distortion and magnification. In some cases, the magnitude of error may approach the therapeutic changes and raise doubt about their validity [12-14]. It is essential that all authors carry out repeatability assessments within a study and consider the effect of measurement variability in the interpretation of the overall results of the study. This is a common fault of cephalometric studies. Recently, a new technology is catching the attention of the orthodontic community-cone beam computed tomography (CBCT). These reconstructed images are accurate and reliable when compared with conventional radiographs. This so-called “bridge” from 3D to 2D images has helped orthodontists use the advantages of CT scans without having to add a lateral cephalometric exposure for craniofacial diagnosis [15,16].
In a word, cephalometric have several limitations, and no study have evaluated the change of point A with three-dimensional imaging methods. Thus, this study used CBCT to evaluate the magnitude of alterations on the position of point A in Class II division 2 malocclusion patients with similar age.
Materials and methods
Ethical approval was obtained from The Ethics Committee of the stomatology hospital of The Wenzhou Medical University. The participants were informed about the treatment procedures and assured of the confidentiality of the collected information. Only those who were given written consent were included in the research. The sample size for each group was calculated based on an alpha significance level of 0.05 and a beta of 0.1 to achieve 90% power to detect a clinically meaningful difference of SNA between the study and control group. The power analysis showed that 35 patients in each group were needed and to compensate for dropouts during the trial, it was adjusted to enroll at least 40 patients.
We recruited 80 subjects await for treatment from the Department of Orthodontics, Wenzhou medical university were divided into two group: 40 subjects (22 males and 18 females) with Class II division 2 malocclusion as the study group and 40 Class I subjects (23 males and 17 females) with minor crowding who required minimal maxillary anterior tooth movement as the control group. The average age of the sample was 20.2 ± 3.8 years, with range from 18 to 25 years.
All radiographs had been taken as part of the standard clinical procedure for diagnosis and treatment of orthodontic patients at the request of the clinician supervising the patient’s care.
All the participants met two criteria. First, the age of subjects in both groups is similar. Second, the difference between the initial and posttreatment U1-PP angle (angle formed by the intersection of the longaxis of the maxillary incisor and the anterior nasal spine and posterior nasal spine line) should be at least 10 degrees for the study group. The upper incisors in the control subjects were of average inclination at the beginning and remained stable or changed minimally after orthodontic treatment.
All subjects took CBCT before treatment and received fixed orthodontic treatment (Roth prescription, slot size 0.022 × 0.028 inch). No lacebacks or cinch back bends were placed in the upper archwire to allow for upper incisor proclination. Orthodontic treatment was continued until sufficient proclination of the upper incisors. In the middle of treatment, CBCT was taken to confirm sufficient upper incisor proclination in Class II divided 2 groups. An angle equal to or greater than 108 degrees between the long axis of the upper central incisors and the maxillary plane indicated sufficient proclination. No headgear or functional appliances were used before or simultaneously with use of the fixed orthodontic appliance. Patients in the control group take CBCT at the end of treatment.
All radiographs used in the present study were taken with the same CBCT machine (New Tom VGi, Italy). Each image was converted to a Digital Imaging and Communications in Medicine (DICOM) format and analyzed using the Dolphin 3D program (Version 11.0, Dolphin Imaging & Management Solutions, Chatsworth, Calif). Measures were traced by the same operator by hand, and all measurements were carried out with a gauge to the nearest 0.1 mm. CBCT landmarks used in this study are identified in Figure 1.
Figure 1.
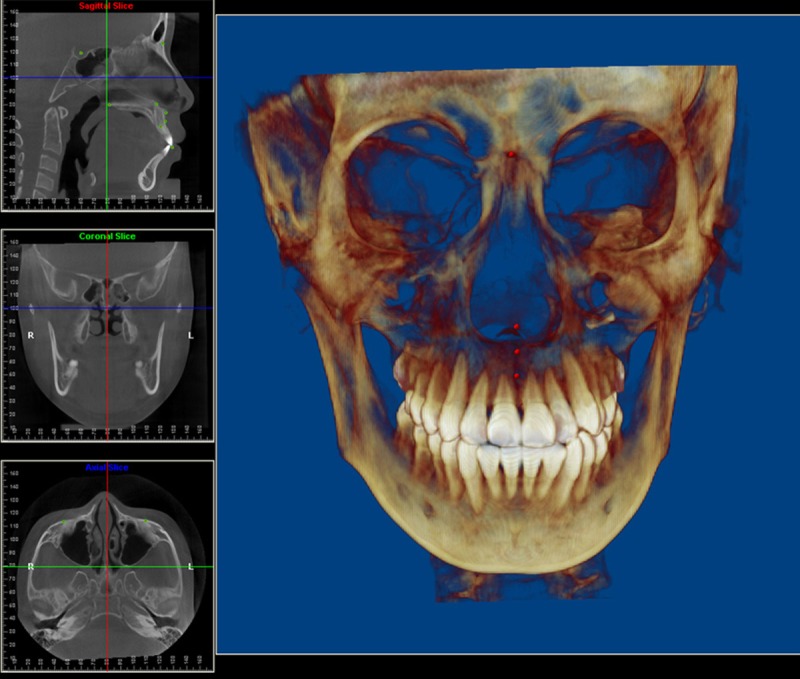
Location of the cephalometric landmarks in the 3D imagine.
We used three mutually perpendicular planes formed a three-dimensional coordinate system which N-point as the origin point. We obtained a three-dimensional coordinate value of the point through measuring the distance of each point to the three reference plane.
Horizontal plane: through nasion and parallel to the frankfort horizontal plane; Sagittal plane: through Sella and the nasion and perpendicular to the horizontal plane; Coronal plane: through nasion and perpendicular to the horizontal plane and sagittal plane, see Figure 2. The x, y, and z coordinates of incisal edge, incisor root apex, point A were defined by using the Dolphin 3D program (Version 11.0, Dolphin Imaging & Management Solutions, Chatsworth, Calif) to standardize the anatomic identification in the three planes of space and to guide the selection of the most precise location in the sagittal, axial, and coronal views. The following parameters were used in this study: 1. SNA angle: angle formed by the intersection of the nasion-sella and nasion-point A lines; 2. U1-palatal plane angle (U1-PP): angle formed by the intersection of the long axis of the maxillary incisor and the anterior nasal spine-posterior nasal spine line; 3. Three-dimensional position of the root: perpendicular distance from the Maxillary incisor root apex to the reference plane; 4. Three-dimensional position of the point A: perpendicular distance from point A to the reference plane; 5. Three-dimensional position of the crown: perpendicular distance from the incisal edge of the maxillary incisor to the reference plane.
Figure 2.

Three-dimensional reference plane.
To calculate systematic and random errors, 10 subjects were randomized retraced, and landmarks were retraced 3 weeks after the first measurement. All measurements were repeated to estimate the repeatability of the measurements. Systematic error was not statistically significant. The random measurement error was calculated according to Dahlberg mention method. For linear and angular measurements, the error varied between 0.22 mm and 1.01 degrees; 0.16 mm and 0.38 degrees, respectively. It revealed that there was no any random measurement error.
Statistical analysis
Data analysis was performed by SPSS for Windows, version 14.0 (SPSS Inc, Chicago, III). The differences for the age, gender, and treatment time were measured using chi-square test. Means and standard deviation between the pretreatment and posttreatment measurements were studied using Wilcoxon paired t-test. Differences between groups were analyzed by Mann-Whitney U-test. The level of significance was set at P < 0.05.
Results
There were no ages and gender differences for the subjects between the two groups. The mean treatment times also did not exhibit difference between two groups (23.64 months vs 22.65 months, p = 0.884).
SNA
The changes in SNA degree were observed to be 0.9 and 0.08 degrees in the study and control groups, respectively. The difference between T1 and T2 measurements for both groups was statistically nonsignificant, Table 1. The change in SNA between the groups was found to be significant, Table 2.
Table 1.
Treatment changes in study and control groups
| Measurement | Class II Division 2 Group (Mean+SD) | Sig | Control Group (Mean+SD) | Sig | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| T1 | T2 | T2-T1 | P | T1 | T2 | T2-T1 | P | |||
| SNA, degree | 80.25 + 3.45 | 79.35 + 3.15 | -0.9 + 1.56 | 564 | NS | 80.23 + 3.14 | 79.73 + 4.12 | -0.05+ 0.85 | 0.92 | NS |
| U1-PP, degree | 95.56 + 2.35 | 111.81 + 3.46 | 15.25 + 2.13 | 0.001 | *** | 110.35 + 4.36 | 112.56 + 2.89 | 2.21 + 1.89 | 0.86 | NS |
| N-U1Ap (x), mm | 1.25 + 1.02 | -1.70 + 1011 | -2.95 + 1.36 | 0.001 | *** | 1.82 + 0.98 | 1.97 + 1.13 | 0.15 + 0.68 | 0.785 | NS |
| N-U1Ap (y), mm | 71.13 + 3.33 | 71.25 + 5.32 | 0.12 + 0.13 | 0.895 | NS | 70.22 + 4.20 | 70.32 + 4.22 | 0.08 + 0.12 | 0.688 | NS |
| N-U1Ap (z), mm | 0.31 + 0.36 | 0.35 + 0.44 | 0.04 + 0.10 | 0.457 | NS | 0.37 + 0.18 | 0.40 + 0.23 | 0.03 + 0.12 | 0.657 | NS |
| N-U1Ed (x), mm | 9.60 + 2.13 | 15.83 + 2.65 | 6.23 + 2.13 | 0.001 | *** | 7.38 + 1.46 | 7.68 + 1.23 | 0.3 + 1.12 | 0.768 | NS |
| N-U1Ed (y), mm | 81.58 + 4.56 | 80.35 + 4.32 | -1.23 + 1.46 | 0.921 | NS | 80.40 + 4.22 | 80.55 + 3.88 | 0.15 + 0.68 | 0.920 | NS |
| N-U1Ed (z), mm | 6.84 + 1.87 | 7.05 + 1.58 | 0.21 + 0.45 | 0.687 | NS | 6.21 + 1.46 | 6.35 + 1.25 | 0.14 + 0.32 | 0.864 | NS |
| N-A (x), mm | 0.56 + 0.33 | -0.68 + 0.45 | -1.24 + 1.23 | 0.001 | *** | 0.23 + 0.36 | 0.05 + 0.24 | -0.18+ 0.87 | 0.38 | NS |
| N-A (y), mm | 60.08 + 0.16 | 60.42 + 0.45 | 0.34 + 0.12 | 0.842 | NS | 60.17 + 0.22 | 60.33 + 0.28 | 0.16 + 0.22 | 0.902 | NS |
| N-A (z), mm | 0.13 + 0.32 | 0.23 + 0.45 | 0.10 + 0.22 | 0.642 | NS | 0.18 + 0.35 | 0.20 + 0.32 | 0.08 + 0.12 | 0.657 | NS |
P < 0.001;
NS indicates not significant.
Table 2.
Comparison of treatment changes between study and control groups for angular and linear measurements
| Measurement | Class II Division 2 Group | Control Group | P | Sig | ||
|---|---|---|---|---|---|---|
|
| ||||||
| T2-T1 | T2-T1 | |||||
|
| ||||||
| Mean | SD | Mean | SD | |||
| SNA, degree | -0.9 | 1.56 | -0.05 | 0.85 | 0.023 | ** |
| U1-PP, degree | 15.25 | 2.13 | 2.21 | 1.89 | 0.001 | *** |
| N-U1Ap (x), mm | -2.95 | 1.36 | 0.15 | 0.68 | 0.001 | *** |
| N-U1Ap (y), mm | 0.12 | 0.13 | 0.08 | 0.12 | 0.662 | NS |
| N-U1Ap (z), mm | 0.04 | 0.10 | 0.03 | 0.12 | 0.821 | NS |
| N-U1Ed (x), mm | 6.23 | 2.13 | 0.3 | 1.12 | 0.001 | *** |
| N-U1Ed (y), mm | -1.23 | 1.46 | 0.15 | 0.68 | 0.001 | *** |
| N-U1Ed (z), mm | 0.21 | 0.45 | 0.14 | 0.32 | 0.435 | NS |
| N-A (x), mm | -1.24 | 1.23 | -0.18 | 0.87 | 0.001 | *** |
| N-A (y), mm | 0.34 | 0.12 | 0.16 | 0.22 | 0.624 | NS |
| N-A (z), mm | 0.10 | 0.22 | 0.08 | 0.12 | 0.620 | NS |
P < 0.05;
P < 0.001;
NS indicates not significant.
U1-PP
The maxillary incisor proclination (U1-PP) was found to be 15.25 degrees and 2.21 degrees for the study and control groups, respectively. The difference between the two measurements performed pre and post treatment (T2-T1) was statistically significant in the study group and nonsignificant in the control group, Table 1. The difference between the two groups was statistically significant, Table 2.
Incisal edges
Linear measurements evaluating the incisal positional changes showed that the incisal apex positional mainly backward and crown forward in both group. Incisal edges of maxillary incisors were moved forward 6.23 mm in the study group, which was statistically significant, Table 1. Statistically non-significant forward movement of 0.3 mm was observed in the control group, Table 1. The difference for the horizontal movement of the incisal edge between the two groups was statistically significant, Table 2. The apex of maxillary incisors was moved backward 2.95 mm and 0.15 mm in the study and control groups, respectively. The movement in the study group was statistically significant, while it was nonsignificant in the control group, Table 1. The difference between the two groups was also statistically significant, Table 2. The local vertical and Z displacement was not statistically significant in both groups, the difference between the two groups was also not statistically significant, Table 2.
Three-dimensional change of A
Assessment of local changes in point A revealed that the position of point A had moved mainly backward in study group. The local vertical and Z displacement was not statistically significant in both groups, but the local horizontal displacement, the difference between the two groups was statistically significant, the A point moved 0.18 mm and 1.24 mm backward in the control and study groups, respectively, Table 2.
Discussion
This study aimed to determine the relationship between maxillary incisor inclination change and the position of point A using CBCT in Class II division 2 malocclusions. Although a number of studies have already evaluated the sagittal position of point A using 2D images, the present study allowed a new imaging technique to record the 3D anatomy of the craniofacial region.
The main goal of imaging is to replicate the anatomic truth to show the 3D anatomy. To reduce costs and risk, orthodontists routinely use 2D static imaging techniques to record the 3D anatomy of the craniofacial region. The conventional two-dimensional imaging methods show that there was no relationship between the position of point A and proclination of the upper incisors in previous studies [6,7]. However, CBCT images could provide a more accurate analysis of treatment results [17-20].
Besides imaging techniques, there was still other limited, according to the previous studies [6-11]. Not only no sample size calculation, lack of a control group, but inability to exclude the effect of growth which facts contribute to the remodeling of point A. Therefore, in this study we calculated the sample size to derive the number of subjects that would give a 90% power of detecting a clinically important change at the 5% level of significance. The minimum number of subjects required was 35. More subjects than this were used to ensure that the results of this study would be as robust as possible and to provide a high level evidence association with the position and maxillary incisor inclination. We finally included 80 patients in order to reduce the impact of drop-out on the results.
Furthermore, The ages of subjects were not homogeneous which range from 13-35 years old and the lack of a control group weak the evidence of the previous studies evaluating the relationship between maxillary incisor inclination and point A. In the present study, we perform the study on non-growing patients in order to eliminate the effect of growth on the sagittal position of point A and the subjects whose maxillary incisor inclinations changed slightly during orthodontic treatment formed control group.
In this study, the total change in the position of the incisal edge was moved 6.23 mm forward, while the apex moved 2.95 mm backward after alignment, which results in 15.25 proclination. This change result in the position of point A moved 1.24 mm backward, this change was statistically significant; and downward by 0.34 mm, although this change was not statistically significant. These findings are coincident with those of Cangialosi and Meistrell [4] who examined the effect of lingual root torque on the sagittal position of point A and showed that 3.5 mm posterior movement of the apex and 1.62 mm forward movement of the incisal edge of the maxillary incisors resulted in 1.7 mm posterior movement of point A. It was demonstrated that point A follows the apex of the upper incisors, however by as much as half. This finding is in accordance with the results of the present study indicating that point A moved 1.24 mm, while the apex of the maxillary incisors moved 2.95 mm backward.
The results of this research are in agreement with those of Erverdi [5] and Arvysts [21,22]. Who found that incisor inclination will result in change of the position of point A. Findings also are consistent with the suggestion of Nanda [3] that “it is important to remember that point A is affected by dento-alveolar movement”.
In the present study, 1.24 mm posterior movement of point A led to 0.9 degrees decrease in the SNA angle, which was found significant. This similar to the studies that 1 mm backward movement of A point resulted in nearly 1 degree decrease in the SNA angle [23-25], the reason was that they included growth patients whose nasion moves in a downward direction, then the inclination of the sella-nasion line (cranial base) will change, and this would lead to a more obtuse SNA angle. In the present study, nasion was stability in adult patients, so it could be considered that the posterior movement of point A which resulted from bone remodeling associated with orthodontic tooth movement could lead to a real significant decrease in SNA angle.
Results of our study also show that the SNA angle actually significantly change during treatment, this similar to the findings of Cleall and BeGole [11] who applied extraoral traction to correct the molar relationship and found that the cephalometric data before and after treatment of Class II division 2 malocclusion indicated that the SNA angle was reduced by a mean of 1.6 degrees. The reason was that the greater proclination in the incisors, the greater posterior movement of the root apices, and, consequently, the greater bone remodeling.
However, the majority of the studies evaluating the relationship between the sagittal position of point A and the SNA angle show that, despite bone remodeling, the SNA angle actually did not significantly change during treatment by cephalometric measurement. The possibly main reason was that their study lack of control. Because it is difficult to have a statistically significant difference in the change of 1 degree SNA compare to normal value which about 80 degrees in included patients. Therefore, this study included subjects who required minimal maxillary anterior tooth movement found that the impact of incisor inclination on point A remodeled is statistically significant. Furthermore, the limitation of traditional cephalometric, such as distortion and magnification, may also contribute to their results.
In conclusions, proclination of maxillary incisors accompanied by backward movement of incisor root apex caused posterior movement of point A. This posterior movement significantly affects the SNA angle.
Acknowledgements
The authors wish to thank Professor Peter for checking English in this study.
Disclosure of conflict of interest
None.
References
- 1.Westwood PV, McNamara JA Jr, Baccetti T, Franchi L, Sarver DM. Long-term effects of Class III treatment with rapid maxillary expansion and facemask therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2003;123:306–320. doi: 10.1067/mod.2003.44. [DOI] [PubMed] [Google Scholar]
- 2.Siqueira DF, de Almeira RR, Janson G, Brandao AG, Coelho Filho CM. Dentoskeletal and soft-tissue changes with cervical headgear and mandibular protraction appliance therapy in the treatment of Class II malocclusions. Am J Orthod Dentofacial Orthop. 2007;131:447, e21–430. doi: 10.1016/j.ajodo.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 3.Nanda R. Biomechanics and Esthetic Strategies in Clinical Orthodontics. Philadelphia: WB Saunders Co; 2005. [Google Scholar]
- 4.Cangialosi TJ, Meistrell ME Jr. A cephalometric evaluation of hard- and soft-tissue changes during the third stage of Begg treatment. Am J Orthod. 1982;81:124–129. doi: 10.1016/0002-9416(82)90036-7. [DOI] [PubMed] [Google Scholar]
- 5.Erverdi N. A cephalometric study of changes in point A under the influence of upper incisor inclinations. J Nihon Univ Sch Dent. 1991;33:160–165. doi: 10.2334/josnusd1959.33.160. [DOI] [PubMed] [Google Scholar]
- 6.Al-Abdwani R, Moles DR, Noar JH. Change of incisor inclination effects on points A and B. Angle Orthod. 2009;79:462–467. doi: 10.2319/041708-218.1. [DOI] [PubMed] [Google Scholar]
- 7.Al-Nimri KS, Hazza’a AM, Al-Omari RM. Maxillary incisor proclination effect on the position of point a in class II division 2 malocclusion. Angle Orthod. 2009;79:880–884. doi: 10.2319/082408-447.1. [DOI] [PubMed] [Google Scholar]
- 8.Goldin B. Labial root torque: effect on the maxilla and incisor root apex. Am J Orthod Dentofacial Orthop. 1989;95:208–219. doi: 10.1016/0889-5406(89)90051-6. [DOI] [PubMed] [Google Scholar]
- 9.van der Linden FP. A study of roentgenocephalometric bony landmarks. Am J Orthod. 1971;59:111–125. doi: 10.1016/0002-9416(71)90044-3. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell DL, Kinder JD. A comparison of two torquing techniques on the maxillary central incisor. Am J Orthod. 1973;63:407–413. doi: 10.1016/0002-9416(73)90145-0. [DOI] [PubMed] [Google Scholar]
- 11.Cleall JF, BeGole EA. Diagnosis and treatment of class II division 2 malocclusion. Angle Orthod. 1982;52:38–60. doi: 10.1043/0003-3219(1982)052<0038:DATOCI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Houston WJ. The analysis of errors in orthodontic measurements. Am J Orthod. 1983;83:382–390. doi: 10.1016/0002-9416(83)90322-6. [DOI] [PubMed] [Google Scholar]
- 13.Battagel JM. A comparative assessment of cephalometric errors. Eur J Orthod. 1993;15:305–314. doi: 10.1093/ejo/15.4.305. [DOI] [PubMed] [Google Scholar]
- 14.Kamoen A, Dermaut L, Verbeeck R. The clinical significance of error measurement in the interpretation of treatment results. Eur J Orthod. 2001;23:569–578. doi: 10.1093/ejo/23.5.569. [DOI] [PubMed] [Google Scholar]
- 15.Kumar V, Ludlow J, Soares Cevidanes LH, Mol A. In vivo comparison of conventional and cone beam CT synthesized cephalograms. Angle Orthod. 2008;78:873–879. doi: 10.2319/082907-399.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lamichane M, Anderson NK, Rigali PH, Seldin EB, Will LA. Accuracy of reconstructed images from cone-beam computed tomography scans. Am J Orthod Dentofacial Orthop. 2009;136:156, e151–156. doi: 10.1016/j.ajodo.2009.04.006. discussion 156-157. [DOI] [PubMed] [Google Scholar]
- 17.Dudic A, Giannopoulou C, Leuzinger M, Kiliaridis S. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofacial Orthop. 2009;135:434–437. doi: 10.1016/j.ajodo.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 18.Patel S, Dawood A, Wilson R, Horner K, Mannocci F. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography- an in vivo investigation. Int Endod J. 2009;42:831–838. doi: 10.1111/j.1365-2591.2009.01592.x. [DOI] [PubMed] [Google Scholar]
- 19.Durack C, Patel S, Davies J, Wilson R, Mannocci F. Diagnostic accuracy of small volume cone beam computed tomography and intraoral periapical radiography for the detection of simulated external inflammatory root resorption. Int Endod J. 2011;44:136–147. doi: 10.1111/j.1365-2591.2010.01819.x. [DOI] [PubMed] [Google Scholar]
- 20.Lund H, Grondahl K, Grondahl HG. Cone Beam Computed Tomography for Assessment of Root Length and Marginal Bone Level during Orthodontic Treatment. Angle Orthod. 2010;80:466–473. doi: 10.2319/072909-427.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arvystas MG. Nonextraction treatment of severe Class II, Division 2 malocclusions. Part 1. Am J Orthod Dentofacial Orthop. 1990;97:510–521. doi: 10.1016/S0889-5406(05)80032-0. [DOI] [PubMed] [Google Scholar]
- 22.Arvystas MG. Nonextraction treatment of severe Class II, division 2 malocclusions. Part 2. Am J Orthod Dentofacial Orthop. 1991;99:74–84. doi: 10.1016/S0889-5406(05)81683-X. [DOI] [PubMed] [Google Scholar]
- 23.Weber FN. Clinical investigations related to use of the Begg technique at the University of Tennessee. Am J Orthod. 1971;59:24–36. doi: 10.1016/0002-9416(71)90213-2. [DOI] [PubMed] [Google Scholar]
- 24.Barton JJ. A cephalometric comparison of cases treated with edgewise and Begg techniques. Angle Orthod. 1973;43:119–126. doi: 10.1043/0003-3219(1973)043<0119:ACCOCT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Venezia AJ. Pure Begg and edgewise arch treatments: comparison of results. Angle Orthod. 1973;43:289–300. doi: 10.1043/0003-3219(1973)043<0289:PBAEAT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]


