Abstract
A decline in cognitive ability commonly occurs among older individuals. This study sought to explore the restorative effects of exercise in older patients with existing cognitive disabilities. Ninety-six patients with mild cognitive impairment were placed in an exercise program for six months. Following completion of the program, participants were assessed via the Chinese Mini Mental Status Examination (MMSE), Activity of Daily Living (ADL) assessment, and body movement testing and compared to a control group of patients with mild cognitive impairment who did not participate in the exercise program (N = 102). Statistical analyses were performed using the Student’s t-test and chi-square test to compare results between groups. Compared with control group, patients who exercised showed improved cognitive function in immediate memory (p < 0.001) and delayed recall (p = 0.004) function. In addition, activities associated with daily living showed improvement (p < 0.001), as did body movement (p < 0.05), arm stability (p < 0.001), and the appearance of rotation (p < 0.05). Based on these results, we conclude that participation in an exercise program can improve patients’ cognitive function, physical abilities, and body movement capacity.
Keywords: Aging, mild cognitive impairment, exercise, cognitive function, dementia
Introduction
As brain function declines with age, so does cognitive function. Cognitive decline represents the decreased ability of the human brain to store, process, and extract information, manifested as decreases in executive function, language understanding and expression, cognitive and processing speed, learning, and memory [1]. As the average human lifespan increases and the world’s aging population grows, issues surrounding the health and care of the aging is gaining increasing attention. Cognitive impairment is an early sign of dementia, and no successful treatment options have yet been identified for senile dementia. Early detection and intervention are essential to help slow the progress of cognitive decline. Previous studies have reported that early exercise intervention can improve cognitive function and significantly improve quality of life [2,3]. In this study, we conducted a longitudinal survey of a group of aging patients between March and December of 2013 to explore the effect of an exercise program on cognitive function.
Subjects and methods
Study participants
This longitudinal study recruited 1362 individuals ages 65 years and over who were randomly selected from a community home between March and May 2013. Any patients exhibiting respiratory, cardiovascular, or metabolic diseases or other severe illness were excluded from the study, as were physical education teachers and servicemen who had existing exercise habits. After exclusion, 1106 individuals (504 males and 602 females, ages 65 to 86 years) completed the survey. The mean age of survey participants was 70.03 ± 10.51 years. Participants were screened using the Chinese Mini Mental Status Examination (MMSE) and 204 participants were found to have mild cognitive impairment. From these, 102 subjects with mild cognitive impairment were randomly selected for the experimental group, while the remaining 102 were assigned to the control group. There was no significant difference in age, gender, education level, or marital status between the two groups (p > 0.05). The study design was approved by the ethics committee of the community home. All subjects and their families provided written informed consent.
General participant information
A general information questionnaire was used to collect information on gender, age, marital status, education level, and history of coronary heart disease, hypertension, diabetes, and surgery.
Assessment of cognitive function
The Chinese Mini Mental Status Examination (MMSE), prepared by Folstein et al., is a widely used screening tool used in the examination and diagnosis of cognitive deficit [4]. MMSE is used to evaluate time, orientation, immediate memory, attention and calculation ability, short-term memory, language repeating, reading comprehension, presentation skill, operational capabilities, and other cognitive skills. The exam is able to distinguish between the normal characteristics of aging people and those of dementia patients [5]. The overall scores ranged from 0 to 30 points, depending on education level: illiteracy (uneducated) ≤ 19 points, elementary school (≤ 6 years of education) ≤ 22 points, and secondary school and above (> 6 years of education) ≤ 26 points were considered as cognitive impairment. Illiteracy 17-19 points, elementary school 20-22 points, secondary school and above 24-26 points were considered as mild cognitive impairment. Illiteracy < 17 points, elementary school < 20 points, and secondary school and above < 24 points, were considered as severe cognitive impairment. All neurocognitive assessments were performed by senior physicians.
Assessment of daily living activities
The revised Activity of Daily Living Scale (ADL) [6] was used to assess operational abilities. A score of 1 point was considered as normal, while 2-4 points were considered as functional decline. A score of 20 indicated completely normal function, and more than 20 points indicated functional decline of different degrees. Some contents in ADL, for example, those who could not take a bus or go shopping due to inability of observing or performing can be evaluated based on other contents that had been completed, or may be asked to complete a separate project to replace the scores.
Measurements of somatic movement
The following tools were used to collect information on somatic movement: a DDX-200 computer multifunction tester for physiological and psychological capabilities, mental rotation test cards, and two stopwatches. The test procedures included: arm stability, hand-foot cross motion, and mental rotation, in which the experimenter randomly presents cards of different rotation angles between 60° and 300° and the subjects are timed in their ability to turn the cards back to 300°. All cards were used 3 times, and the average time obtained.
Exercise training for those with mild cognitive impairment
The 102 subjects with mild cognitive impairment in the experimental group participated in an exercise program for six months between July and December 2013. Before training, 204 subjects with mild cognitive impairment underwent MMSE, ADL assessment, and somatic movement assessment to provide a baseline measurement of ability. The exercise program consisted of jogging for 30 minutes and shadowboxing for 60 minutes once a week. Exercise sessions were supervised by professional staff that provided encouragement and support throughout the program. Six participants dropped out of the program, two due to foot injuries and four due to loss of interest. After completion of the six month program, 96 program participants and 102 control individuals underwent MMSE, ADL assessment, and of somatic movement assessment for a second time.
Statistical methods
Data were entered into an Epidata 3.1 (The Epidata Association, Odense, Denmark) database using double entry method and logic checks. Data were analyzed using SAS 9.2 (SAS Institute, Inc., Cary, North Carolina, USA). Student’s t-test and the x2 test were applied for identifying differences between groups. A P value < 0.05 was considered statistically significant.
Results
Participant demographics
The study included 1106 individuals, 504 males (45.57%) and 602 females (54.43%), ages 65 to 86 years (mean age 70.03 ± 10.51 years). Initial MMSE screening revealed 851 subjects with normal cognitive function, 204 subjects with mild cognitive impairment, and 51 subjects with moderate to severe cognitive impairment. The overall incidence of cognitive impairment was 23.06%. There were statistically significant differences in the distribution of age and gender among those with normal cognitive function, mild cognitive impairment, and moderate to severe cognitive impairment (P < 0.001; Table 1).
Table 1.
Study participant demographics at baseline
| Characteristic | Normal cognitive function (N = 851) | Mild cognitive impairment (N = 204) | Moderate to severe cognitive impairment (N = 51) | χ2 | p |
|---|---|---|---|---|---|
| Age (y) | 43.20 | < 0.001 | |||
| 65-75 | 571 (67.1%) | 91 (44.61%) | 22 (43.14%) | ||
| 76-86 | 280 (32.9%) | 113 (55.39%) | 29 (56.86%) | ||
| Gender | 49.32 | < 0.001 | |||
| Male | 408 (47.94%) | 149 (73.04%) | 37 (72.55%) | ||
| Female | 443 (52.06%) | 55 (26.96%) | 14 (27.45%) |
MMSE scores of subjects with mild cognitive impairment improve with exercise
The cognitive function of study participants with mild cognitive impairment was improved after participation in the exercise program. Improvement was seen in both immediate memory (p < 0.001) and delayed recall (p = 0.004) (Table 2; Figures 1, 2, 3, 4 and 5).
Table 2.
Cognitive function scores among study participants with mild cognitive impairment (X̅ ± s)
| Group | Directional force | Immediate memory | Calculation ability | Delayed recall | Language and structure understanding |
|---|---|---|---|---|---|
| Control (n = 102) | 9.03 ± 1.72 | 2.11 ± 0.76 | 2.68 ± 1.40 | 1.62 ± 1.10 | 7.75 ± 1.59 |
| Experimental (n = 96) | 9.35 ± 2.04 | 2.58 ± 0.71 | 3.02 ± 1.21 | 2.06 ± 1.03 | 8.05 ± 1.94 |
| t | -1.20 | -4.49 | -1.82 | -2.90 | -1.19 |
| p | 0.233 | < 0.001 | 0.070 | 0.004 | 0.234 |
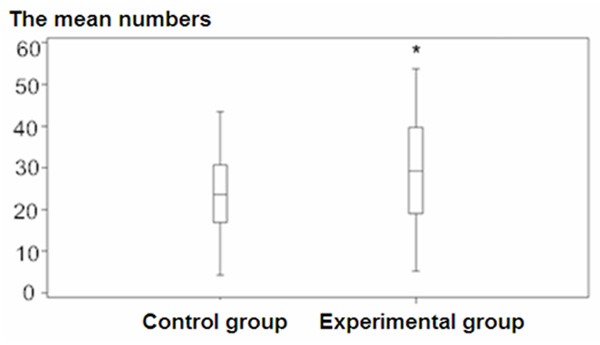
Figure 1.
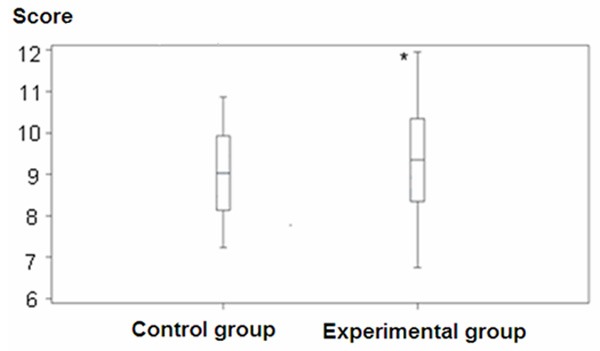
Directional force among study participants (*p < 0.05).
Figure 2.
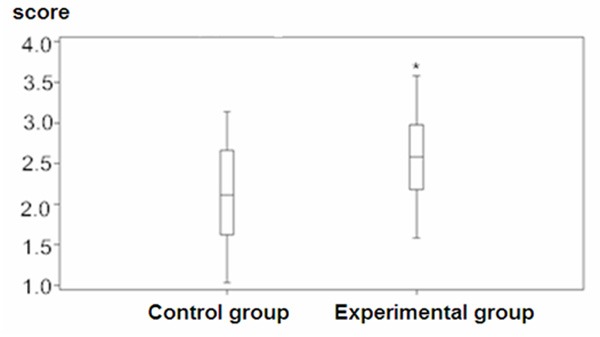
Immediate memory among study participants (*p < 0.05).
Figure 3.
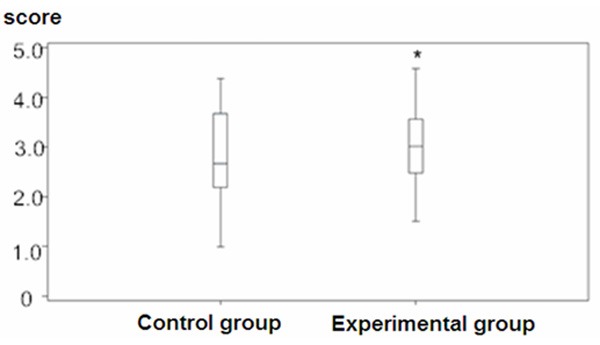
Calculation ability scores among study participants (*p < 0.05).
Figure 4.
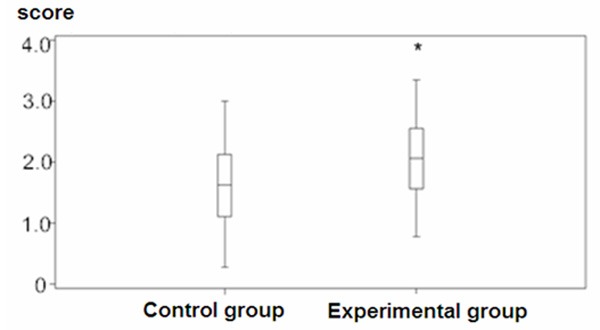
Delayed recall scores among study participants (*p < 0.05).
Figure 5.
Language and structure understanding scores among study participants (*p < 0.05).
ADL scores of subjects with mild cognitive impairment improve with exercise
After participation in the exercise program, the mean ADL was 28.58 ± 2.97, while the mean ADL in the control group was 32.79 ± 3.25. Thus, measurements of daily life abilities in the experimental group were also improved compared to the control group (t = 9.50, p < 0.001).
Somatic movement improves following participation in an exercise program
The somatic movement of participants with mild cognitive impairment was significantly improved after exercise training intervention. Specifically, measurements of the time of hand-foot cross motion (p = 0.013), correct number of times of hand-foot cross motion (p = 0.021), average time of hand-foot motion (p = 0.011), arm stability (p < 0.001), and mental rotation (p = 0.019), were all significantly improved (Table 3, Figures 6, 7, 8, 9 and 10).
Table 3.
Body movement analysis (X̅ ± s)
| Variables | Control group (n = 102) | Experimental group (n = 96) | T | p |
|---|---|---|---|---|
| A (s) | 796.72 ± 338.26 | 679.64 ± 314.37 | 2.52 | 0.013 |
| B | 30.83 ± 14.21 | 35.43 ± 13.53 | -2.33 | 0.021 |
| C (s) | 23.60 ± 12.97 | 29.25 ± 17.61 | -2.58 | 0.011 |
| D (min) | 10.59 ± 6.87 | 14.92 ± 7.37 | -4.28 | < 0.001 |
| E (s) | 2.23 ± 1.05 | 1.91 ± 0.83 | 2.37 | 0.019 |
A: Total numbers of the hands and feet crossover, B: The correct numbers of the hands and feet crossover, C: The mean numbers of the hands and feet movement, D: Arm stability, E: The appearance of rotation.
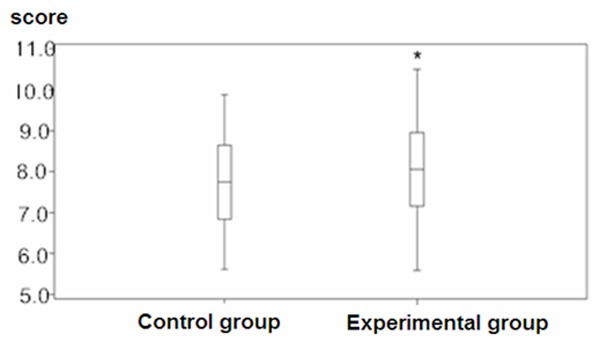
Figure 6.
Total numbers of the hands and feet crossover test (*p < 0.05).
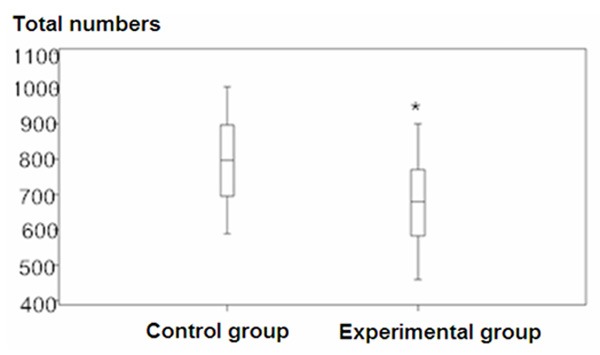
Figure 7.
Correct numbers of the hands and feet crossover test (*p < 0.05).
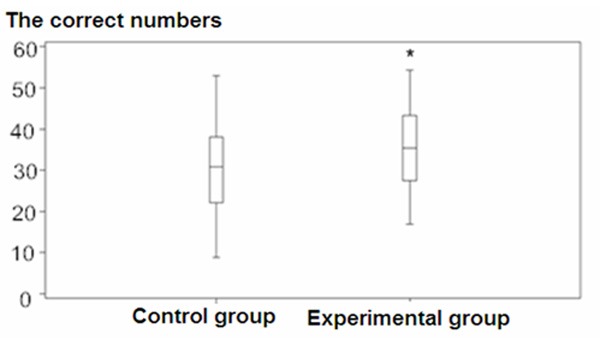
Figure 8.
Mean numbers of the hands and feet movement test (*p < 0.05).
Figure 9.
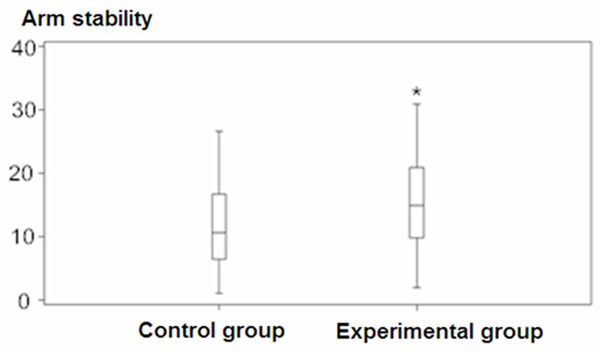
Arm stability among study participants (*p < 0.05).
Figure 10.
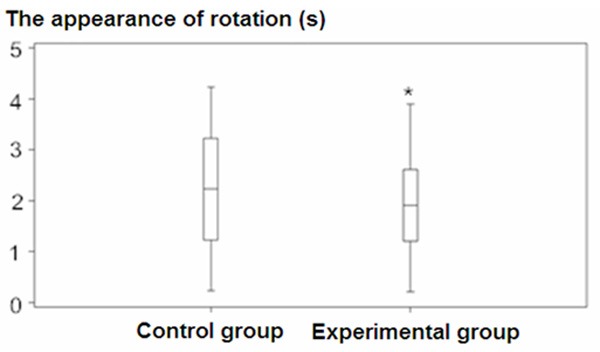
Appearance of rotation (*p < 0.05).
Discussion
With aging, the brain undergoes physical changes leading ultimately to cognitive impairments of varying degrees. Cognitive function can range from mild to severe cognitive impairment (Alzheimer’s disease). Recent reports in China indicate that the incidence of mild cognitive impairment is up to 10%-30% [7] and about 15% of cases of mild cognitive impairment evolve into Alzheimer’s disease every year [8]. The cognitive function of patients with Alzheimer’s disease is severely impaired and accompanied by abnormal behavior, which takes a toll on the quality of life of the individual and on those who care for them [8]. As such, early intervention for cognitive function decline in aging people must be prioritized.
In this study, the cognitive function of individuals with mild cognitive impairment was improved after six months of exercise training. Specifically, improvement in the immediate memory and delayed recall was seen along with improvement in daily living activities. Somatic movement was also improved and there was significant improvement in the overall time of hand-foot cross motion, correct number of times of hand-foot cross motion, average time of hand-foot motion, arm stability, and mental rotation. These results are similar to those obtained by Guiney, Zhang, Nannan, and Scherder et al. [2,9,10]. Baker et al. [11] have reported that, after six months of aerobic and stretching exercises, aging patients with cognitive impairment improved in the accuracy in verbal fluency test and in the number of correct answers in the 120 s in Symbol Digit Modality Test.
Shadowboxing, qigong (a Chinese kung fu), and several other comprehensive activities involve aerobic exercise, flexibility, and energy. Studies have shown that long-term shadowboxing is conducive to the protection of cognitive function of the aging [12]. Aerobic activities are hypothesized to delay encephalatrophy in specific areas of the brain, thereby preserving cognitive function [13]. Exercise may also help to reduce cardiovascular risk factors (such as hypertension) and thus relieve brain ischemia and hypoxia and preserve white matter [14]. In addition, cognitive function in the aging is associated with changes in hippocampal volume of the brain. Erickson et al. investigated the effect of one year of walking therapy on spatial memory of 55-80 year olds, and found that the left and right hippocampal volume increased and that the fore-hippocampus area was selectively activated [15]. The accuracy of spatial memory tasks were likely related to changes in the left and right hippocampal volumes. Even among healthy older individuals, hippocampal volume shrinks at an annual rate of 1% to 2%, thus increasing the risk of Alzheimer’s and mild cognitive impairment. Erickson’s study suggests that aerobic exercise intervention can effectively increase hippocampal volume, and combat the natural degeneration rate.
In summary, the results of this study indicate that participation in an active exercise program can effectively improve cognitive function among aging patients with mild cognitive impairment and help to combat the onset of dementia. Encouraging older individuals to participate in activities such as jogging, shadowboxing, and other aerobic exercises can help to improve cognitive function, activities of daily life, and somatic movement, allowing patients to preserve their independence and quality of life. This serves not only to improve upon the individual’s overall sense of well-being and physical health, but also to offset the burden on caretakers and family members responsible for their care.
Acknowledgements
This work was supported by Science and Technology Department of Henan Province (Number: 142700410395).
References
- 1.Boyle PA, Wilson RS, Yu L, Barr AM, Honer WG, Schneider JA, Bennett DA. Much of late life cognitive decline is not due to common neurodegenerative pathologies. Ann Neurol. 2013;74:478–489. doi: 10.1002/ana.23964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guiney H, Machado L. Benefits of regular aerobic exercise for executive functioning in healthy populations. Psychon Bull Rev. 2013;20:73–86. doi: 10.3758/s13423-012-0345-4. [DOI] [PubMed] [Google Scholar]
- 3.Smith JC, Nielson KA, Woodard JL, Seidenberg M, Rao SM. Physical activity and brain function in older adults at increased risk for Alzheimer’s disease. Brain Sci. 2013;3:54–83. doi: 10.3390/brainsci3010054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang MY. Mini-mental state examination, Psychiatric Assessment Scale Manual. 2nd edition. Chang sha: Hunan Science and Technology Press; 1998. pp. 184–188. (In Chinese) [Google Scholar]
- 5.Mitchell AJ. A meta-analysis of the accuracy of the mini-mental state examination in the detection of dementia and mild cognitive impairment. J Psychiatr Res. 2009;43:411–431. doi: 10.1016/j.jpsychires.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Zhou WJ, Sun QL. Paralysis rehabilitation assessment manual. Beijing: People’s Health Publishing House; 2006. pp. 46–50.pp. 120–121. [Google Scholar]
- 7.Ma YX, Yu ZW. Contemporary Dementia Medicine. Shanghai: Scientific and Technical Documentation Press; 2008. pp. 342–348. [Google Scholar]
- 8.Varela S, Ayán C, Cancela JM, Martin V. Effects of two different intensities of aerobic exercise on elderly people with mild cognitive impairment: a randomized pilot study. Clin Rehabil. 2012;26:442–450. doi: 10.1177/0269215511425835. [DOI] [PubMed] [Google Scholar]
- 9.Zhang NN, Lv XB, Ni W. Effect of long-term Tai Chi exercise on cognitive function of middle-aged and old people. Chinese Journal of Clinical Rehabilitation. 2006;10:7–9. [Google Scholar]
- 10.Scherder EJ, Eggermont LH, Geuze RH, Vis J, Verkerke GJ. Quadriceps strength and executive functions in older women. Am J Phys Med Rehabil. 2010;89:458–463. doi: 10.1097/PHM.0b013e3181d3e9f6. [DOI] [PubMed] [Google Scholar]
- 11.Baker LD, Frank LL, Foster-Schubert K, Green PS, Wilkinson CW, McTiernan A, Plymate SR, Fishel MA, Watson GS, Cholerton BA, Duncan GE, Mehta PD, Craft S. Effects of aerobic exercise on mild cognitive impairment: a controlled trial. Arch Neurol. 2010;67:71–79. doi: 10.1001/archneurol.2009.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor-Piliae RE, Newell KA, Cherin R, Lee MJ, King AC, Haskell WL. Effects of Tai Chi and Western exercise on physical and cognitive functioning in healthy community-dwelling older adults. J Aging Phys Act. 2010;18:261–279. doi: 10.1123/japa.18.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinstein AM, Voss MW, Prakash RS, Chaddock L, Szabo A, White SM, Wojcicki TR, Mailey E, McAuley E, Kramer AF, Erickson KI. The association between aerobic fitness and executive function is mediated by prefrontal cortex volume. Brain Behav Immun. 2012;26:811–819. doi: 10.1016/j.bbi.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith PJ, Blumenthal JA, Hoffman BM, Cooper H, Strauman TA, Welsh-Bohmer K, Browndyke JN, Sherwood A. Aerobic exercise and neurocognitive performance: a meta-analytic review of randomized controlled trials. Psychosom Med. 2010;72:239–252. doi: 10.1097/PSY.0b013e3181d14633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Erickson KI, Prakash RS, Voss MW, Chaddock L, Hu L, Morris KS, White SM, Wójcicki TR, McAuley E, Kramer AF. Aerobic fitness is associated with hippocampal volume in elderly humans. Hippocampus. 2009;19:1030–1039. doi: 10.1002/hipo.20547. [DOI] [PMC free article] [PubMed] [Google Scholar]


