Abstract
Objective
To evaluate the use and effectiveness of two “in-home” strategies for delivering diabetes prevention programming using cable television.
Methods
An individually randomized, two-arm intervention trial including adults with diabetes risk factors living in two US cities. Interventions involved a 16-session lifestyle intervention delivered via “video-on-demand” cable television, offered alone versus in combination with web-based lifestyle support tools. Repeated measures longitudinal linear regression with imputation of missing observations was used to compare changes in body weight.
Results
A total of 306 individuals were randomized and offered the interventions. After 5 months, 265 (87%) participants viewed at least 1, and 110 (36%) viewed ≥9 of the video episodes. A total of 262 (86%) participants completed a 5-month weight measurement. In intention-to-treat analysis with imputation of missing observations, mean weight loss at 5 months for both treatment groups combined was 3.3% (95% CI 0.7-5.0%), regardless of intervention participation (with no differences between randomized groups (P = 0.19)), and was 4.9% (95% CI 2.1-6.5%) for participants who viewed ≥9 episodes.
Conclusions
In-home delivery of evidence-based diabetes prevention programming in a reality television format, offered with or without online behavioral support tools, can achieve modest weight losses consistent with past implementation studies of face-to-face programs using similar content.
Introduction
Over the past 40 years, the burden of type 2 diabetes has escalated dramatically with increases in obesity and decreases in physical activity 1. Currently, 79 million Americans have prediabetes, and 1 in 3 infants born today will develop diabetes in their lifetimes 2,3. Fortunately, strong research such as the US Diabetes Prevention Program (DPP) has demonstrated that the rates of developing type 2 diabetes can be cut by almost 60% when high-risk adults are offered diet and exercise interventions that result, on average, in just 6.7 kg (15 pounds) of weight loss over the first 6 months of intervention 4. Even more modest weight losses have also proved clinically meaningful, with every 1 kg (2.2 pounds) of weight loss conferring a 16% decrease in the risk of diabetes development 5.
Unfortunately, most people with prediabetes remain unaware of their increased risk and the potential actions they might take to avoid developing diabetes 6. In addition, resource-intensive lifestyle programs such as the DPP are costly, with no guarantee that people will participate, even after being made aware. Many groups are confronting these challenges by developing scalable strategies for raising awareness, identifying persons who are at high risk, delivering lower cost adaptations of the DPP, and linking intervention payments to levels of participation or outcomes rather than simply to offering the program alone. Although encouraging, most of these initiatives still require the availability of a nearby intervention site, where participants need to attend multiple face-to-face visits and pay fees that may exceed $400 or more per person per year 7–9.
Given these challenges, the UnitedHealth Center for Health Reform and Modernization (UnitedHealth) partnered with Comcast® to develop and evaluate a novel “virtual” dissemination model that involves a reality-based TV lifestyle support program. One important question is whether such an approach can achieve results without the direct engagement, supportive feedback, and accountability offered by a face-to-face lifestyle coach. Hypothesizing that additional individualized support could enhance weight loss, this study compared the effectiveness of a cable TV-based DPP-like intervention alone against offering this same programming in combination with an interactive web portal that provided supplemental content, tracking tools, and a virtual lifestyle coach.
Methods
Design overview
An individually randomized, two-arm intervention trial design was used to compare changes in body weight with a Video On-Demand (VOD) delivered DPP alone (VOD-Only) versus VOD programming offered in combination with an interactive web portal (VOD-Plus). The protocol was approved by the New England Institutional Review Board in November 2011 and registered in clinicaltrials.gov (NCT01768546), with recruitment commencing in two test markets (Philadelphia, PA, and Knoxville, TN) in February 2012.
Setting and participants
Household residents were invited to participate through four, 30-second public service announcements (PSAs) and two promotional advertisements. PSAs about prediabetes were run from November 2011 through January 2012. Promos for the clinical trial were run for 4 weeks from February to March 2012, until the recruitment goal was reached. Viewers were encouraged to call a toll-free number or visit a website to learn more about the study.
Each volunteer was screened for eligibility by completing a brief web or telephone survey. A volunteer was offered participation if he/she reported being (i) 18 years of age or older; (ii) overweight or obese; and (iii) told by a healthcare provider that he/she has prediabetes or has/had one or more of the following risk factors 10: (a) high blood pressure; (b) abnormal blood cholesterol; (c) a parent or sibling who has/had type 2 diabetes; or (d) a personal history of gestational diabetes. Volunteers were advised not to participate if they reported any of the following: (i) body weight >140 kg (about 310 lb); (ii) planning bariatric surgery within 6 months; (iii) physician-diagnosed diabetes; (iv) poorly controlled high blood pressure (>180/105 mmHg); (v) being pregnant or actively planning pregnancy; (vi) symptoms of chest pain, dizziness, or severe shortness of breath with exertion; (vii) advice from a healthcare provider not to increase physical activity or attempt weight loss; or (viii) another condition that significantly limits physical activities (e.g., advanced heart or lung disease, anemia, severe arthritis). Persons with body weight greater than 140 kg were excluded because the e-scale used to capture weights (see below) had a maximum weight capacity of 150 kg.
Interventions
In collaboration with Met|Hodder, a creative media content company and Haberman, a cause-marketing firm, UnitedHealth developed a multi-episode lifestyle change and promotion program for delivery through Comcast's Xfinity® VOD interface. Xfinity is a subscription-based video communications delivery platform offering digital and high-definition viewing of user-driven, on-demand programming via a television, computer, tablet, or smartphone. UnitedHealth, Met|Hodder, and Haberman, produced a 16-episode video series mirroring the initial 4 to 6 month “core” of the DPP lifestyle intervention, involving education, behavioral goals, and problem-solving strategies as recommended by the national Diabetes Training and Technical Assistance Center 11. Episodes followed an entertainment (reality TV) format and focused on the experiences of six men and women with prediabetes, representing a mix of ages, race, and ethnicities, who actively participated in the lifestyle intervention.
All study participants were offered access to the same VOD episodes and a welcome kit, which included the cellular-enabled weight scale, instructions, and tools for tracking their diet and physical activity behaviors as they participated along in the VOD program. Participants assigned to the VOD-Only arm and those without Internet access were provided paper-tracking booklets and calorie-counting guides. Those in the VOD-Plus group were also given instructions for accessing an interactive web portal offered by SparkPeople™ (Cincinnati, OH), which included additional educational content, electronic behavioral tracking tools, social media platforms, and the option to interact with a virtual lifestyle coach, who responded to participants and group discussions via email and through online forum postings. To support ongoing participation and goal achievement, participants in both groups received weekly automated phone calls that reinforced VOD lessons. Calls were delivered once weekly during each participant's preference for morning, afternoon, or evening contact. If a call was unanswered, a message was left providing an access code that enabled the participant to call back and retrieve the support information at any time.
Randomization and blinding
After completing the baseline survey, each eligible volunteer was enrolled in the study. A computer-generated simple randomization list (generated separately for each city) then auto-assigned each participant to one of two groups: (i) VOD-Only or (ii) VOD-Plus. Although this step unblinded the intervention assignment, participants were not aware of the randomization step or that different participants might receive different information or resources.
Outcomes and follow-up
Weights were measured by a BodyTrace eScale, which transmits weight data wirelessly using a cellular network. The manufacturer reports accuracy within ±0.1 kg to a weight limit of about 150 kg (330 lb). Overall, more than 7,795 weight measures were recorded over the 12-month evaluation period (median = 16 per participant). Range and test-retest variation checks were performed to validate individual weight measures. The last valid weight captured each week was retained for analysis. For comparability to prior studies reporting outcomes following delivery of interventions adapted from the DPP (typically after 4 to 6 months of intervention), the primary study outcome was the change in body weight between baseline and about 5 months. This outcome was constructed using each participant's body weight measure nearest to the week after the 16th intervention episode had been offered (range 17-26 weeks after randomization). A secondary outcome was change in weight between baseline and 12 months, constructed using the nearest participant weight record to 52 weeks (range 46-56 weeks) after randomization. The study's informed consent process granted Comcast permission to provide household VOD viewing data and for SparkPeople to provide website analytic data (i.e., log-in and use of the web portal). Survey items (including demographic characteristics and self-reported global health) were collected at enrolment and again after 5 months using the same telephone and web strategies. Self-reported global health was assessed using the question: “In general, would you say your health is excellent; very good; good; fair; or poor?” The follow-up survey also assessed satisfaction with different intervention components. Participants received the weight scale as a gift and were given a $25 gift card after stepping on the scale for the first time and again upon completion of the follow-up survey and weight measure.
Statistical analysis
The study sample provided at least 90% power (α = 0.05) to detect as small as a 2% mean weight loss difference between study arms, assuming weight losses of 4% (SD 4%) for VOD-Plus participants and 2% (SD 4%) for VOD-Only participants and inflating for 20% attrition and to ensure that an adequate number of participants had Internet access (assumed to be 75%). The targeted sample was 151 participants per arm or about 302 overall.
All analyses were performed using Stata/MP version 12.1 (College Station, TX). VOD viewing statistics were summarized as the percentage of all participants who completed key thresholds of the numbers of episodes viewed (0; 1-3; 4-8; 9-16). Web-portal use was summarized as the percent of participants in the VOD-Plus arm reaching different levels of log-ins (0; 1; 2-10; 11-50; >50). For intention-to-treat (ITT) analysis of percentage weight changes at 5 and 12 months, weight measures were missing for 44 (14.4%) and 55 (18.0%) participants, respectively. Missing observations were multiply imputed using data augmentation, involving an iterative Markov chain Monte Carlo procedure assuming an underlying multivariable normal model. ITT analyses used longitudinal linear regression to estimate overall and between-arm differences in weight change across all time points, regardless of intervention participation. To explore associations between viewing “dose” and weight loss, a dummy variable for each viewing category was introduced into the model. Baseline values for age, sex, race/ethnicity (non-Hispanic white versus other), city, self-reported global health rating, and body weight were included as covariates in these models.
Role of the funding source
The study was funded by the UnitedHealth and Comcast. Members of these two organizations collected the data and provided it in raw format for analysis by the third party evaluator. Coauthors from these organizations contributed to the study design and offered critical revision of the manuscript.
Results
Over the 4-week recruitment period ending in March 2012, 699 individuals expressed interest in the program, and 314 were considered eligible, randomized, and sent a welcome kit. The participant flow is depicted in Figure 1.
Figure 1.
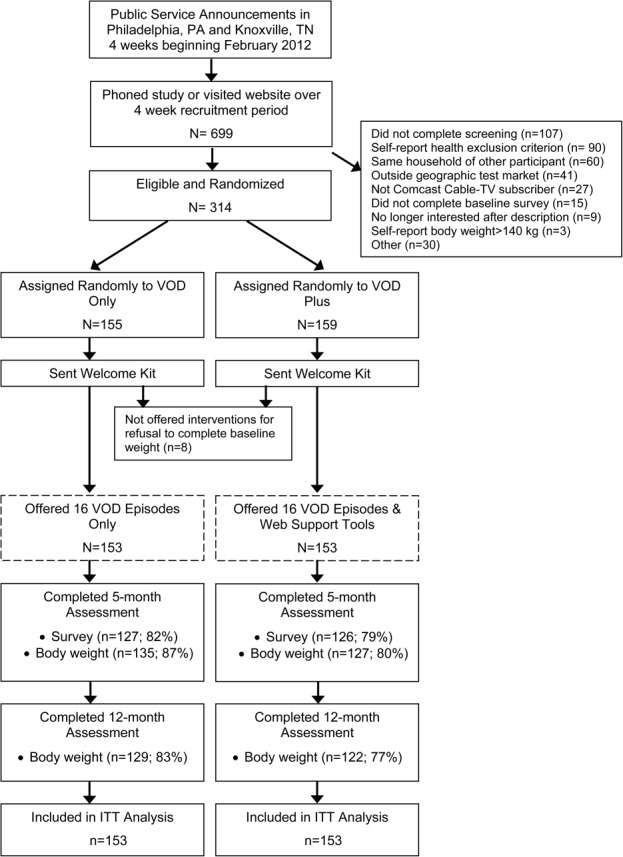
Trial participant flow.
After randomization but before the VOD program was offered, 8 volunteers (2 in VOD-Only; 6 in VOD-Plus) were unwilling to complete a baseline weigh-in. These individuals were withdrawn before being offered the VOD episodes. Baseline characteristics of all 314 randomized volunteers are summarized in Table1. Study arms were similar with respect to age, sex, race, and baseline body mass. There were modest differences in self-reported income, but 19% of participants did not answer this question, hence differences may have resulted from incomplete ascertainment. Comparisons in participant characteristics between study arms did not change after removing the 8 participants who withdrew before the intervention was offered.
Table 1.
Baseline characteristics of all randomized participants
| Characteristic | Overall (N = 314) | VOD VOD-Only (N = 155) | VOD VOD-Plus (N = 159) |
|---|---|---|---|
| Age (years) | 46.7 (SD 11.3) | 46.5 (SD 11.3) | 46.9 (SD 11.3) |
| Women | 82% | 80% | 85% |
| Body Weight (kg) | 99.2 (SD 18.4) | 100.8 (SD 18.3) | 97.6 (SD 18.4) |
| BMI (kg/m2) | 35.6 (SD 5.9) | 36.1 (SD 6.0) | 35.1 (SD 5.7) |
| Race/Ethnicity | |||
| White | 77% | 77% | 77% |
| Black | 18% | 17% | 18% |
| Hispanic | 3% | 2% | 4% |
| Family History Diabetes | 69% | 72% | 67% |
| Weight Loss Goal (kg) | 19.0 (SD 8.8) | 19.1 (SD 9.4) | 18.8 (SD 8.3) |
| Employment Status | N = 312 | N = 154 | N = 158 |
| Employed | 80.5% | 82.5% | 78.5% |
| Unemployed | 5.5% | 5.2% | 5.7% |
| Homemaker | 5.5% | 5.8% | 5.1% |
| Student | 2.6% | 1.3% | 3.8% |
| Retired | 5.1% | 4.6% | 5.7% |
| Unable to Work | 1.0% | 0.7% | 1.3% |
| Household Income | N = 255 | N = 131 | N = 124 |
| <$25,000 per year | 7.8% | 5.3% | 10.5% |
| $25--75,000 per year | 54.5% | 59.5% | 49.2% |
| >$75,000 per year | 37.7% | 35.1% | 40.3% |
| Educational Attainment | N = 308 | N = 154 | N = 154 |
| High school or less | 13.3% | 8.4% | 18.2% |
| 1- to 4 years of college | 58.1% | 63.6% | 52.6% |
| >4 years of college | 28.6% | 27.9% | 29.2% |
| Internet Access | 98.7% | 97.4% | 100% |
After 12 months, 265 (87%) of the 306 study participants offered the interventions had viewed at least one of the VOD episodes. Viewing did not differ significantly between study arms (mean 6.9 episodes for VOD-Only and 6.7 for VOD-Plus). Overall, 41 (13%) participants viewed 0 episodes; 71 (23%) completed 1-4 episodes; 84 (27%) completed 4-8 episodes; and 110 (36%) completed 9 or more episodes. Among survey responders, 87% reported being satisfied or very satisfied with the programming overall, and 93% reported they would recommend it to a friend.
Within the VOD-Plus arm, 52 participants (34%) never logged in to receive SparkPeople web resources; 13 (9%) logged in once; 33 (20%) logged in 2-10 times; 29 (19%) logged in 11-50 times; and 26 (17%) logged in 50 or more times. Among website users (n = 101), 63% reported being satisfied or very satisfied with the web resources, and 32% used a mobile device to access content. Only 11% accessed applications to track physical activities, 9% tracked calories, and 5% attempted to access virtual coaching resources. Data about usability or barriers to using different web tools were not collected.
Observed weight changes
At 5 months, 64% of the 262 participants who completed a follow-up weight had lost weight, 57% achieved 2% or more weight loss, and 33% achieved a 5% or more weight loss (Figure 2). At 12 months, 32% of the 251 participants who completed a follow-up weight maintained a weight loss of 5% or more. In unadjusted analyses of completers, the overall mean percent weight loss was 3.3% (95% CI 2.7-3.9%) at 5 months and 3.3% (95% CI 2.2-4.3%) at 12 months, with no statistically significant differences between study arms (5-month P = 0.16; 12-month P = 0.26).
Figure 2.
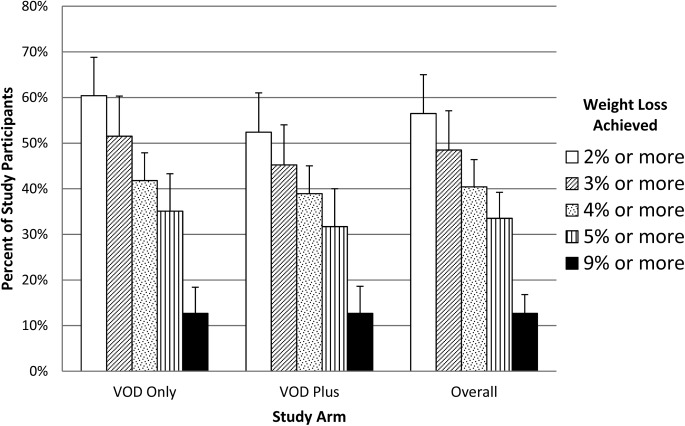
Percentages of participants with a follow-up weight measure who achieved weight loss thresholds after 5 months. *Error bars reflect upper 97.5% confidence bound for percentage estimate.
ITT analysis of weight changes
In ITT analysis, the predicted mean percent weight loss at 5 months, regardless of treatment assignment or episode viewing level, was 3.3% (95% CI 0.7-5.0%) (equivalent to 3.2 kg [95% CI 1.1-4.7 kg]). There was not a statistically significant difference (P = 0.19) in mean weight losses between randomized study arms: 3.7% (95% CI 1.9-5.0%) for VOD-Only participants and 2.9% (95% CI 0.7-4.2%) for VOD-Plus. Significant overall weight losses persisted at 12 months (3.2% [95% CI 0.4-5.0%]), but the difference in weight losses between study arms remained statistically nonsignificant (P = 0.23). In ITT models, there were no statistically significant associations among mean weight losses and participant sex, age group, or race category.
Associations among weight changes and numbers of episodes viewed
In exploratory ITT subgroup analyses, participants who viewed zero episodes (n = 41) had a mean weight loss of 3.2% (95% CI 1.4-4.6%), and those who viewed just one or more episodes (n = 265) had a mean weight loss of 3.3% (CI 0.1-6.5%). Participants in the highest viewing category (≥9 episodes [n = 110]) achieved the highest mean weight loss: 4.9% (95% CI 2.1-6.5%). However, when comparing these higher VOD viewers to those who viewed zero episodes, differences did not achieve statistical significance: 5-month mean weight loss was 1.6% higher (95% CI 0.7% lower to 3.9% higher).
Discussion
Principal findings
By offering a multicomponent lifestyle counseling and support program to adults at high risk for developing diabetes, the US DPP demonstrated that every additional 1 kg of weight loss translates into a 16% further reduction in the development of diabetes. After adapting the DPP approach for in-home delivery by cable TV programming, this study shows that high-risk adults can achieve mean weight losses at 5 months of 3.3% (about 3.2 kg) overall, and those who participate in ≥9 of 16 intervention sessions achieve mean weight losses of 4.9%. Despite these overall effects, our study found no added benefit when Internet-based support was added to the TV-based intervention. Use of the Internet intervention, however, was generally quite low. Because Internet access by trial participants exceeded 98%, this could suggest other barriers or that adults with interest in cable TV weight management resources might simply have less interest in other modes of behavioral support. Unfortunately, the study was not designed to identify reasons for lower adherence or effectiveness among some individuals.
Strengths and weaknesses of the study
Strengths of this study include its randomized design, “pragmatic” recruitment procedures that excluded only 13% of individuals for health related reasons, an objectively measured primary outcome, relatively low loss to follow-up (<15% at 5 months), and ITT analysis. Limitations included lack of a no-intervention control group and nonblinded study design. However, this study involved two active intervention arms with no more than minimal risk of harm to participants. This enabled us to eliminate any discussion of randomization, which likely minimized common biases that result when comparing interventions in which participants are aware they are receiving differential treatment. Also, although we used prespecified viewing categories for “dose-response” analyses, participants were not randomized to those categories, making it impossible to know whether higher participation actually results in greater weight loss. Although a limitation, this approach has been used in several prior studies and allows direct comparisons with past research.
Relationship to prior research
We were only able to identify one other published randomized controlled trial comparing different approaches for delivering a TV-based weight loss intervention for adults 12. This prior study found that offering a 16-episode, cable TV-based lifestyle program to predominantly obese African-American women achieved better body weight outcomes at 3 months compared to wait-list controls (0.72 kg lower; P = 0.01). However, consistent with our own study, there was no incremental effect when some individuals were randomly assigned to additional modes of support (in this case telephonic group chats or telephonic outreach educator support). Weight differences also were not maintained at 8 or 12 months.
There is a more substantial literature reporting mixed effectiveness of weight interventions in which telephonic or Internet platforms are the primary delivery modality (i.e., not simply an adjunct to TV) 13–15. When considered with our current study, it is possible that different remote intervention strategies may not have additive effects for many individuals, or that adults most likely to engage in a TV-based weight management program are simply not the same people as those who might benefit from a telephone or Internet-based intervention. Additional research is needed to guide thoughtful combinations of remote weight management approaches to achieve maximal benefit for individuals and for the entire population.
Past studies also have observed higher mean weight losses among participants completing more lifestyle intervention sessions 8,16. Our study was not designed with sufficient statistical power to test differences in weight losses between different subgroups, but the finding of a 4.9% weight loss among those who viewed ≥9 episodes is consistent with other past DPP translation studies 8. Another finding consistent with prior research was that some volunteers who elected not to take part in the intervention still managed to lose weight. In our study, it is possible that these participants benefited from co-interventions (the eScale; tools for goal-setting and tracking behaviors; automated phone calls). Alternatively, some may have been misclassified (at least two participants reported viewing episodes in another household but were still analyzed as zero-viewers), or there may have been ascertainment bias (34% of zero-episode viewers vs 12% of those viewing one or more episodes had a missing follow-up weight); which may have led to overestimation of weight loss for the zero-episode group 17.
Implications for population health improvement efforts
The findings of this study are novel and have implications for both public health and research. Several past studies have linked television viewing time with reduced physical activity or obesity 18,19. Today, about 114.7 million (96.7%) American households have at least one television, 52% of those have cable TV, and 38% have subscription TV service from a satellite or telephone provider 20. In total, about 280 million Americans spend an average of almost 4½ hours per day watching television 20. Television is a potentially powerful medium for influencing consumer behaviors; for example, soap operas are used to deliver public health messages regarding domestic violence, STD prevention, nutrition, and even peace 21. In addition, about 84 million (75%) households have a broadband Internet connection, in which video content can be streamed and additional web-based tools and resources could be accessed to support lifestyle behavior change 20. Although it is important to explore interventions to reduce sedentary time, it is also thoughtful to consider whether the time already spent in front of a TV or other video devices can be leveraged to promote healthier lifestyles and weight loss.
Although our study was designed to evaluate weight loss and other outcomes among only 300 viewers in just two Comcast markets, subsequent use of the VOD episodes by the broader public was striking; between May 2012 and May 2013 49,953 customers in these two cities viewed or streamed this content 102,326 times. This occurred without full-scale consumer marketing strategies, behavioral economic incentives, maximal reality-TV production techniques, or higher intensity forms of coaching that are now emerging through a variety of web-based platforms.
Conclusions
The vast reach of existing video media channels to engage high-risk individuals and those less likely to seek programs outside of the home underscores the immense potential for television-based lifestyle support interventions to influence the health and behaviors of millions of Americans. This study demonstrates the promise of a novel cable TV diabetes prevention intervention to support meaningful levels of weight loss over a 5- to 12-month period. Additional research is needed to determine the reach of such a strategy at full scale, as well as the costs and effectiveness of offering such an intervention over longer time periods and in combination with other resources and new technologies. Last, it is noteworthy that this study demonstrates the feasibility of using a randomized study design during the implementation phase of a large-scale health promotion program. Such designs should be encouraged for evaluating the comparative effectiveness of emerging health promotion and disease prevention interventions in both public and private sectors.
References
- 1.Gregg EW, Cheng YJ, Cadwell BL, Imperatore G, Williams DE, Flegal KM, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293:1868–1874. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. National Diabetes Fact Sheet, 2011. Atlanta, GA, USA: Department of Health and Human Services; Centers for Disease Control and Prevention; 2011. Available from: http://www.cdc.gov/diabetes/pubs/factsheet11.htm [accessed 22 February 2013] [Google Scholar]
- 3.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290:1884–1890. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 4.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabet Care. 2006;29:2102–7. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Geiss LS, James C, Gregg EW, Albright A, Williamson DF, Cowie CC. Diabetes risk reduction behaviors among U.S. Adults with prediabetes. Am J Prev Med. 2010;38:403–9. doi: 10.1016/j.amepre.2009.12.029. [DOI] [PubMed] [Google Scholar]
- 7.Ackermann RT, Marrero DG, Hicks KA, Hoerger TJ, Sorensen S, Zhang P, et al. An evaluation of cost sharing to finance a diet and physical activity intervention to prevent diabetes. Diabet Care. 2006;29:1237–1241. doi: 10.2337/dc05-1709. [DOI] [PubMed] [Google Scholar]
- 8.Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Aff (Millwood) 2012;31:67–75. doi: 10.1377/hlthaff.2011.1009. [DOI] [PubMed] [Google Scholar]
- 9.Herman WH, Hoerger TJ, Brandle M, Hicks K, Sorensen S, Zhang P, et al. The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann Intern Med. 2005;142:323–332. doi: 10.7326/0003-4819-142-5-200503010-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Diabetes Association. Diabetes Risk Test. Alexandria, VA: American Diabetes Association; 2012. Available from: http://www.diabetes.org/diabetes-basics/prevention/diabetes-risk-test/ [accessed 20 February 2013] [Google Scholar]
- 11.Diabetes Training and Technical Assistance Center. Diabetes Training and Technical Assistance Center (DTTAC) Atlanta, GA: Rollins School of Public Health, Emory University; 2012. Available from: www.dttac.org [accessed 3 March 2013] [Google Scholar]
- 12.Risica PM, Gans KM, Kumanyika S, Kirtania U, Lasater TM. SisterTalk: final results of a culturally tailored cable television delivered weight control program for Black women. Int J Behav Nutr Phys Act. 2013;10:141. doi: 10.1186/1479-5868-10-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang T, Chopra V, Zhang C, Woolford SJ. The role of social media in online weight management: systematic review. J Med Internet Res. 2013;15:e262. doi: 10.2196/jmir.2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coons MJ, Demott A, Buscemi J, Duncan JM, Pellegrini CA, Steglitz J, et al. Technology interventions to curb obesity: a systematic review of the current literature. Curr Cardiovasc Risk Rep. 2012;6:120–134. doi: 10.1007/s12170-012-0222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kodama S, Saito K, Tanaka S, Horikawa C, Fujiwara K, Hirasawa R, et al. Effect of Web-based lifestyle modification on weight control: a meta-analysis. Int J Obes (Lond) 2012;36:675–685. doi: 10.1038/ijo.2011.121. [DOI] [PubMed] [Google Scholar]
- 16.KM McTigue, R Harris, B Hemphill, L Lux, S Sutton, AJ, Bunton. Screening and interventions for obesity in adults: summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;139:933–949. doi: 10.7326/0003-4819-139-11-200312020-00013. [DOI] [PubMed] [Google Scholar]
- 17.Ware JH. Interpreting incomplete data in studies of diet and weight loss. N Engl J Med. 2003;348:2136–2137. doi: 10.1056/NEJMe030054. [DOI] [PubMed] [Google Scholar]
- 18.Pearson N, Biddle SJ. Sedentary behavior and dietary intake in children, adolescents, and adults. A systematic review. Am J Prev Med. 2011;41:178–188. doi: 10.1016/j.amepre.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996-2011. Am J Prev Med. 2011;41:207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 20.The Nielsen Company. The Cross-Platform Report, Quarter 2, 2012 - U.S. New York, NY, USA; 2012:1-12. Available from: http://www.nielsen.com/us/en/reports/2013.html [accessed 8 January 2013]
- 21.Chelala C. Learning From Soap Operas. New York Times; June 4, 2010. Available from: www.nytimes.com [accessed 16 February 2013]


