Abstract
Antiretroviral therapy to treat HIV/AIDS has substantially improved clinical outcomes among patients living with HIV/AIDS, but only in the presence of very consistent adherence. One of the most prevalent and impactful individual-level predictors of poor adherence is depressive symptoms, even at subthreshold levels. Evidence-based cognitive behavioral interventions exist to address improvements in depressive symptoms and adherence in this population, yet these techniques have largely been designed and tested as individual treatments for delivery in mental health settings. This presents a significant challenge when transporting these techniques to medical settings where other formats for delivery may be more appropriate (i.e., groups, less frequent visits) and few hands-on resources exist to guide this process. As such, primary aims of this study were to adapt and implement evidence-based cognitive behavioral techniques for depression (behavioral activation; BA) and HIV medication adherence (Life-Steps) that have potential for dissemination in an outpatient community health center. The intervention incorporated feedback from health center staff and utilized a modular, group format that did not rely on sequential session attendance. Feasibility was examined over 8 weeks (n = 13). Preliminary effects on depression, health-related quality of life, and medication adherence were examined and exit interviews were conducted with a subset of participants (n = 4) to inform future modifications. Treatment descriptions and recommendations for effective clinical implementation based on patient and clinician feedback are provided along with case material of two individual patients and an example group session. Current efforts are an important next step for disseminating evidence-based techniques for depression and HIV medication adherence to community health center or AIDS service organization settings.
Keywords: depression, HIV medication adherence, behavioral activation, CBT, community health center
Antiretroviral therapy to treat HIV/AIDS has substantially improved clinical outcomes among patients living with HIV/AIDS, but only in the presence of very consistent adherence (e.g., Crum et al., 2006). There are numerous barriers to achieving optimal levels of adherence; one of the most prevalent, impactful, and consistent individual-level predictors of poor adherence is depression (Gonzalez, Batchelder, Psaros, & Safren, 2011). Rates of depression among individuals living with HIV/AIDS are estimated to be approximately 42% (Horberg et al., 2008), and the presence of even subthreshold symptoms of depression has been shown to disrupt medication adherence; depressive symptoms have been associated with approximately a twofold increase in likelihood of poor adherence over time (Kacanek et al., 2010). Among HIV-infected substance-using individuals, even a 1-point increase in clinician-rated depressive symptoms on the Clinical Global Impression (CGI) severity scale (Guy, 1976) has been associated with a 75% increase in the odds of HIV medication nonadherence (Gonzalez et al., 2011); additionally, for each standard deviation increase on the Montgomery Asberg Depression Rating Scale (MADRS; Montgomery & Asberg, 1979), a 2.6-fold increased odds of nonadherence has been demonstrated. This has important implications for treatment outcomes, as medication nonadherence is associated with increased likelihood of producing medication-resistant HIV strains, greater health complications, failure to achieve full viral suppression (Bangsberg et al., 2001), and increased risk of death (de Olalla et al., 2002).
Evidence-based cognitive behavioral interventions have been developed to address improvements in both depression and HIV medication adherence among individuals living with HIV/AIDS with either clinical levels of depression or elevated depressive symptoms. Yet, it has been estimated that only 7% of HIV-infected individuals who require treatment for depression are receiving adequate treatment (Pence, O’Donnell, & Gaynes, 2012). These evidence-based techniques are rarely implemented in medical settings where many HIV-infected individuals with the greatest treatment needs—such as low-income, minority individuals with psychiatric comorbidity—receive treatment (Altice, Kamarulzaman, Soriano, Schechter, & Friedland, 2010; Pence et al., 2012; Soller et al., 2011; Weaver et al., 2008).
Specific to medication adherence, a brief, even single-session intervention, Life-Steps, is an evidence-based intervention that integrates informational, problem-solving, and cognitive behavioral components to improve HIV medication adherence (Safren, Otto, & Worthy, 1999; Safren et al., 2001). Life-Steps has empirical support as a brief individual treatment across a range of settings, including outpatient behavioral health (Safren et al., 1999; 2001; 2009), methadone maintenance (Safren et al., 2012), and international contexts (e.g., Cohen et al., 2011; Shiu et al., 2012; Simoni et al., 2011). Although first developed as a single-session intervention, recent adaptations (e.g., in international contexts) have delivered Life-Steps across multiple sessions (Shiu et al., 2012; Simoni et al., 2011). When integrated with other treatments, the Life-Steps module is conducted initially in a single session and then reviewed in subsequent sessions to continue to identify barriers and strategies to improve adherence (Safren et al., 2009; 2012).
To address depression alongside improvements in adherence, evidence-based treatments for depression have been integrated with Life-Steps, including cognitive behavioral therapy (CBT) for depression (Safren et al., 2009; 2012) and behavioral activation (BA; Daughters, Magidson, Schuster, & Safren, 2010). BA holds particular promise when considering potential relevance for dissemination and flexible delivery of evidence-based techniques in HIV community health centers. BA is an evidence-based behavioral intervention based upon reinforcement theories of depression that targets increases in value-driven rewarding behaviors (Cuijpers, Van Straten, & Warmerdam, 2007; Lejuez, Hopko, Acierno, Daughters, & Pagoto, 2011; Lejuez, Hopko, LePage, Hopko, & McNeil, 2001; Mazzucchelli, Kane, & Rees, 2009; Sturmey, 2009). It is similar to the activity scheduling module of CBT (Jacobson et al., 1996), with a few key distinctions: BA includes an in-depth psychoeducation component on the relationship between depression and engaging in enjoyable and important behaviors. BA also includes behavioral monitoring with associated ratings of enjoyment and importance and a values-based assessment to guide activity selection.
Given its practical, straightforward nature, BA has been suggested to be particularly suitable for dissemination. Evidence suggests BA can be delivered as an individual or group approach and condensed into a briefer formats as practical barriers necessitate (e.g., Daughters et al., 2008; MacPherson et al., 2010; Magidson et al., 2011). It is also appropriate for training nonspecialized primary care providers (Ekers, Richards, McMillan, Bland, & Gilbody, 2011). These are characteristics that support its broad application across a range of clinical settings. Further, there is some evidence that more elaborate cognitive techniques may not be feasible or appropriate for individuals with low psychological insight, low education levels, chronic substance use histories, or cognitive impairment (Aharonovich et al., 2006; Aharonovich, Nunes, & Hasin, 2003). In addition to clinical depression, BA has been used to improve subthreshold depressive symptoms and distress regardless of depression diagnosis (Daughters et al., 2008; Magidson et al., 2011; Manos et al., 2009). BA also has been suggested to be easily tailored for medical and psychiatric comorbidities (Mazzucchelli et al., 2009; Sturmey, 2009) and has demonstrated positive effects on comorbid outcomes often independent of changes in depression (i.e., smoking, substance use; MacPherson et al., 2010; Magidson et al., 2011).
More specifically, BA has been adapted for low-income substance using and HIV-positive individuals; adaptations include emphasizing the link between activity, mood, and substance use, generating ideas for substance-free activities, incorporating relapse prevention into treatment (Daughters et al., 2008; Magidson et al., 2011), and identifying links between activities and poor HIV medication adherence (Daughters et al., 2010). These modified BA techniques have been previously integrated with Life-Steps in a 16-session, manualized individual treatment format (Daughters et al., 2010).
Despite the potential for dissemination of BA to improve depression across a range of settings and empirical support for delivery of BA in groups (e.g., Daughters et al., 2008; Magidson et al., 2011; Porter, Spates, & Smitham, 2004) and in primary care specifically (Ekers et al., 2011), BA and Life-Steps have largely been delivered as individual treatments in mental health settings. This presents a significant challenge when transporting these techniques to medical settings, where many individuals with the greatest need for treatment—such as low-income, minority HIV-infected individuals with psychiatric comorbidity—seek care (Soller et al., 2011). Few resources exist to guide how to adapt these interventions and techniques for a medical setting and, in particular, into a group format, which may be the most feasible and cost-effective option for low-resource community health settings. Further, other features of a mental health setting, such as trained mental health providers, sequential, weekly treatment attendance, and a unified presenting problem may not be realistic in medical settings. Implementing interventions in a medical setting that were tested and designed for individual treatment in a mental health setting is a struggle across types of disorders and interventions, particularly for low-resource settings such as HIV community health centers that commonly treat individuals with multiple psychiatric and medical comorbidities (Altice et al., 2010; Soller et al., 2011).
As such, the primary aim of the current study was to adapt evidence-based BA treatment techniques for depression and Life-Steps for HIV medication adherence for low-income, minority patients infected with HIV who were receiving care at an outpatient community health center. This treatment center had not implemented evidence-based CBT techniques prior to this project. In this report, the resulting “Act Healthy” group treatment is described in more depth, including the specific modifications and adaptations for implementation in a community health center. Case material of two individual patients and an example group session are depicted to portray this approach with greater clarity. Feedback from individual exit interviews is presented, along with recommendations for effective clinical implementation based on clinician and patient feedback. Effects on depressive symptoms, medication adherence, and mental and physical health-related functioning over 8 weeks are briefly discussed. If evidence-based interventions for adherence and depression can be integrated into real-world outpatient medical settings where patients typically receive regular, ongoing care, this has important clinical implications for both treatment and prevention, particularly if treatment platforms with the greatest potential reach are considered.
Material and Methods
Treatment Setting
The current study was conducted at an urban outpatient community health center that specializes in HIV/AIDS and LGBT health care and also provides primary health-care services for the community regardless of HIV status, sexual orientation, or gender identity. Center services include primary medical care, HIV/AIDS primary care, dental care, medical adherence, legal help, pharmacy services, behavioral health, and a computer for patient access. For patients with severe mental health needs, daily treatment groups are offered, which are typically delivered by a licensed clinical social worker (LCSW) and focus on topics such as addictive behaviors, aging with HIV/AIDS, and spirituality. Given few evidence-based cognitive and behavioral techniques being utilized in the center to address psychiatric comorbidity, most commonly depression, the Act Healthy group was implemented and evaluated for use at this center.
Specific Adaptations for This Format and Setting
Prior to implementing the group, we met with core treatment staff (center director, head registered nurse, and LCSW) to understand primary treatment needs, center structure, and patterns of attendance. The primary difference that emerged in comparison to traditional mental health settings was the less frequent, irregular attendance (i.e., as opposed to regular weekly or biweekly treatment sessions). In comparison, patients were not attending weekly or on consistent days, and thus we could not rely on sequential weekly treatment structure often implemented in an outpatient mental health setting. Another key theme that emerged was the reliance on a group format. Given the high patient caseloads and staff burden, particularly for dedicated behavioral health staff, the majority of treatment was delivered in groups. Thus, the key challenge was how to design a structure that would utilize the evidence-based techniques effectively in a group using a format that would be effective for both patients who had attended the previous week(s) alongside those who had not been present. Given this challenge, we aimed to design an evidence-based curriculum that would build upon previous content but also provide a sufficient overview and review for members who had not attended previously.
Another key issue presented by center staff was the preference to include all interested patients, regardless of psychiatric diagnosis. In line with this suggestion, we chose to not have specific inclusion criteria for the group or study, which seemed clinically appropriate given the high rates of depressive symptoms among low-income, minority HIV-infected individuals, particularly those with co-occurring substance abuse (Berger-Greenstein et al., 2007). Further, general distress and disruptions in mood can have a powerful impact on adherence regardless of diagnosis (Leserman, Ironson, O'Cleirigh, Fordiani, & Balbin, 2008), suggesting that even individuals without clinical levels of depression may benefit from this approach.
Treatment Overview and Structure: The “Act Healthy” Group
The intervention described here integrates Life-Steps (Safren et al., 1999) and BA (Lejuez et al., 2001; 2011) for group delivery in a medical setting. Balancing the factors at this center described above, the group utilizes a flexible, modular format (e.g., CBT-AD; Safren et al., 2009; 2012), with content repeated each week to account for nonsequential session attendance. The time spent on each module per session depends on patients’ presenting issues, similar to the flexible approach of other integrated CBT interventions for depression and adherence (i.e., CBT-AD; Safren, Gonzalez, & Soroudi, 2007; Safren et al., 2009; 2012). This modular approach has been demonstrated to be a useful format to accommodate complex patient populations and stems from qualitative work suggesting the need for flexibility of interventions when working with HIV-infected individuals with multiple comorbidities (Berg, Raminani, Greer, Harwood, & Safren, 2008; Soroudi et al., 2008). The treatment structure also includes a strong emphasis on peer contribution to lead review of previous sessions and to work collaboratively with others throughout treatment.
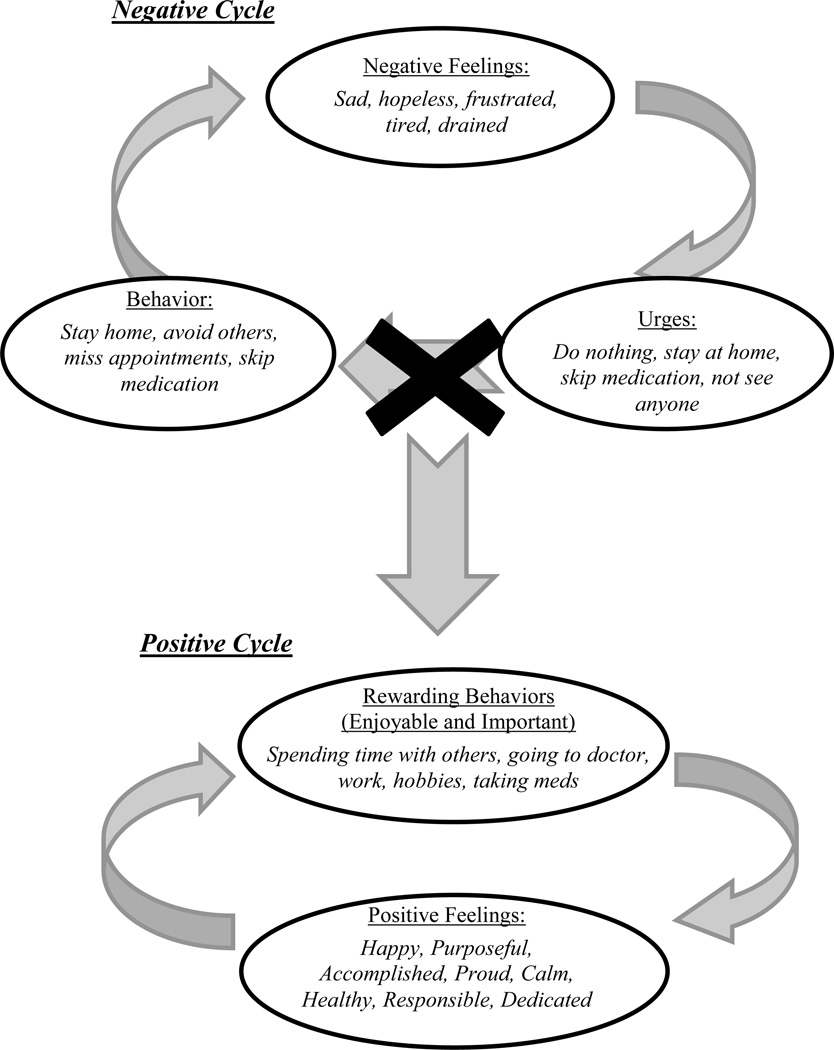
As part of the need to address variations in attendance, each and every session includes: (a) a discussion of medication adherence and skills within Life-Steps; (b) a review of the basic BA treatment rationale (see Figure 1 and description below), highlighting how disruptions in regular, meaningful, and enjoyable activities can contribute to worsening mood and medication nonadherence; and (c) activity monitoring, selection, and scheduling following from a goals-based assessment. These three main components are described in more detail below.
Figure 1.
Depiction of BA treatment rationale reviewed at the start of each session. This was based upon the BA treatment rationale depicted in Act Healthy (Daughters et al., 2010). Specifically, this figure is introduced to patients step-by-step illustrating how the treatment is meant to break the negative cycle (i.e., where the “x” is) and start a new more positive cycle.
Life-Steps Module
As described previously, Life-Steps (Safren et al., 1999) is a brief, evidence-based intervention to improve HIV medication adherence that integrates informational, problem-solving, and cognitive behavioral techniques through 11 “steps” (e.g., psychoeducation, attending appointments, obtaining medications, communicating with providers, coping with side effects, formulating a daily medication schedule, storing medications, utilizing cue-control strategies for pill-taking, responding to slips, etc.). For each step, barriers and solutions are identified, along with a plan for implementing a solution. In the Act Healthy group, each step is briefly described every session, and patients decide as a group on one to two steps to discuss each week. Patients who attended previously have the opportunity to lead the Life-Steps review with assistance from the therapist. Problem-solving solutions and plans for implementing solutions are typically facilitated by the therapist with peer input.
BA Modules
BA techniques utilized in the Act Healthy group are derived from the most straightforward and brief version of BA (i.e., Lejuez et al., 2001; 2011) with adaptations previously tested for low-income individuals living with HIV/AIDS (Daughters et al., 2010). In the Act Healthy group, there are two main BA treatment modules: (a) the BA treatment rationale/psychoeducation; and (b) activity monitoring, selection, and scheduling.
BA treatment rationale
The BA treatment rationale is typically the first module covered in each session. Specifically, the links between negative feelings/emotions, urges, and negative behavior patterns are illustrated, along with ways to break this cycle with rewarding, enjoyable, and meaningful behavior. Next, the positive feelings that come along with this behavior change are highlighted, and it is illustrated how these feelings often increase the likelihood of continued engagement in positive behavior. See Figure 1 for an example depiction of the BA treatment rationale. The therapist typically leads the rationale in the initial sessions with active participation and engagement from patients when eliciting examples. After the first one to two sessions, patients are asked to volunteer to lead the treatment rationale with input from the therapist and other patients. Patients typically rotate to lead the cycle each week. This exercise transitions nicely into the next BA module—activity monitoring, selection, and scheduling—in that the “positive” cycle elicits examples of positive behaviors that can be scheduled into one’s week.
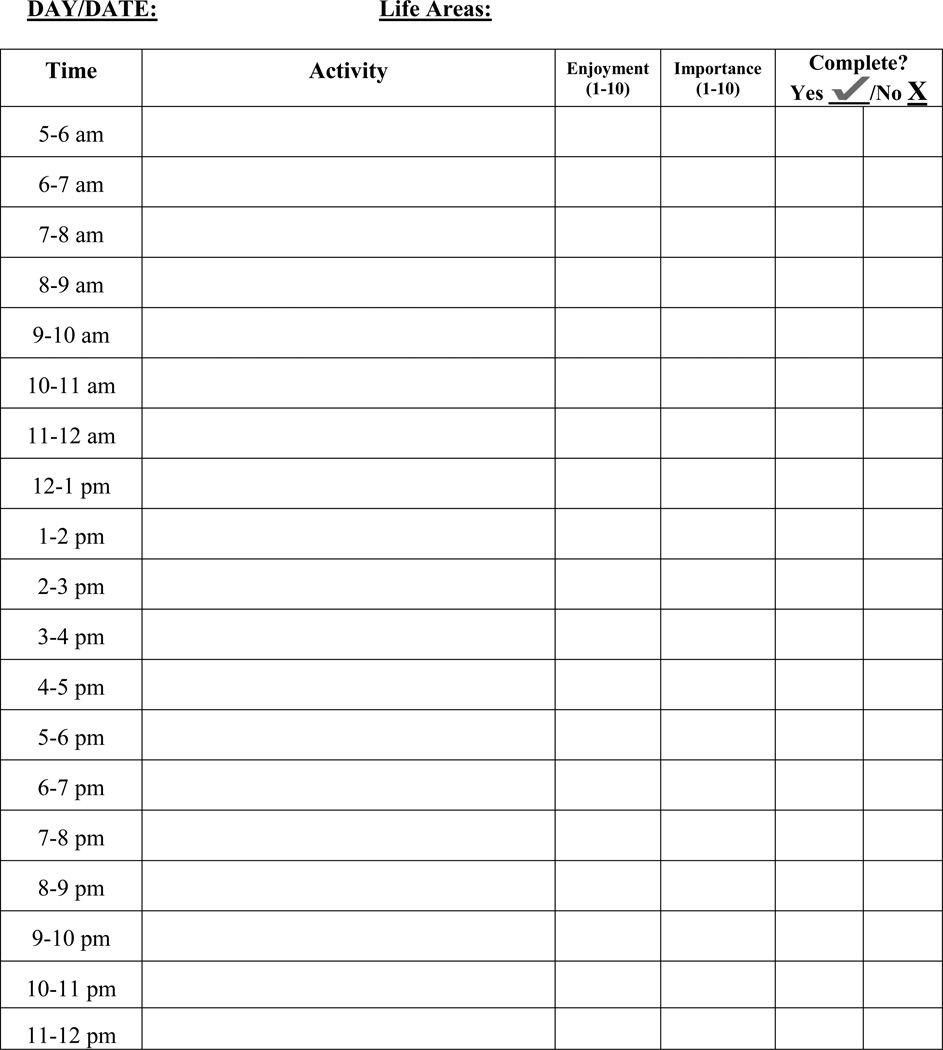
Activity monitoring, selection, and scheduling
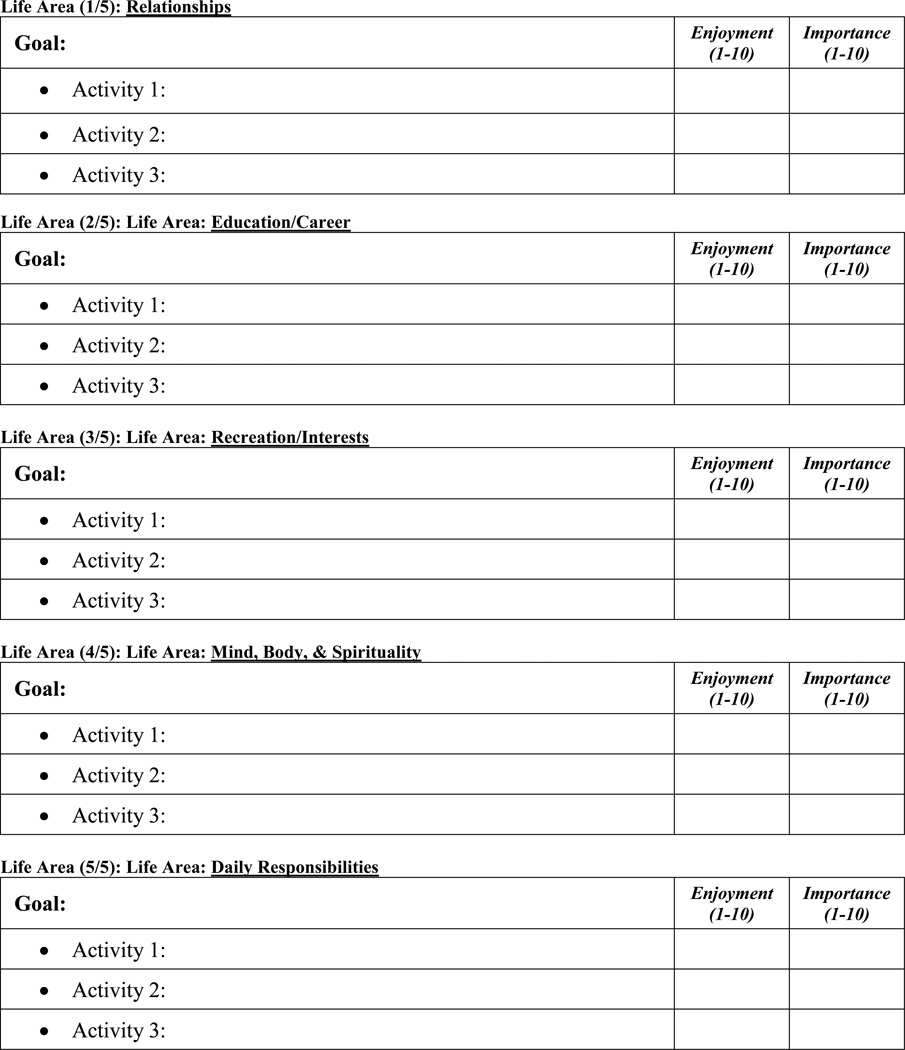
In this module, attention turns to daily monitoring of activities and associated importance and enjoyment ratings, identifying values/goals across numerous areas of one’s life, generating measurable, observable activities that may reflect living a life according to these values/working towards these goals, and scheduling these activities into one’s day and week at concrete times. The activity monitoring and scheduling procedures are derived from Lejuez et al. (2011), which developed a more simplified approach to monitoring and scheduling activities using a single form (see Figure 2). This form is introduced as a monitoring form to be completed throughout the week (one per day), with specific activities scheduled throughout the week. Patients are instructed to indicate (by checking off “yes” or “no”) whether they were able to complete the scheduled activities. Scheduled activities are derived from a goals/values-based assessment across five life area domains (relationships, education/career, daily responsibilities, mind/body/spirituality, and interests/recreation; see Figure 3). Specifically, patients are asked to think about what is important to them in each of these five domains, and what types of activities would align with these goals/values. Patients are encouraged to select activities that are concrete and specific that they can schedule into their week. A problem-solving based approach is incorporated into the activity selection and scheduling exercise; activities are broken down into small, manageable steps before they are incorporated into one’s schedule. The goal selection process is patient-driven, and goals within each life area may not be measurable or achievable. However, the activities within each goal are meant to be objective and measurable. It is with activity selection that the therapist may be more likely to provide guidance in helping identify or select activities that are concrete, measurable, and that can then be assigned to schedule into one’s day or week. The life areas assessment is both introduced and reviewed in each session. Patients who have attended previously build upon previous weeks’ life area goals and activities, either selecting new life areas to focus on or adding to existing life area goals. Patients are encouraged to bring these forms back with them the next time they attend the session. Blank forms are also available in session for new patients and patients who do not bring their forms back to session.
Figure 2.
Activity monitoring and scheduling forms introduced and reviewed at each session. This form was adapted from Lejuez et al. (2011).
Figure 3.
Life Areas, Goals, and Activities Inventory. Note that only one table per life area is depicted here due to space constraints; however, participants could work on more than one goal in each life area.
Participants and Procedure
In total, 13 patients participated in the group over an 8-week period. Patients were 92.3% African American (n = 12), 46.2% female (n = 6), and mean age was 50.75 (SD = 9.88). Patients attended a mean of 3.46 sessions (range 1–8). There was a mean of 4.85 patients per group session (range 2–9). The group was delivered weekly for 8 weeks by a predoctoral graduate student in clinical psychology with previous training and 4 years of experience providing Life-Steps and BA, but no prior training in implementing a nonsequential treatment protocol. Treatment sessions lasted approximately 1 hour.
Participation in all aspects of this study was entirely voluntary, including treatment, exit interviews, and brief outcome assessments. Patients at this center were told by center staff that there was a weekly group available to them that would focus on improving their mood and ability to take their medications, ways to improve “healthy living” and reduce barriers to medication use, and that there would also be opportunities to provide feedback on their experiences in the group and participate in brief research assessments. They were also told that they could participate in the treatment group regardless of their interest in participating in the research assessments or exit interviews. The center implements guidelines for all groups run at the center that were also in place for this treatment group; for instance, patients could not attend if they presented drunk or high. Patients were also required to meet with a psychiatrist or primary care provider (PCP) for medication evaluation/management at least two times per year, and if clinical staff believed patients’ current symptoms were too severe or may be disruptive to group members, they were required to attend the medication appointment prior to entry. There were no incentives given for participation in the research aspect of this group intervention.
Assessments
Assessment measures were administered at Week One (prior to the start of the first session) and at Week Eight (after the eighth session) and included a brief assessment of mental and physical health-related functioning, clinician-related depressive symptoms, and medication adherence. Mental and physical health-related functioning were assessed using the SF-12 (Ware, Kosinski, & Keller, 1996). SF-12 scores range from 0–100 with a mean of 50 in the general population and higher scores reflecting better functioning. Two summary scores are calculated using the SF-12: a physical health composite score (PCS) and a mental health composite score (MCS). Clinician-related depressive symptoms were assessed using the Hamilton 7-item Rating Scale for Depression (HAMD-7; McIntyre et al., 2005). For the HAMD-7, scores range from zero to 26, and a score greater than 3 indicates clinically significant depressive symptoms. Medication adherence was assessed using a visual analogue scale of % medications taken in the past month from 0 to 100% adherence (Giordano, Guzman, Clark, Charlebois, & Bangsberg, 2004) and self-reported frequency of doses missed across a range of common reasons for nonadherence using a section of the AIDS Clinical Trials Group (ACTG) questionnaire (Chesney et al., 2000). In this section of the ACTG questionnaire, respondents are presented a list of 14 reasons why people may ever miss taking their medications (e.g., being away from home, busy with other things, simply forgot) and asked “how often have you missed taking your medications because you …” for each reason. Participants rate responses on a 4-point scale (never, rarely, sometimes, often) to indicate the frequency of nonadherence due to each of the 14 reasons. Responses are summed, with higher scores indicating greater frequency of reasons endorsed for nonadherence (scores range from zero to 42). We also examined the reasons each patient endorsed to provide richer information on individual barriers to adherence.
Research assessments took approximately 15 minutes and were conducted by a postbaccalaureate research assistant. The assessments were conducted separately from the clinical services provided, and participating in research was not required to attend the group. If patients were interested in participating in the assessments and exit interviews following treatment, all study procedures were described in depth and potential participants were provided written informed consent. Informed consent, exit interviews, and assessments were conducted in a private room at the center. All procedures were approved by the University IRB and approved by the program director and director of research at the host community health center. Four individuals participated in the research protocol (both research assessments and follow-up exit interviews). Exit interviews lasted approximately 15 minutes (see Table 1 for a list of exit interview questions).
Table 1.
Compilation of exit interview questions and example participant responses.
| Questions | Participant Responses* |
|---|---|
| 1. In your own words, what would you say was the purpose of the group? | The group helped me and motivated us to think ahead of time, as opposed to just saying, ‘OK, I woke up this morning. Now what?’ We went further into our thought pattern and said, ‘Hey, let’s plan for the next day.’ And it [the group] not only talked about your physical, but about your mental health, and accomplishments—what you want to do, and some life stressors. [We talked about] things you can do to take the stress off, and how to remember to take your medication. |
| 2. Tell me something that you feel you will take away from the group. | I learned to be specific with what I plan. Even if I don’t do it, I have something planned each day. Positive things. |
| 3. What were some goals that you set for yourself? What was your progress with those goals? | One thing I did was to go to bed later. I was going to bed too early and waking up in the middle of the night. That [change] has worked out great. I’m sleeping my eight hours and feel good in the morning. It also helped with my morning meds. |
| 4. What, if anything, made it difficult to bring the homework forms back to group? | Because during the week you get caught up in your day, your family activities, and you forget. Maybe it’s my medication … it’s easy to forget those types of things and papers. For me, I don’t like to do a lot of homework. It wasn’t fun. |
| 5. What changes would make it easier to bring the goal forms back with you? | Leave homework forms somewhere you are each day and can fill them out on a daily basis. The same place every day so it doesn’t get lost. Or, instead of doing logs, we could use stickies that you put on your refrigerator, and make the stickies colorful, too, so that they stand out. |
| 6. Did you learn anything from the other group members? | They gave me ideas for my goals, like how to find a good case manager, and I got tips on how to make transportation to appointments easier. |
| 7. What was the most helpful part of the group for you? | Probably I would say the [positive and negative] cycles. I still want to see if I can do them by myself. And talking about appointments and taking meds. |
| 8. What was the least helpful part of the group for you? | The homework forms because they were hard to remember. |
| 9. If you missed a week of the group, did you feel lost or behind when you came the next time? | We never got behind because there was always review. The other group members helped a lot, too. A few people really took the lead when they could be there the past couple weeks. |
| 10. Would you recommend this group to other patients like you? Why or why not? | Yes, I’d really recommend it to someone who just got diagnosed, to learn about taking your medications. I wanted to get undetectable with my viral load and I accomplished that. |
| 11. What would you change about the group? | Sometimes I don’t want to hear no more about this medicine! Most of us learned the hard way not to miss our meds. I think focusing on other medical stuff more besides taking meds. |
Note.
A single participant’s response was included for each question. The feedback received in the exit interviews was quite uniform; we provided a single answer for each response to avoid redundancy.
Case Examples
The following section provides case material to give interested clinicians a clearer sense of how these techniques may be implemented in the flexible, group format. First, an example group session is provided to depict more clearly the implementation of this approach. Next, case examples are presented of two individuals who attended the group and participated in assessments and exit interviews. Case illustrations are provided to illustrate how the treatment, although delivered in a group format, was individualized based on distinct medical and psychological patient needs. The two cases profiled were representative of the 13 total group members. Their relatively high levels of self-reported adherence were in line with the high adherence of other group members. Although patients had different medical and psychiatric comorbidities, these cases are representative of the other members of the group who also had multiple medical and psychiatric comorbidities. Case descriptions are deidentified to preserve patient confidentiality.
“Group Session” Case Study
Although a “case study” often refers to profiling an individual patient in an intervention, a “group session” case example is presented here to provide a clearer depiction of this group in practice. Given the nonsequential format of this intervention, it is not a specific session “number” per se; the profiled session below was the fourth group session administered at this center. Although this is the “fourth” session, the content is representative of other sessions delivered given that there is not a sequential structure.
At this session, six patients were in attendance. Three had attended the group the previous week, one had attended 2 weeks prior, and two had not previously attended. The group began with the BA treatment rationale module. In this session, it was co-led by the therapist and one patient who had attended the previous week. The treatment rationale was depicted visually on a white board (see Figure 1 for another example), and patients discussed themes of sadness, frustration, loneliness, and numbness leading to urges to avoid friends and family, skip medications and appointments, smoke cigarettes, and “just give up.” They described often not being able to resist these urges—a point that was shared and resonated among group members— and then discussed strategies that had helped them in the past resist these urges.
The patient co-leading the module illustrated where to “break the cycle” (see Figure 1) with more meaningful, enjoyable, and rewarding activities, and fellow patients provided examples of positive activities, such as calling a friend, seeing a family member (particularly grandchildren), doing something artistic, getting outside, performing light exercise, dancing, and listening to music. Patients reported that although they could often identify these activities and knew that they may relieve some negative feelings, it was difficult to initiate the positive activities when they felt this way. This became a discussion point in the group, along with a discussion of what types of feelings typically follow when patients are able to engage in these activities. The dialogue between patients was thoughtful and engaging when reviewing the treatment rationale cycle, and this module lasted approximately 20 minutes.
Next, the session focused on the BA activity monitoring and scheduling module. New activity monitoring and scheduling forms (see Figure 2) were given to the two patients who had not previously attended. Of the three that had attended the group the previous week, two brought the monitoring/scheduling forms to session. Both had monitored approximately 50% of activities and had checked off the activities they planned for themselves. These two patients presented to the group what they had completed, focusing mostly on how the scheduled activities went. The therapist praised the homework completion and reinforced their efforts. Both patients discussed barriers and how they felt after engaging in the activities. This review took approximately 10 minutes and was used as a guide for new patients on how to complete the forms for next week.
The focus then turned to a discussion of the goal/activity assessment form across five life areas (see Figure 3). Each patient identified one life area and then established goals within that life area. The goal selection process is patient-driven, and as such the therapist did not intervene much in this process. Former patients added to previously completed forms (or identified a new life area if they did not bring their forms). Next, patients selected activities within each goal, and the therapist first led a discussion of the distinction between goals and activities for new patients, highlighting in particular the importance of breaking down activities into small, manageable pieces that are objective and measurable to work toward a larger goal. Next, the group members worked in groups or pairs to select specific activities to schedule for homework, with the therapist consulting each subgroup to monitor their progress and provide suggestions to select activities that are concrete, measurable, and that can then be assigned to schedule into one’s day or week. This allowed the therapist to give specialized attention to new patients who needed more guidance and allowed returning patients to take the lead in their own activity scheduling. Once this was set, two activities from each goal were transferred to the activity scheduling forms, each with a specific date and time for completion. This component took approximately 15 minutes.
This session finished with the Life-Steps module (approximately 15 minutes). First, each step was listed on the white board (written by a group member who had attended 2 weeks prior with the aid of other patients), and two steps were selected by the group as the focus of the session (appointment attendance and provider communication). Patients had an open discussion of barriers to attending appointments and challenges in provider communication (i.e., discomfort with PCP, difficulty remembering questions). Structured problem-solving techniques were led by the therapist to address these issues in addition to recommendations provided by other group members. Appointments and medication times were also written into the activity scheduling homework forms for patients who had difficulties with these issues.
Although each group session differed somewhat in terms of time spent on each module or the specific themes or highlights addressed in each module (i.e., what types of activities or specific life areas in the BA module, what medication adherence-focused concerns in the Life-Steps module), a somewhat similar structure remained across sessions, and all content was drawn from consistent modules across sessions. Additionally, some sessions began with Life-Steps as opposed to BA in order to balance any potential impact that order may have had on the amount of time spent on each module.
Case 1
Mike H. is an African American heterosexual man in his mid-50s who was infected with HIV in the late 1980s through injection drug use. At the time of treatment, he lived in urban low-income housing in an apartment with his brother. He had been receiving his outpatient medical care at the study site for 8 years and had a regular PCP at this site. In addition to HIV, Mike also had been diagnosed with hepatitis C, hypertension, and sleep apnea. Mike was not engaged in consistent psychiatric or psychological care and tended to address any psychiatric symptoms with his PCP. His medical record indicated previous diagnoses of bipolar disorder and schizophrenia (both diagnoses were first documented in his early thirties). Mike reported no current symptoms of mania or schizophrenia at entry into the group and could not recall the last time he experienced any of these symptoms. Mike’s antiretroviral therapy regimen included the drugs Isentress (one pill twice a day) and Truvada (one pill taken once a day). His first antiretroviral treatment began in the early 1990s, and the current regimen was initiated in 2009.
Mike reported interest in participating in this group because he often felt down and had concerns that he was sleeping too much. In his first session, he stated he felt like he did not have many coping skills to improve his mood or take his medications on days he felt down. At the baseline assessment, Mike’s HAMD-7 score was 4, indicating clinically elevated depressive symptoms (scores range from zero to 26 and greater than 3 on the HAMD-7 indicates clinically significant depressive symptoms). Although Mike reported 100% medication adherence in the past month on the visual analogue scale, he endorsed missing doses across a range of reasons (being away from home, being busy with other things, simply forgetting, wanting to avoid side effects, feeling sick or ill, and having problems taking pills at specified times), indicating there were barriers to adherence. His score on the ACTG frequency of reasons endorsed across reasons for nonadherence scale was a 25 at baseline (although no clinical ranges are available for this measure, scores range from zero to 42). Mike’s scores on the subscales of the SF-12 at baseline were 29.1 for the PCS and 50.1 for the MCS, indicating worse physical health functioning as compared to the general population and average mental health functioning compared to the general population (a score of 50 on both subscales reflects the mean for the general population). Over the 8-week period, Mike attended five sessions, which was above the mean for the group (on average patients attended a mean of 3.46 sessions over the 8-week study period).
During the course of treatment, Mike showed a strong grasp of the treatment rationale and acknowledged the importance of positive daily activities in his life. Although Mike tended to be reticent during sessions, the therapist made sure to call on Mike when topics arose that were especially relevant to him (i.e., oversleeping, and how to address it) to maximize his participation. When called upon to contribute, he demonstrated a clear understanding of the negative and positive cycles depicted in the treatment rationale module. He also provided insightful comments to others when they reported negative feelings and urges—for instance, pointing out that taking time to think about the specific negative consequences, such as jail time or health complications, was often an effective way to resist negative urges. One challenge was that Mike would be reluctant to endorse feelings of depression or sadness, yet he did identify with corresponding urges of “wanting to give up” and “trying to sleep all day.” Throughout his participation, the therapist was careful to utilize the expressions and descriptions of symptoms that were most in line with those Mike recognized and with which he identified.
Mike wanted to focus almost exclusively on the life area of education/career. Specifically, he wanted to obtain a full-time job working at a local pharmacy. He often found that in the past when he was working, he would have fewer days that he felt this desire to just “give up” and he could not sleep all day. He reported feeling happier during these periods, and he was also much more easily able to take his medications when he had a rigid routine. Given Mike’s strong desire to obtain employment, he prioritized this goal and breaking down this goal into manageable pieces consistently throughout treatment. Due to his high computer literacy skills, many of Mike’s scheduled activities outside of treatment involved designating time in his day to search for and apply to entry-level jobs on the Internet. During group, he broke down these activities into smaller pieces (i.e., how long to search for, what websites to use, how many to apply to each day, gathering necessary materials for the application). He also prioritized creating a resume, which involved numerous specific activities (e.g., asking former coworkers for examples and asking a counselor at the center, with whom he had a good relationship, to review his first draft). Additionally, he wanted to prepare for interviews, and one activity he identified was to ask this same counselor at the center if he would do a mock interview with him. Although staff are not typically available to patients for job-related support, Mike skillfully asked this counselor for specific feedback and support, and the staff member agreed. By the end of the treatment period, Mike had secured a part-time temporary position at a local pharmacy for 1 month. At the 8-week assessment, he reported that he was continuing to look for full-time employment at pharmacies and grocery stores using the same strategies he focused on in BA.
Mike’s adherence-related goals were very closely linked with obtaining employment. Mike reported rarely missing medications during previous periods of employment given the regularity of the routine, more regular sleep schedule, and his overall improved mood and “purpose.” Thus, he felt that prioritizing obtaining employment would also enable improved adherence. One challenge with Mike was that he initially felt that finding a job was the only thing he could do to improve his adherence. However, the therapist encouraged him to set an additional adherence-specific goal prior to obtaining employment, which was to increase the use of alarms to prevent times in which oversleeping interfered with his morning medication schedule. By the end of the 8-week period, he had successfully borrowed an extra backup alarm from his brother and had implemented regular alarm use to wake up prior to his morning medication time.
Mike’s homework completion was among the highest of the group members. He brought his activity monitoring and scheduling homework forms back to each of four later sessions he attended. Mike completed all of the activities he had scheduled during group, and on two occasions he added four additional activities. He preferred to focus on activity scheduling as opposed to monitoring, and this became even more of a priority once he started work, as he did not want to bring his forms to his job. Once he started working, we also discussed ways in which he could continue the activity scheduling exercises without the use of forms (i.e., putting scheduled activities into his personal calendar). He discussed how having the same activities scheduled each week helped with regularity of routine, which was important to him for his adherence, as well as for remembering the scheduled activities without the use of paper forms.
From the baseline assessment to Week Eight, Mike’s HAMD score dropped from above the clinical threshold initially (score of 4) to zero, indicating no depressive symptoms. His reported adherence in the past month on a visual analogue scale remained steady at 100%. Following treatment, he reported a lower frequency of missing doses and fewer reasons for missed doses (wanting to avoid side effects, feeling like the drug was toxic/harmful, feeling sick or ill, or feeling good). The total frequency of his reasons endorsed for nonadherence of 25 at baseline decreased to 9 following treatment. His SF-12 PCS score rose to 42.7 at Week Eight, which reflects physical health functioning below the mean in the general population, and his MCS score remained stable (51.1) at the population mean.
Case 2
Tawanda M. was an African American woman in her mid-30s who had more recently initiated care at the center (in the past year). She was diagnosed with HIV in the mid-1990s when she became pregnant. She believes she was infected with HIV from a casual male partner. At the time of treatment, Tawanda lived with her husband of 10 years and her 17-year-old daughter. Five years prior, Tawanda was diagnosed with bipolar disorder after suffering a “nervous breakdown” when her mother died, which was also documented in her medical record. Tawanda’s medical history included genital herpes (diagnosed in early 2000s), a hernia, hypothyroidism, and high cholesterol. Tawanda’s antiretroviral therapy regimen included one pill of Prezista, Epzicom, and Norvir once a day and one pill of Isentress twice a day, which was a regimen she had started 2 years prior. Tawanda initiated antiretroviral therapy in the late 90s.
Tawanda had severe depressive symptoms at baseline (HAMD score of 14; scores range from zero to 26 with a score above 3 indicating clinically significant depressive symptoms). She reported no suicidal ideation at baseline. On a self-reported visual analogue scale of adherence, Tawanda indicated 97% adherence over the month before baseline. She reported numerous reasons for missing doses, including being away from home, simply forgetting, having too many pills to take, wanting to avoid side effects, having a change in daily routine, feeling like the drug was toxic/harmful, feeling depressed/overwhelmed, running out of pills, and feeling good. The frequency of missing doses across these reasons was a 12 at baseline (scores range from zero to 42). On the SF-12, her baseline PCS score was 40.9 and 32.8 for the MCS, indicating physical and mental health functioning below the mean of 50 in the general population on both physical and mental health functioning.
Tawanda elected to focus on the life areas of education/career and mind, body, and spirituality. More specifically, Towanda focused on the goals of finding a job and getting closer to God through involvement with her church. Activities related to finding a job centered around using a computer available at the center during times she came in for her appointments to search for jobs, asking a nurse social worker at the center to talk with her for 15 minutes after one of her appointments about guidance in the job application process, and to stop by local stores and movie theaters on her way home from the center to inquire about potential employment opportunities. Regarding her spirituality goal, Tawanda planned to go to church each Sunday with her daughter—also a chance to spend quality time with her—as well as get involved in the biweekly events the church put on that included volunteering, cleaning the church, and choir-related activities. Tawanda identified these activities as a way to get closer to God and connect with others who also value the church in their lives. In the group setting together with the therapist and other peers, she broke down these activities into the smallest, most specific possible steps to then schedule into her day. She also discussed potential barriers in this process; for instance, she had some concerns regarding others knowing her HIV status, which she described as a barrier to engaging in these activities.
Towards the end of eight weeks, Tawanda had asked to meet with the social worker at the Center, met with her for 15 minutes on two occasions, spent two hours using the Center computer to apply for jobs, stopped by a local movie theater on her way home, and applied to two jobs (at a movie theater and local retail store), although she had not received a response from either. Additionally, she attended church regularly on Sundays with her daughter and attended two church-sponsored events (volunteering and choir). She continued to report some concern regarding others knowing her HIV status at the church, but that she attended regardless and that it was easier on Sundays with her daughter. She described the accountability of the treatment groups as a motivating factor to follow through with scheduled activities.
In the Life-Steps module, she discussed her frequent struggles with transportation to appointments. She identified numerous strategies and activities that may reduce transportation barriers to appointments (i.e., speaking with her husband about her transportation needs, scheduling appointments back to back when possible). As this was a recurring challenge for Tawanda, the therapist asked other group members if they had ideas of suggestions or resources for her. This strategy proved very successful, as a fellow group member pointed Tawanda toward a resource that pays the cost of public transportation to appointments—a resource that she was successfully utilizing by the end of treatment. Another key focus for Tawanda during the Life-Steps module was what her medications reminded her of; she indicated that medication acted as a reminder that she infected her husband with HIV. The Life-Steps strategies that focus on changing the meaning of medications were very relevant to Tawanda—specifically to change the meaning of the medications to be a reminder that the pills are lifegiving and a sign she is taking care of her health. Although Tawanda reported understanding this concept, it was unclear whether this shift in her views of her medications was achieved by the final week of treatment.
Tawanda’s BA goals and medication adherence strategies in Life-Steps were closely connected. Specifically, Tawanda had not disclosed her HIV status to anyone outside her family. Regarding female relationships in particular, she felt disconnected from her close female friends and reported feeling overly reliant on her 17-year-old daughter for emotional support. During treatment, her daughter was in the process of applying to college, and she experienced significant anxiety associated with her daughter leaving home. Additional BA goals focused on expanding her network of female friends as well as doing more social activities outside the home through her church. Related to medication adherence specifically, Tawanda would often hide her medications when she wanted to have friends over, which would contribute to nonadherence. Alternatively, she would also have periods of not inviting friends to her home, which was a valued activity for her. In both the Life-Steps and BA modules, balancing these two priorities was discussed; although she was not ready to disclose her status to her friends, other ways to maintain social contact and continue to prioritize adherence-related goals were discussed. Given that Tawanda’s fears about disclosing her status to others were such a pervasive concern, the therapist invited the entire group to comment briefly on any of their experiences related to disclosure (or lack thereof) of their HIV status. The short anecdotes two group members shared as part of this discussion appeared as helpful to them to share as they were for Tawanda to hear, and served to build rapport among the group members and the therapist.
Completing the monitoring and scheduling forms in between sessions was challenging for Tawanda. Specifically, she often forgot to record her activities on the homework forms and to check off scheduled activities to indicate she completed them. She attended five of the eight treatment sessions and brought her forms back to group one out of four possible sessions. Tawanda indicated she struggled to keep track of her forms after she went home but decided to keep them in a prominent place (the top of her dresser). This strategy worked for her for the last session she attended. She also reported more heavily relying on her own personal calendar.
After 8 weeks, Tawanda demonstrated clinically significant reductions in depression; her HAMD scores reduced from 14 at baseline to two, which is below the cutoff for clinically significant depressive symptoms. On the self-reported visual analogue scale of adherence, she increased from 97% to 100% adherence in the final 4 weeks of treatment. At 8 weeks, she reported similar reasons for nonadherence prior to treatment, and the frequency these reasons interfered with her medication adherence also remained stable (score of 13). Her physical health and mental-health-related functioning improved slightly over 8 weeks. Her PCS score increased from 40.9 to 49.7, and her MCS score increased from 32.8 to 39.5, both of which remained below the mean for the general population for both mental and physical health-related functioning.
Results
Preliminary Evidence
Examining outcomes over 8 weeks (n = 4), there were clinically significant reductions in HAMD scores from baseline from above the clinical cutoff of three (mean = 5.00; S.D. = 6.22) to below this clinical cut-off at Week Eight (mean = .75; S.D. = .96). There were also improvements in overall physical health-related functioning from baseline (mean = 41.63; SD = 11.32) to Week Eight (mean = 48.38; SD = 5.15) and improvements in mental-health-related functioning from baseline (mean = 46.28; SD = 11.99) to Week Eight (mean = 49.98; SD = 8.32), although both the mean baseline and Week Eight scores remained below the mean in the general population (50 for both the PCS and MCS). Regarding adherence, there were slight increases in adherence on a visual analogue scale from baseline (mean = 99.0; SD = 1.73) to Week 8 (mean = 100.0; SD = 0.0), and lower frequency of reasons endorsed for nonadherence from baseline (mean = 12.25; SD = 9.11) to Week 8 (mean = 9.5; SD = 6.95). Although clinical ranges are not available for this section of the ACTG assessing frequency of reasons endorsed for nonadherence, total scores range from zero to 42.
Exit Interview Feedback on the Intervention
Exit interviews were conducted after 8 weeks. Patients were asked to provide candid feedback about what aspects of group they found effective and recommendations for future modifications. Exit interview questions and synthesis of patient responses (n = 4) are included in Table 1. A few main themes emerged from participant feedback: an understanding of the treatment rationale, a sense of accomplishment from activity scheduling, an appreciation of being able to lead components of the group, and difficulties with homework completion.
Patients’ summaries of the group reflected a strong grasp of its content; patients described planning positive activities as a main focus of the group and gave concrete examples of goals they accomplished through completion of smaller, goal-directed activities. These included activities such as going to sleep at a specific time, taking walks for exercise every day, cleaning the kitchen, job application–related activities, and talking to doctors about side effects of HIV medications. Patients cited repeated review of the treatment rationale as a strength of the treatment; they felt it gave them an outlet to not just describe negative feelings, but also to get feedback on potential positive outlets from other group members and the therapist. Patients also indicated it allowed them to show what content they learned and recalled from previous sessions. The collaborative nature of the group was also referenced throughout interviews. For example, patients who missed a group one week reported they never felt lost or behind when they came back to group because their peers filled them in and led a review of previous sessions’ content.
Completing homework was something most patients felt was challenging, whether it was forgetting to fill out the forms, losing them at home, or forgetting to bring them back to the center. There were homework challenges that seemed unique to each patient, and several suggestions were provided that may be useful to adapt homework in the future. For instance, one patient recommended writing activities for each day on colorful sticky-notes (i.e., for the fridge). Overall, the interview feedback was positive, with all patients stating that they would recommend the group to others. This feedback will also help to inform future adaptations of the approach. See Table 1 for a list of exit interview questions and a compilation of example participant responses.
Discussion
Implementation Tips and Challenges
There were numerous challenges faced and lessons learned in the process of implementing BA and Life-Steps in a modular, nonsequential group format in an HIV community health center. A primary challenge was how to implement techniques effectively in the nonsequential format, balancing the need to engage patients who had attended the previous week with the needs of patients attending for the first time. One strategy that became particularly important to engage patients with regular past attendance was to utilize peer-led strategies. In particular, as done in previous BA studies (Daughters et al., 2008; Magidson et al., 2011), weekly patients volunteered to lead the treatment rationale cycle on a white board in front of the group after previous weeks’ attendance, which was facilitated by therapist and other patient input. Peers also offered support to other group members when filling out forms, brainstorming ideas for activities, and discussing obstacles to medication adherence. Individuals who had attended prior sessions could continue to build upon the life areas goals assessment, adding new goals across life areas and/or additional activities for existing life area goals; this allowed for all group members to be working on the same forms even if at different stages of completion. Additionally, regarding therapist training in this approach, future efforts to train clinicians in this type of protocol may consider content focused on adjusting to the nonsequential format.
Homework is a primary component of traditional CBT interventions delivered in a mental health setting; yet, assigning and reviewing written homework forms became less central in this nonsequential format. Many patients scheduled activities in other formats (using personalized calendars, notes at home, or without writing), and all formats for homework completion were reinforced regardless of format or whether the patient was planning to attend the following week. In BA protocols specifically, an in-depth review of activity monitoring is central to the therapeutic process; however, this became less feasible in a group format, particularly when multiple weeks had passed and the focus became more about training patients to be their own therapists to identify patterns in their activities and mood. Reviewing activity scheduling/completion during session was more feasible than a detailed review of activity monitoring. Patients were encouraged to find accountability from others in their environment for activity scheduling and completion when they could not attend the following week. Although other formats and techniques were utilized, assigning and reviewing homework in this context was perhaps the most challenging aspect of delivering the intervention.
Based on these experiences and feedback from patients, we believe the amount and type of homework should take into consideration the frequency and quality of clinical contact with patients, and clinicians should be prepared to adapt the homework format and delivery based upon these characteristics. For instance, some patients had multiple appointments per week, whereas others only came to the center once per month or less frequently. Thus, from our experience delivering the intervention, we found that the amount of activities to be scheduled in the BA protocol may change based on the frequency of clinical contact. More specifically, we found that it would not be feasible to generate a month’s worth of BA activities at one monthly appointment. In this case, the therapist and patient may consider generating a new activity that will likely happen each week to be scheduled on a specific day of the week (e.g., “take my grandchild to the park every Sunday afternoon.”) On the other hand, patients who have more frequent group attendance (e.g., once per week), could schedule activities for each day until their next group session. For patients who struggle a lot with homework, the therapist may consider just assigning one activity per week for later that same day of the group session. The essence of these recommendations is less that homework should be optional or only happen for certain sessions, but rather the amount/difficulty/frequency of the activities for homework should take into account how long it will be until the patient is likely able to attend group again.
In addition to modifications based upon schedule, there was also some feedback that the homework “wasn’t fun.” Some recommendations to make the homework forms more appealing include making them into a more colorful booklet, planner, or peel-away day calendar. Another option is to make the homework booklet small and easy to carry around at all times (i.e., similar to the pocket BA manuals utilized in Daughters et al., 2008, and Magidson et al., 2011). Another option to tailor homework to patient preferences is to ask patients in what ways they keep themselves organized currently, and attempt to integrate the format of the homework with what already works (e.g., notes on the refrigerator, Post-it notes, reminder stickers, or using a notes/calendar function on a cell phone). Additionally, although it is ideal for patients to be tracking activity completion and/or adherence in some way, if they prefer to verbally discuss activity completion without recording it (e.g., due to literacy issues or disabilities), this would also be preferable to not assigning homework.
Another key challenge that emerged was that patients were not presenting necessarily with a specific “diagnosis” or “presenting problem.” Patients were not screened into the group based on a formal depression or substance use disorder diagnosis; rather, the group was open to all patients interested (although there were policies in place at the center to ensure that patients who would be too disruptive could not be included—for instance, patients who presented drunk or high or were not stabilized on psychotropic medication/in psychiatric care through a specialist or a PCP could not participate). Patients were told the group would focus on various aspects of “healthy living,” including mood, healthy behaviors, and adhering to medication. Although this was particularly appealing to community health center staff wanting to maximize mental health resources for treatment-seeking patients, the heterogeneity of the group also presented challenges when prioritizing patient needs; for instance, the group often included patients with a wide range of ages, years living with HIV/AIDS, depression severity, and substance use issues, which influenced what content was most heavily focused upon in BA and Life-Steps. Each of the treatment components could easily be individualized and adapted to specific patient needs even in a group format, which has been a noted advantage of BA protocols (i.e., that they can be easily individualized to patient needs and priorities; Lejuez et al., 2011; Sturmey, 2009). For instance, specific adherence difficulties and strategies were individualized to each patient, as were the targeted goal-driven activities patients selected to implement. Given the flexible, modular format, we could also vary the specific time spent on each component based on patients’ needs and presenting issues on that day, but all components were covered in all sessions. Additionally, in line with this issue, not all patients identified with feeling “depressed” or “anxious.” The therapist was careful to use the words patients used to describe symptoms, normalize feelings of being down or depressed, and discuss how even when not “diagnosed” with depression, these tendencies can affect our ability to take our medications and engage in enjoyable activities. As depicted in the BA treatment rationale (Figure 1), the term “negative feelings” was used, as patients identified with this terminology.
Another significant challenge in this experience was how to accommodate various disabilities of patients who attended the group, including learning disabilities and other handicaps, which are often more common among individuals living with HIV/AIDS. For instance, one patient who attended regularly was visually impaired. The visual nature of the treatment rationale cycle and use of written forms were not feasible for this patient. However, one of her goals was to work on her handwriting, so she used the forms as a way to practice that goal. Other patients also helped her with completing her forms and tried to verbally summarize session concepts when possible to avoid overreliance on visual depictions.
Another challenge that presented in this group was how to engage patients, many of whom had been infected with HIV/AIDS for over 10 years, on Life-Steps material. Even in the presence of overall high levels of adherence, revisiting this material can be helpful, as previous research has shown that individuals may be likely to demonstrate poor adherence even after many years of managing HIV (Howard et al., 2002). Further, even individuals in this study who reported 100% adherence continued to report barriers to adherence, suggesting there is still room to address specific reasons or obstacles to adherence. Further, inaccurate beliefs may remain, even among those with high self-reported adherence. For instance, in this group, overall rates of adherence were high, but there were often gaps in their knowledge; they could identify that a high CD4 count and low viral load were “good,” but few of the group members knew or could recall what CD4 counts or viral loads meant prior to attending the Life-Steps module.
In examining patient feedback, individual patients appeared to give contradictory feedback on Life-Steps material, with one patient saying he was “sick of hearing about medicine” and later requesting “more information about side effects of HIV meds.” Overall, feedback on Life-Steps seemed to suggest that patients were “tired” of hearing about the importance of taking HIV medication and attending medical appointments, as this information had been presented to them in the same way for years. Many patients indicated that the adherence-related material they had received in the past was not helpful in increasing their level of adherence, and patients thought initially that this information would be the same. However, patients reported that they liked that the medication-related information in the Life-Steps module was discussed in the context of other activities and their mood and “not just the facts.” Many patients also discussed wanting more of a say in dictating what types of questions and information would be most useful to them. For example, many patients had questions about side effects of specific antiretroviral therapy drugs, new regimens available, how adherence to antiretroviral therapy could affect HIV transmission, and how medications work to stop replication of the virus. Despite years and even decades of contact with medical providers, group members expressed a feeling they were always “following doctors’ orders” without understanding the rationale behind those orders or the implications of them. This feedback was addressed using the flexible nature of the Life-Steps approach; the therapist made every effort to focus on particular “steps” that were most pertinent to the patients in attendance.
Although adaptations stemmed from setting-specific staff feedback and treatment needs, similar changes may be applicable to other medical settings without existing implementation of CBT. Settings with fewer resources available—for instance, without computers available to patients or on-site mental health staff who were available for ongoing support—may require even more attention in BA to assisting patients in creatively exploring what resources are indeed available at low cost in their community. This may in fact be more challenging when not on-site or immediately available, yet may provide even more opportunities for building these skills, which are the core of the BA approach. Other ideas for adaptation in low-resource community health settings may include the therapist focusing on identifying activities that may put patients in touch with external resources and available support systems, for example, how to become connected with a case manager or mental health worker. Those in substance abuse recovery may have a sponsor and sober network they can access. Additionally, as we learned throughout the implementation of this group, peers can be an incredibly helpful resource, and in this case, peers may also offer ideas for generating activities to determine what resources may be available. One example in the current study occurred when a patient said she struggled to afford transportation to appointments; a fellow group member pointed her to a program that covered the cost of public transportation for appointments, and by the end of the treatment she was successfully utilizing that resource. A similar idea may be to develop a list of low-cost activities and resources based on ideas generated throughout treatment, which could later serve as a reference to future groups being run at a given center. In sum, at low-resource settings, it is not necessary in this approach that patients find resources at the center where the treatment is being delivered. In fact, it may be even more helpful for patients long-term if they have to learn how to skillfully identify resources externally in order to make these changes more lasting in their environment. This may also further strengthen the key focus of BA—learning this skill of how to identify and pursue goal-driven activities.
Finally, regarding attendance, it is important to note that participants on average attended less than half of the eight sessions (i.e., a mean of 3.46 sessions). It is unclear at this stage of research whether nonattendance may be an issue for this program. There is empirical support for a single session of Life-Steps (Safren et al., 2001) and BA (Gawrysiak, Nicholas, & Hopko, 2009), which would suggest that even fewer than half of the sessions would be beneficial, particularly given that content is repeated weekly; however, larger trials evaluating this group will be necessary to determine the optimal number of sessions necessary for this approach to be effective. Further, in the current study, there were no efforts to promote or incentivize attendance: we were interested in rates of attendance without these efforts. However, it will be important to investigate strategies to promote attendance if nonattendance is an issue in future trials.
Limitations
In interpreting the preliminary outcomes of the patients assessed in this study, key limitations to consider may be the questionable representativeness of the research protocol sample. Only four individuals out of 13 total who attended the group completed research assessments; research involvement was not required for clinical participation, and thus, it may be a biased sample that elected to participate in research. Future plans to conduct a randomized trial to test the efficacy of this intervention will require higher rates of research participation. Similarly, it is also important to note that the 2 case studies presented may not be representative of the 13 total group members, as these 2 patients had higher attendance than the mean for the sample.
Another limitation is that throughout the sample as well as in the individual cases, there were high rates of adherence at baseline. Thus, we cannot ascertain from this study how this treatment may affect individuals with low baseline adherence. Previous studies of Life-Steps have demonstrated significant improvements in adherence among individuals with low baseline adherence. In future trials (vs. clinical adaptation projects such as this study), it will be important to consider recruiting based upon adherence levels; however, given that this project was a clinical service and staff wanted to provide it to anyone interested, it was not a key focus here, but remains a point important to acknowledge as a limitation and key consideration for future work.
Additionally, given the high rates of self-reported adherence, we relied more on the assessment of the frequency of missed doses across a range of reasons for nonadherence when capturing the changes in adherence in this sample. Although querying for reasons for nonadherence has been suggested to be a strategy to minimize social desirability biases and other inaccuracies of self-reported adherence by not asking about missed doses directly (Simoni et al., 2006), there are limitations to this measure. It may be that some individuals perceive greater barriers to adherence and report nonadherence across a range of reasons, whereas other individuals may consistently miss more doses but for a single reason. In this case, the measurement of frequency of reasons endorsed for nonadherence may not accurately reflect number of missed doses. However, despite these potential limitations of using reasons endorsed for nonadherence as a proxy for adherence behavior, the measure does provide rich clinical information about barriers to adherence that is not captured by reporting on missed doses, which has the potential to provide useful clinical targets in future developments of this work.
Conclusions
This report represents initial efforts to implement an integrated BA and Life-Steps treatment to improve depression and medication adherence in an outpatient community health center for individuals living with HIV/AIDS. Specific adaptations were necessary for delivery in a community health center, including a flexible, modular group format that did not rely on weekly, sequential session attendance. This report represents the first effort to implement Life-Steps in a group setting in conjunction with a brief BA protocol. There were numerous lessons learned, including how to address homework assignments and review without sequential session attendance, how to tailor medication adherence content most effectively, and how to utilize peer-led strategies to balance frequent attendees’ engagement with new patients’ needs. Preliminary evidence suggests feasibility of the approach and positive effects on mental and physical health functioning, depressive symptoms, and barriers to medication adherence over an 8-week period. This is a first step in disseminating integrated, evidence-based techniques for depression and adherence into a community health center for a hard-to-reach and difficult-to-treat population. Implementing interventions tested and designed for individual treatment in a mental health setting for group delivery in a medical setting is a struggle across types of disorders and interventions; it is our hope that the adaptation process and format depicted here may guide similar efforts in the future.
Highlights.
Implemented behavioral activation and Life-Steps in an HIV community health center
Designed a modular, group format that did not rely on sequential session attendance
Used peer-led and therapist-facilitated strategies to balance treatment needs of previous and new patients
Learned that homework assignment and review should be tailored based on attendance
Provide case examples and materials to depict how to implement techniques
Acknowledgments
Work on this manuscript was supported by grants R01DA022974 (PI: Daughters) and R36DA034513 (PI: Magidson). Dr. Safren is supported by grant K24MH094214. We would also like to acknowledge the support and assistance of Dr. Lance Morgan throughout the project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jessica F. Magidson, Massachusetts General Hospital/Harvard Medical School and University of Maryland, College Park
C. J. Seitz-Brown, University of Maryland, College Park
Steven A. Safren, Massachusetts General Hospital/Harvard Medical School
Stacey B. Daughters, University of Maryland, College Park, and University of North Carolina, Chapel Hill
References
- Aharonovich E, Hasin DS, Brooks AC, Liu X, Bisaga A, Nunes EV. Cognitive deficits predict low treatment retention in cocaine dependent patients. Drug and Alcohol Dependence. 2006;81(3):313–322. doi: 10.1016/j.drugalcdep.2005.08.003. [DOI] [PubMed] [Google Scholar]
- Aharonovich E, Nunes E, Hasin D. Cognitive impairment, retention and abstinence among cocaine abusers in cognitive-behavioral treatment. Drug and Alcohol Dependence. 2003;71(2):207–211. doi: 10.1016/s0376-8716(03)00092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376(9738):367–387. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangsberg DR, Perry S, Charlebois ED, Clark RA, Roberston M, Zolopa AR, Moss A. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15(9):1181–1183. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- Berg C, Raminani S, Greer J, Harwood M, Safren S. Participants’ perspectives on cognitive-behavioral therapy for adherence and depression in HIV. Psychotherapy Research. 2008;18(3):271–280. doi: 10.1080/10503300701561537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger-Greenstein JA, Cuevas CA, Brady SM, Trezza G, Richardson MA, Keane TM. Major depression in patients with HIV/AIDS and substance abuse. AIDS Patient Care and STDs. 2007;21(12):942–955. doi: 10.1089/apc.2006.0153. [DOI] [PubMed] [Google Scholar]
- Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, Wu W & the Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) Self-reported adherence to antiretroviral medications among participants in the HIV clinical trials: The AACTG Adherence Instruments. AIDS Care. 2000;12:255–266. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Fleming TR. Prevention of HIV-1 infection with early antiretroviral therapy. The New England Journal of Medicine. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crum NF, Riffenburgh RH, Wegner S, Agan BK, Tasker SA, Spooner KM, Wallace MR. Comparisons of causes of death and mortality rates among HIV-infected persons: analysis of the pre-, early, and late HAART (highly active antiretroviral therapy) eras. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2006;41(2):194–200. doi: 10.1097/01.qai.0000179459.31562.16. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Van Straten A, Warmerdam L. Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review. 2007;27(3):318–326. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Braun AR, Sargeant MN, Reynolds EK, Hopko DR, Blanco C, Lejuez CW. Effectiveness of a brief behavioral treatment for inner-city illicit drug users with elevated depressive symptoms: The Life Enhancement Treatment for Substance Use (LETS Act!) Journal of Clinical Psychiatry. 2008;69(1):122. doi: 10.4088/jcp.v69n0116. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Magidson JF, Schuster RM, Safren SA. ACT HEALTHY: A combined cognitive-behavioral depression and medication adherence treatment for HIV-infected substance users. Cognitive and Behavioral Practice. 2010;17:309–321. doi: 10.1016/j.cbpra.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Olalla PG, Knobel H, Carmona A, Guelar A, Lopez-Colomes JL, Cayla JA. Impact of adherence and highly active antiretroviral therapy on survival in HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes. 2002;30:105–110. doi: 10.1097/00042560-200205010-00014. [DOI] [PubMed] [Google Scholar]
- Ekers D, Richards D, McMillan D, Bland JM, Gilbody S. Behavioural activation delivered by the non-specialist: phase II randomised controlled trial. The British Journal of Psychiatry. 2011;198(1):66–72. doi: 10.1192/bjp.bp.110.079111. [DOI] [PubMed] [Google Scholar]
- Gawrysiak M, Nicholas C, Hopko DR. Behavioral activation for moderately depressed university students: Randomized controlled trial. Journal of Counseling Psychology. 2009;56(3):468. [Google Scholar]
- Giordano TP, Guzman D, Clark R, Charlebois ED, Bangsberg DR. Measuring adherence to antiretroviral therapy in a diverse population using a visual analogue scale. HIV Clinical Trials. 2004;5:74–79. doi: 10.1310/JFXH-G3X2-EYM6-D6UG. [DOI] [PubMed] [Google Scholar]
- Gonzalez J, Batchelder AW, Psaros C, Safren S. Depression and HIV/AIDS treatment nonadherence: A review and meta-analysis. Journal of Acquired Immune Deficiency Syndromes. 2011;58:181–187. doi: 10.1097/QAI.0b013e31822d490a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez JS, Psaros C, Batchelder A, Applebaum A, Newville H, Safren S. Clinician-assessed depression and HAART adherence in HIV-infected individuals in methadone maintenance treatment. Annals of Behavioral Medicine. 2011;42:120–126. doi: 10.1007/s12160-011-9268-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy W. ECDEU Assessment Manual for Psychopharmacology. U.S. Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration (DHEW Pub. No. 76-338; 1976. Retrieved from http://archive.org/stream/ecdeuassessmentm1933guyw/ecdeuassessmentm1933guyw_djvu.txt. [Google Scholar]
- Horberg MA, Silverberg MJ, Hurley LB, Towner WJ, Klein DB, Bersoff-Matcha S, Kovach DA. Effects of depression and selective serotonin reuptake inhibitor use on adherence to highly active antiretroviral therapy and on clinical outcomes in HIV-infected patients. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2008;47(3):384–390. doi: 10.1097/QAI.0b013e318160d53e. [DOI] [PubMed] [Google Scholar]
- Howard AA, Arnsten JH, Lo Y, Vlahov D, Rich JD, Schuman P, Schoenbaum EE. A prospective study of adherence and viral load in a large multi-center cohort of HIV-infected women. AIDS. 2002;16(16):2175–2182. doi: 10.1097/00002030-200211080-00010. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Dobson KS, Truax P, Addis ME, Koerner K, Gollan JK, Prince SE. A component analysis of cognitive behavioral treatment for depression. Journal of Consulting and Clinical Psychology. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- Kacanek D, Jacobson DL, Spiegelman D, Wanke C, Isaac R, Wilson IB. Incident depression symptoms are associated with poorer HAART adherence: A longitudinal analysis from the Nutrition for Healthy Living Study. Journal of Acquired Immune Deficiency Syndromes. 2010;53:266–272. doi: 10.1097/QAI.0b013e3181b720e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, Acierno R, Daughters SB, Pagoto SL. Ten year revision of the brief behavioral activation treatment for depression: Revised treatment manual. Behavior Modification. 2011;35(2):111–161. doi: 10.1177/0145445510390929. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, LePage JP, Hopko SD, McNeil DW. A brief behavioral activation treatment for depression. Cognitive and Behavioral Practice. 2001;8(2):164–175. [Google Scholar]
- Leserman J, Ironson G, O'Cleirigh C, Fordiani JM, Balbin E. Stressful life events and adherence in HIV. AIDS Patient Care and STDs. 2008;22(5):403–411. doi: 10.1089/apc.2007.0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPherson L, Tull MT, Matusiewicz AK, Rodman S, Strong DR, Kahler, Lejuez CW. Randomized controlled trial of behavioral activation smoking cessation treatment for smokers with elevated depressive symptoms. Journal of Consulting and Clinical Psychology. 2010;78(1):55–61. doi: 10.1037/a0017939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Gorka SM, MacPherson L, Hopko DR, Blanco C, Lejuez CW, Daughters SB. Examining the effect of the Life Enhancement Treatment for Substance Use (LETS ACT) on residential substance abuse treatment retention. Addictive Behaviors. 2011;36(6):615–623. doi: 10.1016/j.addbeh.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manos RC, Kanter JW, Rusch LC, Turner LB, Roberts NA, Busch AM. Integrating functional analytic psychotherapy and behavioral activation for the treatment of relationship distress. Clinical Case Studies. 2009;8(2):122–138. [Google Scholar]
- Mazzucchelli T, Kane R, Rees C. Behavioral activation treatments for depression in adults: A meta-analysis and review. Clinical Psychology: Science and Practice. 2009;16(4):383–411. [Google Scholar]
- McIntyre RS, Konarski JZ, Mancini DA, Fulton KA, Parikh SV, Grigoriadis S, Kennedy SH. Measuring the severity of depression and remission in primary care: validation of the HAMD-7 scale. Canadian Medical Association Journal. 2005;173(11):1327–1334. doi: 10.1503/cmaj.050786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiat. 1979;13:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Pence BW, O’Donnell JK, Gaynes BN. Falling through the cracks: the gaps between depression prevalence, diagnosis, treatment, and response in HIV care. AIDS. 2012;26(5):656. doi: 10.1097/QAD.0b013e3283519aae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter JF, Spates CR, Smitham S. Behavioral Activation group therapy in public mental health settings: A pilot investigation. Professional Psychology: Research and Practice. 2004;35(3):297. [Google Scholar]
- Safren SA, Gonzalez JS, Soroudi N. Coping with chronic illness: Cognitive behavioral therapy for adherence and depression in individuals with chronic illness, Therapist Guide. New York, NY: Oxford University Press; 2007. [Google Scholar]
- Safren SA, O'Cleirigh CM, Bullis JR, Otto MW, Stein MD, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2012;80:404–415. doi: 10.1037/a0028208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, O'Cleirigh C, Tan J, Raminani S, Reilly LC, Otto MW, Mayer KH. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychology. 2009;28(1):1–10. doi: 10.1037/a0012715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Otto M, Worth J. Life-Steps: applying cognitive behavioral therapy to HIV medication adherence. Cognitive and Behavioral Practice. 1999;6:332–341. [Google Scholar]
- Safren SA, W Otto M, Worth JL, Salomon E, Johnson W, Mayer K, Boswell S. Two strategies to increase adherence to HIV antiretroviral medication: life-steps and medication monitoring. Behaviour Research and Therapy. 2001;39(10):1151–1162. doi: 10.1016/s0005-7967(00)00091-7. [DOI] [PubMed] [Google Scholar]
- Shiu CS, Chen WT, Simoni J, Fredriksen-Goldsen K, Zhang F, Zhao H. The Chinese Life-Steps Program: A cultural adaptation of a cognitive-behavioral intervention to enhance HIV medication adherence. Cognitive and Behavioral Practice. 2012 doi: 10.1016/j.cbpra.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Chen WT, Huh D, Fredriksen-Goldsen KI, Pearson C, Zhao H, Zhang F. A preliminary randomized controlled trial of a nurse-delivered medication adherence intervention among HIV-positive outpatients initiating antiretroviral therapy in Beijing, China. AIDS and Behavior. 2011;15(5):919–929. doi: 10.1007/s10461-010-9828-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS and Behavior. 2006;10:227–245. doi: 10.1007/s10461-006-9078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soller M, Kharrazi N, Prentiss D, Cummings S, Balmas G, Koopman C, Israelski D. Utilization of psychiatric services among low-income HIV-infected patients with psychiatric comorbidity. AIDS Care. 2011;23:1351–1359. doi: 10.1080/09540121.2011.565024. [DOI] [PubMed] [Google Scholar]
- Soroudi N, Perez GK, Gonzalez JS, Greer JA, Pollack MH, Otto MW, Safren SA. CBT for medication adherence and depression (CBT-AD) in HIV-infected patients receiving methadone maintenance therapy. Cognitive and Behavioral Practice. 2008;15:93–106. [Google Scholar]
- Sturmey P. Behavioral activation is an evidence-based treatment for depression. Behavior Modification. 2009;33(6):818–829. doi: 10.1177/0145445509350094. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Weaver MR, Conover CJ, Proescholdbell RJ, Arno PS, Ang A, Ettner SL. Utilization of mental health and substance abuse care for people living with HIV/AIDS, chronic mental illness, and substance abuse disorders. Journal of Acquired Immune Deficiency Syndromes. 2008;47(4):449–458. doi: 10.1097/QAI.0b013e3181642244. [DOI] [PubMed] [Google Scholar]