Threats to an optimal end-of-life (EOL) experience of the American Indian and Alaska Native (AI/AN) people could be twofold. First, many AI/ANs consider discussing the topic of EOL and death taboo.1 In this view, speaking the words of death could invite evil spirits and elicit fear.1 Further, discussions on the topic could compartmentalize life and death and may force AI/ANs to detach personal meaning to life, which diverges from their cultural view where life is a continuum.2 Second, the limited availability of hospice services on AI/AN reservations is another threat to an optimal EOL experience where over 1.1 million AI/ANs reside.3
The avoidance of EOL discussions amongst the AI/AN patients and families may be part of the cause of the disparity in hospice use. Of all Medicare decedents in the United States (U.S.), 44.6% occurred under the care of a hospice program in 2011.4 While the AI/AN population comprises 0.9% of the U.S. population, they are only 0.2% of the users of hospice care.5
To narrow this hospice disparity, a partnership between an AI tribe and a university faculty member was established with a goal of introducing hospice services that were culturally appropriate. The research team initiated an assessment with the purpose of identifying the tribal values and contributing factors that influenced EOL care and decision making. Interview data regarding EOL experiences described by people in the partner tribe were analyzed. Reported here are the findings including the experiences of coping with the patients’ life-threatening chronic illnesses and the final stage of life, and the description of a culturally proper EOL. Implication introduces an intervention to address the taboo perception of discussing EOL issues while practicing the tribal culture and beliefs associated with death.
BACKGROUND
Partnership
The partnership between the tribe and the university was established in 2007 by using principles of community-based participatory research (CBPR).6 This community-centered approach engaged both partners in every research step and was conducive to collecting and analyzing data about the experiences of life-threatening illnesses and EOL care. The research team members included health care related professionals and academic associates from the tribe. Our study was modeled after six tribally successful palliative programs in the U.S.3,7
Partner Tribe
Forced to locate in a rural area of a frontier state, the partner tribe has suffered financially, physically, mentally, and spiritually since the encounter with Europeans.3 Despite the presence of an Indian Health Service (IHS) community hospital on the reservation that currently serves about 8,000 eligible tribal members, many of them feel abandoned by the U.S. government due to the inadequate health services provided as a result of a limited IHS budget.8 A lack of entitled health care frustrates them since their understanding of entitlement of health care was the U.S. government's commitment to the exchange of the most of the Indians’ land.9
The tribal government and health care workers of the partner tribe previously identified the need for hospice care. Efforts to address this need included unsuccessfully applying for external funding for hospice care, hosting a national level hospice teleconference, and designating a hospice room in the reservation nursing home. However, the overall attitude of tribal members toward EOL issues varied. The potential reasons for the open attitude were an exposure to Christianity and acculturation, which may have contributed to “[dispelling] the notion of the involvement of evil spirits in the death of people.”1(p.423)
The negative stigma associated with death exemplified a label of “death room” to an area at IHS hospital and the rarely used hospice room at the nursing home that only two patients used in 4 years. Instead of using this room, individuals when desired, went to the nearest cities (120 miles away) for available hospice care leaving home and family.
American-Indian Values and Beliefs related to Health
The family is a central core contributing to AI values and beliefs.2 Family, including extended kinships, is a unit of an individual AI's identity, a source of internal and external connections, and a foundation of their collectivism ideology.2 The family provides balance, harmony, and responsibility to the tribal life. Spirituality is another critical concept. It is defined as “a state of mind and heart, being a good person and living in harmony with nature.”2(p.75) Ceremonies, including powwows, sweat lodges (ritual steam baths for purification), drumming, prayers, smudging (use of herbal smoke for purification), etc. are ways of honoring or communicating with the people, land, life, and Creator that are in the spiritual realm.2
A disease is seen as “a disturbance in the relationship among self, spiritual forces, community and environment”2(p.16) and a process of regaining a balanced or meaningful relationship among these factors is described as healing in AI medicine. Death itself is a part of life and accepted when caused by accident or war. However, when death is the result of disease, many AIs have difficulty accepting it. This is especially true concerning infectious diseases because these diseases were not recognized until encountering Europeans.9
METHOD
An exploratory study was designed with the grounded theory method. Combined with interviews, this approach was appropriate to the study purposes since data analysis is grounded in collected data to identify meanings of the participant's EOL experiences and interactions with others.10
Samples
The team recruited participants from four cohort groups. They were: (1) family members who lost their loved ones with a life-threatening illness, (2) patients who had a life-threatening illness, (3) family caregivers of a family member with a life-threatening illness, and (4) health care providers (HCPs; physicians, nurses, and social workers) who had worked on the reservation for more than 2 years with license. The inclusion criteria regarding age (over 21), language (English), and self-identification of tribal members or the descendants who lived on the reservation were set to avoid extraneous data and to focus on the tribal culture.
Procedure
The academic partner (AP) drafted interview questions based on her dissertation study of Japanese Americans’ EOL experiences.11 A typical starting question was “Could you share with me your story?—What was it like to be with your (loved one) when he/she was getting weak?” or “—How would you be dealing with your cancer after you were diagnosed?” In addition to asking all of the participants about their daily life experiences associated with a life-threatening illness and a view on hospice care, the interview for each cohort group had different focus. The focal areas for cohort 1 were their interaction with the deceased and the process of EOL decision making. The focal areas for cohort 2 and cohort 3 were their perceptions of the illness and future. The focal areas for cohort 4 were their perspectives on EOL decision making and care. The research team members examined the questions in terms of cultural relevance and comprehensiveness, and made an amendment expanding participant's age range from over 40 years old to 21 years old and patient's age range from over 60 years old to over 40 years old based on the pilot study results to be more inclusive. Two community research associates were trained by the AP using three methods: reviewing sample interview questions, observing an interview with the interviewee's permission, and being an interviewee to promote an interviewer's role and understand an interviewee's feelings. Then all three took an interviewer's role independently.
Five Institutional Review Boards (Tribe, university, regional and national IHS, and NIH) approved the research protocol. Methods of recruitment included approach by the team members, advertisement through posters and workshops, and visits to the health care agencies. In general, tribal team members approached potential participants, explained about the research, and obtained their permission for an interview. The team members shared the contact information of the potential participants with the interviewers. The interviewers called respectively and made an appointment for an interview if the potential participants were interested and met inclusion criteria. The research team was very careful to avoid the perception of coercion. Demographic-based purposive sampling in gender and generation was used for later recruitment (i.e., inclusion of more males and younger participants).
After receiving informed consent, a one-time, in-person interview, ranging from 23 minutes to 2 hours and 15 minutes, was done at the interviewee's residence for most of the interviews. A transcriptionist transcribed the audio-taped interviews verbatim and two interviewers reviewed each transcription for content accuracy (e.g., verbatim, observation).
Data Analysis
QRS NVivo 8 software program (Doncaster, Australia) was used for the initial data analysis. Participant's experiences were constantly compared based on their demographic characteristics, difficulty living with a life-threatening illness of self or family member, their interactions with others, and the process of decision making. The AP initiated an open coding. Data analysis was facilitated through participation of the research team and the community. For example, discussions among the research team, the Tribal Council, and the community led to deeper understanding of the participants’ experiences from not only the outsider's viewpoint but also among themselves. Many tribal members who were immersed into their own culture had some difficulty identifying the uniqueness of the EOL experiences. The gatherings with community members and the research team, focusing on theoretical coding and the use of theoretical memo and document trails assisted in identifying categories and relationships. Community members and Tribal Council confirmed the accuracy of the final stage of the data interpretation.
RESULTS
Participants
After 85 potential participants were identified, a total of 73 individuals made the interview appointments over 3 years. With 10 people unable to attend the interviews and 5 people who did not meet the inclusion criteria, 58 participants contributed to the analyzed data. Data consisted of 65 patients’ stories since the participants often shared multiple patients’ stories. For example, one participant talked about a deceased father, a deceased grandmother, and a mother with cancer diagnosis, which produced 3 patient cases and 3 relationships. Tables 1 and 2 show the demographic data of the participants and patients in detail.
Table 1.
Participants’ demographic data
| Participants N=58(%) | Group 1 n= 37(%) | Group 2 n=10(%) | Group 3 n=17(%) | Group 4 n=6(%) | |
|---|---|---|---|---|---|
| Gender | |||||
| Men | 29(50) | 17(46) | 5(50) | 8(47) | 2(33) |
| Women | 29(50) | 20(54) | 5(50) | 9(53) | 4(67) |
| Age | |||||
| 20-29 | 10(17) | 6(16) | 4(24) | ||
| 30-39 | 6(10) | 5(14) | 2(12) | ||
| 40-49 | 12(21) | 7(19) | 5(50) | 3(18) | 1(17) |
| 50-59 | 14(24) | 8(22) | 2(20) | 2(12) | 1(17) |
| 60-69 | 9(16) | 7(19) | 1(10) | 5(29) | 3(50) |
| 70-79 | 3(5) | 2(5) | 1(10) | 1(17) | |
| >80 | 4(7) | 2(5) | 1(10) | 1(6) | |
| Race | |||||
| Indian | 57 (98) | 37(100) | 10(100) | 17(100) | 5(83) |
| Non-Indian | 1(2) | 1(17) | |||
| Religion | |||||
| Catholic | 42(72) | 26(70) | 9(90) | 16(94) | 2(33) |
| Native | 6(10) | 4(11) | 1(6) | 1(17) | |
| Both | 8(14) | 5(14) | 1(10) | 3(50) | |
| Others | 2(4) | 2(6) | |||
| Recruitment | |||||
| Personal | 46(79) | 29(78) | 7(70) | 17(100) | 3(50) |
| Self-identified | 7(12) | 4(11) | 1(10) | 2(33) | |
| Awareness project | 2(3) | 2(5) | 2(20) | ||
| Direct approach | 2(3) | 1(3) | 1(17) | ||
| Snowballing | 1(2) | 1(3) | |||
| Family unit | |||||
| Dyad | 9 | 4 | [3] | 5 | |
| Triad | 2 | 1 | [1] | 1 | |
| Relationships | |||||
| Mother | 15(18) | 11(22) | 4(24) | ||
| Father | 13(15) | 12(24) | 1(6) | ||
| Self | 10(12) | 10(100) | |||
| Grandmother | 8(10) | 7(14) | 1(6) | ||
| Aunt | 7(8) | 4(8) | 3(18) | ||
| Friend/ Husband | 5(6)each | 4(8)each | 1(6)each | ||
| Brother | 5(6) | 2(4) | 3(18) | ||
| Sister/ Ex-husband | 2(2)each | 1(2)each | 1(6)each | ||
| Grandfather | 2(2) | 2(4) | |||
| Wife/ Uncle | 1(1)each | 1(2)each | |||
| Unofficial wife | 1(1) | 1(6) | |||
| Partner | 1(1) | 1(2) | |||
| Health Care Provider | 6(7) | 6(100) | |||
| Total | 84(100) | 51(100) | 10(100) | 17(100) | 6(100) |
Group 1: Family members who lost their loved ones; Group 2: Patients with a life-threatening diagnosis; Group 3: Family caregivers of an ill family member currently; Group 4: health care providers (physicians, nurses, & social workers)
Table 2.
Demographic Data of All Patient Cases
| Patient cases n=65(%) | Group 1 n=45(%) | Group 2 n=10(%) | Group 3 n=14(%) | |
|---|---|---|---|---|
| Gender | ||||
| Men | 31(48) | 24(53) | 5(50) | 5(36) |
| Women | 34(52) | 21(47) | 5(50) | 9(64) |
| Age | ||||
| 40-49 | 9(14) | 1(2) | 5(50) | 4(29) |
| 50-59 | 16(25) | 12(27) | 2(20) | 3(21) |
| 60-69 | 10(15) | 7(16) | 1(10) | 2(14) |
| 70-79 | 15(23) | 11(24) | 1(10) | 4(29) |
| >80 | 10(15) | 9(20) | 1(10) | 1(7) |
| >40 but unknown | 5(8) | 5(11) | ||
| Medical Diagnoses | ||||
| Lung Cancer | 14(22) | 11(24) | 1(10) | 3(21) |
| Breast Cancer | 10(15) | 4(9) | 2(20) | 4(29) |
| Stomach Cancer | 7(11) | 4(9) | 1(10) | 2(14) |
| Brain Cancer | 4(6) | 3(7) | 1(7) | |
| Prostate Cancer | 3(5) | 2(4) | 1(10) | 1(7) |
| Blood/Colon Cancer | 2(3)each | 2(4)each | ||
| Cervical Cancer | 2(3) | 1(2) | 1(7) | |
| Ovarian/Testicular Cancer | 1(2) each | 1(10)each | 1(7)each | |
| Bone Cancer | 1(2) | 1(2) | ||
| Unspecified cancer | 6(9) | 6(13) | ||
| Heart Disease | 2(3) | 2(4) | ||
| Lung Disease | 2(3) | 1(2) | 1(10) | |
| Kidney/Liver Disease | 1(2) each | 1(2) each | ||
| Other | 6(9) | 4(9) | 2(20) | |
| Length of illness | ||||
| <3 months | 5(11) | 1(7) | ||
| 3- <6 months | 1(2) | 1(10) | 1(7) | |
| 6- <12 months | 8(18) | 2(20) | 1(7) | |
| 1- <2 years | 4(9) | 3(30) | 2(14) | |
| 2 - <5 years | 8(18) | 2(20) | 2(14) | |
| 5 - <10 years | 3(7) | 2(20) | 4(29) | |
| >10 years | 5(11) | 2(14) | ||
| Unknown | 11(24) | 1(7) | ||
| Perception difference | 3 pairs(5) | |||
| Place of death | ||||
| Hospital | 20(44) | |||
| Home | 12(27) | |||
| Hospice | 5(11) | |||
| Nursing Home | 4(9) | |||
| Missing data | 4(9) | |||
| Religion | ||||
| Catholic | 26(58) | 9(90) | 11(79) | |
| Native | 2(4) | 1(7) | ||
| Both | 3(7) | 1(10) | ||
| Methodist | 1(2) | |||
| Missing data | 13(29) | 2(14) |
Cohort 1 was comprised of 37 family members who described a total of 45 deceased individuals. The hospital was the location of 20 patient deaths (44%) while 5 patients (11%) used hospice either at home (out of state) or a facility. Cohort 2 consisted of 10 ill patients. Six patients were in remission after cancer treatments. Another patient passed away 3 days after the interview. Cohort 3 was comprised of 17 family caregivers who described 14 living patients. Among the 14 patients, four patients were in the cohort 2. Cohort 4 included six HCPs, one was non-AI and five were AI HCPs. The genders and ages of participants and patients were evenly distributed. The participants expressed their emotions verbally or nonverbally (e.g., tears, pauses) during the interviews and completed their interview except for one participant who discussed one patient's story and then desired to stop talking about a second patient's story while in the process of sharing. The participant gave the interviewer permission to include the first patient's story.
Overview
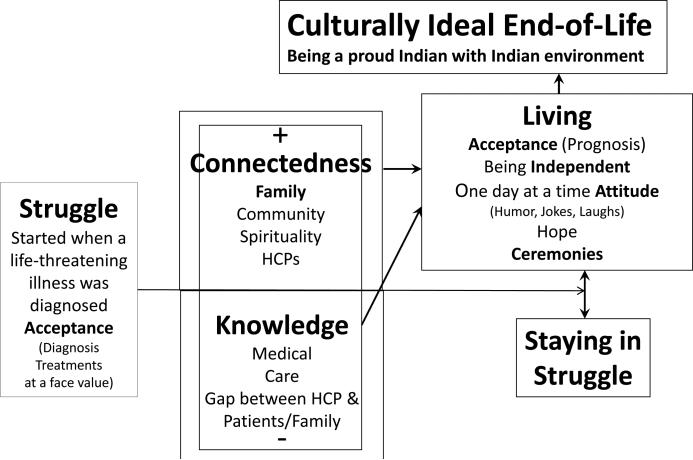
We found a main theme, two influential factors, two dimensions, and AI's values from the interview data of AI's EOL experiences. The main theme identified was Struggle (Figure 1). This core theme of Struggle proceeded to two dimensions of Living (the majority) and Staying in Struggle (the minority) after being influenced by two factors of Knowledge and Connectedness. Knowledge and Connectedness occurred along a continuum from low level to high level. These two factors were not mutually exclusive as indicated with their overlapping rectangles in the Figure 1. Two types of Acceptance occurred in the Struggle and Living section respectively. Living involved various coping strategies including two influential factors of Knowledge and Connectedness and the values. Then Living directed towards an ultimate value, Culturally Ideal EOL, signifying being a proud Indian and longing for an Indian way of life internally with an Indian environment and culture externally at their life ending. The following sections expand on the elements of the figure, starting with the theme (Struggle), two influential factors (Knowledge, Connectedness), two dimensions (Living, Staying in Struggle) and their components, then describe the relationship between the ideal life ending and the dimension of Living.
Figure 1.
Struggle end-of-life experience by American Indians was influenced by Knowledge and Connectedness to cope with a life-threatening chronic illness and proceeded to Living or Staying in Struggle, ultimately wishing to have Culturally Ideal End of Life.
Struggle
Struggle was defined as making strenuous efforts in the face of difficulties, or proceeding with difficulty or with great effort. The participants’ struggle started when they were given a life-threatening diagnosis of self or their family member. Acceptance was defined as a mental state of being able to take things as they are. The initial stage of Acceptance was that of diagnosis and treatment and occurred at face value in almost all cases while there may be struggle with other aspects.12 Without questioning the diagnosis and treatment or having an opportunity to ask for a second opinion, the AI participants felt that the diagnosis was given to them.12 Usually the family accepted after the patient did. Limited access to health care services was an identified external source of Struggle. Many participants perceived difficulties in the areas of struggle including the financial, geographical, and timing aspects that had affected their daily life.
If he would have taken [radiation], we'd have to take him to B (a location 120 miles away) every day, every day, if that's what he [had chosen].
...but we were just really unable to go [to the hospice facility] and spend the time with her that she needed, so sometimes she was alone in a hospice, and I think it took a toll on her, not having people around her all the time.
Internal source of Struggle was associated with levels of two influential factors, Knowledge and Connectedness.
Knowledge
Knowledge was divided into two categories: Medical and Care. Medical knowledge about the physical and mental progression of the illness and cancer associated pain, were the main areas discussed. Informative medical knowledge was not always conveyed from the HCPs to the patients and families from the latter's viewpoint. For example, lack of knowledge about cancer causing depression or pain led some family to criticize their ill family member's antisocial behavior. Later, they regretted their actions and wished they would have known the illness trajectory and psychological effects on the patient's mind.
Care knowledge was defined as information needed for self-care or patient care in daily life. Knowledge and resources were insufficient for individuals to confidently take care of themselves or ill family members with the gap of knowledge between the HCPs and the patients and families perceived as being enormous. Available knowledge sources included the limited experiences of their own, relatives, and/or acquaintances, brochures and some nurses’ advice.
Knowledge that was needed but patients and family members didn't have included (1) physical care (e.g., [tube] feeding, dressing changes), (2) practical care related to life adjustments (e.g., foods to avoid, adaption of wig, bra, and catheter), (3) support care (e.g., how to approach the cancer patient), and (4) what to do in the case of an emergency (e.g., when an imminent moment preceding death arrived). One patient stated that her illness experience was a trial and error on her own body since no resource was available for her specific concerns and questions. Perception of a lack of knowledge resulted in the patients and families feeling helpless, hopeless, anxious, panicked, and frustrated. The patients and families took an attitude of one day at a time to overcome their limited knowledge and to accept their new daily life.
Regarding hospice care, the participants were rarely aware of the hospice room in the local nursing home. The participants’ responses to the infrequent use included: (1) negative connotations of the nursing home, (2) community-wide unfamiliarity with the word “hospice,” (3) a lack of formal hospice training for nursing home staff, and (4) possible miscommunication of the meaning of the hospice concept. Some participants believed a discussion about EOL issues was taboo and others thought that choosing hospice meant “giving up” hope for, and life of, an ill-family member. However, once correct information about hospice was shared after the interview, the participants praised its holistic approach that resembled an AI healing approach.13
Connectedness
Connectedness was defined as association with, or relation to, others or between two entities. Four categories of Connectedness were family, community, spirituality and HCPs. Family was used to include blood relations and extended family. Family was the participants’ critical support system and provided resources as well as their identity. Family connectedness was manifested in offering physical care and support, sharing knowledge, being there, visiting, talking with humor and laughter, and praying. A participant shared how her connection to the patient helped to cope with the situation.
... Because at the time, the way that everything was [going], I guess, I guess I could say that I was more of a best friend to him, than I was a wife, because of what I went through (an alcoholic patient went to heart surgery then cancer was found). But as a best friend, it was really hard for me because he would go through all that...I made myself stand, step back, and take it in as a best friend, that somebody who would be there right up to the end.
Community connectedness (visits and a fundraising) was appreciated while disappointing when social isolation happened due to a stigma that cancer was contagious. Spirituality was practiced through prayer, smudging, face painting, and/or visiting a personal sacred place. Prayer was the most used ceremony that communicates with the Creator to supports the self, patients and families. Especially, it was emphasized when a participant could not be present with the ill family member. The connectedness to HCPs was expressed with a “distant” or authoritative figure in the majority cases12 while a fewer participants described it as a trustable or reliable relationship. Culturally, the participants felt that they should not question their physicians. The IHS service was applauded for making the rapid treatment decisions after diagnosed with cancer.
Living
Living was an overarching dimension to describe participants’ coping mechanisms including attitudes and values during the EOL experiences and the survival period. Five components to Living were: Knowledge, Connectedness, Independence, Attitude of Life, and Ceremonies. In general, the more knowledge the participants perceived they had and the stronger their connectedness to family, community, spirituality, and HCPs, the easier they appeared to cope with the Struggle situations. Acceptance of prognosis and death varied among individual cases depending on components of Living. For example, gaining knowledge about her family member’s illness made the participant stronger and better prepared to cope.
The rest of them (the family members) dealt with it (patient's illness) in different ways. I understood that... because they didn't know how to deal with it too; they kind of ran away from it, you know... I just tried to help them (patient & the spouse)... cope with it by being there in any way I could. So I am just glad, I think, and thankful that I was able to learn about it (disease) in the beginning and grieve it first, then be there throughout the whole you know two years that it happened because I felt like I accepted it.
A patient's losing independence (physically, psychologically, or spiritually) facilitated a process of Acceptance of the patient's prognosis and death through one's own self-awareness or family member's recognition of the patient's unrecoverable condition. When the patient's dignity was threatened, the participant felt it as leading to the patient's loss of living force/life energy.
After my dad fell, I think that's when his fight went because they put a catheter in, and he cried. He literally cried, and begged them not to. He even promised he wouldn't pee anymore because he didn't want them to do that. And I remember standing out in the hallway, and hearing him scream ... and cry. When we went back in there, it was like somebody had beaten him, or violated him. He was a broke man then, and I saw that difference, in that fight, to no fight.
Keeping hope was extremely critical and a driving force of Living. Attitudes of keeping hope and ‘not giving up’ versus acceptance illustrated vacillating minds of the participants with a balance between fighting or supporting a fight against a life-threatening illness and making the patient comfortable. Also, the content of hope changed along with the progression of an illness. When family members hoped for a patient's recovery, for example, they had hard time to accept the actual prognosis. However, their hope was not for recovery but, rather, for the patient's comfort, “do not give up” meant to live up to fulfill their destiny and faith until death. Then, hope and an acceptance of the prognosis were able to coexist.
Staying in Struggle
Staying in Struggle was a state of a participant who could not move on to Living and was manifested through acting out, use of alcohol, and statements of regret and prolonged grief at the time the death occurred or when they were interviewed. The individuals in this state tended to isolate themselves from their family. Even though laughter could be a medicine, it also appeared to be used for hiding emotions and psychological despondency such as sadness, loneliness, and feelings of abandonment and depression. A belated notice of a life-threatening diagnosis of the patient made the family feel anger and guilt. The family wished they could have done more for their deceased. HCPs observed that an unhealthy connection, selfishness, and dysfunctional family tie led to a vicious cycle and crisis oriented behaviors, thus, prolonging the grief.
Culturally Ideal End of Life & Its Relation to Living
A participant summarized that AIs would be most comfortable staying in their own environment and practicing their native culture and own spirituality to handle the EOL situation. Their ideal life ending was to recognize them self as a proud Indian. Maintaining physical strength, being spiritual, not being depressed, and connecting to the Creator (many participants overlapped this with religious faith) were highlighted in the Living dimension toward the ideal life ending. A participant reflected his/her own attitude toward death.
Don't drink around, crying around about me passing away because then you neglect your family; you neglect your kids; you neglect your life; you neglect your neighbor; you neglect everything... You can still be a teacher. You can still help your family. Show them that there is a good way to die. It (Death) isn't something that you have to... It is all going to happen to us. It is not something that you have to fear or be afraid of but you can teach people how to live well by how you die.
In addition, several participants shared their observed symbols/signs near or after the loved one's passing. The symbols/signs (eagles, eagle feathers, music, shape of clouds, feeling of love) assisted the family members to make sense out of their EOL experiences and led them to a healing process. Therefore, the culturally ideal life ending would represent connection with nature and environment, and death should be accepted when the time came.
DISCUSSION
Data analysis indicated that EOL experiences by the AI participants were reiterated with Struggle and that they tried to cope with the situations by seeking Knowledge and applying Connectedness to family, community, spirituality, and HCPs (Figure 1). Whatever levels of Knowledge and Connectedness were acquired in a particular circumstance of the patient, the majority of the AI participants reached Living, and the minority had Stayed in Struggle. With knowledge of their own, vicarious experiences, and interactions with family, relatives, community, and Creator, the participants coped with the Struggle through their traditional cultural values and ceremonies. Their Culturally Ideal EOL was identified as being a proud Indian and living the Indian way of life to the end.
What does the Indian way of life mean to the participants? AI culture is dynamically evolving along with time, locations, and situations.14 This evolvement could be seen as “adaptive behavior for the sake of survival” rather than “a natural cycle of change”15(p.63) of the AI's responses to White privileged society, especially medicine. Our data indicated that many participants had incorporated traditional “healing” practices (i.e., family gatherings and ceremonies) to deal with the patient's medical condition as if they value “maintaining a strong cultural identity while resisting assimilation.”16(p.21)
A balance between the two concepts of self is an adaptation example. A significant value of connectedness or interdependent-self appeared to co-exist with their independent self. Self-concept depends on inner attributes, abilities, and opinions from the community based on collective ideology. Connectedness to family and community was revealed with caring, ‘being there’, humor, jokes, laughter, and ceremonies that signified relational values. In contrast, spirituality and being independent expressed personal internal values. Thus, the Indian way of life emphasizes both traditional values of family and two types of connectedness (relational & internal) within a current living condition.
Peroff and Wildcat present a continuum model of AI identity that was supported by a theory of understanding tribes as complex adaptive systems (CAS).14 A CAS is defined as “a dynamic process of self-organizing parts that come from and go back to the environment.”14(p.6) The participants of the current study can be called “a spatially defined Indian identity” that lies “fundamentally shaped and literally ‘grounded’ in specific, geographically identifiable places”14(abstract) and “emerges from the experience of real life activities and events, some everyday in character and some extraordinary.”14(p.13) The land-based philosophy is the center of AIs;17 therefore, the reservation would have a special meaning for the participants.
All of the elements of the developed figure in this study (Figure 1) were found in the Medicine Wheel, which validated our data analysis despite the non-resemblance of the figure to Medicine Wheel.18 The Medicine Wheel is a circle with 4 divisions that represents the general AI culture of harmony and connections. Many participants practiced prayer, seeking a direct connection to the Creator to maintain their own integrity. To live a meaningful life, discovering a purpose through a vision quest or prayer was a traditional practice that deepened the individual's connection to the Creator.2 Living with a life-threatening illness of one's own or that of an ill family member was an opportunity for some participants to practice such spirituality.
Our finding revealed similarities to and differences from the existing literature. For example, Revier, Meiers and Herth19 investigated the concept of hope through the experiences of six Caucasion family caregivers who cared for their terminally ill loved one in a hospice program. The authors illustrated that hope was a possibility as opposed to suffering. Hope focused on seeking comfort and important connections. Thus, hope was conceptualized more broadly and deeper. Revier, et al. found 4 interconnected themes in their phenomenology study:19 (1) engaging, strengthening, and maintaining connections, (2) easing of self, (3) finding meaning in the situation, and (4) acceptance. The themes of connections and acceptance were identified in our study as well. The third theme of finding meaning in the situation could be matched with symbols/signs in our study where AIs found meanings in events and phenomena and use nature and animals to symbolize the meanings.17 In particular, the Creator was divine and the only one to control the world and life.17 Therefore, symbolization may make them connect with the Creator, realize the meanings, and find it easier to accept life as it is.
However, the theme of easing of self by Revier, et al. did not appear as a strong statement in our study. A potential explanation for this difference is that the patients in the Revier et al.'s study19 were under hospice care; thus, the study participants received physical and informational supports and reassurance from HCPs whereas the participants in our study did not. Further, the authors19 explained a phenomenon of paradoxical rhythm of connecting/separating and comfort/discomfort that occurred during the final days. While connecting with the dying loved one, the family caregiver's mind was separating “physically and emotionally in preparation for a future without them.”19 Even though the attitude of one day at a time was common in both studies, apparent separation between the caregiver and the patient was not described in our study. A different view of construed self, one is an independent self in the White population versus a mixed self-concept within the AI population, could be a potential explanation of the difference. A present-time orientation of AIs might have discouraged their future thinking as well.
In conclusion, we identified both medical and care knowledge acquisition by the patient and family as well as strengthening connectedness among involved parties (i.e., patient, family, community, spirituality, and HCPs) as critical factors to improve AI's EOL experiences. The patient's feeling of interdependence of body, mind, and spirit and wholeness would be actualized at the end2 if a homelike environment were provided for patients and their families.
Implication
How can EOL discussion be introduced to the partner tribe? The research team plans an intervention that includes a training of selected local people to be lay health educators who can share the hospice concept to the tribal public. Culturally sensitive, trusted relationships among tribal members, use of oral tradition, and regularly held workshops will be conducive to increase the knowledge and resources for EOL care and options. It is the hope that reducing hospice disparity will lead AI patients and families to their ideal life ending experience.
Acknowledgements
The authors would like to express appreciation to the research participants, the tribal council, the research team members, and the colleagues at MSU for their support.
This work was supported by the National Institute on Minority Health and Health disparities [P20MD002317], the LIVESTRONG Foundation, and MSU-Bozeman College of Nursing Block Grant. Approved by Blackfeet Nation IRB# 14-04.
Contributor Information
Yoshiko Yamashita Colclough, Montana State University- Bozeman, Associate Professor Current address: PO Box 173560, Bozeman MT 59717-3560
Gary M. Brown, Current address: Montana resident Contact information: garymbrown2012@yahoo.com.
References
- 1.Reid R, Rhoades ER. Cultural Considerations in Providing Care to American Indians. In: Rhoades ER, editor. American Indian Health: Innovations in Health Care, Promotion, and Policy. The Johns Hopkins University Press; Baltimore: 2000. pp. 418–425. [Google Scholar]
- 2.Cohen K. Honoring the Medicine. Ballantine Books; New York: 2003. [Google Scholar]
- 3.Baldridge D. [April 13, 2012];Moving Beyond Paradigm Paralysis: American Indian End-of-Life Care. 2011 www.chronicdisease.org.
- 4.National Hospice and Palliative Care Organization . NHPCO Facts and Figures: Hospice Care in America. Alexandria, VA: 2012. [Google Scholar]
- 5.Hackbarth GM, Berenson RA, Miller ME. Report to the Congress: Medicare Payment Policy. Washington D.C.: Mar, 2011. p. 384. [Google Scholar]
- 6.Christopher S, Saha R, Lachapelle P, et al. Applying Indigenous Community-Based Participatory Research Principles to Partnership Development in Health Disparities Research. Family & Community Health. 2011;34(3):246–255. doi: 10.1097/FCH.0b013e318219606f. 210.1097/FCH.1090b1013e318219606f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DeCourtney CA, Jones K, Merriman MP, Heavener N, Branch PK. Establishing a Culturally Sensitive Palliative Care Program in Rural Alaska Native American Communities. Journal of Palliative Care. 2003;6(3):501–510. doi: 10.1089/109662103322144871. [DOI] [PubMed] [Google Scholar]
- 8.National Tribal Budget Formulation Workgroup Creating A Legacy of Honor and Trust: Striving for Health Parity for all American Indians and Alaska Natives. 2013 [Google Scholar]
- 9.Dejong DH. If You Knew the Conditions. Lexington Books; Lanham, MD: 2008. [Google Scholar]
- 10.Glaser B, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. Aldine; Chicago: 1967. [Google Scholar]
- 11.Colclough YY, Young HM. Decision Making at End of Life Among Japanese American Families. Journal of Family Nursing. 2007;13(2):201–225. doi: 10.1177/1074840707300761. [DOI] [PubMed] [Google Scholar]
- 12.Colclough YY, Brown GM. End-of-Life Treatment Decision Making: American Indians' Perspective. Journal of Hospice & Palliative Care Medicine. 2013 doi: 10.1177/1049909113489592. doi 10.1177/1049909113489592. [DOI] [PubMed] [Google Scholar]
- 13.Marr L, Neale D, Wolfe V, Kitzes J. Confronting Myths: The Native American Experience in an Academic Inpatient Palliative Care Consultation Program. J Palliat Med. 2012 doi: 10.1089/jpm.2011.0197. [DOI] [PubMed] [Google Scholar]
- 14.Peroff NC, Wildcat DR. Who is an American Indian? Social Science Journal. 2002 Nov 11;39(3):349–362. 2012. [Google Scholar]
- 15.Horse PG. Native American Identity. In: Fox MJT, Lowe SC, McClellan GS, editors. Serving Native American Students. Vol. 109. Joseey-Bass; San Francisco: 2005. pp. 61–68. [Google Scholar]
- 16.Larimore JA, McClellan GS. Native American Student Retention in U.S. Postsecondary Education. In: Fox MJT, Lowe SC, McClellan GS, editors. Serving Native American Students. Vol. 109. Joass; San Francisco: 2005. pp. 17–32. [Google Scholar]
- 17.Fitzgerald MO, Fitzgerald J, editors. Indian Spirit. 2nd ed World Wisdom, Inc.; 2006. [Google Scholar]
- 18.Roberts RL, Harper R, Bull T-E, Heideman-Provost LM. The Native American Medicine Wheel and Individual Psychology: Common Themes. Journal of Individual Psychology. 1998;54(1):135. [Google Scholar]
- 19.Revier SS, Meiers SJ, Herth KA. The Lived Experience of Hope in Family Caregivers Caring for a Terminally Ill Loved One. Journal of Hospice and Palliative Nursing. 2012;14(6):438–446. [Google Scholar]