Abstract
Purpose
To study time trends of antidepressant drug (AD) prescriptions in a geographically defined US population between 2005 and 2011 for men and women separately.
Methods
Using the Rochester Epidemiology Project medical records-linkage system, we identified all Olmsted County, MN residents who received AD outpatient prescriptions between 2005 and 2011 (seven years). We calculated the annual age-and sex-specific prevalence over seven years, and used generalized estimating equation models to test for time trends.
Results
The prevalence of subjects receiving at least one AD prescription was approximately two times higher in women than men consistently across the seven years of the study. The standardized annual prevalence increased from 10.8% in 2005 to 14.4% in 2011 overall, from 7.0% in 2005 to 9.9% in 2011 for men, and from 14.4% in 2005 to 18.6% in 2011 for women. The absolute percent increase was greater in women (4.2% vs. 2.9%; standardized); however, the relative percent increase was greater in men (41.4% vs. 29.2%; standardized). The relative percent increase was greater in the age group 65+ years for both men and women.
Conclusions
AD prescriptions are increasing over time, especially in the elderly. Women receive more AD prescriptions than men. However, the relative increase in AD prescriptions over time is greater in men than women.
Keywords: antidepressants, drug prescriptions, population-based, time trends, pharmacoepidemiology, sex differences
Introduction
During the past two decades, there has been a dramatic increase in the use of antidepressant drugs (AD). (Mojtabai, 2008; Olfson and Marcus, 2009) Many factors may have influenced the increase in AD use, including increased recognition and more aggressive treatment of depression, approval of new AD drugs, direct-to-consumer advertising, off label use of AD for conditions such as chronic pain or sleep problems, and changing advisories from federal or local regulatory agencies. (Compton et al., 2006) Two recent surveys of self-reported use indicated that the yearly rate of AD use increased from 5.8% in 1996 to 10.1% in 2005, and the monthly rate of AD use increased from 1.8% in 1988–1994 to 8.9% in 2005–2008. (National Center for Health Statistics, 2012; Olfson and Marcus, 2009)
Although over the last decade there have been major changes in development, admission to the market, and withdrawal from the market of AD medications, there is little published literature on recent trends in AD prescriptions in the US. (Harman et al., 2009) In addition, although the overall use of AD has generally increased over time, there is mounting concern that this overall trend fails to capture under-use by traditionally disadvantaged populations. (Harman et al., 2009) Therefore, the purpose of this study was to describe age- and sex-specific time trends in AD prescriptions for all indications (not just depression) in a defined US population between 2005 and 2011.
Materials & Methods
Setting and population
We used the resources of the Rochester Epidemiology Project (REP) medical records-linkage system to identify all Olmsted County, MN residents who received at least one AD prescription between 2005 and 2011. Details about the REP have been described previously. (Rocca et al., 2012; St Sauver et al., 2011; St Sauver et al., 2012a; St Sauver et al., 2012b) In brief, the REP is a research infrastructure that links medical record information from the local health care providers in Olmsted County, MN. Due to the relative isolation of the county from major metropolitan areas, and to the presence of a major referral medical center (Mayo Clinic), almost all residents seek health care from a limited number of health care providers. The REP captures information on residents as they visit their health care providers for routine medical care. This medical records-linkage system is unique in its capture of virtually all health care information delivered to an entire population, regardless of age, sex, or insurance status. (Rocca et al., 2012; St Sauver et al., 2011; St Sauver et al., 2012a; St Sauver et al., 2012b)
Measures
Outpatient prescription records from health care providers in Olmsted County were electronically available from 2005 to 2011 (seven years). Prescriptions were coded using the RxNorm classification system, and were further grouped into categories using the National Drug File – Reference Terminology (NDF-RT) classification. (Pathak et al., 2011; Zhong et al., 2013) We considered all AD prescriptions, including transdermal patches. We grouped AD medications into five categories: 1) tricyclic antidepressants: amitriptyline, clomipramine, desipramine, doxepin, amoxapine, imipramine, maprotiline (tetracyclic), nortriptyline, protriptyline, and trimipramine; 2) monoamine oxidase inhibitors: phenelzine, selegiline, and tranylcypromine; 3) selective serotonin reuptake inhibitors: citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline, and vilazodone; 4) serotonin–norepinephrine reuptake inhibitors: desvenlafaxine, duloxetine, milnacipran, and venlafaxine; and 5) others: bupropion, mirtazapine, nefazodone, and trazodone.
Statistical analyses
The age-and sex-specific prevalence of subjects receiving at least one AD prescription in each calendar year was calculated by dividing the number of people who received an AD prescription by the total corresponding age- and sex-specific population for that year. (Zhong et al., 2013) Age-standardized, or age- and sex-standardized, annual prevalence figures were obtained by direct standardization to the US total population. (2000 US Census; using the seven age groups listed in Table 1). These standardized prevalence figures were intended for internal comparison across calendar years, not as national projections.
Table 1.
Age and sex-specific annual prevalence (per 100 population) of prescriptions for antidepressant drugs in Olmsted County, MN from 2005 to 2011
| Age and sex stratum | Annual prevalence (per 100 population)*
|
Change from 2005 to 2011 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2005
|
2006
|
2007
|
2008
|
2009
|
2010
|
2011
|
|||||||||||
| No | Prev. | No | Prev. | No | Prev. | No | Prev. | No | Prev. | No | Prev. | No | Prev. | Prev.† | %╪ | P value§ | |
| Men (or boys) | |||||||||||||||||
| 0–4 | 0 | --- | 0 | --- | 0 | --- | 2 | --- | 1 | --- | 3 | --- | 4 | --- | --- | --- | |
| 5–12 | 90 | 1.2 | 78 | 1.0 | 84 | 1.1 | 101 | 1.3 | 108 | 1.3 | 106 | 1.3 | 100 | 1.2 | 0 | 0 | |
| 13–18 | 269 | 4.3 | 255 | 4.1 | 235 | 3.8 | 274 | 4.6 | 293 | 5.1 | 293 | 5.2 | 302 | 5.5 | 1.2 | 27.9 | |
| 19–29 | 576 | 5.2 | 688 | 6.1 | 701 | 6.3 | 745 | 6.6 | 847 | 7.6 | 852 | 7.6 | 885 | 7.9 | 2.7 | 51.9 | |
| 30–49 | 1,773 | 9.0 | 1,893 | 9.6 | 1,844 | 9.4 | 1,916 | 10.0 | 2,122 | 11.2 | 2,299 | 12.2 | 2,292 | 12.3 | 3.3 | 36.7 | |
| 50–64 | 1,158 | 11.3 | 1,251 | 11.6 | 1,255 | 11.1 | 1,379 | 11.9 | 1,700 | 14.2 | 1,864 | 15.0 | 1,977 | 15.4 | 4.1 | 36.2 | |
| 65 + | 685 | 10.4 | 739 | 10.8 | 781 | 11.0 | 935 | 12.7 | 1,100 | 14.5 | 1,294 | 16.4 | 1,363 | 16.7 | 6.3 | 60.6 | |
| Total, crude | 4,551 | 6.8 | 4,904 | 7.2 | 4,900 | 7.1 | 5,352 | 7.7 | 6,171 | 8.9 | 6,711 | 9.5 | 6,923 | 9.8 | 3.0 | 44.1 | |
| Total, standardized || | --- | 7.0 | --- | 7.4 | --- | 7.3 | --- | 7.9 | --- | 9.1 | --- | 9.7 | --- | 9.9 | 2.9 | 41.4 | 0.03 |
| Women (or girls) | |||||||||||||||||
| 0–4 | 2 | --- | 2 | --- | 2 | --- | 1 | --- | 0 | --- | 2 | --- | 1 | --- | --- | --- | |
| 5–12 | 69 | 0.9 | 60 | 0.8 | 74 | 1.0 | 89 | 1.2 | 69 | 0.9 | 69 | 0.9 | 67 | 0.8 | −0.1 | −11.1 | |
| 13–18 | 448 | 7.4 | 440 | 7.4 | 445 | 7.6 | 471 | 8.2 | 494 | 8.8 | 496 | 9.0 | 523 | 9.6 | 2.2 | 29.7 | |
| 19–29 | 1,703 | 12.9 | 1,841 | 13.6 | 1,835 | 13.3 | 1,987 | 14.1 | 2,125 | 15.4 | 2,163 | 15.2 | 2,178 | 15.1 | 2.2 | 17.1 | |
| 30–49 | 4,121 | 19.6 | 4,279 | 20.2 | 4,319 | 20.6 | 4,465 | 21.7 | 4,694 | 23.0 | 4,933 | 24.4 | 4,889 | 24.4 | 4.8 | 24.5 | |
| 50–64 | 2,741 | 24.1 | 2,897 | 24.2 | 2,990 | 23.8 | 3,287 | 25.3 | 3,783 | 28.1 | 4,152 | 29.6 | 4,337 | 29.8 | 5.7 | 23.7 | |
| 65 + | 1,587 | 17.7 | 1,727 | 18.8 | 1,793 | 19.0 | 1,998 | 20.7 | 2,423 | 24.6 | 2,748 | 27.2 | 2,911 | 28.2 | 10.5 | 59.3 | |
| Total, crude | 10,671 | 14.5 | 11,246 | 15.0 | 11,458 | 15.1 | 12,298 | 16.1 | 13,588 | 17.7 | 14,563 | 18.7 | 14,906 | 19.0 | 4.5 | 31.0 | |
| Total, standardized || | --- | 14.4 | --- | 14.9 | --- | 14.9 | --- | 15.9 | --- | 17.4 | --- | 18.4 | --- | 18.6 | 4.2 | 29.2 | 0.01 |
| Both sexes | |||||||||||||||||
| 0–4 | 2 | --- | 2 | --- | 2 | --- | 3 | --- | 1 | --- | 5 | --- | 5 | --- | --- | --- | |
| 5–12 | 159 | 1.1 | 138 | 0.9 | 158 | 1.0 | 190 | 1.2 | 177 | 1.1 | 175 | 1.1 | 167 | 1.0 | −0.1 | −9.1 | |
| 13–18 | 717 | 5.8 | 695 | 5.7 | 680 | 5.7 | 745 | 6.4 | 787 | 6.9 | 789 | 7.0 | 825 | 7.5 | 1.7 | 29.3 | |
| 19–29 | 2,279 | 9.4 | 2,529 | 10.2 | 2,536 | 10.1 | 2,732 | 10.8 | 2,972 | 11.9 | 3,015 | 11.8 | 3,063 | 11.9 | 2.5 | 26.6 | |
| 30–49 | 5,894 | 14.5 | 6,172 | 15.1 | 6,163 | 15.2 | 6,381 | 16.1 | 6,816 | 17.4 | 7,232 | 18.5 | 7,181 | 18.6 | 4.1 | 28.3 | |
| 50–64 | 3,899 | 18.0 | 4,148 | 18.2 | 4,245 | 17.8 | 4,666 | 19.0 | 5,483 | 21.5 | 6,016 | 22.7 | 6,314 | 23.0 | 5.0 | 27.8 | |
| 65 + | 2,272 | 14.6 | 2,466 | 15.4 | 2,574 | 15.6 | 2,933 | 17.2 | 3,523 | 20.2 | 4,042 | 22.5 | 4,274 | 23.1 | 8.5 | 58.2 | |
| Total, crude | 15,222 | 10.8 | 16,150 | 11.3 | 16,358 | 11.3 | 17,650 | 12.1 | 19,759 | 13.5 | 21,274 | 14.4 | 21,829 | 14.6 | 3.8 | 35.2 | |
| Total, standardized || | --- | 10.8 | --- | 11.2 | --- | 11.2 | --- | 12.0 | --- | 13.4 | --- | 14.2 | --- | 14.4 | 3.6 | 33.3 | 0.01¶ |
Number indicates the actual number of subjects who received at least one prescription for an antidepressant medication during the one-year period. For the age group 0–4 years, we did not compute the prevalence because the numbers of subjects with AD prescriptions were small (≤ 5).
Absolute change = prevalence (per 100) in 2011 minus prevalence in 2005.
Relative change = absolute change divided by the prevalence in 2005 and expressed as a percent.
P value for linear trend of increasing prevalence of prescriptions by calendar year. All models also included a quadratic term for calendar year (the quadratic term was only significant in the model with both sexes, p=0.03).
The total prevalence in men and women separately was standardized by age, and the total prevalence for both sexes combined was standardized by age and sex using the 2000 US Census population (direct standardization using the seven age groups listed in this table). These standardizations allow comparison of the total prevalence across calendar years by removing age and sex trends. However, they should not be used as national projections.
The interaction of sex by calendar year was significant indicating a higher relative increase in men compared with women (p=0.0003).
We used generalized estimating equation (GEE) models with a negative binomial distribution to test for temporal trends in antidepressant prescriptions overall and by selected categories. (Frome and Checkoway, 1985; Gardner et al., 1995; McCullagh and Nelder, 1983) Specific counts for each calendar year, age (using the seven age groups listed in Table 1), and sex were used as the unit of observation. Percent change for the entire study period was also estimated using the GEE models. Comparisons of temporal trends across specific groups (e.g., men vs. women) were performed by including a two-way interaction term (in models including also the main effects). Because the graphical assessment suggested that the rate of change differed between the 2005–2007 and the 2008–2011 time periods, a quadratic term for calendar year was included in all models.
To address the problem of subjects receiving only one prescription that was never refilled, we conducted a set of sensitivity analyses restricted to subjects who received two or more prescriptions. To provide a window of five years in which we could capture the refills, we focused on the three central years of the study period (2007, 2008, and 2009). A person receiving one AD prescription in a given year (index year) could receive one or more additional AD prescriptions in the same year, in the two years preceding the index year, or in the two years following the index year (total of 5 years). SAS version 9.2 was used for all analyses (SAS Institute Inc., Cary, NC).
Results
Prevalence by age and sex
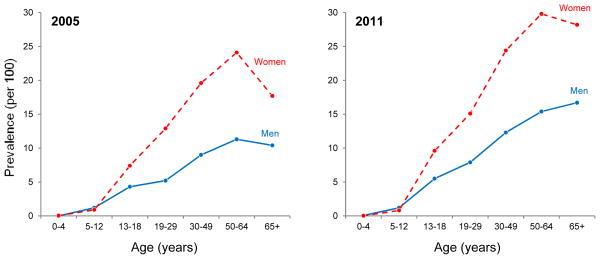
Table 1 shows the age-specific prevalence of AD prescriptions for each of the seven years of the study for men and women separately and combined. The age- and sex-specific prevalence at the beginning of the study (2005; left panel) and at the end of the study (2011; right panel) are also shown graphically in Figure 1. For all study years and for all ages after age 12 years, the prevalence was higher for women than for men. In each calendar year, the age-specific prevalence of prescriptions in women increased from age 5–12 to age 50–64 years and declined slightly or remained stable in the 65+ year group (Figure 1). Similarly, the age-specific prevalence in men increased from age 5–12 to age 50–64 years and declined slightly or remained stable in the 65+ year group in 2005 through 2007 (Figure 1; left panel); however, the age-specific prevalence in men continued to increase in the age group 65+ years in 2008 through 2011 (Figure 1; right panel). In sensitivity analyses restricted to subjects who had two or more AD prescriptions within a 5-year time window, the overall prevalence of subjects with AD prescriptions reduced from 11.3% to 10.6% in 2007, from 12.1% to 11.4% in 2008, and from 13.5% to 12.7% in 2009 (crude prevalence; data not shown in Table 1).
Fig. 1.
Age- and sex-specific prevalence of AD prescriptions for any indication in 2005 (left panel) and 2011 (right panel).
Time trends by age and sex
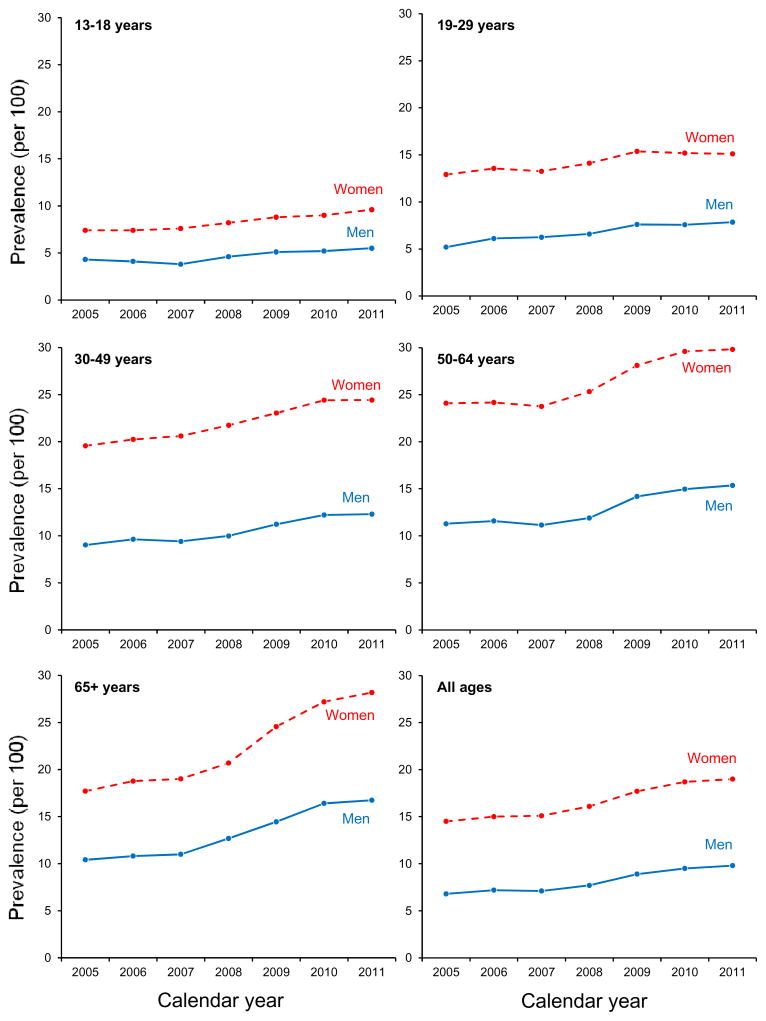
Figure 2 shows the time trends of AD prescriptions for any indication between 2005 and 2011 for men and women in five age groups and overall (lower right panel). Consistently across the seven years of the study, the annual prevalence of AD prescriptions was approximately two times higher in women compared to men (Table 1 and Figure 2). The age- and sex-adjusted prevalence of subjects receiving at least one AD prescription increased from 10.8% in 2005 to 14.4% in 2011 overall, from 14.4% to 18.6% in women, and from 7.0% to 9.9% in men (Table 1). The test for linear trend over calendar year was significant for both men (p = 0.03) and women (p = 0.01; all models included a quadratic term for calendar year). Although the absolute change in standardized prevalence over the seven years of the study was greater for women (4.2%) than for men (2.9%), the relative increase (in percent of the 2005 prevalence) was greater for men (41.4%) than for women (29.2%; sex by calendar year interaction, p = 0.0003). The relative percent increase per year estimated by the regression model was 5.7% overall, and was greater in 2008–2011 (6.1%) than in 2005–2007 (1.7%).
Fig. 2.
Prevalence (per 100 population) of AD prescriptions for any indication by sex and by calendar year between 2005 and 2011 in five age groups and in all ages combined (lower right panel). The time trends for children age 0–4 and 5–12 years were not shown because the numbers were small.
The rapid increase in AD prescriptions between 2008 and 2011 was attributable primarily to an increased number of prescriptions to Olmsted County men and women in the age groups 50–64 years and 65+ years (Table 1 and Figure 2). In particular, the largest increase in AD prescriptions from 2005 through 2011 was observed in the age group 65+ years, from 14.6% in 2005 to 23.1% in 2011 for both sexes combined (Table 1 and Figure 2).
Time trends by type of drug
We also examined trends in AD prescriptions by type of AD. The most frequently prescribed antidepressants were selective serotonine reuptake inhibitors (citalopram, sertraline, fluoxetine, paroxetine, and escitalopram) and their prevalence of prescriptions increased from 7.0% in 2005 to 9.5% in 2011. During the same time frame, the prevalence increased from 3.5% to 4.8% for “other AD” and from 1.2% to 1.8% for serotonin–norepinephrine reuptake inhibitors. The increase in prevalence of tricyclic antidepressants and monoamine oxidase inhibitors prescriptions was negligible (0.2%).
Discussion
Our population-based study showed that the prevalence of AD prescriptions for all indications (not just depression) was about two times higher in women than in men throughout the entire study period. This finding confirms a number of recent studies that showed a higher use of AD in women compared to men. (Athanasopoulos et al., 2013; Atlantis et al., 2012; Kuo et al., 2011; Lockhart and Guthrie, 2011; Meng et al., 2013; Mojtabai and Olfson, 2014; Parabiaghi et al., 2011; Sundell et al., 2011; Wu et al., 2012) We also observed that the prevalence of AD prescriptions reached a peak at age 50–64 years in women but not in men. This age group corresponds approximately with the early-postmenopausal years (the median age at menopause in the United States is 51 years). (Shuster et al., 2010) This pattern may suggest a causal link between the endocrinological changes of menopause and the exacerbation of existing depressive symptoms or the appearance de novo depressive symptoms. (Rocca et al., 2008; Shuster et al., 2010)
AD prescriptions increased steadily from 2005 to 2011, similar to trends observed in previous studies from earlier time frames. (Mojtabai, 2008; Olfson and Marcus, 2009) Although women experienced a greater absolute increase in prescriptions between 2005 and 2011, the relative increase over time was significantly greater in men compared with women. Interestingly, the increase in AD prescriptions was mostly driven by prescriptions to older adults, particularly after 2007. Nearly 1 in 4 Olmsted County residents aged 65+ years received at least one AD prescription in 2011. The relative increase in AD prescriptions in residents aged 65+ was similar in men and women.
In our study population, the most commonly prescribed ADs were selective serotonin reuptake inhibitors, and the increase in AD prescriptions was mostly confined to this drug group. Citalopram, which may be used to treat multiple disorders, had both the highest prevalence and the greatest increase in prevalence over time. These data are in agreement with a previous national survey that showed that about 67% of all AD prescriptions in 2005 were for selective serotonin reuptake inhibitors. (Olfson and Marcus, 2009)
Our study revealed a greater relative increase in prescriptions in men compared to women. This trend may suggest that the care seeking behavior in men has improved over time reducing the under-diagnosis and the under-treatment of anxiety and depressive disorders in men. We also observed a significant increase in prescriptions of ADs to the elderly population. Depression in older adults has been historically underdiagnosed and undertreated; (Lavretsky and Kumar, 2002) however, our data suggest that these practices may be changing. The reasons for the rapid increase in AD prescriptions among persons 65 years of age and older from 2008–2011 are not clear. One possible explanation is that many selective serotonin reuptake inhibitors became available generically just prior to this time frame (e.g., paroxetine in 2003, citalopram in 2004, and sertraline in 2006). The lower cost, combined with new information about the safety and efficacy of selective serotonin reuptake inhibitors in the elderly, may have also contributed in part to this increase. (Mottram et al., 2006)
A second possible explanation is the US Food and Drug Administration (FDA) advisory released in May 2007 (Friedman and Leon, 2007) reporting an increased risk of suicidal thoughts and behaviors among young adults aged 18–24 years taking antidepressants, but not among adults older than 24 years. The FDA advisory also emphasized the increased risk of suicide among adults 65 or older who were not treated for depression. This important FDA statement may have encouraged physicians to prescribe AD to the elderly. (Lineberry et al., 2007) However, further studies are needed to validate this hypothesis.
A third possible explanation for the increased AD prescriptions in this community may have been the release of new national recommendations for depression screening in adults in December, 2009. (Whitlock, 2010) Olmsted County medical care providers began routine depression screening programs at this time. In addition, the Depression Improvement Across Minnesota, Offering a New Direction (DIAMOND) program was launched in 2008 (https://www.icsi.org/health_initiatives/mental_health/diamond_for_depression/) to increase the treatment of adults with known and previously diagnosed depression.
A first important limitation of our study is the geographic specificity of the sample. Our study was based on a single Midwestern county, and our findings may not apply to other communities in the US with different demographic and socioeconomic characteristics and different access to health care. On the other hand, we have previously reported that the population of Olmsted County is comparable to the population of Minnesota, of the Upper Midwest, and of a large segment of the entire US population. (St Sauver et al., 2012a) The age-standardized and age- and sex-standardized prevalence figures reported in Table 1 are only intended for internal comparison across the seven calendar years. Extrapolations and generalizations from this study, or from any other study in a single selected population, to the entire US population must be judged considering specific demographic, socioeconomic, or medical practice differences. Our findings from a geographically-defined population are most useful when they are compared with findings from other populations in the United States or worldwide to investigate geographic similarities or differences in patterns of AD prescriptions. Geographic similarities or differences can be used to guide our decisions in clinical practice or in public health. (St Sauver et al., 2012a)
A second limitation of our study is that we included all AD prescriptions irrespective of the indications for the prescription or of the duration of treatment. ADs are often prescribed for conditions other than depression, including anxiety, sleep problems, smoking cessation, and pain. It was not possible to assess and validate the indications for the thousands of patients included in this study. Further studies are ongoing in an effort to validate indications and duration of use in samples of the total resident population included in this paper. Third, we may have underestimated the prevalence of AD prescriptions because we did not include data from a few local psychiatrists and AD prescriptions given during hospitalizations. However, this underestimation should be minimal.
Fourth, our study examined the frequency of prescriptions, which is a useful measure of the prescribing behavior of physicians. However, it was not possible to determine whether the prescriptions were filled and taken by patients. (Zhong et al., 2013) In a set of sensitivity analyses restricted to subjects who had two or more AD prescriptions within a 5-year time window, the reduction in overall prevalence (compared with the prevalence including also subjects who had only one prescription) was small. These findings suggest that it was uncommon for subjects to receive a single isolated AD prescription without subsequent refills, and that our prevalence of AD prescriptions may be a reasonable surrogate for the prevalence of use.
Strengths of this study include the ability to capture health information on a complete Midwestern population using the REP medical records-linkage system. (Rocca et al., 2012; St Sauver et al., 2011; St Sauver et al., 2012a; St Sauver et al., 2012b; Zhong et al., 2013) Due to the relative geographical isolation of Olmsted County from major metropolitan areas, virtually all of the county residents receive health care from a few local health care providers; therefore, our findings can be considered population-based. (Rocca et al., 2012; St Sauver et al., 2011; St Sauver et al., 2012a; St Sauver et al., 2012b) In addition, this population has adequate access to a full spectrum of psychiatric care including child and adolescent services.
Conclusion
We found that the annual prevalence of AD prescriptions was higher in women than men at all ages after age 12 years, and it increased steadily between 2005 and 2011. The relative increase in prescriptions over seven years was mainly driven by increased prescriptions to the elderly, especially after 2007, and was greater in men compared with women. These trends should be monitored in the future, and patterns of under-utilization or over-utilization by sex, age, socioeconomic status, insurance status, and other determinants should be investigated.
Acknowledgments
Financial support: The Rochester Epidemiology Project is currently supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG034676. The findings and conclusions of this report are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. Additionally, this publication was supported by the Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery at Mayo Clinic.
Footnotes
Disclosures
The authors have no conflicts of interest to disclose.
Contributor Information
Wenjun Zhong, Email: zhongw@email.chop.edu, General Pediatrics, The Children’s Hospital of Philadelphia, Philadelphia, PA, USA.
Hilal Maradit Kremers, Email: maradit@mayo.edu, Division of Epidemiology, Department of Health Sciences Research, Mayo Clinic, Rochester, MN, USA.
Barbara P. Yawn, Email: byawn@olmmed.org, Department of Research, Olmsted Medical Center
William V. Bobo, Email: bobo.william@mayo.edu, Department of Psychiatry and Psychology, Mayo Clinic, Rochester, MN, USA
Jennifer L. St Sauver, Email: stsauver.jennifer@mayo.edu, Division of Epidemiology, Department of Health Sciences Research, Mayo Clinic, Rochester, MN, USA
Jon O. Ebbert, Email: ebbert.jon@mayo.edu, Division of Primary Care Internal Medicine, Mayo Clinic, Rochester, MN, USA
Lila J. Rutten, Email: rutten.lila@mayo.edu, Division of Epidemiology, Department of Health Sciences Research, Mayo Clinic, Rochester, MN, USA
Debra J. Jacobson, Email: djacobsn@mayo.edu, Division of Biomedical Statistics and Informatics, Department of Health Sciences Research, Mayo Clinic, Rochester, MN, USA
Scott M. Brue, Email: brue.scott@mayo.edu, Division of Biomedical Informatics Support System, Department of Data Management Systems, Mayo Clinic, Rochester, MN, USA
Walter A. Rocca, Email: rocca@mayo.edu, Division of Epidemiology, Department of Health Sciences Research, Mayo Clinic, Rochester, MN, USA
References
- Athanasopoulos C, Pitychoutis PM, Messari I, Lionis C, Papadopoulou-Daifoti Z. Is drug utilization in Greece sex dependent? A population-based study. Basic Clin Pharmacol Toxicol. 2013;112:55–62. doi: 10.1111/j.1742-7843.2012.00920.x. [DOI] [PubMed] [Google Scholar]
- Atlantis E, Sullivan T, Sartorius N, Almeida OP. Changes in the prevalence of psychological distress and use of antidepressants or anti-anxiety medications associated with comorbid chronic diseases in the adult Australian population, 2001–2008. Aust N Z J Psychiatry. 2012;46:445–456. doi: 10.1177/0004867411433218. [DOI] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991–1992 and 2001–2002. AM J Psychiatry. 2006;163:2141–2147. doi: 10.1176/ajp.2006.163.12.2141. [DOI] [PubMed] [Google Scholar]
- Friedman RA, Leon AC. Expanding the black box - depression, antidepressants, and the risk of suicide. N Eng J Med. 2007;356:2343–2346. doi: 10.1056/NEJMp078015. [DOI] [PubMed] [Google Scholar]
- Frome EL, Checkoway H. Epidemiologic programs for computers and calculators. Use of Poisson regression models in estimating incidence rates and ratios. Am J Epidemiol. 1985;121:309–323. doi: 10.1093/oxfordjournals.aje.a114001. [DOI] [PubMed] [Google Scholar]
- Gardner W, Mulvey EP, Shaw EC. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychological Bulletin. 1995;118:392–404. doi: 10.1037/0033-2909.118.3.392. [DOI] [PubMed] [Google Scholar]
- Harman JS, Edlund MJ, Fortney JC. Trends in antidepressant utilization from 2001 to 2004. Psychiatr Serv. 2009;60:611–616. doi: 10.1176/ps.2009.60.5.611. [DOI] [PubMed] [Google Scholar]
- Kuo CC, Chien IC, Lin CH, Lee WG, Chou YJ, Lee CH, Chou P. Prevalence, correlates, and disease patterns of antidepressant use in Taiwan. Compr Psychiatry. 2011;52:662–669. doi: 10.1016/j.comppsych.2011.01.002. [DOI] [PubMed] [Google Scholar]
- Lavretsky H, Kumar A. Clinically significant non-major depression: old concepts, new insights. Am J Geriatric Psychiatry. 2002;10:239–255. [PubMed] [Google Scholar]
- Lineberry TW, Bostwick JM, Beebe TJ, Decker PA. Impact of the FDA black box warning on physician antidepressant prescribing and practice patterns: opening Pandora’s suicide box. Mayo Clin Proc. 2007;82:518–520. doi: 10.4065/82.4.518. [DOI] [PubMed] [Google Scholar]
- Lockhart P, Guthrie B. Trends in primary care antidepressant prescribing 1995–2007: a longitudinal population database analysis. Br J General Prac. 2011;61:e565–72. doi: 10.3399/bjgp11X593848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullagh P, Nelder J. Generalized Linear Models. Chapman and Hall; London: 1983. [Google Scholar]
- Meng X, D’Arcy C, Tempier R. Trends in psychotropic use in Saskatchewan from 1983 to 2007. Can J Psychiatry. 2013;58:426–431. doi: 10.1177/070674371305800708. [DOI] [PubMed] [Google Scholar]
- Mojtabai R. Increase in antidepressant medication in the US adult population between 1990 and 2003. Psychother Psychoso. 2008;77:83–92. doi: 10.1159/000112885. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M. National trends in long-term use of antidepressant medications; results from the US National Health and Nutrition Examination Survey. J Clin Psychiatry. 2014;75:169–177. doi: 10.4088/JCP.13m08443. [DOI] [PubMed] [Google Scholar]
- Mottram P, Wilson K, Strobl J. Antidepressants for depressed elderly. Cochrane database of systematic reviews. 2006;(1):CD003491. doi: 10.1002/14651858.CD003491.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD: Library of Congress; 2012. (Statistics NCfH publication no. 76–641496) [PubMed] [Google Scholar]
- Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66:848–856. doi: 10.1001/archgenpsychiatry.2009.81. [DOI] [PubMed] [Google Scholar]
- Parabiaghi A, Franchi C, Tettamanti M, Barbato A, D’Avanzo B, Fortino I, Bortolotti A, Merlino L, Nobili A. Antidepressants utilization among elderly in Lombardy from 2000 to 2007: dispensing trends and appropriateness. Eur J Clin Pharmacol. 2011;67:1077–1083. doi: 10.1007/s00228-011-1054-z. [DOI] [PubMed] [Google Scholar]
- Pathak J, Murphy SP, Willaert BN, Kremers HM, Yawn BP, Rocca WA, Chute CG. Using RxNorm and NDF-RT to classify medication data extracted from electronic health records: experiences from the Rochester Epidemiology Project. AMIA Annu Symp Proc. 2011:1089–1098. [PMC free article] [PubMed] [Google Scholar]
- Rocca WA, Grossardt BR, Geda YE, Gostout BS, Bower JH, Maraganore DM, de Andrade M, Melton LJ., 3rd Long-term risk of depressive and anxiety symptoms after early bilateral oophorectomy. Menopause. 2008;15:1050–1059. doi: 10.1097/gme.0b013e318174f155. [DOI] [PubMed] [Google Scholar]
- Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ., 3rd History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87:1202–1213. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuster LT, Rhodes DJ, Gostout BS, Grossardt BR, Rocca WA. Premature menopause or early menopause: long-term health consequences. Maturitas. 2010;65:161–166. doi: 10.1016/j.maturitas.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, 3rd, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester Epidemiology Project. Am J Epidemiol. 2011;173:1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012a;87:151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, 3rd, Pankratz JJ, Brue SM, Rocca WA. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012b;41:1614–1624. doi: 10.1093/ije/dys195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundell KA, Gissler M, Petzold M, Waern M. Antidepressant utilization patterns and mortality in Swedish men and women aged 20–34 years. Eu J Clin Pharmacol. 2011;67:169–178. doi: 10.1007/s00228-010-0933-z. [DOI] [PubMed] [Google Scholar]
- Whitlock EP, O’Connor EA, Gaynes BN. Efficacy of Antidepressants and USPSTF Guidelines for Depression Screening. Ann Int Med. 2010;152:753–754. doi: 10.7326/0003-4819-152-11-201006010-00016. [DOI] [PubMed] [Google Scholar]
- Wu CS, Shau WY, Chan HY, Lee YC, Lai YJ, Lai MS. Utilization of antidepressants in Taiwan: a nationwide population-based survey from 2000 to 2009. Pharmacoepidemiol Drug Saf. 2012;21:980–988. doi: 10.1002/pds.3255. [DOI] [PubMed] [Google Scholar]
- Zhong W, Maradi-Kremers H, St Sauver JL, Yawn BP, Ebbert JO, Roger VL, Jacobson DJ, McGree ME, Brue SM, Rocca WA. Age and sex patterns of drug prescribing in a defined american population. Mayo Clin Proc. 2013;88:697–707. doi: 10.1016/j.mayocp.2013.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]