Abstract
AIM: To evaluate the outcome of over-the-scope-clip system (OTSC) for endoscopic treatment of various indications in daily clinical practice in Switzerland.
METHODS: This prospective, consecutive case series was conducted at a tertiary care hospital from September 2010 to January 2014. Indications for OTSC application were fistulae, anastomotic leakage, perforation, unroofed submucosal lesion for biopsy, refractory bleeding, and stent fixation in the gastrointestinal (GI) tract. Primary technical success was defined as the adequate deployment of the OTSC on the target lesion. Clinical success was defined as resolution of the problem; for instance, no requirement for surgery or further endoscopic intervention. In cases of recurrence, retreatment of a lesion with a second intervention was possible. Complications were classified into those related to sedation, endoscopy, or deployment of the clip.
RESULTS: A total of 28 OTSC system applications were carried out in 21 patients [median age 64 years (range 42-85), 33% females]. The main indications were fistulae (52%), mostly after percutaneous endoscopic gastrostomy tube removal, and anastomotic leakage after GI surgery (29%). Further indications were unroofed submucosal lesions after biopsy, upper gastrointestinal bleeding, or esophageal stent fixation. The OTSC treatments were applied either in the upper (48%) or lower (52%) GI tract. The mean lesion size was 8 mm (range: 2-20 mm). Primary technical success and clinical success rates were 85% and 67%, respectively. In 53% of cases, the suction method was used without accessories (e.g., twin grasper or tissue anchor). No endoscopy-related or OTSC-related complications were observed.
CONCLUSION: OTSC is a useful tool for endoscopic closure of various GI lesions, including fistulae and leakages. Future randomized prospective multicenter trials are warranted.
Keywords: Over-the-scope-clip system, OTSC, Bear claw, Endoscopic closure, Gastrointestinal lesion, Perforations, Fistulae, Leakage
Core tip: In this prospective case series, we report the outcome of the over-the-scope-clip system (OTSC) in endoscopic treatment of various indications, including closing fistulae and repairing anastomotic leakages in daily clinical practice in Switzerland. The OTSCs (n = 28) were applied in 21 patients. Primary technical and clinical success rates were 85% and 67%, respectively. No complications were observed related to endoscopy or OTSC. OTSC is a useful tool for endoscopic closure of various gastrointestinal lesions.
INTRODUCTION
The over-the-scope-clip (OTSC) system (Ovesco Endoscopy AG, Tübingen, Germany) is a new endoscopic device, suitable for closing gastrointestinal (GI) fistulae or anastomotic leakages. It can also be used as a hemostatic tool for controlling GI bleeding and for esophageal stent fixation. To the best of our knowledge, only case reports or small case series have described the efficacy and safety of the OTSC; to date, no human clinical randomized controlled trials are available. The available case series and reports are inhomogeneous, in terms of the indication, study design, site of application, and definition of success.
We present a prospective case series that reflects our daily clinical experience with OTSC in a tertiary endoscopy center in Switzerland. This case series describes primary successful closure in over 80% of GI lesions, mainly fistulae or anastomotic leakages. This data contributes to the knowledge of OTSC experiences.
MATERIALS AND METHODS
Methods
This observational, single-arm, prospective and consecutive case series was conducted at a hospital with tertiary care endoscopy from September 2010 to January 2014. Simple descriptive statistics were used and no hypothesis testing was performed. Data are expressed in absolute numbers (f.e. 6/21) and in percentages (f.e. 29%) in relation to all patients or the concerning group. Data on sex, age, indication, details of the procedure, and outcome were collected prospectively. Approval for using pseudonymized patient data was obtained from the local Ethics committee. The indications for OTSC applications included fistulae, anastomotic leakages, perforations, unroofed submucosal lesions after biopsy, refractory bleeding, and stent fixation. Exclusion criteria included pregnancy, patients < 18 years of age, or failure to provide informed consent. Primary technical success was defined as the adequate deployment of the OTSC on the target lesion. Clinical success was defined as resolution of the problem; for instance, no requirement for surgery or further endoscopic intervention. In cases of recurrence, retreatment of a lesion with a second intervention was possible. Complications were classified into those related to sedation, endoscopy, or deployment of the clip.
Seven experienced endoscopists performed OTSC applications. They were trained by the most experienced endoscopist. The OTSC was applied at the discretion of the endoscopist.
We used GIF-1TQ, GIF-H, CF-HQ, and PCF-H endoscopes (Olympus, Tokyo, Japan). The OTSC deployment was arranged according to the manufacturer's instructions. All interventions were performed under non-anaesthesiologist-administered propofol. After the endoscopic evaluation of the gastrointestinal lesion, the endoscope was withdrawn, re-inserted with the mounted and loaded OTSC device, and positioned towards the lesion (Figure 1). Afterwards, the tissue around the lesion was invaginated into the applicator cap by use of suction, OTSC Twin Grasper or OTSC Anchor (both Ovesco Endoscopy AG, Tübingen, Germany), at the discretion of the operator. The operator chose on the basis of lesion size and type of tissue the size and type of OTSC. When the tissue was trapped adequately, the OTSC could be released and the technical success was evaluated visually. Additionally, the procedure was documented with fluoroscopy.
Figure 1.
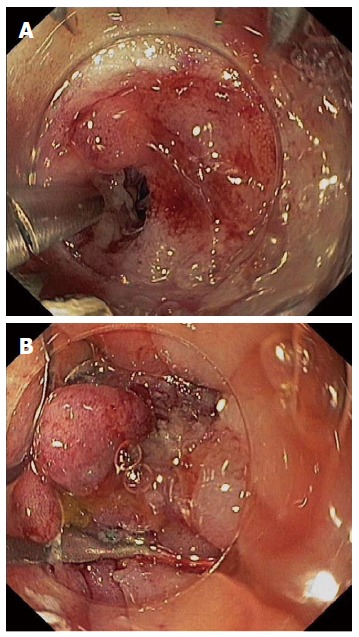
Case number 21 with fistula. A: Fistula between descending colon and rectum after surgery. Cap and loaded over-the-scope-clip (OTSC) visible; B: Fistula closed with OTSC.
RESULTS
Individual patient data are presented in detail in Table 1. A total of 28 OTSC applications were carried out in 21 patients. The main indications (Figure 2) were fistulae [11/21 (52%)] (Figure 1) and anastomotic leakage after GI surgery [6/21 (29%)]. In two cases [2/21 (10%)], OTSC was successfully used to close an unroofed submucosal gastric tumor after biopsy (e.g., Figure 3). Ten [10/21 (47%)] lesions were in the upper GI tract (Table 2). Only 4/21 (19%) patients had prior endoscopic therapy. The mean lesion size was 8 mm (range 2-20 mm; Table 2). In 2/21 (9.5%) patients, the lesion site was not accessible endoscopically due to stenosis. In one of those 2 cases, the OTSC application was possible after the colonoscope was replaced with a gastroscope.
Table 1.
Demographic data, indications, lesion sizes, interventions and successes/outcomes of 21 patients treated with over-the-scope-clip
| No. | Sex | Age (yr) | Indication | Lesion size (mm) | OTSC type | Twin grasper (T) Anchor (A) | Technical success | Clinical success | 2nd OTSC | Clinical success after 2nd OTSC |
| 1 | M | 59 | Right-sided colocutaneous fistula with abscess | 5 | 14/6 | - | Y | Y | N | |
| 2 | M | 42 | Fibrotic cardiac fistula with recurrent infections after gastric sleeve surgery, 21 mo prior | 2 | 12/3a 12/6a | T | N | N | 12/6a | Y |
| 3 | M | 70 | 2 anastomotic leakages 3 wk after low anterior resection of adenocarcinoma | Each 20 | 3 clips | A | N | Same session | Y | |
| 4 | F | 63 | PEG gastrostomy closed due to secondary peritonitis | 5 | 1 clip | A | Y | Y | N | |
| 5 | M | 71 | Ileorectal anastomotic leakage after colectomy 6 mo prior, due to stenosing chronic diverticulitis | 7 | 14/6 | A | Y | N | N | |
| 6 | F | 62 | Anastomotic leakage after right hemicolectomy | 3 | 12/6a | - | Y | Y | N | |
| 7 | M | 60 | Anastomotic leakage 6 wk after low anterior resection | 5 | 12/6a | A | Y | Y | N | |
| 8 | F | 59 | 2 rectoabdominocutaneous fistulae after small and large bowel resections with rectal stump in Crohn’s disease | Each 2 × 2 | 14/6a | A | Y | N | 14/6a | Y |
| 9 | M | 55 | Gastrocutaneous fistula after PEG tube removal 7 days prior | 20 × 5 | - | - | Not amenable due to esophageal stenosis | |||
| 10 | F | 47 | Gastrocutaneous fistula after gastric sleeve resection | 6 | 2 × 11/6a | A | Y | Y | N | |
| 11 | M | 45 | Infected gastrocutaneous fistula after PEG tube removal | 2 | 11/6a | - | Y | Y | N | |
| 12 | F | 67 | Fistula of the rectum and abscess in the small pelvis after surgery | 8 | 12/6a | T + A | Y | N | 2 × 12/3a | N |
| 13 | M | 84 | Anastomotic leakage after ileosigmoidostomy | 8 | 12/6t | A | Y | Y | N | |
| 14 | M | 51 | Endoscopic unroofing of a submucosal antral tumor for biopsy | 10 | 12/6gc | - | Y | Y | N | |
| 15 | F | 82 | Infected gastrocutaneous fistula after PEG tube removal | 3 | 12/6gc | - | Y | Y | N | |
| 16 | M | 85 | Gastrocolic migration of PEG tube | 4 | 12/6a | - | Y | Y | N | |
| 17 | M | 63 | Anastomotic leakage after colorectal resection | 5 | 12/6t | - | Y | Y | N | |
| 18 | M | 59 | Endoscopic unroofing of a submucosal gastric tumor for biopsy (Figure 3) | 15 | 12/6gc | - | Y | Y | N | |
| 19 | F | 81 | Dieulafoy lesion, Forrest Ia; known achalasia | 8 | 12/6t | - | Y | Y | N | |
| 20 | M | 68 | Fixation of esophageal stent | - | 11/6a | - | Y | Y | N | |
| 21 | M | 71 | Fistula between colon and rectal stump after Hartmann procedure due to rectal cancer | 15 | 12/6a | A | Y | N | Y | N |
No. 12: In the first session, the anal stenosis did not allow passage of the colonoscope with the mounted OTSC system; No. 16: Combined with colonoscopic removal of the PEG tube; No. 20: After endoscopic removal of the dislocated esophageal stent. History of aortoesophageal fistula, mediastinitis, and thoracic endovascular aortic repair 1 mo prior; No. 21: Further failure with 12/6a and 12/6gc. OTSC: Over-the-scope-clip; PEG: Percutaneous endoscopic gastrostomy; M: Male; F: Female.
Figure 2.

Indications for over-the-scope-clip application in 21 patients.
Figure 3.

Case number 18 with submucosal gastric tumor. A: Submucosal gastric tumor, the clip was applied three months ago due to a bleeding after biopsy; B: Incision, unroofing, and biopsy of the yellowish tumor with a radial jaw (later histopathology indicated it was a lipoma); C: Closure of the resected area with over-the-scope-clip.
Table 2.
Demographic data, indications, lesion size and localization of the over-the-scope-clip applications
| Characteristics | Patients (n, unless otherwise indicated) |
| Number of patients (% females) | 21 (33%) |
| Age, median (range), yr | 64 (42-85) |
| Indications Fistulae (OTSC application) Colon After PEG tube removal (colon or stomach) Stomach after surgery Anastomotic leakage Unroofed submucosal lesion after biopsy Upper gastrointestinal bleeding Esophageal stent fixation | 11 4 5 2 6 2 1 1 |
| Localization Upper GI tract Lower GI tract | 10 11 |
| Lesion size, mean (range), mm | 8 (2-20) |
OTSC: Over-the-scope-clip; PEG: Percutaneous endoscopic gastrostomy.
In 52% (11/21) of the patients, the suction method was used. Accessories, including the OTSC Twin Grasper and the OTSC Anchor (both Ovesco Endoscopy AG, Tübingen, Germany) were applied in 48% of patients (10/21). Primary technical success and clinical success were achieved in 85% (18/21) and 67% (14/21) of cases, respectively (Table 3). There were two failures 2/10 (20%) in the upper GI tract: one was a fibrotic fistula, 2 mm in diameter; another was at an inaccessible site, due to an esophageal stenosis. There were five failures 5/11 (45%) in the lower GI tract; two anastomotic leakages and three fistulae could not be successfully treated technically or clinically. One of these patients had a history of Crohn’s disease.
Table 3.
Outcome data of the 28 applied over-the-scope-clip in 21 patients, technical and clinical success, use of accessories, complications n (%)
| Outcome | Value |
| Number of OTSC applications | 28 |
| Primary technical success Permanent clinical success Clinical success after 2nd intervention | 18 (85) 14 (67) 3 out of 5 (60) |
| Use of accessories Twin grasper, n Tissue anchor, n | 10 patients (47) 2 9 |
| Complications, n | 0 |
Please note that in one case Twin grasper and Tissue anchor were both used. OTSC: Over-the-scope-clip.
Overall, five of twenty-one patients required additional OTSCs; three of these resulted in technical and clinical success. No complications were reported (Table 3).
DISCUSSION
This prospective series is representative of our daily clinical routine experience with the OTSC system in a tertiary endoscopy center in Switzerland. The distribution of GI lesions was typical, with a wide spectrum of indications in the upper and lower GI tract. To date, only two smaller Swiss case series on OTSC have been described. In one, Seebach et al[1] presented their experience with 7 patients that received OTSCs for treating GI perforations. In the other, Gubler et al[2] reported the successful closure of iatrogenic perforations in 14 patients.
Our series revealed an overall clinical success rate of 67% and confirmed other studies that showed that the OTSC is a useful endoscopic device for treating lesions in the GI tract. The definition of success is variable in the literature. Some authors - like us - generally defined success as the resolution of the problem[2,3], but others did not provide a specific definition[4,5]. Some studies used endoscopy to evaluate the success of an OTSC application[6]. In a systematic review, Weiland et al[7] found that OTSC showed technical and clinical success rates of 80%-100% and 57%-100%, respectively, for endoscopic closure of iatrogenic GI perforations. Other authors reported clinical success rates ranging from 71% to 95%[3,4,8-11]. To the best of our knowledge, the largest series published to date was conducted in the US, and it comprised 45 patients with a variety of indications, similar to those in our series; they reported a clinical success rate of 71%[8]. In Europe, although the results are currently unpublished, OTSC data are available for up to 84 patients, and the technical success rate was notably higher (93%)[12]. However, the authors mainly treated severe GI bleeding in the upper GI; thus, it is difficult to compare those data with ours. The current case series showed good efficacy in OTSC applications, with no severe adverse events. However, few studies have reported severe adverse events due to clip placement; adverse events included lumen obstruction of the small bowel[8], esophageal perforation[13], or the situation that the Twin grasper was fixed by an OTSC clip application by accident[12].
In our study, fistulae were the main indication; most (45%) occurred after percutaneous endoscopic gastrostomy (PEG) tube removals. In a pediatric population, persistent gastrocutaneous fistulae appeared after a PEG removal in 34% of cases[14]. For adults, to the best of our knowledge, no data exist regarding the incidence of fistulae. Our series confirmed findings from other studies that showed that fistulae are typically treated successfully with the OTSC[4,8,15,16]. We reported technical and clinical failure rates regarding fistulae of 18% and 45%, respectively. One failure appeared in a patient with Crohn’s disease. One fistula after PEG removal was not accessible, due to esophageal stenosis. The other two fistulae were related with cancer or infection. One was a fibrotic fistula. Manta et al[6] described similar problems with fibrotic tissue. Baron et al[8] reported that fistulae were the main indication in their US multicenter study. They reported a broad spectrum of clinical success, depending on the indication, but most patients had a history of bariatric surgery.
Anastomotic leakage is currently the most frequent major complication after colorectal surgery. The incidence has not decreased over the last ten years, despite technical improvements, like the stapler technique and other surgical modalities[17]. The OTSC is a helpful, innovative option for treating anastomotic leakage, given its minimally invasive character. OTSC has shown a relatively high clinical success rate and a negligible complication rate. In the present study, we reported a technical and clinical success rate of both 83% regarding the closure of anastomotic leakage. Baron et al[8] reported a success rate of 65%, but some of the patients that experienced failures had a history of extensive radiation treatment and cancer.
OTSC is described as a successful tool for achieving hemostasis in refractory upper GI bleeding after failed conventional therapy[18]. Its greatest value is found in particular situations, like Dieulafoy bleedings. A fairly new complementary hemostatic tool is known as Hemospray (Cook Medical, Winston-Salem, North Carolina, United States). In our hospital, many endoscopists have performed Hemospray in various applications, and they have achieved a very high success rate. They were also convinced with its practicability[19]. Moreover, in the event of Hemospray failure, OTSC can be applied subsequently. However, to date, no studies have compared Hemospray to OTSC.
We successfully used OTSC for closure after the unroofing of a submucosal gastric lesion to acquire a biopsy. To our knowledge, this indication has not been reported previously, and we recommend using OTSC for this kind of lesion.
One technical limitation of OTSC is the presence of endoluminal stenosis that does not allow passage of the endoscope with a mounted OTSC device. In this situation, the endoscopist can mount an OTSC with a smaller diameter or change the type of endoscope. Furthermore, fibrotic tissue is an important reason for technical failure. Fibrotic tissue is rigid and difficult to suction or pull into the transparent cap. In addition, other studies have reported limitations in using OTSC for treating chronic fistulae, particularly after radiation therapy or after thermal damage[8].
It is important to be aware that there is a maximum size limit for lesions that can be closed successfully with OTSC. Gubler et al[2] closed iatrogenic perforations up to 30 mm in diameter with OTSC, and they achieved technical success in 13 of 14 patients. They recommended the OTSC for treating perforations up to 30 mm in diameter. The lesion diameters in our series ranged from 2 to 20 mm.
This case series study had some limitations. First, our series comprised a relatively small number of patients. Second, we did not provide a control group with other therapeutic options, like surgery, alternative endoscopic devices, or a non-interventional approach. Third, the observation period and the assessment of clinical success after intervention varied, and they were not standardized. Fourth, patients treated in a tertiary endoscopy center are typically not comparable with patients in district hospitals; this represents a selection bias. Finally, the decision of whether to apply OTSC depended on the endoscopist’s judgment; therefore, patient inclusion criteria were subjective, and the study was neither case-controlled nor randomized.
In conclusion, OTSC is a useful endoscopic device for treating a variety of lesions in the upper and lower GI tract. OTSC showed a good success rate and noticeably few complications. To date, OTSC applications have only been described in case series. Future randomized prospective controlled multicenter trials are needed to compare the OTSC with other therapies.
COMMENTS
Background
The over-the-scope-clip system is a new device for endoscopic treatment of various diseases in the gastrointestinal tract like postsurgical problems or bleeding.
Research frontiers
This innovative endoscopic clip system is fairly new and therefore it is important to analyze its success and side effects.
Innovations and breakthroughs
This is the first case series that reflects daily clinical experience with the over-the-scope-clip system in a tertiary endoscopy center in Switzerland.
Applications
This case series showed a good success rate and noticeably few complications for a variety of gastrointestinal lesions with the over-the-scope-clip system. The authors provide further information to the existing literature.
Terminology
Gastro- and colonoscopes are instruments for the examination of the gastrointestinal tract. An endoscopic clip is a device for the closure of a defect. A fistula is an abnormal connection between two structures, e.g., between stomach and skin. An anastomotic leakage is an abnormal defect between two parts of the intestine that have been connected surgically.
Peer review
This case series carried information about clinical application of over-the-scope-clip in various indications of gastrointestinal lesions. The high success rate and expended indications may be interested for other gastroenterologists.
Footnotes
P- Reviewer: Gong JS, Tellez-Avila F S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
References
- 1.Seebach L, Bauerfeind P, Gubler C. “Sparing the surgeon”: clinical experience with over-the-scope clips for gastrointestinal perforation. Endoscopy. 2010;42:1108–1111. doi: 10.1055/s-0030-1255924. [DOI] [PubMed] [Google Scholar]
- 2.Gubler C, Bauerfeind P. Endoscopic closure of iatrogenic gastrointestinal tract perforations with the over-the-scope clip. Digestion. 2012;85:302–307. doi: 10.1159/000336509. [DOI] [PubMed] [Google Scholar]
- 3.Mönkemüller K, Peter S, Toshniwal J, Popa D, Zabielski M, Stahl RD, Ramesh J, Wilcox CM. Multipurpose use of the ‘bear claw’ (over-the-scope-clip system) to treat endoluminal gastrointestinal disorders. Dig Endosc. 2014;26:350–357. doi: 10.1111/den.12145. [DOI] [PubMed] [Google Scholar]
- 4.Sandmann M, Heike M, Faehndrich M. Application of the OTSC system for the closure of fistulas, anastomosal leakages and perforations within the gastrointestinal tract. Z Gastroenterol. 2011;49:981–985. doi: 10.1055/s-0029-1245972. [DOI] [PubMed] [Google Scholar]
- 5.Kirschniak A, Kratt T, Stüker D, Braun A, Schurr MO, Königsrainer A. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162–167. doi: 10.1016/j.gie.2007.01.034. [DOI] [PubMed] [Google Scholar]
- 6.Manta R, Manno M, Bertani H, Barbera C, Pigò F, Mirante V, Longinotti E, Bassotti G, Conigliaro R. Endoscopic treatment of gastrointestinal fistulas using an over-the-scope clip (OTSC) device: case series from a tertiary referral center. Endoscopy. 2011;43:545–548. doi: 10.1055/s-0030-1256196. [DOI] [PubMed] [Google Scholar]
- 7.Weiland T, Fehlker M, Gottwald T, Schurr MO. Performance of the OTSC System in the endoscopic closure of iatrogenic gastrointestinal perforations: a systematic review. Surg Endosc. 2013;27:2258–2274. doi: 10.1007/s00464-012-2754-x. [DOI] [PubMed] [Google Scholar]
- 8.Baron TH, Song LM, Ross A, Tokar JL, Irani S, Kozarek RA. Use of an over-the-scope clipping device: multicenter retrospective results of the first U.S. experience (with videos) Gastrointest Endosc. 2012;76:202–208. doi: 10.1016/j.gie.2012.03.250. [DOI] [PubMed] [Google Scholar]
- 9.Parodi A, Repici A, Pedroni A, Blanchi S, Conio M. Endoscopic management of GI perforations with a new over-the-scope clip device (with videos) Gastrointest Endosc. 2010;72:881–886. doi: 10.1016/j.gie.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, Oryu M, Masaki T. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19:2752–2760. doi: 10.3748/wjg.v19.i18.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stückle J, Probst A, Bittinger M, Scheubel R, Ebigbo A, Messmann H, Gölder sk. Klinische Erfahrungen bei der Behandlung von Perforationen, Leckagen und Fistelungen im Gastrointestinaltrakt mit dem Over the scope Clip (OTSC) Apr 3-5; Hamburg, Germany. Thieme. (Abstract in German) Deutschen Gesellschaft für Endoskopie und Bildgebende Verfahren eV Hamburg: 44th congress; 2014. p. Endoskopie heute, 2014. [Google Scholar]
- 12.Wedi E, Menke D, Hochberger J. Der Einsatz des OTSC-Makroclips bei 84 Patienten mit schwerer GI-Blutung, Fisteln und Insuffizienzen. March 14-16; Munich, Germany. Thieme. (Abstract in German) Deutsche Gesellschaft für Endoskopie und Bildgebende Verfahren: 43rd congress;; 2013. p. Endoskopie heute, 2013. [Google Scholar]
- 13.Voermans RP, Le Moine O, von Renteln D, Ponchon T, Giovannini M, Bruno M, Weusten B, Seewald S, Costamagna G, Deprez P, et al. Efficacy of endoscopic closure of acute perforations of the gastrointestinal tract. Clin Gastroenterol Hepatol. 2012;10:603–608. doi: 10.1016/j.cgh.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 14.Janik TA, Hendrickson RJ, Janik JS, Landholm AE. Analysis of factors affecting the spontaneous closure of a gastrocutaneous fistula. J Pediatr Surg. 2004;39:1197–1199. doi: 10.1016/j.jpedsurg.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Turner JK, Hurley JJ, Ketchell I, Dolwani S. Over-the-scope clip to close a fistula after removing a percutaneous endoscopic gastrostomy tube. Endoscopy. 2010;42 Suppl 2:E197–E198. doi: 10.1055/s-0030-1255693. [DOI] [PubMed] [Google Scholar]
- 16.Bertolini R, Meyenberger C, Sulz MC. First report of colonoscopic closure of a gastrocolocutaneous PEG migration with over-the-scope-clip-system. World J Gastroenterol. 2014;20:11439–11442. doi: 10.3748/wjg.v20.i32.11439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Daams F, Wu Z, Lahaye MJ, Jeekel J, Lange JF. Prediction and diagnosis of colorectal anastomotic leakage: A systematic review of literature. World J Gastrointest Surg. 2014;6:14–26. doi: 10.4240/wjgs.v6.i2.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan SM, Chiu PW, Teoh AY, Lau JY. Use of the Over-The-Scope Clip for treatment of refractory upper gastrointestinal bleeding: a case series. Endoscopy. 2014;46:428–431. doi: 10.1055/s-0034-1364932. [DOI] [PubMed] [Google Scholar]
- 19.Sulz MC, Frei R, Meyenberger C, Bauerfeind P, Semadeni GM, Gubler C. Routine use of Hemospray for gastrointestinal bleeding: prospective two-center experience in Switzerland. Endoscopy. 2014;46:619–624. doi: 10.1055/s-0034-1365505. [DOI] [PubMed] [Google Scholar]


