Abstract
Background:
Astragalus and Panax notoginseng are traditional Chinese Medicines used for the treatments of ischemic cerebrovascular disease, being often combined together in China and achieving a good effect.
Objective:
The objective of this study is to investigate the effects of astragaloside-IV (AST-IV) (the effective component of Astragalus) combined with ginsenoside Rg1, ginsenoside Rb1, notoginsenoside R1 (the effective components of P. notoginseng) on oxidative stress injury after cerebral ischemia-reperfusion in mice, and to explore the mechanisms through nuclear factor-erythroid 2-related factor-2/heme oxygenase-1 (Nrf2/HO-1) signaling pathway.
Materials and Methods:
C57BL/6 mice were randomly grouped after treated for 3 days, the model of cerebral ischemia-reperfusion injury was established, and the brain tissues were detected.
Results:
AST-IV combined with ginsenoside Rg1, ginsenoside Rb1, notoginsenoside R1 could increase significantly the survival rate of nerve cell; decrease the contents of malondialdehyde, nitric oxide, increase the activity of superoxide dismutase and the level of glutathione; Nrf2 was down-regulated in the cytoplasm while up-regulated in nucleus, nuclear translocation rate raised as well as HO-1 messenger ribonucleic acid and protein expressions increased. The effects of four active components combination were better than those of the active components alone.
Conclusion:
Active components of Astragalus and P. notoginseng had the effects against cerebral ischemia-reperfusion injury, which were related to the antioxidative stress after cerebral ischemia-reperfusion. AST-IV combined with ginsenoside Rg1, ginsenoside Rb1, notoginsenoside R1 could strengthen the antagonism effects on ischemia-reperfusion and oxidative stress injury, the mechanism underlying might be associated with jointly activating Nrf2/HO-1 signaling pathway after cerebral ischemia-reperfusion.
Keywords: Astragaloside IV, combination, ginsenoside Rb1, ginsenoside Rg1, notoginsenoside R1, nuclear factor-erythroid 2-related factor-2/heme oxygenase
INTRODUCTION
Pharmaceutical chemistry research shows that astragalosides (AST) is the effective ingredient with cardio-cerebrovascular pharmacological effect in Astragalus, and the main active component of which is AST-IV; Panax notoginseng saponins (PNS) is the effective ingredient with cardio-cerebrovascular pharmacological effect in P. notoginseng, containing mainly ginsenoside Rg1, ginsenoside Rb1 and notoginsenoside R1. Our previous studies showed that AST combined with PNS enhanced the protective effect against cerebral ischemia-reperfusion injury, which was associated with the antioxidative stress injury.[1] Because AST-IV and ginsenoside Rg1, ginsenoside Rb1, notoginsenoside R1 are the active components of AST and PNS, we speculated that the effect of the combination between AST and PNS might come from the combination of the active components.
Oxidative stress has important significance in cerebral ischemia-reperfusion injury.[2] After cerebral ischemia-reperfusion, a large amount of free radicals generated by cerebral tissues have a severe injury effects on nerve cell, inhibiting oxidative stress reaction becomes an important means to prevent ischemic injury. Nuclear factor-erythroid 2-related factor 2 (Nrf2) is an important transcription factor regulating oxidative stress. Study showed that the activation of Nrf2/anti-oxidant response elements (ARE) pathway could increase nuclear localization of Nrf2, and induce the expression of the Nrf2/ARE-dependent genes such as heme oxygenase-1 (HO-1), lessen cerebral ischemic injury.[3,4] Hence, we supposed that AST combined with PNS enhanced the antioxidative stress action may be associated with activating Nrf2/HO-1 pathway. Hence, the work studied the effect of AST-IV combined with ginsenoside Rg1, ginsenoside Rb1, notoginsenoside R1 on antioxidative stress injury, and the mechanisms through Nrf2/HO-1 signaling pathway.
MATERIALS AND METHODS
Experimental animal
C57BL/6 male mice, weighing 18-22 g, were provided by Hunan Vital River Laboratory Animal Technology Co. Limited (certificate of conformity: SCXK 2009-0004). Animals were allowed food and water ad libitum, caged in specific pathogen free animal laboratory with room temperature of 20°C ~ 25°C and humidity of 50~60%. The animal protocols were approved by Animal Ethics Committee of Hunan University of Chinese Medicine (approval number: HNCTCM 2011–085, date: June 17, 2011) and disposal of animals during the experiment accorded with “Guidance Suggestions for the Care and Use of Laboratory Animals” from the Ministry of Science and Technology of the People's Republic of China.
Drugs
Astragaloside IV was provided by Chengdu MUST bio-technology Co. Limited, extracted from the root of leguminous plants Astragalus membranaceu (Fisch.) Bunge, purity ≥98%, voucher specimen number was A0070; ginsenoside Rg1, ginsenoside Rb1 and notoginsenoside R1 were purchased from Chengdu MUST bio-technology Co. Limited, extracted from the dried roots of araliaceae plant P. notoginseng, purity ≥98%, voucher specimen number was A0237, A0234, A0273, respectively; AST-IV, ginsenoside Rg1, ginsenoside Rb1 and notoginsenoside R1 were prepared into the suspension with 0.5% sodium carboxymethyl cellulose before use. Edaravone (3-Methyl-1-phenyl-2-pyrazolin-5-one) was provided by Nanjing Pharmaceutical Co. Limited (Batch number: 80-090104, Specs: 10 mg/5 mL), prepared into the solution of 0.4 mg/mL with normal saline.
Main reagents
Malondialdehyde (MDA) kit (Batch number: A003-2), nitric oxide (NO) kit (Batch number: A012) superoxide dismutase (SOD) kit (Batch number: A001-1) and glutathione (GSH) kit (Batch number: A006) were purchased from Nanjing Jiancheng Bioengineering Co., Limited; Total protein extraction kit (Batch number: KGP2100) was purchased from Nanjing KeyGen Biotech Co., Limited; Nuclear and cytoplasmic protein extraction kit (Batch number: BB-3112-1), phosphatase inhibitor complex III (Batch number: PL019-1), modified bicinchoninic acid protein assay kit (Batch number: SK3051) were purchased from Shanghai Sangon Biotech Co., Limited; Animal tissue total ribonucleic acid (RNA) extraction kit (Batch number: Lo423) was purchased from Beijing TianGen Biotech Co., Limited; Reverse transcription kit (Batch number: ADA3500) was purchased from Promega; Rabbit antimouse β-actin antibody (Batch number: sc-130656), HO-1 antibody (Batch number: sc-10789), Nrf2 antibody (Batch number: sc-722) were purchased from Santa Gruz Biotech Co., Limited.
Model of cerebral ischemia-reperfusion
The mice were fixed in the supine position after mild anesthesia with ether, made 1 cm incision in the middle of the neck, exposed and separated the common carotid artery (CCA), and the accompanies vagus nerve, then, bilateral CCA were occluded with artery clip for 20 min followed by reperfusion for 24 h.[5,6] Mice of the sham group were only exposed bilateral CCA. Sutured the skin, the mice continued to be fed and medicated as above while body temperature was maintained at 37-38°C. After reperfusion, the mice were decapitated, the brain stem and cerebellar cortex were removed, and the remaining brain tissues were detected.
Animal groups and administration
Our previous study showed that the effective combination dose of AST-IV, ginsenoside Rg1, ginsenoside Rb1, and notoginsenoside R1 antagonizing oxidative stress and improving energy metabolism was 40 mg/kg, 50 mg/kg, 40 mg/kg and 10 mg/kg, respectively. Hence, the mice were randomly divided into eight groups: Sham, model, AST-IV (40 mg/kg), ginsenoside Rg1 (50 mg/kg), ginsenoside Rb1 (40 mg/kg), notoginsenoside R1 (10 mg/kg), four active components combination (AST-IV 40 mg/kg + ginsenoside Rg1 50 mg/kg + ginsenoside Rb1 40 mg/kg + notoginsenoside R1 10 mg/kg) and edaravone (4 mg/kg), with eight mice in each group. Edaravone group were received intraperitoneal injection (10 ml/kg), twice daily for 3 days. Sham group and model group were gavaged with 0.5% sodium carboxymethyl cellulose (10 ml/kg), the left were given the same volume/weight medicine by gavage at AM 8:00, once a day for 3 days. After treatment for 1 h on day 3, the cerebral ischemia-reperfusion model was established. The same administration was carried out as above during reperfusion.
Detections of histomorphology in hippocampus CA1
After reperfusion for 24 h, 2 cm brain tissues were removed from the posterior of the optic chiasm, fixed with paraformaldehyde, and embedded in paraffin. Pathological changes in hippocampus CA1 were observed with hematoxylin and eosin staining, and nerve cells were counted. In normal nerve cells, cell membrane was clear, cytoplasm was red, nucleus was blue, and nucleoli could be seen, hematoxylin was even; but damaged nerve cells appeared karyopyknosis, dissolution, acidophilic or vacuolar degeneration. Five nonoverlapping views were taken of each section at high magnification (×400), percentage of normal nerve cells among total nerve cells was the survival rate of nerve cells. The mean of five visual fields was used for statistical analysis.
Detections of oxidative stress parameters
Brain tissues were mixed with cold phosphate buffered saline (PBS) (brain tissue: PBS = 1:9) to acquire 10% homogenate, which were centrifuged for 15 min at 4°C (3500 rpm) to obtain the supernatant to test. The activity of SOD was detected by nitroblue tetrazolium,[7] the contents of MDA and NO were detected using thiobarbituric acid reaction and nitrate reductase methods,[8,9] GSH examination adopted chemical chromometry method.[10]
Detections of nuclear factor-erythroid 2 related factor 2 messenger ribonucleic acid and heme oxygenase-1 messenger ribonucleic acid in brain tissues (reverse transcription polymerase chain reaction)
A total of 20 mg of brain tissues were removed from the front of the optic chiasm, total RNA was extracted by Trizol method, A260/A280 of which was 1.8-2.0, purity >90%. Then RNA was transcripted reversely into complementary deoxyribonucleic acid (cDNA) by random primers, cDNA was used as the template for polymerase chain reaction (PCR) amplification. Nrf2 gene (RS ID: NM-010902.3): The upstream primer: 5’-ATCAAAAAGCCCCATTCACA-3’, the downstream primer: 5’-CCGCCTTTTCAGTAGATGGA-3’, the amplified fragment was 364 bp; HO-1 gene (RS ID: NM-010442.2): The upstream primer: 5’-AGCCCCACCAAGTTCAAACA-3’, the downstream primer: 5’-TGCCAACAGGAAGCTGAGAG-3’, the amplified fragment was 321 bp; β-actin gene (RS ID: NM-007393.3): The upstream primer: 5’-GAGACCTTCAACACCCCAGC-3’, the downstream primer: 5’-CCACAGGATTCCATACCCAA-3’, the amplified fragment was 446 bp. Amplification system: 10 × butter 2 μL, deoxynucleotide triphosphates (all 2.5 mmol/L) 1 μL, primer (10 pmol/μL) l μL, Taq enzyme (5 U/μL) 2.5 U, Mg2+ (25 mmol/L) 1.0 μL, template DNA 1 μL, ddH2O 13.5 μL, and the final volume was 20 μL; amplification conditions: 95°C for 2 min, 94°C for 45s, 60°C for 30s and 72°C for 2 min, 35 cycles, and then 72°C for 10 min. To detect the products of PCR amplification with 1% agarose gel electrophoresis, scan the target band with ChampGel5500 gel image system and mensurate the integral optical density (IOD) with pro-plus image analysis software. The ratio of the IOD values of the objective gene band and β-actin band was taken as relative expression of the objective gene.
Detections of nuclear factor-erythroid 2-related factor 2 protein in the cytoplasm and nucleus, heme oxygenase-1 protein in whole cell of brain tissues (western-blotting)
First, to take the remaining brain tissues to extract the whole cell, cytoplasm and nuclear protein according to the instructions of the kits; to determine the protein concentration to ascertain the sample protein contents of whole cell, cytoplasm and nucleus. Then, the protein sample was mixed with 4× sodium dodecyl sulfate gel sample buffer, boiled and denatured for 5-10 min, separated for 2-3 h with 100 V electrophoresis, transferred into the 3 × 7 cm poly vinylidene fluoride membrane for 1 h with 300 mA constant current. Next, the membrane was closed for 3 h with Tris buffered saline solution, washed for 3 times with TBST, incubated respectively with β-actin antibody (1:1000), Nrf2 antibody (1:500), HO-1 antibody (1:500), overnight at 4°C, washed for 3 times. Finally, the membrane was continued to incubate with the corresponding second antibodies labeled by horseradish peroxidase (1:1000) at room temperature for 1 h, washed for 3 times, developed with the enhanced diaminobenzidine chromogenic substrate kit to scan and test the IOD of protein band. To use the β-actin expression of the total protein as an internal reference, and the ratio of the IOD values of the objective protein band and β-actin protein band as relative expression of the target protein.
Statistical analysis
Statistical package SPSS16.0 (SPSS Inc., Chicago, IL, USA) was used for analyses; all data were expressed as mean ± standard deviation (SD). One-way analysis of variance was used for multigroup comparison, among every two groups, least significant difference test was used for analysis of homogeneity of variance (heterogeneity of variance was converted into homogeneity). Values of P < 0.05 were considered statistically significant.
RESULTS
Comparison of nerve cells injury in hippocampus CA1 among the groups
In the sham group, nerve cell injury hardly could be seen, cell hierarchical structure was clear, morphology was normal. In model group, pyramidal cells had lost their normal structure and were disorganized, partial cells presented edema, eosinophilic degeneration and karyopyknosis change, the survival rate of nerve cells was far lower than that of the sham group (P < 0.01). Compared with model group, nerve cell injury was alleviated significantly; the survival rate was increased significantly in treatment groups (all P < 0.01). The survival rate in four active components combination group was higher than that in four active components alone (P < 0.01 or P < 0.05), had no significant difference compared with edaravone (P > 0.05) [Figures 1 and 2].
Figure 1.
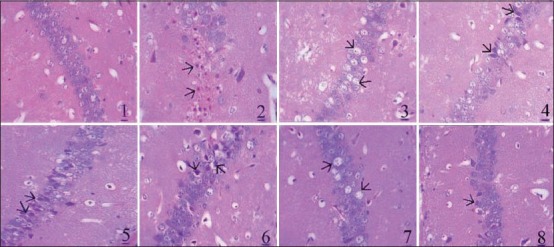
Pathological changes in hippocampus CA1 among the groups (H and E, ×400, ×400, bar = 20 μm). Hematoxylin and eosin sections of brain tissues showed normal morphology in sham group, edema, eosinophilic degeneration and karyopyknosis of nerve cells could be seen in model group and treatment groups (arrows). (1) Sham. (2) Model. (3) Astragaloside IV. (4) Ginsenoside Rg1. (5) Ginsenoside Rb1. (6) Notoginsenoside R1. (7) Four active components combination. (8) Edaravone
Figure 2.
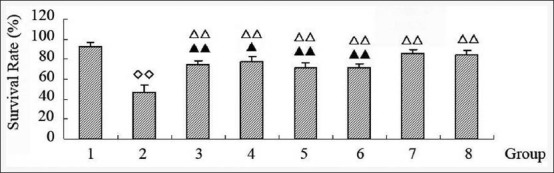
Comparison of neurocyte survival rate in hippocampus CA1 among the groups (1) Sham. (2) Model. (3) Astragaloside IV. (4) Ginsenoside Rg1. (5) Ginsenoside Rb1. (6) Notoginsenoside R1. (7) Four active components combination. (8) Edaravone. Values represent the mean ± standard deviation from the eight mice in each group; ∞P < 0.01, versus sham; ΔΔP < 0.01, versus model; ▴P < 0.05, ▴▴P < 0.01, versus four active components combination
Comparison of oxidative stress parameters in brain tissues among the groups
After cerebral ischemia-reperfusion, the contents of MDA and NO in brain tissues were increased significantly, while SOD activity and GSH level were decreased (P < 0.01 or P < 0.05). AST-IV decreased significantly MDA and NO contents (all P < 0.01), ginsenoside Rg1 decreased significantly NO content (P < 0.01), ginsenoside Rb1 and notoginsenoside R1 had no effects on MDA, NO, SOD, GSH (all P > 0.05). Four active components combination decreased significantly MDA and NO contents, increased SOD activity and GSH level, furthermore, the effects were better than most of active components alone (P < 0.01 or P < 0.05). There were no significant differences between four active components combination and edaravone (all P > 0.05) [Table 1].
Table 1.
Comparison of oxidative stress parameters among the groups
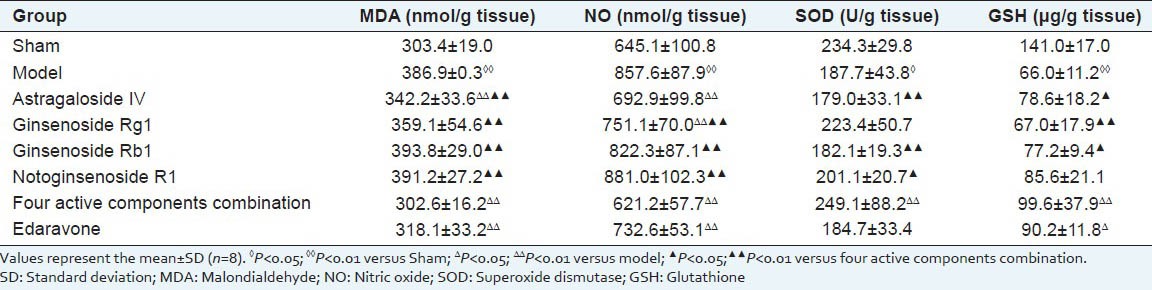
Comparison of nuclear factor-erythroid 2-related factor 2 messenger ribonucleic acid and protein expressions in brain tissues among the groups
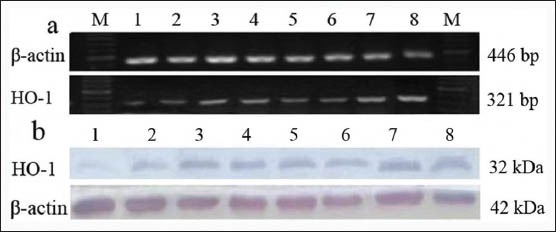
Compared with sham group, Nrf2 messenger ribonucleic acid (mRNA) was up-regulated significantly in model group (P < 0.05). Compared with model group, there was no significant change in treatment groups (all P > 0.05) [Figure 3, Table 2].
Figure 3.
Gene and protein expression of nuclear factor-erythroid 2-related factor 2 among the groups: (a) Messenger ribonucleic acid map. (b) Western-blotting pattern in cytoplasm. (c) Western-blotting pattern in nucleus. (1) Sham. (2) Model. (3) Astragaloside IV. (4) Ginsenoside Rg1. (5) Ginsenoside Rb1. (6) Notoginsenoside R1. (7) Four active components combination. (8) Edaravone
Table 2.
Comparison of Nrf2 mRNA, protein expression and Nrf2 nuclear translocation rate among the groups in the brain tissues
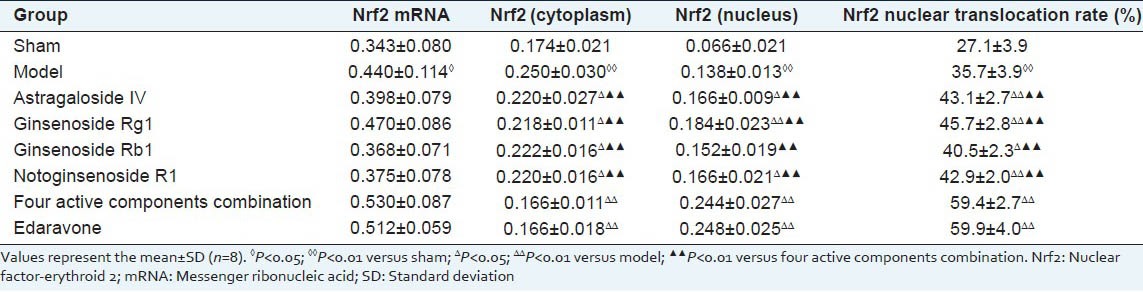
Compared with sham group, Nrf2 protein expression of cytoplasm was up-regulated significantly in model group (P < 0.01), while down-regulated significantly in treatment groups compared to model group (P < 0.05 or P < 0.01), and the fall of four active components combination group on Nrf2 protein of cytoplasm was more obvious than that of four active components alone (all P < 0.01), presented no significant difference compared to edaravone (P > 0.05) [Figure 3, Table 2].
Compared with sham group, Nrf2 protein expression of nucleus was increased obviously in model group (P < 0.01). Compared with model group, Nrf2 protein expression of nucleus was further increased in AST-IV, ginsenoside Rg1, notoginsenoside R1, four active components combination and edaravone (P < 0.05 or P < 0.01), had no significant change in Ginsenoside Rb1 (P > 0.05). The increase of Nrf2 protein of the nucleus in four active components combination was stronger than that in four active components alone (all P < 0.01), had no significant difference compared to edaravone (P > 0.05) [Figure 3, Table 2].
Compared with sham group, Nrf2 nuclear translocation rate was raised significantly in model group (P < 0.01), further increased in treatment groups compared to model group (P < 0.05 or P < 0.01). The effect on Nrf2 nuclear translocation rate in four active components combination was above four active components alone (P < 0.05), had no significant difference compared to edaravone (P > 0.05) [Table 2].
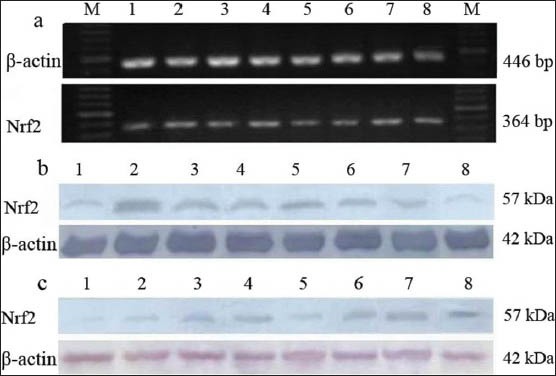
Comparison of heme oxygenase-1 messenger ribonucleic acid and protein expressions in brain tissues among the groups
Compared with sham group, HO-1 mRNA and protein expressions were increased significantly in model group (P < 0.01 or P < 0.05). Compared with model group, HO-1 mRNA and protein expressions were further increased in AST-IV, ginsenoside Rg1, four active components combination and edaravone (P < 0.01 or P < 0.05), had no significant changes in ginsenoside Rb1 and notoginsenoside R1 alone (all P > 0.05). The increases of four active components combination on HO-1 mRNA and protein expressions were better than those of four active components alone (all P < 0.01), the differences were not statistical significances between four active components combination and edaravone (all P > 0.05) [Figures 4 and 5].
Figure 4.
Gene and protein expressions of heme oxygenase-1 (HO-1) among the groups. (a) HO-1 messenger ribonucleic acid map. (b) Western-blotting pattern of HO-1. (1) Sham. (2) Model. (3) Astragaloside IV. (4) Ginsenoside Rg1. (5) Ginsenoside Rb1. (6) Notoginsenoside R1. (7) Four active components combination. (8) Edaravone
Figure 5.
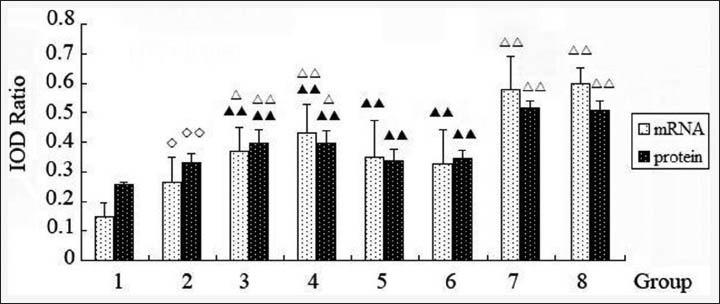
Comparison of heme oxygenase-1 messenger ribonucleic acid and protein expression in brain tissues among the groups: (1) Sham. (2) Model. (3) Astragaloside IV. (4) Ginsenoside Rg1. (5) Ginsenoside Rb1. (6) Notoginsenoside R1. (7) Four active components combination. (8) Edaravone. Values represent the mean ± standard deviation from the eight mice in each group; ◊P < 0.05, ◊◊P < 0.01, versus sham; ΔP < 0.05, ΔΔP < 0.01, versus model; ▴▴P < 0.01, versus four active components combination
DISCUSSION AND CONCLUSION
About the toxicity of the effective components of Astragalus and P. notoginseng, it was reported that the lethal dose 50 (LD50) of ginsenoside Rg1 in mice by oral administration was more than 5000 mg/kg, the LD50 of ginsenoside Rg1, ginsenoside Rb1, notoginsenoside R1 by intraperitoneal injection was 1250 mg/kg, 1208 mg/kg, 688 mg/kg, respectively.[11,12] It was laid down in the Pharmacopoeia of the People's Republic of China that the content of AST-IV in Astragalus was not <0.04%, mice were given A. membranaceus 75 g/kg by gavage, no abnormal reaction was observed within 48 h, the LD50 of intraperitoneally injected Astragalus in mice was 40 g/kg. It suggested that the effective components of Astragalus, P. notoginseng were scarcely toxicity, belongs to the nontoxic grade according to “Chemicals-Test method of acute oral toxicity for chemicals-acute toxic class method (GB/T 21757-2008)”. So, we inferred that the toxicity of AST-IV combined with ginsenoside Rg1, ginsenoside Rb1 and notoginsenoside R1 was low.
After cerebral ischemia, especially reperfusion, a lot of free radicals are produced, resulting in oxidative damage of brain tissues. Oxygen free radical (OFR) often attacks unsaturated fatty acid; causing lipid peroxidation to generate MDA, MDA level in tissues indirectly reflects the metabolic status of OFR and the damaged degree of tissues by free radicals. NO, also is a free radical, has neurotoxicity.[13,14] Normally, the body also has natural free radical scavenging systems, such as GSH peroxidase (GSH-PX), SOD, GSH and so on.[15,16] The activity level of SOD in tissues can reflect partly the body's ability of eliminating free radicals. GSH can integrate with peroxides and free radicals, reducing the damage to the proteins and enzymes. After cerebral ischemia, SOD, GSH-PX, GSH are decreased significantly because of free radical generated and antioxidant substances consumed.[17,18]
Our study showed that nerve cell in hippocampus CA1 happened to degeneration and necrosis after cerebral ischemia-reperfusion for 24 h, the survival rate was decreased; AST-IV and ginsenoside Rg1, ginsenoside Rb1, notoginsenoside R1 could prevent the decrease of nerve cell livability in hippocampus CA1, suggesting that AST-IV and Ginsenoside Rg1, Ginsenoside Rb1, notoginsenoside R1 had an inhibitory effect on cerebral ischemia-reperfusion injury. Furthermore, the effect of four active components combination was better than that of four active components alone. The results proved that AST-IV combined with ginsenoside Rg1, ginsenoside Rb1, notoginsenoside R1 could strengthen the effects against cerebral ischemia-reperfusion injury, also confirmed that the effect of AST combined with PNS on enhancing the anticerebral ischemia-reperfusion injury mainly come from the combination of the active components.
Our results also showed that MDA and NO contents in brain tissues were increased significantly while SOD activity and GSH content were decreased after cerebral ischemia-reperfusion, suggesting that free radicals were produced, antioxidants were consumed, oxidative damage was occurred in brain tissues. AST-IV could inhibit the increase of MDA and the production of NO; ginsenoside Rg1 could reduce NO generated; There were no effects on MDA, NO, SOD and GSH in ginsenoside Rb1 and notoginsenoside R1. However, four active components combination could decrease significantly the productions of MDA and NO, increase SOD activity and GSH content, AST-IV combined with ginsenoside Rg1, ginsenoside Rb1, notoginsenoside R1 had a stronger effect against oxidative stress injury after cerebral ischemia-reperfusion. It indicated that the combination of four active components could strengthen the anti-oxidative stress injury, thus enhance the protective effect on ischemic brain tissues.
Normally, Kelch-like ECH-associated protein-1 (Keap 1) in kytoplasm forms complexes with Nrf2 to inhibit the activity of Nrf2. Under oxidative stress, Nrf2 is separated from Keap 1, translocating into the nucleus, combining with ARE, and activating the expressions of anti-oxidant genes, enhancing cells resistance on oxidative stress.[19] The mode of transient middle cerebral artery occlusion and Nrf2 gene knockout experiments had confirmed that Nrf2 played an important endogenous neuroprotective response after ischemic stroke,[20,21] the activation of Nrf2/ARE pathway could relieve cerebral ischemic injury.[3] HO-1 is a major antioxidant gene regulated by ARE, expressed widely in the brain tissues as well as up-regulated after transient cerebral ischemia.[22] The increase of HO-1 expression induced by HO-1 inducer or transgenic technology can prompt the anti-oxidant ability of tissues, inhibit the inflammatory reaction, reduce cerebral ischemia-reperfusion injury, have protective effects on ischemia-reperfusion tissues.[23] Study showed that the neurons of HO-1 knockout increased susceptibility to oxidative stress injury while the increase of HO-1 expression enhanced neuronal tolerance to oxidative stress.[24,25]
Our results showed that Nrf2 mRNA expression in brain tissues was significantly up-regulated, at the same time, Nrf2 protein content was increased in the cytoplasm and nucleus, nuclear translocation rate was raised, HO-1 mRNA and protein expressions were enhanced after cerebral ischemia-reperfusion. It suggested that Nrf2/HO-1 pathway was activated to meet the stimulation of ischemia and hypoxia after cerebral ischemia, which was a protective response generated by the body. All active components could promote the activation of Nrf2; moreover, AST-IV and ginsenoside Rg1 could increase the expression of HO-1, suggesting that the inhibitory effect of active components on oxidative damage after cerebral ischemia-reperfusion was related to the activation of Nrf2/HO-1 pathway. Furthermore, the effects of four active components combination promoting Nrf2 activation and HO-1 expression were better than those of the active components alone. It suggested that the combination of four active components could enhance the activation of Nrf2/HO-1 signaling pathway, up-regulated the expression and synthesis of anti-oxidant HO-1, thereby played stronger effects than single components, which might be one of the mechanisms that four active components combination enhanced the antagonism against oxidative stress injury after cerebral ischemia-reperfusion. However, the enhancement of the combination on antioxidative stress injury came from the joint effect of four active components or some of four active components were unclear in this work. In the future, there are important values to study the combination among the active components for further clarifying the synergistic mechanisms of active components combination, promoting the rational combination of active components.
Footnotes
Source of Support: National Natural Science Foundation of China (No. 81102557); Doctoral Program Foundation of Higher Education of China (No. 20104323110001); Aid Project for Innovation Platform Open Fund of Hunan province university (No. 11K050); Key Project of Administration of traditional Chinese Medicine of Hunan province (No. 201301); General Project of Education Bureau of Hunan Province (No. 11C0963); Aid Program for Science and Technology Innovative Research Team in Higher Educational Institutions of Hunan Province for “Related research on prevention and treatment of cardio-cerebrovascular diseases with integrated traditional Chinese and Western Medicine”, Hunan Province Natural Science Innovation Group for “Fundamental research of Chinese medicine on prevention and treatment of cardio-cerebrovascular diseases”
Conflict of Interest: None declared.
REFERENCES
- 1.Tan H, Huang XP, Deng CQ. Effects of astragaloside and Panax notoginseng saponins combination on oxidative stress of cerebral ischemic reperfusion injury in mice. Zhong Xi Yi Jie He Xue Bao. 2010;8:448–52. doi: 10.3736/jcim20100508. [DOI] [PubMed] [Google Scholar]
- 2.Rodrigo J, Fernández AP, Serrano J, Peinado MA, Martínez A. The role of free radicals in cerebral hypoxia and ischemia. Free Radic Biol Med. 2005;39:26–50. doi: 10.1016/j.freeradbiomed.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 3.Son TG, Camandola S, Arumugam TV, Cutler RG, Telljohann RS, Mughal MR, et al. Plumbagin, a novel Nrf2/ARE activator, protects against cerebral ischemia. J Neurochem. 2010;112:1316–26. doi: 10.1111/j.1471-4159.2009.06552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang C, Zhang X, Fan H, Liu Y. Curcumin upregulates transcription factor Nrf2, HO-1 expression and protects rat brains against focal ischemia. Brain Res. 2009;1282:133–41. doi: 10.1016/j.brainres.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Yonekura I, Kawahara N, Nakatomi H, Furuya K, Kirino T. A model of global cerebral ischemia in C57 BL/6 mice. J Cereb Blood Flow Metab. 2004;24:151–8. doi: 10.1097/01.WCB.0000096063.84070.C1. [DOI] [PubMed] [Google Scholar]
- 6.Yang G, Kitagawa K, Matsushita K, Mabuchi T, Yagita Y, Yanagihara T, et al. C57BL/6 strain is most susceptible to cerebral ischemia following bilateral common carotid occlusion among seven mouse strains: Selective neuronal death in the murine transient forebrain ischemia. Brain Res. 1997;752:209–18. doi: 10.1016/s0006-8993(96)01453-9. [DOI] [PubMed] [Google Scholar]
- 7.Minami M, Yoshikawa H. A simplified assay method of superoxide dismutase activity for clinical use. Clin Chim Acta. 1979;92:337–42. doi: 10.1016/0009-8981(79)90211-0. [DOI] [PubMed] [Google Scholar]
- 8.Buege JA, Aust SD. Microsomal lipid peroxidation. Methods Enzymol. 1978;52:302–10. doi: 10.1016/s0076-6879(78)52032-6. [DOI] [PubMed] [Google Scholar]
- 9.Kiechle FL, Malinski T. Nitric oxide. Biochemistry, pathophysiology, and detection. Am J Clin Pathol. 1993;100:567–75. doi: 10.1093/ajcp/100.5.567. [DOI] [PubMed] [Google Scholar]
- 10.Zhang J. 1st ed. Beijing: Beijing Medical University and China Xie-He Medical University Joint Publishing House; 1998. The method of modern pharmacology experiment [M] pp. 1656–7. [Google Scholar]
- 11.1st ed. 5[M] Shanghai: Science and Technology Publishing House; 1999. State Administration of Traditional Chinese Medicine. Chinese Materia Medica; pp. 839–50. [Google Scholar]
- 12.Huang TK. 1st ed. 5[M] Beijing: Chinese Medicine Science and Technology Press; 1994. Handbook of Composition and Pharmacological action Commonly Used Traditional Chinese Medicine; pp. 125–174.pp. 15–119. [Google Scholar]
- 13.Liu DH, Yuan FG, Hu SQ, Diao F, Wu YP, Zong YY, et al. Endogenous nitric oxide induces activation of apoptosis signal-regulating kinase 1 via S-nitrosylation in rat hippocampus during cerebral ischemia-reperfusion. Neuroscience. 2013;229:36–48. doi: 10.1016/j.neuroscience.2012.10.055. [DOI] [PubMed] [Google Scholar]
- 14.Chen XM, Chen HS, Xu MJ, Shen JG. Targeting reactive nitrogen species: A promising therapeutic strategy for cerebral ischemia-reperfusion injury. Acta Pharmacol Sin. 2013;34:67–77. doi: 10.1038/aps.2012.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Endo H, Nito C, Kamada H, Yu F, Chan PH. Reduction in oxidative stress by superoxide dismutase overexpression attenuates acute brain injury after subarachnoid hemorrhage via activation of Akt/glycogen synthase kinase-3beta survival signaling. J Cereb Blood Flow Metab. 2007;27:975–82. doi: 10.1038/sj.jcbfm.9600399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vasiljević B, Maglajlić-Djukić S, Gojnić M, Stanković S. The role of oxidative stress in perinatal hypoxic-ischemic brain injury. Srp Arh Celok Lek. 2012;140:35–41. [PubMed] [Google Scholar]
- 17.Mršić-Pelčić J, Pilipović K, Pelčić G, Vitezić D, Župan G. Temporal and regional changes of superoxide dismutase and glutathione peroxidase activities in rats exposed to focal cerebral ischemia. Cell Biochem Funct. 2012;30:597–603. doi: 10.1002/cbf.2839. [DOI] [PubMed] [Google Scholar]
- 18.Cao Y, Mao X, Sun C, Zheng P, Gao J, Wang X, et al. Baicalin attenuates global cerebral ischemia/reperfusion injury in gerbils via anti-oxidative and anti-apoptotic pathways. Brain Res Bull. 2011;85:396–402. doi: 10.1016/j.brainresbull.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Kensler TW, Wakabayashi N, Biswal S. Cell survival responses to environmental stresses via the Keap1-Nrf2-ARE pathway. Annu Rev Pharmacol Toxicol. 2007;47:89–116. doi: 10.1146/annurev.pharmtox.46.120604.141046. [DOI] [PubMed] [Google Scholar]
- 20.Tanaka N, Ikeda Y, Ohta Y, Deguchi K, Tian F, Shang J, et al. Expression of Keap1-Nrf2 system and antioxidative proteins in mouse brain after transient middle cerebral artery occlusion. Brain Res. 2011;1370:246–53. doi: 10.1016/j.brainres.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 21.Shah ZA, Li RC, Thimmulappa RK, Kensler TW, Yamamoto M, Biswal S, et al. Role of reactive oxygen species in modulation of Nrf2 following ischemic reperfusion injury. Neuroscience. 2007;147:53–9. doi: 10.1016/j.neuroscience.2007.02.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schipper HM, Song W, Zukor H, Hascalovici JR, Zeligman D. Heme oxygenase-1 and neurodegeneration: Expanding frontiers of engagement. J Neurochem. 2009;110:469–85. doi: 10.1111/j.1471-4159.2009.06160.x. [DOI] [PubMed] [Google Scholar]
- 23.Li Volti G, Sorrenti V, Murabito P, Galvano F, Veroux M, Gullo A, et al. Pharmacological induction of heme oxygenase-1 inhibits iNOS and oxidative stress in renal ischemia-reperfusion injury. Transplant Proc. 2007;39:2986–91. doi: 10.1016/j.transproceed.2007.09.047. [DOI] [PubMed] [Google Scholar]
- 24.Chen-Roetling J, Benvenisti-Zarom L, Regan RF. Cultured astrocytes from heme oxygenase-1 knockout mice are more vulnerable to heme-mediated oxidative injury. J Neurosci Res. 2005;82:802–10. doi: 10.1002/jnr.20681. [DOI] [PubMed] [Google Scholar]
- 25.Li Q, Li J, Zhang L, Wang B, Xiong L. Preconditioning with hyperbaric oxygen induces tolerance against oxidative injury via increased expression of heme oxygenase-1 in primary cultured spinal cord neurons. Life Sci. 2007;80:1087–93. doi: 10.1016/j.lfs.2006.11.043. [DOI] [PubMed] [Google Scholar]


