Abstract
Endosseous implants have revolutionized the field of Implants and Periodontics. Implant placement is a viable option in the treatment of partial and full edentulism. However, placement of implants in alveolar deficiencies may lead to adverse angulations, mechanical overload and esthetic dissatisfaction. When minimum dimensions for implant placement are not present in alveolar process, it is necessary to augment the size of the ridge. This can be achieved by various methods and materials. Here we present a successful case of vertical and horizontal ridge augmentation in anterior maxilla using autograft, xenograft and titanium mesh with simultaneous placement of implants, where autograft was obtained from the same site avoiding secondary surgical site.
Keywords: Alveolar ridge augmentation, autograft, endosseous implants, titanium mesh, xenograft
INTRODUCTION
Resorption of alveolar bone is a common clinical problem which can be a physiologic or a pathologic process. The deformities and defects may occur as a result of tooth loss due to extraction, advanced periodontal diseases or trauma, long term use of removable appliances, dehiscence and fenestration defects, developmental defects/clefts, congenitally missing teeth and odontogenic cysts and tumors.[1]
Advanced alveolar bone loss (>7 mm) may result in esthetically and functionally compromised dental prosthesis like removable and fixed partial dentures and ideal implant placement in prosthetically driven position.[1] The end goal of the therapy is to provide a functional restoration that is in harmony with the adjacent natural dentition. Thus augmentation of bone is often necessary.[2] Advances in biologic understanding of different bone regenerating materials and continuous innovations in surgical techniques have led to increased predictability in reconstruction of alveolar ridge defects and functional implant placement.[3]
Augmentation of insufficient bone volume can be brought about by different methods, including, particulate and block grafting materials, Guided Bone Regeneration with or without growth and differentiation factors, ridge splitting, expansion and distraction osteogenesis, either alone or in combination. These techniques may be used for horizontal/vertical ridge augmentation, socket preservation and sinus augmentation.[2]
In this article, we present a unique case of vertical and horizontal ridge augmentation in anterior maxilla using autograft, xenograft and titanium mesh with simultaneous placement of endosseous implants, where autograft was obtained from the same site avoiding second surgical site.
CASE REPORT
A 45 year male patient reported, seeking treatment for his missing front teeth. He lost four anteriors and a premolar at the age of 25 years in a road traffic accident and had been using removable partial denture since then [Figure 1a] The patient was in good health with non-contributory medical history, good oral hygiene and a strong desire to restore the area with a permanent fixed prosthesis.
Figure 1.
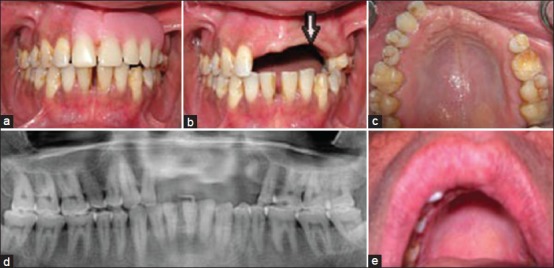
(a) Preoperative intraoral view. (b) Vertical ridge resorption with reversal of architecture. (c) Horizontal ridge resorption. (d) Preoperative orthopantamograph. (e) Drooping of lips on left side
Clinical and radiographic examination revealed severe vertical ridge resorption in maxillary anterior region with highest resorption in left lateral incisor region, leading to reversal of architecture [Figure 1b and d]. Decrease in horizontal width of alveolar ridge was evident from left central incisor to left first premolar region [Figure 1c]. Also, drooping of lips was evident on left side [Figure 1e].
The amount of bone available was inadequate for implant supported bridge. Hence, vertical and horizontal alveolar bone augmentation with simultaneous placement of endoosseous implants in right and left central incisor and left premolar region were planned. Autograft from the left canine region, for vertical bone augmentation in left lateral incisor region, was planned, as patient was not willing for secondary surgical site. For horizontal bone augmentation, Bio-oss, a xenograft, and Titanium mesh were planned. Later, for esthetic purpose, soft tissue augmentation was planned, if required, for which patient did not agree. The complete treatment procedure was explained to the patient and duly signed consent according to Declaration of Helsinki was obtained.
Surgical procedure
The surgical procedure was performed in sterile surgical field. Preoperative decontamination of oral cavity with chlorhexidine 0.2% mouthrinse (Clohex Plus, Dr Reddy's Laboratories Limited, Hyderabad, India) for 1 min and perioral skin disinfection with 5% povidone-iodine solution (Nicodin, Abbott Healthcare Pvt Ltd, Mumbai, India) was done. Site was anesthetized using 2% Lidocaine with 1:80000 adrenaline (La-Force, Anhil Parenterals Pvt. Ltd, Patan, India). Horizontal incision on the alveolar crest and two vertical releasing incisions were given and a full thickness flap was reflected. A knife edge type ridge was seen on reflection of flap [Figure 2a]. Bleeding points were created on the recipient bed. A rectangular corticocancellous block graft was harvested from the canine region of the same site using trephine bur [Figure 2b], shaped, positioned firmly in the lateral incisor area and then anchored with the help of titanium screws. Three endosseous implants (Osstem, GS system, South Korea) were placed with cover screw [Figure 2c]. Bio-oss (Geistlich Pharmaceutical, Wolhusen, Switzerland) was used to cover the entire area contained in titanium mesh (Micromesh, Stryker Leibinger, Kalamazoo, MI) [Figure 2d]. The mesh was stabilized with three fixation screws to prevent any micromovement during the healing phase. Following this, the surgical site was closed with the flap and primary wound closure was obtained by horizontal mattress and interrupted sutures (Ethicon 5-0, LNW 5080, Johnson & Johnson Pvt. Ltd, H.P, India) [Figure 2e]. The area was covered with the periodontal dressing (Coe pack, GC America Inc, USA) to protect it and facilitate healing.
Figure 2.
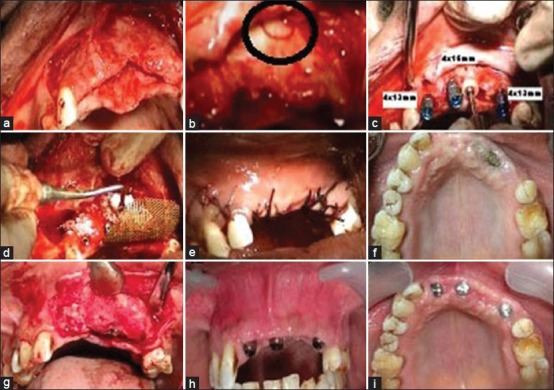
(a) Knife edge ridge. (b) Bone graft harvested from same surgical site using trephine bur. (c) Autogenous block graft secured with titanium screw and 3 endosseous implants placed in recipient site. (d) Placement of Bio-oss and fixation of titanium mesh. (e) Recipient site sutured. (f) Exposure of titanium mesh in 3rd month. (g) Regenerated bone with embedded implants seen after 6 months. (h) and (i) Improved Vertical height and horizontal width after 6 months
Post-surgical and Oral hygiene instructions were given to the patient. Chemical plaque control with chlorhexidine 0.2% (1 min mouthrinse, 3 times a day) was instituted for 2 weeks along with nonsteroidal antiinflammatory analgesic (Diclofenac 50 mg, 3 times a day for 3 days initially and SOS thereafter) and antibiotic (Amoxicillin 500 mg, 3 times a day for 10 days).
Sutures were removed after 10 days. Patient was examined weekly for the first 4 weeks; and then once every month. In the third month, exposure of titanium mesh in the central incisor region was noticed [Figure 2f]. Patient was asked to maintain the area using 1% Chlorhexidine gel application (Hexigel, ICPA Health Products Ltd, Mumbai India) twice a day. After 6 months the site was re-entered with reflection of full thickness flap and titanium mesh was removed. Newly formed bone was seen with implants embedded in it [Figure 2g]. There was appreciable increase in vertical height and horizontal width of bone [Figure 2h and i]. Screw caps were removed and transfer abutments were placed [Figure 3a]. A 5 unit metal ceramic bridge was subsequently fabricated and cemented [Figure 3b]. The lip drooping on left side was completely eliminated which can be compared from Figure 1e and 3c. Intraoral periapical radiograph of left central incisor region revealed bone regeneration [Figure 3 and e].
Figure 3.
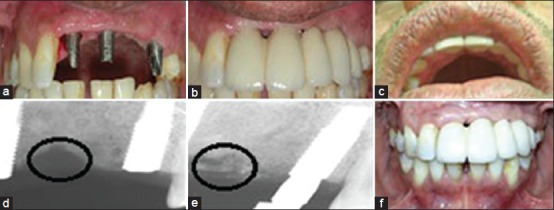
(a) Transfer abutments placed. (b) Final prosthesis - Five unit metal ceramic bridge cemented. (c) Lip drooping eliminated on left side. (d) Preoperative IOPA radiograph of left lateral incisor region. (e) Postoperative IOPA radiograph showing bone fill in left lateral incisor region. (f) One year postoperative picture showing partial filling of black triangles
On 1 year follow up, partial filling of black triangles in the interdental areas was evident due to creeping attachment. [Figure 3f].
DISCUSSION
Ridge augmentation procedures prior to conventional fixed prosthodontics or implant therapy are indicated when an adequate width or height of the alveolar ridge is not present. Overall the survival rates of implants placed in augmented ridges is 87% (range from 60% to 100%).[4] The present case had severe bone resorption due to trauma as well as long term wear of removable partial dentures. Thus augmentation was necessary to place the implants in a biologically accepted and prosthetically driven location to achieve optimal function and esthetics.
The use of corticocancellous bone grafts for ridge augmentation in implant dentistry was first reported by Breine and Branemark.[5] The revascularization of corticocancellous block grafts takes place at a much faster rate than in cortical bone autografts. Revascularization of block grafts enables maintenance of their vitality, and, hence, reduces chances of graft infection and necrosis.[2]
Autograft is considered as the Gold Standard for bone transplantation[2] and various studies have shown efficacy for same.[6,7,8,9,10,11,12,13,14] It is osteogenic, osteoconductive and osteoinductive. Autografts can be derived from extraoral source (iliac crest, ribs) or intraoral source (chin, ramus). They can be used in block or particulate form.[2] Corticocancellous block grafts are preferred because of enhanced revascularization of the cancellous portion, and mechanical support and rigidity of the cortical portion, which ensures optimal ridge augmentation.[15] The healing of autogenous block grafts has been described as “creeping substitution” where viable bone replaces the necrotic bone within the graft and is highly dependent on graft angiogenesis and revascularization.[2] There is no risk of rejection or adverse immunological reaction with autogenous bone grafts. They are highly advantageous but are associated with risks, such as donor site morbidity, limited bone availability, size mismatch, drooping of chin, nerve damage, tooth devitalization, gingival recession, increased postoperative discomfort, infection and blood loss.[16] In our case, we obtained autogenous coticocancellous block graft from canine region of same surgical site, thus avoiding secondary site morbidity and used it for vertical ridge augmentation in left lateral incisor area. Bleeding points were created on recipient bed, which increases rate of revascularization, the availability of osteoprogenitor cells and the rate of remodeling. Block graft was stabilized using titanium screws to avoid movement. The key to success is elimination of graft mobility and dead space between the graft and host bone.[16]
The use of xenografts for bone grafting was reported in 1889 by Senn.[17] Xenografts are derived from another species and are considered to be biocompatible and osteoconductive. Bovine xenografts are commonly used and well tolerated in intraoral procedures. They have better results in maxillary bone (D3, D4 type). Bovine Bone Material (BBM) has been successfully used to correct defects adjacent to implants as well as in sinus lift and alveolar ridge augmentation procedures. Grafted BBM particles once embedded in mineralized bone, and as long as no special stimuli occurs, act similarly to host bone, which often undergoes remodeling process at a very slow rate.[18] In this case, we used a potential BBM, Bio-oss for horizontal ridge augmentation, which provided excellent results after 6 months.
In 1996, von Arx et al., introduced titanium micromesh for reconstructive implant surgery with positive results for staged approach[6] as well as simultaneous procedure[7] for implant placement. Titanium mesh has excellent biocompatibility and handling properties that allow their application for three dimensional reconstruction of alveolar bone defects. 0.2 mm thick mesh is most commonly used, which gives the flap sufficient retention to prevent dehiscence. It acts as a protective matrix to contain graft material, maintain space and facilitate bone in growth, but is not cell occlusive.[19] Recent clinical studies[14,5,6,7,8,9,10,11,12,13,14,15,16,19,20] have confirmed reliability of this technique with different types of grafts. Because of the porosity, the rate of revascularization is likely more rapid compared to more conventional techniques, such as titanium-reinforced polytetrafluoroethylene or collagen membranes.[20] It is also important to note that titanium mesh is very technique sensitive, with exposure rates reported from 20% to 40%.[2] Mesh exposure complications can often be managed without a significant impact on the results. For example, a small exposure of the mesh can usually be managed with plaque removal at the exposed portion of the mesh and local application of 0.12% chlorhexidine. As long as no obvious infection is present, the mesh removal can be delayed until the originally planned time,[20] as done in the present case.
Complete soft tissue coverage was obtained after the graft and mesh stabilization. Degree of regeneration directly correlates with the adequacy of soft tissue coverage and surface area of the vascularized bony walls.[21] Thus implying that primary wound coverage is a necessity for bone regeneration.
The combination approach is useful in treating severe defects involving multiple missing teeth, where individual approaches alone may not be sufficient to achieve desired results [Table 1]. Implant supported bridges are equally good alternative to removable or fixed prosthesis in restoration of long span edentulous areas, with less failure rates.[22] Hence in this case we planned ridge augmentation with implant supported bridge, in which 1 year follow up results were satisfactory [Figure 3f].
Table 1.
Brief review of studies related to use of autogenous bone graft, bovine bone material and titanium mesh

CONCLUSION
Combination of autogenous graft, bovine bone material and titanium mesh for horizontal and vertical augmentation with simultaneous placement of implants resulted in better functional and esthetic restorations. Autogenous bone grafts from same surgical site can be used for augmentation of smaller defects, but may not be feasible for larger areas.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Wang HL, Al-Shammari K. HVC ridge deficiency classification: A therapeutically oriented classification. Int J Periodontics Restorative Dent. 2002;22:335–43. [PubMed] [Google Scholar]
- 2.McAllister BS, Haghighat K. Bone augmentation techniques. J Periodontol. 2007;78:377–96. doi: 10.1902/jop.2007.060048. [DOI] [PubMed] [Google Scholar]
- 3.Klokkevold PR. Localized bone augmentation and implant site development. In: Newman MG, Takei HH, Klokkevold PR, Carranza FA, editors. Clinical Periodontology. 10 ed. Philadelphia: Saunders; 2006. pp. 1133–47. [Google Scholar]
- 4.Chiapasco M, Casentini P, Zaniboni M. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants. 2009;24(Suppl):237–59. [PubMed] [Google Scholar]
- 5.Breine U, Branemark PI. Reconstruction of alveolar jaw bone: An experimental and clinical study of immediate and preformed autologous bone grafts in combination with osseointegrated implants. Scand J Plast Reconstr Surg. 1980;14:23–48. doi: 10.3109/02844318009105733. [DOI] [PubMed] [Google Scholar]
- 6.von Arx T, Hardt N, Wallkmamm B. The TIME technique: A new method for localized ridge augmentation prior to placement of dental implants. Int J Oral Maxillofac Implants. 1996;11:387–94. [PubMed] [Google Scholar]
- 7.von Arx T, Wallkmamm B, Hardt N. Localized ridge augmentation using a micro titanium mesh: A report on 27 implants followed from 1 to 3 years after functional loading. Clin Oral Implants Res. 1998;9:123–30. doi: 10.1034/j.1600-0501.1998.090208.x. [DOI] [PubMed] [Google Scholar]
- 8.Proussaefs P, Lozada J, Kleinman A, Rohrer MD, McMillan PJ. The use of titanium mesh in conjunction with autogenous bone graft and inorganic bovine bone material (Bio-oss) for localized alveolar ridge augmentation: A human study. Int J Periodontics Restorative Dent. 2003;23:185–95. [PubMed] [Google Scholar]
- 9.Roccuzzo M, Ramieri G, Spada MC, Bianchi SD, Berrone S. Vertical alveolar ridge augmentation by means of a titanium mesh and autogenous bone grafts. Clin Oral Implants Res. 2004;15:73–81. doi: 10.1111/j.1600-0501.2004.00998.x. [DOI] [PubMed] [Google Scholar]
- 10.Proussaefs P, Lozada J. Use of titanium mesh for staged localized alveolar ridge augmentation: Clinical and histologic-histomorphometric evaluation. J Oral Implantol. 2006;32:237–47. doi: 10.1563/1548-1336(2006)32[237:UOTMFS]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Corinaldesi G, Pieri F, Marchetti C, Finn M, Aldini NN, Giardino R. Histologic and histomorphometric evaluation of alveolar ridge augmentation using bone grafts and titanium micromesh in humans. J Periodontol. 2007;78:1477–484. doi: 10.1902/jop.2007.070001. [DOI] [PubMed] [Google Scholar]
- 12.Pieri F, Corinaldesi G, Fini M, Aldini MM, Giardino R, Marchetti C. Alveolar ridge augmentation with titanium mesh and a combination of autogenous bone and anorganic bovine bone: A 2 year prospective study. J Periodontol. 2008;79:2093–103. doi: 10.1902/jop.2008.080061. [DOI] [PubMed] [Google Scholar]
- 13.Corinaldesi G, Pieri F, Sapigni L, Marchetti C. Evaluation of survival and success rates of dental implants placed at the time of or after alveolar ridge augmentation with an autogenous mandibular bone graft and titanium mesh: A 3 to 8 year retrospective study. Int J Oral Maxillofac Implants. 2009;24:1119–124. [PubMed] [Google Scholar]
- 14.Khamees J, Darwiche MA, Kochaji N. Alveolar ridge augmentation using chin bone graft, bovine bone mineral, and titanium mesh: Clinical, histological, and histomorphometric study. J Ind Soc Periodontol. 2012;16:235–40. doi: 10.4103/0972-124X.99268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenberg E, Rose LF. Biologic and clinical considerations for autografts and allografts in periodontal regeneration therapy. Dent Clin North Am. 1998;42:467–90. [PubMed] [Google Scholar]
- 16.Fu JH, Wang HL. Horizontal Bone Augmentation: The Decision Tree. Int J Periodontics Restorative Dent. 2011;31:429–36. [PubMed] [Google Scholar]
- 17.Senn. On the healing of aseptic bone cavities by implantation of antiseptic decalcified bone. Ann Surg. 1889;10:352–68. doi: 10.1097/00000658-188907000-00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zitzmann NU, Scharer P, Mrinello CP, Schupbach P, Berglundh T. Alveolar ridge augmentation with Bio-oss: A histological study in humans. Int J Periodontics Restorative Dent. 2001;21:288–95. [PubMed] [Google Scholar]
- 19.Misch C, Wang HL. Clinical applications of recombinant human bone morphogenetic Protein-2 for bone augmentation before dental implant placement. Clin Adv Periodontics. 2011;1:118–31. doi: 10.1902/cap.2011.110037. [DOI] [PubMed] [Google Scholar]
- 20.McAllister BS, Eshraghi VT. Alveolar ridge augmentation with allograft stem cell–abased matrix and titanium mesh. Clin Adv Periodontics. 2013;3:1–7. [Google Scholar]
- 21.Hiatt WH, Schallhorn RG. Intraoral transplants of cancellous bone and marrow in periodontal lesions. J Periodontol. 1973;44:194–08. doi: 10.1902/jop.1973.44.4.194. [DOI] [PubMed] [Google Scholar]
- 22.Dhingra K. Oral rehabilitation consideration for partially edentulous periodontal patients. J Prosthodontics. 2012;21:494–13. doi: 10.1111/j.1532-849X.2012.00864.x. [DOI] [PubMed] [Google Scholar]


