Abstract
High-resolution ultrasound has been used recently to characterize median and ulnar nerves, but is seldom used to characterize radial nerves. The radial nerve is more frequently involved in entrapment syndromes than the ulnar and median nerves. However, the reference standard for normal radial nerves has not been established. Thus, this study measured the cross-sectional areas of radial nerves of 200 healthy male or female volunteers, aged 18 to 75, using high-resolution ultrasound. The results showed that mean cross-sectional areas of radial nerves at 4 cm upon the lateral epicondyle of the humerus and mid-humerus (midpoint between the elbow crease and axilla) were 5.14 ± 1.24 and 5.08 ± 1.23 mm2, respectively. The age and the dominant side did not affect the results, but the above-mentioned cross-sectional areas were larger in males (5.31 ± 1.25 and 5.19 ± 1.23 mm2) than in females (4.93 ± 1.21 and 4.93 ± 1.23 mm2, respectively). In addition, the cross-sectional areas of radial nerves were positively correlated with height and weight (r = 0.38, 0.36, respectively, both P < 0.05). These data provide basic clinical data for the use of high-resolution ultrasound for the future diagnosis, treatment, and prognostic evaluation of peripheral neuropathies.
Keywords: nerve regeneration, high-resolution ultrasound, radial nerve, cross-sectional area, peripheral nerve, nerve lesion, neural regeneration
Introduction
The current approach for localizing and assessing the severity of traumatic peripheral nerve injuries involves clinical evaluation and electrodiagnostic studies. However, the ability of these approaches to determine the extent of nerve damage within the first 6 weeks after trauma is limited (Cartwright et al., 2007b). Furthermore, the availability of CT and MR neurography may be limited, and the costs can be significant. In comparison, ultrasonography is a portable, dynamic, and relatively low-cost technology (Lee et al., 2011). With the development of scientific technology, applications of high-resolution ultrasound have rapidly developed in biomedical fields. High-resolution sonography clearly depicts peripheral nerve size spaces occupying lesions and anatomic variants along the entire length of the normative nerve. Using sonography, peripheral nerves have a fibrillar appearance, which is tape-like on longitudinal scans and ovoid on transverse scans. Ultrasonographic patterns correlate well with histological structures. Normal peripheral nerves have a characteristic echotexture. Nerves are composed of hypoechoic fascicules within a hyperechoic environment. The radial nerve is frequently more involved in entrapment syndromes than the ulnar and median nerves. However, an accurate diagnosis is not apparent, and is obtained only by exclusion, which sometimes delays initiation of effective treatment. In addition, reference values have not been published for the cross-sectional areas of radial nerves studied in diseases of the peripheral nervous system (Kleinert and Mehta, 1996). The median, radial, and ulnar nerves of the upper limbs may be affected by various peripheral neuropathies, each of which may be categorized according to its cause, as either an entrapment or a nonentrapment neuropathy (Martinoli et al., 2004). High-resolution ultrasonography has been shown to be useful for the localization of ulnar neuropathy (Ng et al., 2011), and can support clinical and electrophysiological testing for detection of a variety of nerve abnormalities, including entrapment neuropathies, traumas, infectious disorders, and tumors (Bacigalupo et al., 2003). In the last 20 years, many studies have examined the usefulness of this technology, but most have explored imaging of the median nerve (Cartwright et al., 2007a; Chen et al., 2011). The radial nerve is frequently more involved in entrapment syndromes than the ulnar and median nerves (Kleinert and Mehta, 1996), but the reference standard for normal radial nerves has not been established. Thus, the present study sought to obtain high-resolution ultrasonography images of radial nerves, and sought to assess possible relationships between the cross-sectional areas and the patient's height and weight.
Participants and Methods
Participants
A total of 245 volunteers were recruited by advertisement. Recruited individuals included medical students, hospital staff and patients, all without peripheral neuropathy or upper-limb injury. Forty-five of these volunteers were excluded because of a history of peripheral neuropathy, acute trauma involving the upper extremity, previous trauma in the region of the wrist, or brachial plexus injury. Specifically, individuals were excluded if they experienced numbness, tingling pain, and needle sensation pain or weakness in their hand or arm (Cartwright et al., 2009). All participants provided written informed consent. The experimental protocol was approved by the Institutional Human Study Committee of the Affiliated Hospital of Guiyang Medical College, China.
Inclusion and exclusion of participants at different ages are listed in Figure 1.
Figure 1.
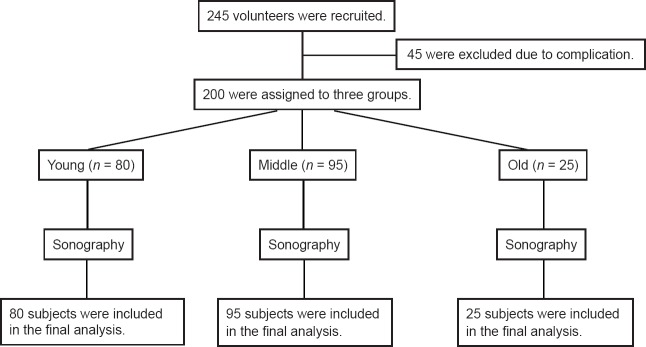
Inclusion and exclusion preceeding of participants.
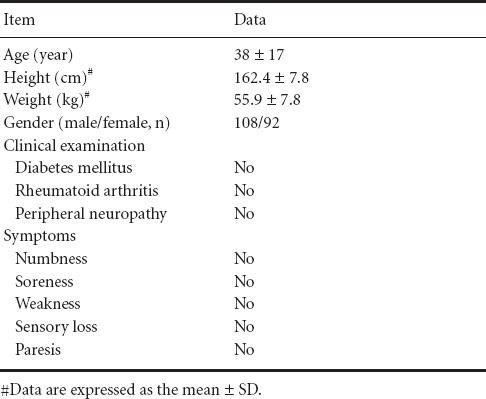
Therefore, 200 subjects were included in the final analysis. The clinical features of the included 200 normal volunteers are shown in Table 1.
Table 1.
Clinical features of 200 normal volunteers
According to their age, the subjects were assigned to young (18–30 years, n = 80), middle (31–60 years, n = 95), and old (61–75 years, n = 25) groups. The clinical features of healthy volunteers in different groups are shown in Table 2. The clinical features of healthy volunteers with different genders are shown in Table 3.
Table 2.
Clinical features of healthy volunteers in different groups
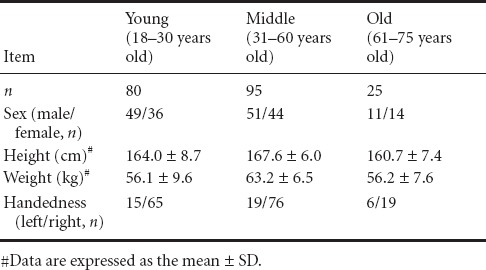
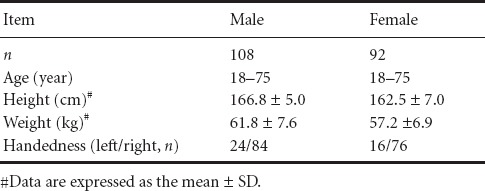
Table 3.
Clinical features between male and female healthy volunteers
Ultrasound measurements
A high-resolution ultrasound system (AKOKA SSD-4000; Toshiba, Tokyo, Japan) with a linear array transducer of 10 MHz was used. Depth, gain, and dynamic range were adjusted appropriately for optimal differentiation between nerves and other soft tissue structures. The ultrasound images were obtained by experienced operators, by placing the transducer perpendicular to the normal radial nerve at all levels of the normal radial nerve on bilateral arms. To generate reference values, an ultrasonographer measured the cross-sectional area of the radial nerve at two sites in 200 volunteers. Pressure of the transducer on the skin was kept to a minimum to minimize deformation of underlying structures (Beekman et al., 2004; Visser, 2009). At each site, the cross-sectional area of the radial nerve was obtained by circumferentially tracing just inside the hyperechonic rim of the nerve. The transducer was placed perpendicular to the nerve, so the smallest and most accurate cross-sectional area could be obtained, and the mean value was used in further calculations. The images were obtained with the participant in a supine position. The cross-sectional area value was measured three times at the same site. Cross-sectional areas were measured at the following locations: 4 cm upon the lateral epicondyle of the humerus (4 cm), and mid-humerus (midpoint between the elbow crease and the axilla) (Figure 2). At each site, the cross-sectional area of the radial nerve was obtained by tracing just inside the hyperechoic rim of the nerve. Age, sex, height, and weight were obtained from each volunteer. We compared nerve size in dominant and nondominant upper arms as well as between men and women. Correlation coefficients were calculated by comparing nerve size with height and weight.
Figure 2.
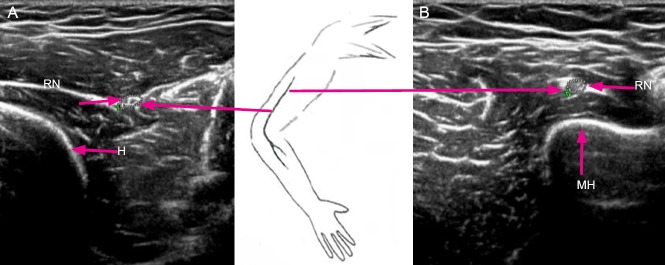
High-resolution ultrasonography of two measuring sites of the radial nerve (RN).
(A) Transverse sonogram of the radial nerve at 4 cm proximal to the tip of the lateral epicondyle of humerus (4 cm); (B) transverse sonogram of the radial nerve at mid-humerus (midpoint between elbow crease and axilla). H: Humerus bone; MH: mid-humerus.
Statistical analysis
Data were analyzed using SPSS 11.5 software (SPSS, Chicago, IL, USA), and were expressed as the mean ± SD. Statistical analysis was performed using the independent sample t-test. P values less than 0.05 were considered statistically significant. To correlate the cross-sectional area of nerves with other parameters, Pearson's correlation analysis was used.
Results
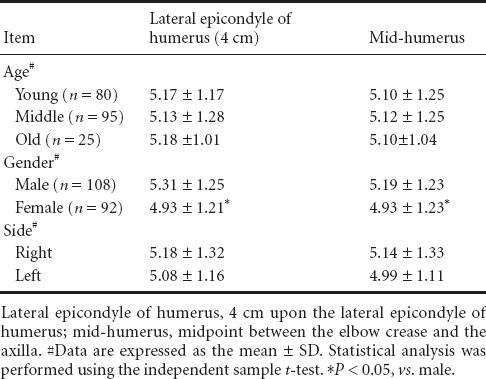
Cross-sectional area of the upper-radial nerves of healthy people
The mean cross-sectional areas of the radial nerves were as follows: at 4 cm at the lateral epicondyle of the humerus (4 cm), 5.14 ± 1.24 mm2; and at mid-humerus (midpoint between the elbow crease and axilla), 5.08 ± 1.23 mm2. There was no statistical difference in mean cross-sectional areas of the radial nerves among the three groups (P > 0.05). Women had smaller mean cross-sectional areas of the radial nerve than men in two measuring sites (lateral epicondyle of humerus and mid-humerus) (P < 0.05). There was no statistical difference in mean cross-sectional areas of radial nerves when dominant and nondominant arms were compared (P > 0.05; Table 4).
Table 4.
Cross-sectional area (mm2) of the radial nerve of normal subjects
Relationships of cross-sectional areas of upper-radial nerves to height and weight in healthy people
Pearson's correlation analysis showed that the mean cross-sectional areas of radial nerves were strongly correlated with height and weight, with a correlation coefficient of 0.38 (P < 0.05). There was also a correlation between weight and the cross-sectional areas of radial nerves, with a correlation coefficient of 0.36 (P < 0.05, Figure 3).
Figure 3.
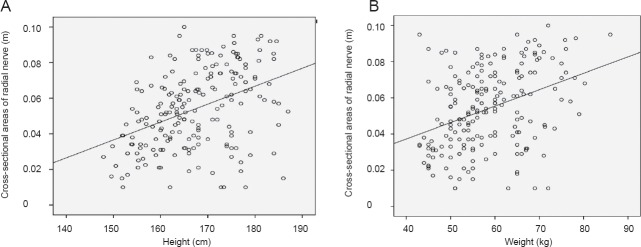
Cross-sectional areas of the radial nerve and its correlation with height and weight.
There are positive correlations between the radial nerve cross-sectional area and height (A; r = 0.38, P < 0.05), and positive correlations between the radial nerve cross-sectional area and weight (B; r = 0.36, P < 0.05).
Discussion
The radial nerve is the largest branch of the brachial plexus. It is the continuation of the posterior cord, with nerve fibers from C6, C7, C8, and occasionally T1. Radial nerve compression or injury may occur at any point along the anatomic course of the nerve, and may have varied etiologies. The most frequent site of compression is in the proximal forearm in the area of the supinator muscle, which involves the posterior interosseous branch. However, problems occur proximally in relation to fractures of the humerus at the junction of the middle and proximal thirds, as well as distally on the radial aspect of the wrist (Thomsen and Dahlin, 2007; Robson et al., 2008). The radial nerve was visible throughout the upper arm, and could be easily identified and measured at two sites. The area of the nerve was consistent throughout its entire length. Clinical, laboratory, and electrodiagnostic studies are the main parameters used in the diagnosis of polyneuropathy. An accurate etiological diagnosis is of paramount importance, providing information for appropriate treatment, prognosis, and genetic counseling. High-resolution sonography of the peripheral nervous system allows nerves to be readily visualized to assess their morphologies (Goedee et al., 2013). Using this technique, the main pathological changes have been nerve enlargement and increased hypoechogenicity. The normal reference values may be helpful in the diagnosis of pathologies involving these nerves. High-resolution ultrasound and electrophysiological examination can be used in the diagnosis and evaluation of ulnar nerve entrapment at the elbow (Zhong et al., 2012). Ultrasonography is capable of providing morphological information of nerves, including the exact location, course, and extent (Zhang et al., 2013). For example, sonography has revealed intriguingly different patterns of nerve enlargement between inflammatory neuropathies and axonal and inherited polyneuropathies.
High-resolution ultrasound is a powerful tool in the assessment of peripheral nerve disease. Nerve ultrasound is an evolving new discipline (Hobson-Webb et al., 2012). Normal peripheral nerves have a typical sonographic appearance, exhibiting multiple longitudinal hypoechoic bands, which represent fascicular bundles. These are separated by discontinuous bands of increased echogenicity, corresponding to the surrounding epineurium (Hammer et al., 2006; Tagliafico et al., 2008; Thoirs et al., 2008; Yoon et al., 2008). A previous study supported the hypothesis that high-resolution ultrasound could reliably measure the cross-sectional areas of peripheral nerves (Alshami et al., 2009). Nonetheless, the diameter rather than cross-sectional area was commonly used to evaluate nerve size (Kincaid and Barrett, 2005; Cartwright et al., 2007a; Alshami et al., 2009). Measurement of the cross-sectional area instead of maximal nerve diameter is preferred, which has been advocated by other studies (Park et al., 2004; Mallouhi et al., 2006; Koenig et al., 2009).
The radial nerves in the present study had quite different configurations, suggesting that calculations using a continuous boundary trace of the nerves should provide the most accurate cross-sectional areas. The observed variations in the shape of the nerves involved from round to oval shapes at different locations throughout the upper arm. In the present study, it may be speculated that the cross-sectional area is a more consistent index for measurement, and a more reliable measurement than the diameter, because nerves have inconsistent radial shapes. There was no statistical difference in nerve size when dominant and nondominant arms were compared, but women did have smaller nerves than men. The radial nerve in two measuring sites (lateral epicondyle of the humerus, 4 cm; and mid-humerus) showed statistical differences between men and women. Of all the variables measured, linear regression analysis showed a significant correlation of the cross-sectional areas of radial nerves with weight and height in healthy adults. This finding implied that height should be considered to have a major impact on the evaluation of the measured area of the radial nerve in normal patients. There was no significant difference between the three groups, and no significant difference in cross-sectional areas between dominant and nondominant arms, with significantly higher nerve areas in men than women.
The precise reason for such discrepancy is largely unknown. Much of this variability may be due to differences in measurement techniques, along with differences between the populations studied. Apart from the known interindividual differences in nerve thicknesses, there may be a reason, in the literature, for the broad range of normative values reported for the ultrasonographic diagnosis of peripheral nerve entrapments (Wein and Albers, 2002; Wong et al., 2002). High-frequency ultrasound evaluation should be considered in the evaluation of nerve injury, which can facilitate the early diagnosis and treatment of surgical nerve injuries (Hollister et al., 2012). Our experience seems to favor the conclusion that examination of nerves in the extremities is a promising new application of high-resolution ultrasound. This study provides normative data on radial nerve sonoanatomy at the upper arm. We feel the reference values obtained in this study are essential for facilitating a better diagnosis of abnormal nerve conditions, such as entrapment, hereditary neuropathies, acquired neuropathies, trauma, and nerve tumors, which can result in an increase in nerve cross-sectional areas. High-resolution sonography can therefore be useful to assess the underlying cause of superficial radial nerve pathology, and cross-sectional area reference values at sites along the nerve will therefore assist in the evaluation of these conditions (Beekman et al., 2004; Cartwright et al., 2007a; Cartwright et al., 2008; Hobson-Webb et al., 2012).
In our routine studies, a 10-MHz linear array transducer was used to scan the radial nerve of the upper arm in both the transverse and longitudinal planes. We found that the cross-sectional area is a more consistent measurement. There are several study limitations that should be considered. There was a small sample in every group, and there were only two ultrasonic measurement points. Healthy individuals displayed a strong correlation between cross-sectional area of the radial nerve and weight or height. The cross-sectional areas of the radial nerves of healthy people displayed little difference between left and right sides, although nerves in males seemed to be larger than females in the upper arm. The reference values obtained in this study will help facilitate the study of abnormal nerve conditions, and the information on side-to-side variations and sex-specific differences should also be helpful. Although the ultrasound study of peripheral nerves is relatively new, with further refinement of ultrasound technology, clinicians should be able to gain more precise knowledge of the ultrasound appearance of the extremities. It is therefore expected that this technology will have a major impact on the diagnosis, treatment, and prognosis of patients who are suspected of having a nerve lesion.
Acknowledgments:
We thank the staff from the Ultrasound Room of the Department of Neurology, the Affiliated Hospital of Guiyang Medical College in China for their help.
Footnotes
Funding: This study was supported by the Natural Science Foundation of Guizhou Province, No. J[2009]2157.
Conflicts of interest: None declared.
Copyedited by Takemoto L, Frenchman B, Yu J, Qiu Y, Li CH, Song LP, Zhao M
References
- Alshami AM, Cairns CW, Wylie BK, Souvlis T, Coppieters MW. Reliability and size of the measurement error when determining the cross-sectional area of the tibial nerve at the tarsal tunnel with ultrasonography. Ultrasound Med Biol. 2009;35:1098–1102. doi: 10.1016/j.ultrasmedbio.2009.01.011. [DOI] [PubMed] [Google Scholar]
- Bacigalupo L, Bianchi S, Valle M, Martinoli C. Ultrasonography of peripheral nerves. Radiologe. 2003;43:841–849. doi: 10.1007/s00117-003-0963-y. [DOI] [PubMed] [Google Scholar]
- Beekman R, Schoemaker MC, Van Der Plas JP, Van Den Berg LH, Franssen H, Wokke JH, Uitdehaag BM, Visser LH. Diagnostic value of high-resolution sonography in ulnar neuropathy at the elbow. Neurology. 2004;62:767–773. doi: 10.1212/01.wnl.0000113733.62689.0d. [DOI] [PubMed] [Google Scholar]
- Cartwright MS, Shin HW, Passmore LV, Walker FO. Ultrasonographic findings of the normal ulnar nerve in adults. Arch Phys Med Rehab. 2007a;88:394–396. doi: 10.1016/j.apmr.2006.12.020. [DOI] [PubMed] [Google Scholar]
- Cartwright MS, Chloros GD, Walker FO, Wiesler ER, Campbell WW. Diagnostic ultrasound for nerve transection. Muscle Nerve. 2007b;35:796–799. doi: 10.1002/mus.20761. [DOI] [PubMed] [Google Scholar]
- Cartwright MS, Passmore LV, Yoon JS, Brown ME, Caress JB, Walker FO. Cross-sectional area reference values for nerve ultrasonography. Muscle Nerve. 2008;37:566–571. doi: 10.1002/mus.21009. [DOI] [PubMed] [Google Scholar]
- Cartwright MS, Shin HW, Passmore LV, Walker FO. Ultrasonographic reference values for assessing the normal median nerve in sdults. J Neuroimaging. 2009;19:47–51. doi: 10.1111/j.1552-6569.2008.00256.x. [DOI] [PubMed] [Google Scholar]
- Chen J, Wu S, Ren J. Ultrasonographic measurement of median nerve cross-sectional area reference values in a healthy Han population from Guiyang, China. Neural Regen Res. 2011;6:1883–1887. [Google Scholar]
- Goedee HS, Brekelmans GJ, van Asseldonk JTH, Beekman R, Mess WH, Visser LH. High resolution sonography in the evaluation of the peripheral nervous system in polyneuropathy -a review of the literature. Eur J Neurol. 2013;20:1342–1351. doi: 10.1111/ene.12182. [DOI] [PubMed] [Google Scholar]
- Hammer HB, Hovden IAH, Haavardsholm EA, Kvien TK. Ultrasonography shows increased cross-sectional area of the median nerve in patients with arthritis and carpal tunnel syndrome. Rheumatology (Oxford) 2006;45:584–588. doi: 10.1093/rheumatology/kei218. [DOI] [PubMed] [Google Scholar]
- Hobson-Webb LD, Padua L, Martinoli C. Ultrasonography in the diagnosis of peripheral nerve disease. Expert Opin Med Diagn. 2012;6:457–471. doi: 10.1517/17530059.2012.692904. [DOI] [PubMed] [Google Scholar]
- Hollister AM, Simoncini A, Sciuk A, Jordan J. High frequency ultrasound evaluation of traumatic peripheral nerve injuries. Neurol Res. 2012;34:98–103. doi: 10.1179/1743132811Y.0000000048. [DOI] [PubMed] [Google Scholar]
- Kincaid BR, Barrett SL. Use of high-resolution ultrasound in evaluation of the forefoot to differentiate forefoot nerve entrapments. J Am Podiatr Med Assoc. 2005;95:429–432. doi: 10.7547/0950429. [DOI] [PubMed] [Google Scholar]
- Kleinert JM, Mehta S. Radial nerve entrapment. Orthop Clin North Am. 1996;27:305–315. [PubMed] [Google Scholar]
- Koenig RW, Pedro MT, Heinen CPG, Schmidt T, Richter H-P, Antoniadis G, Kretschmer T. High-resolution ultrasonography in evaluating peripheral nerve entrapment and trauma. Neurosurg Focus. 2009;26:E13. doi: 10.3171/FOC.2009.26.2.E13. [DOI] [PubMed] [Google Scholar]
- Lee FC, Singh H, Nazarian LN, Ratliff JK. High-resolution ultrasonography in the diagnosis and intraoperative management of peripheral nerve lesions. J Neurosurg. 2011;114:206–211. doi: 10.3171/2010.2.JNS091324. [DOI] [PubMed] [Google Scholar]
- Mallouhi A, Pültzl P, Trieb T, Piza H, Bodner G. Predictors of carpal tunnel syndrome: accuracy of gray-scale and color Doppler sonography. Am J Roentgenol. 2006;186:1240–1245. doi: 10.2214/AJR.04.1715. [DOI] [PubMed] [Google Scholar]
- Martinoli C, Bianchi S, Pugliese F, Bacigalupo L, Gauglio C, Valle M, Derchi LE. Sonography of entrapment neuropathies in the upper limb (wrist excluded) J Clin Ultrasound. 2004;32:438–450. doi: 10.1002/jcu.20067. [DOI] [PubMed] [Google Scholar]
- Ng ES, Vijayan J, Therimadasamy AK, Tan TC, Chan YC, Lim A, Wilder-Smith E. High resolution ultrasonography in the diagnosis of ulnar nerve lesions with particular reference to post-traumatic lesions and sites outside the elbow. Clin Neurophysiol. 2011;122:188–193. doi: 10.1016/j.clinph.2010.04.035. [DOI] [PubMed] [Google Scholar]
- Park GY, Kim JM, Lee SM. The ultrasonographic and electrodiagnostic findings of ulnar neuropathy at the elbow1. Arch Phys Med Rehab. 2004;85:1000–1005. doi: 10.1016/j.apmr.2003.09.016. [DOI] [PubMed] [Google Scholar]
- Robson AJ, See MS, Ellis H. Applied anatomy of the superficial branch of the radial nerve. Clin Anat. 2008;21:38–45. doi: 10.1002/ca.20576. [DOI] [PubMed] [Google Scholar]
- Tagliafico A, Pugliese F, Bianchi S, Bodner G, Padua L, Rubino M, Martinoli C. High-resolution sonography of the palmar cutaneous branch of the median nerve. Am J Roentgenol. 2008;191:107–114. doi: 10.2214/AJR.07.3383. [DOI] [PubMed] [Google Scholar]
- Thoirs K, Williams MA, Phillips M. Ultrasonographic measurements of the ulnar nerve at the elbow: role of confounders. J Ultrasound Med. 2008;27:737–743. doi: 10.7863/jum.2008.27.5.737. [DOI] [PubMed] [Google Scholar]
- Thomsen NOB, Dahlin LB. Injury to the radial nerve caused by fracture of the humeral shaft:Timing and neurobiological aspects related to treatment and diagnosis. Scand J Plast Recons. 2007;41:153–157. doi: 10.1080/02844310701445586. [DOI] [PubMed] [Google Scholar]
- Visser LH. High-resolution sonography of the superficial radial nerve with two case reports. Muscle Nerve. 2009;39:392–395. doi: 10.1002/mus.21246. [DOI] [PubMed] [Google Scholar]
- Wein TH, Albers JW. Electrodiagnostic approach to the patient with suspected peripheral polyneuropathy. Neurol Clin. 2002;20:503–526. doi: 10.1016/s0733-8619(01)00010-x. vii. [DOI] [PubMed] [Google Scholar]
- Wong SM, Griffith JF, Hui ACF, Tang A, Wong KS. Discriminatory sonographic criteria for the diagnosis of carpal tunnel syndrome. Arthritis Rheum. 2002;46:1914–1921. doi: 10.1002/art.10385. [DOI] [PubMed] [Google Scholar]
- Yoon JS, Walker FO, Cartwright MS. Ultrasonographic swelling ratio in the diagnosis of ulnar neuropathy at the elbow. Muscle Nerve. 2008;38:1231–1235. doi: 10.1002/mus.21094. [DOI] [PubMed] [Google Scholar]
- Zhang W, Zhong W, Yang M, Shi J, Guowei L, Ma Q. Evaluation of the clinical efficacy of multiple lower-extremity nerve decompression in diabetic peripheral neuropathy. Br J Neurosurg. 2013;27:795–799. doi: 10.3109/02688697.2013.798854. [DOI] [PubMed] [Google Scholar]
- Zhong W, Zhang W, Zheng X, Li S, Shi J. The high-resolution ultrasonography and electrophysiological studies in nerve decompression for ulnar nerve entrapment at the elbow. J Reconstr Microsurg. 2012;28:345–348. doi: 10.1055/s-0032-1313766. [DOI] [PubMed] [Google Scholar]


