Abstract
Objective:
To investigate the association between a low-risk lifestyle and risk of stroke.
Methods:
The study population comprised 31,696 women, in the population-based Swedish Mammography Cohort who at baseline had completed a questionnaire about diet and lifestyle and were free from cardiovascular disease and cancer. We defined a low-risk lifestyle as a healthy diet (top 50% of a Recommended Food Score), moderate alcohol consumption (5–15 g/d), never smoking, physically active (walking/bicycling ≥40 min/d and exercise ≥1 h/wk), and body mass index below 25 kg/m2. Stroke cases were identified from the Swedish National Patient Register and the Swedish Cause of Death Register.
Results:
We ascertained 1,554 incident stroke cases, including 1,155 cerebral infarctions, 246 hemorrhagic strokes, and 153 unspecified strokes during 10.4 years of follow-up. The risk of stroke, in particular cerebral infarction, decreased steadily with increasing number of low-risk lifestyle factors. Compared with no low-risk factors, the multivariable relative risks (95% confidence interval) of cerebral infarction across increasing number of low-risk factors (1–5) were 0.72 (0.56–0.93), 0.67 (0.52–0.85), 0.57 (0.44–0.74), 0.54 (0.40–0.73), and 0.38 (0.20–0.73).
Conclusions:
These findings indicate that a low-risk lifestyle can substantially reduce the risk of stroke, especially cerebral infarction.
Stroke is a major cause of disability and mortality. Because the consequences of stroke are usually devastating and irreversible, primary prevention is of great importance. Hypertension is a strong and well-documented risk factor for stroke.1 Diet, alcohol consumption, smoking, physical activity, and adiposity can modify blood pressure and thus the risk of stroke.1,2 Few studies have examined the combined effect of a low-risk lifestyle on the incidence of stroke.3–6
The objective of the present study was to examine the combined effect of multiple low-risk lifestyle factors (healthy diet,7 moderate alcohol consumption, never smoking, physically active, and healthy body weight) on incidence of total stroke and stroke types in a population-based prospective cohort of Swedish women.
METHODS
Study population.
For the present study, we used data from the Swedish Mammography Cohort, which has been described in detail previously.8 Briefly, in the autumn of 1997, 39,227 women who resided in Uppsala and Västmanland counties, central Sweden, and were born between 1914 and 1948 completed a 350-item questionnaire concerning diet and lifestyle.
Standard protocol approvals, registrations, and patient consents.
The Regional Ethical Review Board at Karolinska Institutet in Stockholm, Sweden, approved this study. Return of the completed questionnaire was considered to imply informed consent.
Assessment of lifestyle factors.
At baseline in 1997, all participants of the Swedish Mammography Cohort completed a self-administered questionnaire that solicited information on education, body weight, height, smoking, physical activity, use of aspirin, history of hypertension and diabetes, family history of myocardial infarction before the age of 60 years, alcohol consumption, and diet. Participants indicated how many minutes or hours per day they had walked/bicycled (almost never, <20 min/d, 20–40 min/d, 40–60 min/d, 1–1.5 h/d, or ≥1.5 h/d) as well as how many hours per week they had exercised (<1, 1, 2–3, 4–5, or ≥5 h/wk) in the last year. Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared. Total alcohol (ethanol) intake was calculated by multiplying the reported frequency of consumption of beer, wine, and liquor by the amount consumed at each occasion.
Dietary intake was assessed by using a 96-item, validated9 food-frequency questionnaire. Participants were asked to indicate how often they had consumed various foods and food items during the previous year, with 8 predefined frequency categories (0, 1–3/mo, 1–2/wk, 3–4/wk, 5–6/wk, 1/d, 2/d, ≥3/d). For frequently consumed foods, such as dairy foods and bread, participants were asked to report the number of servings, per day or per week, they consumed of that food. A diet with a variety of healthy foods was defined by a Recommended Food Score (RFS), which is a way to define the overall diet quality by separating “healthy” from “less healthy” foods based on dietary guidelines and present knowledge.10 The RFS was developed by Kant et al.11 to measure dietary diversity in the National Health and Nutrition Examination Survey and adapted for the food-frequency questionnaire used in our study.10,12 In brief, the RFS included foods with a beneficial effect on cardiovascular health,13–15 i.e., fruits (apples/pears, citrus fruits, bananas, and berries), vegetables (cabbage, cauliflower, broccoli/Brussels sprouts, lettuce/green salad, spinach, carrots, beetroots, tomatoes/tomato juice, green peas, sweet pepper, and mixed vegetables), legumes, nuts, low-fat dairy foods (reduced-fat milk and yogurt), whole grain foods (whole grain bread, crisp/hard bread, oatmeal), and fish (cod/saithe/fish fingers, herring/mackerel, salmon/whitefish/char). A food score of 1 (summing up to a maximum of 25) was assigned for one or more servings per week of any of 2 reduced-fat dairy foods, whole grain bread, and crisp/hard bread. For the other food items (fruits, vegetables, legumes, nuts, oatmeal, and fish), a food score was assigned if the consumption frequency was at least 1 to 3 times/mo. We also calculated a Non-RFS (NRFS), based on 21 less healthy food items, including red meat (beef/veal, pork, minced meat, liver/kidney), processed meat (ham/salami/processed meat cuts, sausage/hot dogs, blood sausage, liver paté), full-fat dairy foods (full-fat milk, cheese, ice cream, cream), spaghetti/macaroni, white bread, fried potatoes, French fries, potato crisps, solid fats, sugar, sweets, and buns/cookies.10
Definition of low-risk lifestyle.
We considered 5 lifestyle factors, as previously proposed,3,4,16 for our low-risk group. The 5 factors included diet, alcohol consumption, cigarette smoking, physical activity, and BMI. We created a binary variable for each lifestyle factor. The participant received 1 if she met the criteria for low risk and 0 otherwise. A low-risk diet was defined as an RFS in the top 50% of the distribution in the cohort (score ≥21), based on results from our previous study on RFS and stroke risk.7 We defined moderate alcohol consumption as an intake between 5 and 15 g/d, corresponding to approximately 3 to 9 standard drinks (12 g alcohol/drink) per week. For smoking, low risk was defined as never smoking. A low-risk physical activity behavior was considered to include both low to moderate activities (walking/bicycling ≥40 min/d) and more vigorous activities (exercise ≥1 h/wk), prespecified according to previous use in a study of lifestyle factors and myocardial infarction in this cohort.16 A healthy body weight was defined as BMI below 25 kg/m2.15
Ascertainment of stroke cases and follow-up.
Information on dates of stroke diagnoses and dates of death was obtained by linkage of the study population with the Swedish National Patient Register and the Swedish Cause of Death Register. We classified stroke types according to ICD-10: cerebral infarction (code I63), intracerebral hemorrhage (I61), subarachnoid hemorrhage (I60), and unspecified stroke (I64). Unspecified strokes were included in analyses of total strokes.
Study population for analyses.
We excluded participants with a missing or an erroneous National Registration Number (n = 243), those with a previous diagnosis (in the Swedish registries) of cancer (n = 1,811) or cardiovascular disease (stroke, ischemic heart disease, angina, and heart failure; n = 2,492), and those who died before start of follow-up (January 1, 1998; n = 26). In addition, we excluded women with extreme values for total energy intake (i.e., 3 SDs from the loge-transformed mean energy intake; n = 405) and those with missing data on the exposure variables (n = 2,554). After exclusions, 31,696 women aged 49 to 83 years (SD 8.9 years) remained for analysis.
Statistical analysis.
Follow-up time for each woman was calculated from January 1, 1998 to the date of diagnosis of stroke, date of death, or December 31, 2008, whichever occurred first. We used Cox proportional hazards regression models (age as time scale) to estimate relative risks (RRs) with corresponding 95% confidence intervals (CIs). Entry time was defined as a woman's age in months at start of follow-up, and exit time was defined as a woman's age (in months) at the date of stroke diagnosis or censoring. In addition to age, the multivariable models were controlled for educational level (less than high school, high school, or university), use of aspirin (never, 1–6 tablets/wk, or ≥7 tablets/wk), diabetes (yes or no), atrial fibrillation (yes or no), family history of myocardial infarction before the age of 60 years (yes or no), total energy intake (continuous), and NRFS (quintiles). The individual low-risk factors were mutually adjusted. We did not control for history of hypertension and high blood cholesterol levels in the primary model because these factors are potential intermediates of the relation between a low-risk lifestyle and stroke risk. In a sensitivity analysis, we removed women with diabetes or a diagnosis of atrial fibrillation before baseline. Schoenfeld residuals were used to test the proportional hazards assumption; no violation of the assumption was observed.
We conducted analyses stratified by history of hypertension and age (split at the median age in the cohort, i.e., <60 years or ≥60 years) to evaluate whether these variables modified the relation between a low-risk lifestyle and stroke risk. Tests for interaction were conducted by using the likelihood ratio test. We performed all statistical analyses in SAS (version 9.2; SAS Institute, Cary, NC). Two-tailed p values <0.05 were considered statistically significant.
RESULTS
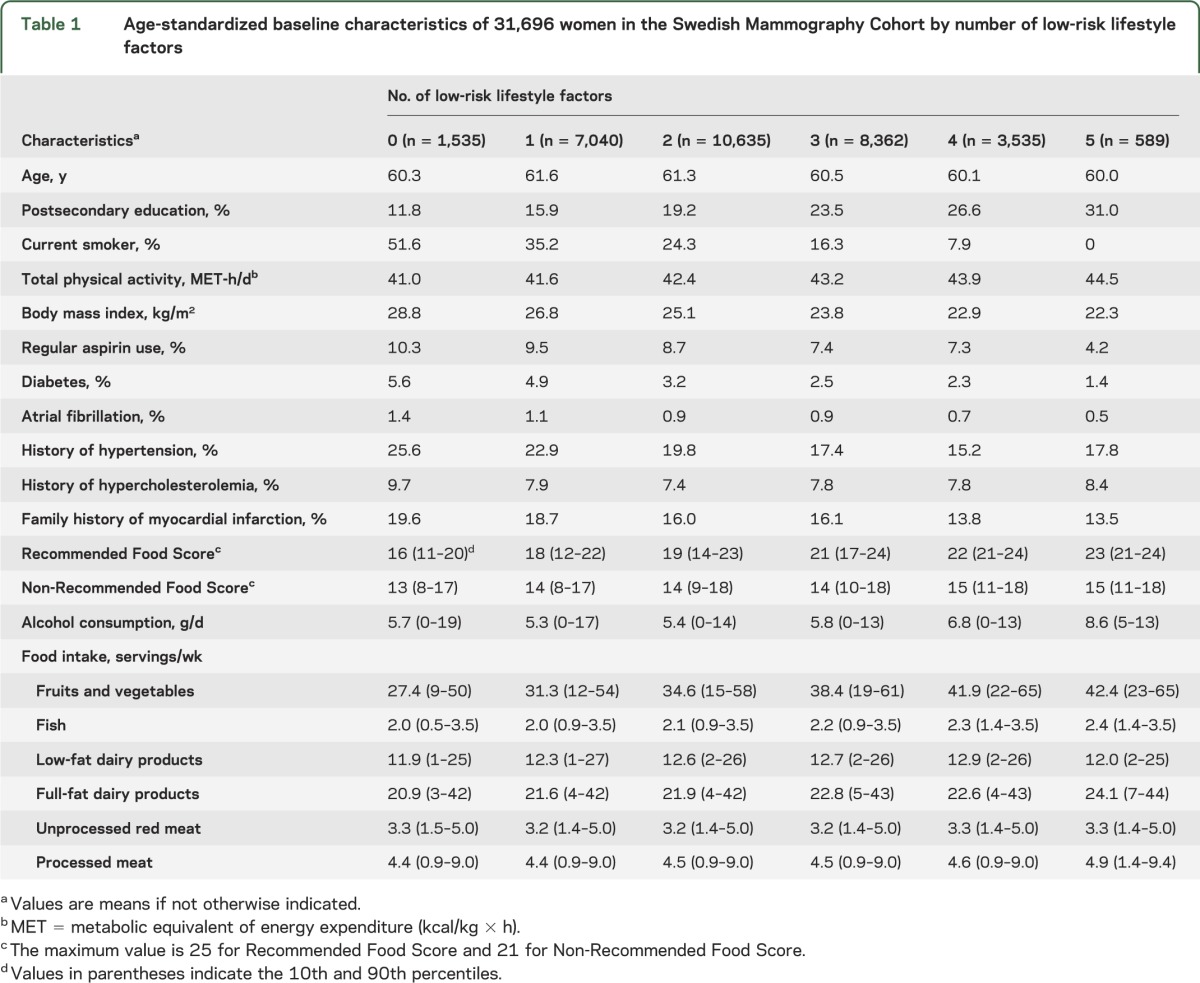
Baseline characteristics of the study population by number of low-risk lifestyle factors are presented in table 1. Compared with women with no low-risk lifestyle factors, those with all 5 low-risk factors were much more likely to have a postsecondary education but less likely to have a family history of myocardial infarction. As expected, those with all 5 low-risk factors consumed more alcohol, had higher physical activity level, had lower BMI, and were less likely to have diabetes, atrial fibrillation, and hypertension than those with no low-risk factors.
Table 1.
Age-standardized baseline characteristics of 31,696 women in the Swedish Mammography Cohort by number of low-risk lifestyle factors
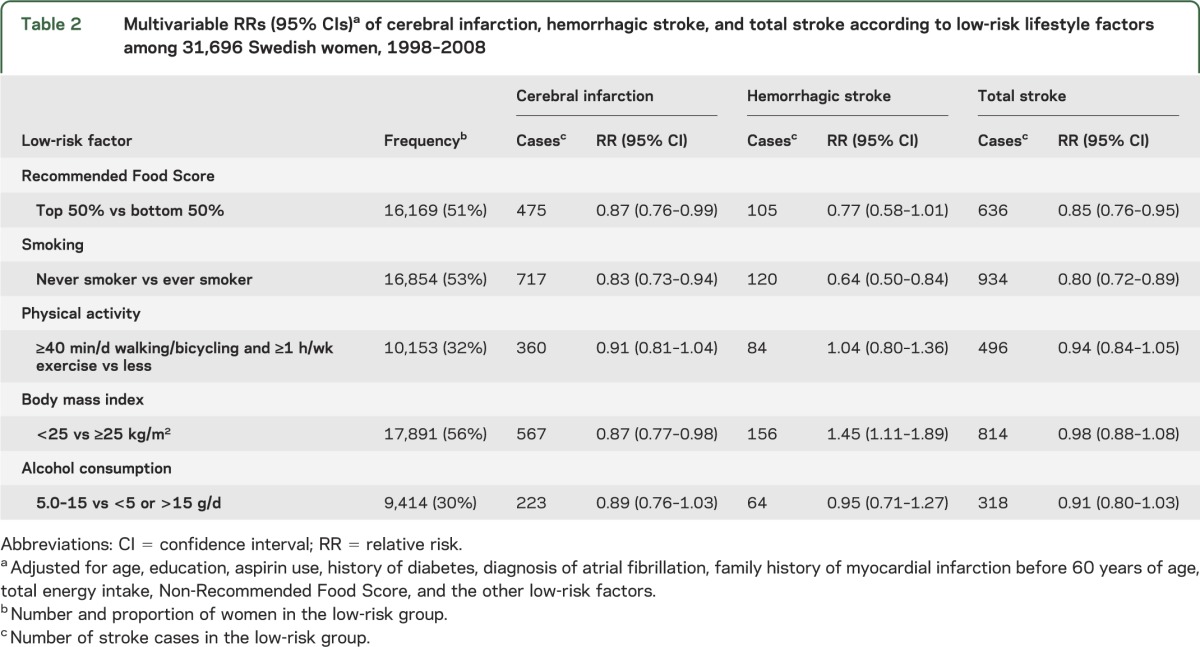
During a mean follow-up of 10.4 years (327,070 person-years), we ascertained 1,554 cases of stroke, including 1,155 cerebral infarctions, 246 hemorrhagic strokes (157 intracerebral hemorrhages and 89 subarachnoid hemorrhages), and 153 unspecified strokes. All 5 components of the low-risk lifestyle were inversely associated with risk of cerebral infarction, although only the associations with low-risk diet, never smoking, and BMI reached statistical significance (table 2). The reduction in cerebral infarction risk ranged from 9% for physical activity to 17% for never smoking. Only a low-risk diet and never smoking were inversely associated with risk of total stroke and hemorrhagic stroke. In contrast, a BMI <25 kg/m2 was associated with an increased risk of hemorrhagic stroke, both intracerebral hemorrhage (RR = 1.44; 95% CI, 1.04–2.01) and subarachnoid hemorrhage (RR = 1.46; 95% CI, 0.94–2.27).
Table 2.
Multivariable RRs (95% CIs)a of cerebral infarction, hemorrhagic stroke, and total stroke according to low-risk lifestyle factors among 31,696 Swedish women, 1998–2008
The risk of cerebral infarction and total stroke decreased steadily with increasing number of low-risk lifestyle factors (figure 1). Compared with women with no low-risk lifestyle factors (4.8% of the study population), those with all 5 low-risk factors (1.9%) had a 62% lower risk of cerebral infarction and a 54% lower risk of total stroke. Further adjustment for potential intermediates, including history of hypertension and high blood cholesterol, did not alter the results. None of the findings changed appreciably when we excluded women with diabetes (RR = 0.37; 95% CI, 0.19–0.72 for cerebral infarction) or atrial fibrillation (RR = 0.40; 95% CI, 0.21–0.75 for cerebral infarction). The association between a low-risk lifestyle and risk of cerebral infarction or total stroke was not modified by history of hypertension or age (all pinteraction ≥0.17). We observed no association between number of low-risk lifestyle factors and hemorrhagic stroke. The multivariable RRs (95% CI) of hemorrhagic stroke for increasing number of low-risk lifestyle factors (1–5), compared with 0 lifestyle factors, were 1.14 (0.58–2.24), 1.32 (0.69–2.54), 0.95 (0.48–1.88), 1.06 (0.50–2.22), and 0.77 (0.21–2.81). When we removed BMI, which was positively associated with hemorrhagic stroke, the multivariable RRs (95% CI) for increasing number of low-risk lifestyle factors (1–4) were 0.87 (0.58–1.29), 0.60 (0.42–0.97), 0.60 (0.37–0.99), and 0.63 (0.26–1.51).
Figure 1. Relative risksa with 95% confidence interval of cerebral infarction (A) and total stroke (B) according to number of low-risk lifestyle factorsb among 31,696 Swedish women, 1998–2008.
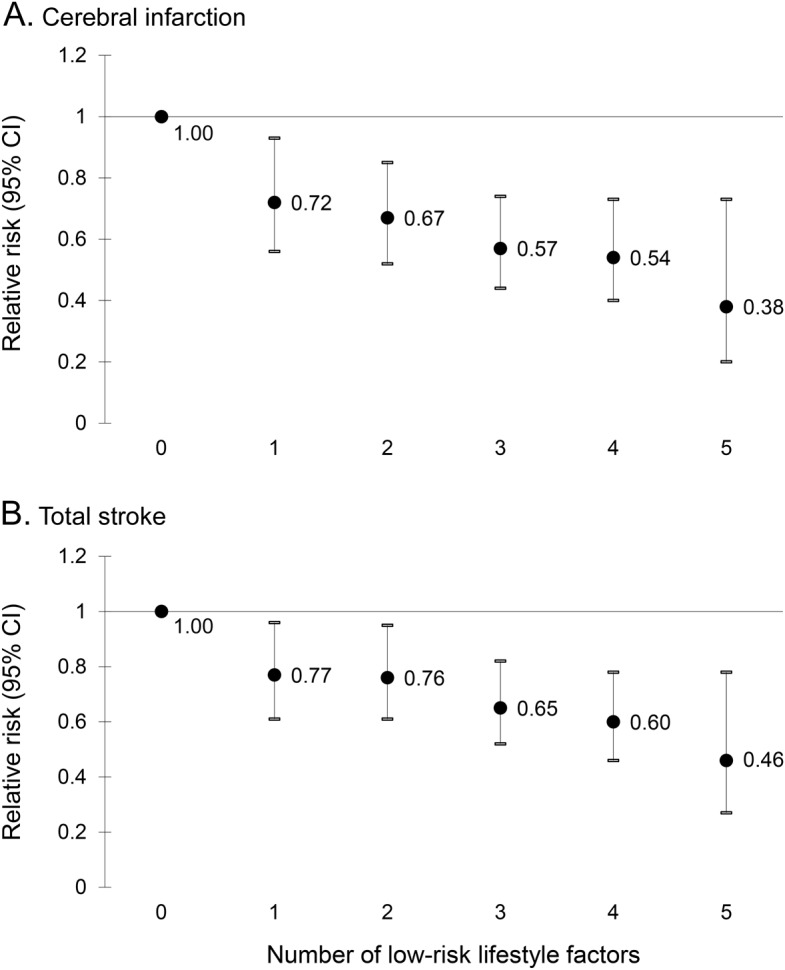
a Adjusted for age, education, aspirin use, history of diabetes, diagnosis of atrial fibrillation, family history of myocardial infarction before 60 years of age, total energy intake, and Non-Recommended Food Score. b Low-risk factors was defined as scoring within the top 50% of a Recommended Food Score, moderate alcohol consumption (5–15 g/d), never smoking, physically active (≥40 min/d of walking/bicycling and ≥1 h/wk of exercise), and BMI <25 kg/m2. Compared with the reference group with no low-risk factors (4.8% of the study population), the adjusted relative risks (95% confidence interval [CI]) of cerebral infarction across increasing number of low-risk factors (1–5) were 0.72 (0.56–0.93), 0.67 (0.52–0.85), 0.57 (0.44–0.74), 0.54 (0.40–0.73), and 0.38 (0.20–0.73). The corresponding relative risks (95% CI) for total stroke were 0.77 (0.61–0.96), 0.76 (0.61–0.95), 0.65 (0.52–0.82), 0.60 (0.46–0.78), and 0.46 (0.27–0.78).
The associations between different combinations of the low-risk lifestyle factors and risk of cerebral infarction and total stroke are shown in figure e-1, A and B, on the Neurology® Web site at Neurology.org. All combinations with the exception of physical activity and alcohol consumption were associated with a statistically significant lower risk of cerebral infarction, and there was little diversity in the strengths of the associations for different combinations.
DISCUSSION
In this cohort of women, a low-risk lifestyle was associated with a considerably lower risk of cerebral infarction and total stroke, but not hemorrhagic stroke, and the risk decreased with increasing number of low-risk lifestyle factors. Those with all 5 low-risk lifestyle factors had a 62% lower risk of cerebral infarction compared with women with no low-risk factors.
To our knowledge, this is the first study to report results on different combinations of low-risk lifestyle factors. For cerebral infarction, there were no substantial differences in the strength of the inverse associations for different combinations.
Our results for cerebral infarction and total stroke are similar to those from a prospective study of US nurses and health professionals.4 That study found that women with a low-risk lifestyle (2% of participants), defined as a scoring within the top 40% of a healthy diet score, modest alcohol consumption (5–15 g/d), not smoking, 30 min/d of moderate activity, and a BMI <25 kg/m2, had an 81% lower risk of cerebral infarction. Likewise, in the Health Professionals Follow-Up Study, such a low-risk pattern (4% of participants) was associated with a 69% lower risk of the disease.4 In the Women's Health Study, women with 17 to 20 health index points (4.7% of women), based on 5 low-risk lifestyle factors (healthy diet, never smoking, 4–10.5 drinks/wk of alcohol, exercise ≥4 times/wk, and a BMI <22 kg/m2), had a 71% reduced risk of cerebral infarction compared with those with 0 to 4 health index points (4.3% of women).3 The association between 5 healthy lifestyle factors and risk of stroke was also examined in a cohort of 36,686 Finnish women and men.5 In that study, participants with all 5 low-risk lifestyle factors (vegetable consumption ≥3 times/wk, alcohol intake ≥140 g/wk in women and ≥210 g/wk in men, never smoker, moderate or high physical activity, and BMI <25 kg/m2) had a 70% lower risk of cerebral infarction compared with those with no low-risk factors.5 A healthy lifestyle, based on 3 food groups (fruits, fish, and milk) and 5 other factors (alcohol consumption, physical activity, BMI, smoking, and sleep duration), was associated with a similar reduction in stroke in a cohort of Japanese women and men.6
We observed no association between a healthy lifestyle (all 5 low-risk lifestyle factors) and risk of hemorrhagic stroke. Because of the relatively small number of hemorrhagic stroke cases (n = 246), the CIs for the risk estimates were wide and overlapped with those for cerebral infarction. We can therefore not exclude a potential association. When we removed BMI, which was positively associated with risk of hemorrhagic stroke, we found an inverse association with a low-risk lifestyle. In 2 previous studies that have reported results on a combination of low-risk lifestyle factors, including BMI, and risk of hemorrhagic stroke, an inverse association was observed in a cohort of Finnish women and men5 but not in the Women's Health Study.3
Regarding specific lifestyle factors, cigarette smoking is a well-established risk factor for both cerebral infarction and hemorrhagic stroke.1,2 In this study, smoking was the lifestyle factor that was most strongly associated with total stroke and cerebral infarction. For alcohol, there appears to be a J-shaped relationship between alcohol consumption and risk of cerebral infarction and hemorrhagic stroke among women.1,2 A meta-analysis showed that an alcohol intake up to 46 g/d had a protective effect against cerebral infarction morbidity in women.2 The greatest reduction in risk of cerebral infarction was observed at a consumption level of approximately 1 alcoholic drink/d (corresponding to 8 g [UK] to 13.6 g [Canada] of alcohol).2 In our cohort of middle-aged and elderly women, alcohol consumption was low and we observed a statistically nonsignificant reduction in stroke risk in women who consumed 5 to 15 g/d of alcohol. Both overweight (BMI 25–30 kg/m2) and obesity (BMI ≥30 kg/m2) are associated with increased risk of cerebral infarction, whereas only obesity seems to increase hemorrhagic stroke risk.17 In a meta-analysis of 25 prospective studies, the RR for cerebral infarction was 1.22 (95% CI, 1.05–1.41) for overweight and 1.64 (95% CI, 1.36–1.99) for obesity, whereas the RR for hemorrhagic stroke was 1.01 (95% CI, 0.88–1.17) and 1.24 (95% CI, 0.99–1.54), respectively.17 As in the meta-analysis, we observed that a healthy body weight (compared with overweight/obesity) was inversely associated with risk of cerebral infarction. However, we observed an inverse association between overweight and risk of hemorrhagic stroke. Physical activity and exercise have been inversely associated with stroke in some but not all studies in women.3,18 We observed a nonsignificant inverse association between physical activity and cerebral infarction. As a measure of an overall healthy diet, we used RFS, which is inversely associated with risk of stroke in the present cohort.7
This study has several strengths, including a prospective and population-based design, large number of cases of cerebral infarction and total stroke, information on potential confounders, and the almost complete follow-up of participants by linkage with population-based Swedish registries. Because this study was population-based and well represented the source population, the results should be generalizable to all women. The observational design is a limitation of this study. Hence, we cannot exclude the possibility of residual confounding. Another limitation is that diet and lifestyle were self-reported and based on a single assessment at baseline. Therefore, some measurement error in the exposure assessment is inevitable.
Our findings based on a population-based cohort of women indicate that a low-risk diet and lifestyle can substantially reduce the risk of stroke, especially cerebral infarction.
Supplementary Material
GLOSSARY
- BMI
body mass index
- CI
confidence interval
- ICD-10
International Classification of Diseases, tenth revision
- NRFS
Non-Recommended Food Score
- RFS
Recommended Food Score
- RR
relative risk
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
The contributions of the authors to the manuscript were as follows: study concept and design (S.C.L., A.Å., A.W.), data collection (A.W.), statistical analyses (S.C.L.), manuscript writing (S.C.L.), interpretation of results (S.C.L., A.Å., A.W.), and critical revision of manuscript (S.C.L., A.Å., A.W.). S.C.L. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
STUDY FUNDING
This study was supported by research grants from the Swedish Research Council for Health, Working Life and Welfare (Forte) and the Swedish Research Council. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the article.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Goldstein LB, Bushnell CD, Adams RJ, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011;42:517–584. [DOI] [PubMed] [Google Scholar]
- 2.Patra J, Taylor B, Irving H, et al. Alcohol consumption and the risk of morbidity and mortality for different stroke types: a systematic review and meta-analysis. BMC Public Health 2010;10:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kurth T, Moore SC, Gaziano JM, et al. Healthy lifestyle and the risk of stroke in women. Arch Intern Med 2006;166:1403–1409. [DOI] [PubMed] [Google Scholar]
- 4.Chiuve SE, Rexrode KM, Spiegelman D, Logroscino G, Manson JE, Rimm EB. Primary prevention of stroke by healthy lifestyle. Circulation 2008;118:947–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y, Tuomilehto J, Jousilahti P, Wang Y, Antikainen R, Hu G. Lifestyle factors on the risks of ischemic and hemorrhagic stroke. Arch Intern Med 2011;171:1811–1818. [DOI] [PubMed] [Google Scholar]
- 6.Eguchi E, Iso H, Tanabe N, et al. Healthy lifestyle behaviours and cardiovascular mortality among Japanese men and women: the Japan Collaborative Cohort Study. Eur Heart J 2012;33:467–477. [DOI] [PubMed] [Google Scholar]
- 7.Larsson SC, Åkesson A, Wolk A. Overall diet quality and risk of stroke: a prospective cohort study in women. Atherosclerosis 2014;233:27–29. [DOI] [PubMed] [Google Scholar]
- 8.Larsson SC, Virtamo J, Wolk A. Red meat consumption and risk of stroke in Swedish women. Stroke 2011;42:324–329. [DOI] [PubMed] [Google Scholar]
- 9.Messerer M, Johansson SE, Wolk A. The validity of questionnaire-based micronutrient intake estimates is increased by including dietary supplement use in Swedish men. J Nutr 2004;134:1800–1805. [DOI] [PubMed] [Google Scholar]
- 10.Michels KB, Wolk A. A prospective study of variety of healthy foods and mortality in women. Int J Epidemiol 2002;31:847–854. [DOI] [PubMed] [Google Scholar]
- 11.Kant AK, Schatzkin A, Graubard BI, Schairer C. A prospective study of diet quality and mortality in women. JAMA 2000;283:2109–2115. [DOI] [PubMed] [Google Scholar]
- 12.Messerer M, Håkansson N, Wolk A, Akesson A. Dietary supplement use and mortality in a cohort of Swedish men. Br J Nutr 2008;99:626–631. [DOI] [PubMed] [Google Scholar]
- 13.Hu FB, Willett WC. Optimal diets for prevention of coronary heart disease. JAMA 2002;288:2569–2578. [DOI] [PubMed] [Google Scholar]
- 14.WHO. Diet, Nutrtion and the Prevention of Chronic Diseases. Geneva: World Health Organization; 2003. [Google Scholar]
- 15.Lichtenstein AH, Appel LJ, Brands M, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 2006;114:82–96. [DOI] [PubMed] [Google Scholar]
- 16.Åkesson A, Weismayer C, Newby PK, Wolk A. Combined effect of low-risk dietary and lifestyle behaviors in primary prevention of myocardial infarction in women. Arch Intern Med 2007;167:2122–2127. [DOI] [PubMed] [Google Scholar]
- 17.Strazzullo P, D'Elia L, Cairella G, Garbagnati F, Cappuccio FP, Scalfi L. Excess body weight and incidence of stroke: meta-analysis of prospective studies with 2 million participants. Stroke 2010;41:e418–e426. [DOI] [PubMed] [Google Scholar]
- 18.Li J, Siegrist J. Physical activity and risk of cardiovascular disease: a meta-analysis of prospective cohort studies. Int J Environ Res Public Health 2012;9:391–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


