Abstract
Objective
We examined the concurrent and lagged effects of registered nurse (RN) turnover on unit-acquired pressure ulcer rates and whether RN staffing mediated the effects.
Data Sources/Setting
Quarterly unit-level data were obtained from the National Database of Nursing Quality Indicators for 2008 to 2010. A total of 10,935 unit-quarter observations (2,294 units, 465 hospitals) were analyzed.
Methods
This longitudinal study used multilevel regressions and tested time-lagged effects of study variables on outcomes.
Findings
The lagged effect of RN turnover on unit-acquired pressure ulcers was significant, while there was no concurrent effect. For every 10 percentage-point increase in RN turnover in a quarter, the odds of a patient having a pressure ulcer increased by 4 percent in the next quarter. Higher RN turnover in a quarter was associated with lower RN staffing in the current and subsequent quarters. Higher RN staffing was associated with lower pressure ulcer rates, but it did not mediate the relationship between turnover and pressure ulcers.
Conclusions
We suggest that RN turnover is an important factor that affects pressure ulcer rates and RN staffing needed for high-quality patient care. Given the high RN turnover rates, hospital and nursing administrators should prepare for its negative effect on patient outcomes.
Keywords: Registered nurse turnover, nurse staffing, inpatient outcomes, pressure ulcers
Over the past decade, a shortage of registered nurses (RNs) has been one of the most critical concerns for health care institutions, particularly hospitals (Spetz and Given 2003; Buerhaus, Auerbach, and Staiger 2009). The Bureau of Health Professions of the Health Resources and Services Administration estimated that the RN shortage would grow from 6 percent in 2002 to 20 percent by 2020 (DHHS 2002). Researchers proposed that high turnover and intent of RNs to leave the profession would further worsen the future shortage (Aiken et al. 2001; HSM Group 2002). Since 2007, however, when the U.S. economy slipped into a severe recession, immediate concern over the RN shortage abated. During the recession, RN employment and retention sharply increased compared with other professions, virtually ending the decade-long shortage of hospital RNs (Staiger, Auerbach, and Buerhaus 2012). Nevertheless, workforce researchers expect that the absence of an RN shortage may be short-lived and that increases in RN turnover and a shortage will reemerge once the economy has recovered (Buerhaus, Auerbach, and Staiger 2009; Staiger, Auerbach, and Buerhaus 2012). Thus, policy makers, administrators, and researchers must closely monitor RN turnover because it affects stability in the nursing workforce and threatens the consistency and quality of patient care.
Past studies have identified an array of complex and multifaceted factors associated with nurse turnover; however, most of them have focused on the determinants of nurse turnover such as organizational factors, management style, workload, burnout, and pay/benefits (O'Brien-Pallas et al. 2006; Hayes et al. 2012). Few studies have examined the consequences of nurse turnover, particularly its effect on the quality of hospital patient care.
Many researchers assume that nurse turnover will negatively affect the quality of patient care that is provided by nurses (Shortell et al. 1994; Tai, Bame, and Robinson 1998; O'Brien-Pallas et al. 2006). However, this assumption has been supported by only a few empirical studies that examined the relationship between nurse turnover and patient outcomes (Leiter, Harvie, and Frizzell 1998; O'Brien-Pallas et al. 2010; VHA 2002). Moreover, their findings could be challenged because the studies were based mostly on small sample sizes, used data from a narrow set of unit types or a limited number of hospital settings, analyzed facility-level data that might not account for differences in turnover rates among unit types, used a cross-sectional design that might make it difficult to account for changes in nurse turnover and outcomes over time, or considered turnover intention as a proxy for actual turnover instead of testing the direct effect of actual turnover on patient outcomes (Hayes et al. 2012). To address these concerns, therefore, we longitudinally examined the association between turnover of nurses, specifically RNs, and the patient outcome of pressure ulcers at the unit level.
Conceptual Framework
Figure1 is a longitudinal framework showing relationships among RN turnover, pressure ulcers, and RN staffing, which is relevant to workforce adequacy as well as care quality, and controlling for unit and hospital characteristics. Our longitudinal framework incorporates Granger causality between variables of interest, indicating that the lags of explanatory variables can be helpful to predict the outcome variable even though the relationships may not represent actual causality (Greene 2012).
Figure 1.
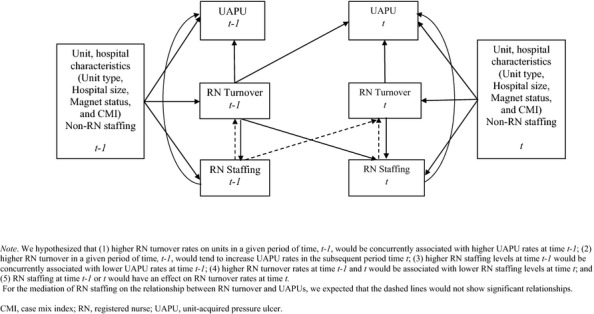
Conceptual Framework of RN Turnover, RN Staffing, and Unit-acquired Pressure Ulcers Showing the Combined Hypotheses
RN Turnover
Nurse turnover occurs when a nurse leaves a hospital (external turnover) or transfers from one position to another within a hospital (internal turnover) (Jones 1990; LeVasseur et al. 2009). External turnover is usually attributable to a nurse employee who voluntarily seeks a change of employment; internal turnover may be voluntary or involuntary when triggered by employer mandates such as hospital restructuring or downsizing. In the literature, definitions and measures of turnover are inconsistent. O'Brien-Pallas et al. (2006, 2010) included internal and external departures for voluntary reasons but excluded turnover due to involuntary reasons such as dismissal, forced retirement, layoff, and medical disability. Some researchers included external turnover while excluding transfers within a facility (Jones 2005; Beecroft, Dorey, and Wenten 2008). Other researchers investigated total turnover attributable to both internal and external turnover for both voluntary and involuntary reasons (Baernholdt and Mark 2009; LeVasseur et al. 2009; Bae, Mark, and Fried 2010). Considering these diverse operational definitions, we determined that total turnover may more appropriately capture the overall effect on the quality of patient care in that, whatever the reasons, nurse turnover reduces the stability, efficiency, and productivity of the nursing workforce in providing patient care on nursing units (Jones 1990, 2005).
Despite serious concerns about quality of patient care in units with frequent turnover, only a few studies have identified the detrimental effect of nurse turnover or intent to leave on patient outcomes. Leiter, Harvie, and Frizzell (1998), using survey data from 605 patients and 711 nurses (82.8 percent RNs) in two hospitals, found that patients were less satisfied with nursing care when the nurses on their units felt exhausted and planned to leave. Bae, Mark, and Fried (2010) examined possible mechanisms underlying the turnover and outcome relationship and found that workgroup learning was negatively related to RN turnover and medication errors. Only two cross-sectional studies, using data from multiple hospitals, examined the direct relationship between turnover and patient outcomes (O'Brien-Pallas et al. 2010; VHA 2002). These studies showed that higher rates of nurse turnover were associated with longer patient stays, greater risk-adjusted patient mortality rates (VHA 2002), and more medical errors (O'Brien-Pallas et al. 2010). Based on these study findings, we hypothesized that higher RN turnover rates on units would be concurrently associated with poorer patient outcomes (Hypothesis 1, H1) (see Figure1).
RN turnover may also have a lagged effect on patient outcomes; however, past studies offer little empirical evidence linking RN turnover with patient outcomes in a longitudinal design. When nurses leave a unit, those who remain behind can become overburdened with patient care until vacant positions are filled and new staff members are trained (Tai, Bame, and Robinson 1998; O'Brien-Pallas et al. 2006). Newly hired or transferred nurses usually perform less efficiently until fully integrated into the new environment. Thus, higher RN turnover on units may gradually increase residual staff's workloads and nurse burnout, diminish workgroup collaboration, and adversely affect patient outcomes during transition periods. Based on this concern, units with higher RN turnover in a given period of time, t − 1, would tend to have poorer patient outcomes in the subsequent time period, t (H2).
RN Staffing
As found in previous research, lower RN staffing levels are associated with higher rates of mortality and more adverse patient outcomes (Aiken et al. 2002; Needleman et al. 2002; Blegen et al. 2011), and high RN turnover rates can inhibit the retention of a sufficient number of RNs to provide safe and high-quality patient care (Gardner et al. 2007; Hayes et al. 2012). Thus, it is possible that the relationship between RN turnover and patient outcomes is mediated by RN staffing. For such mediation, we hypothesized that higher RN staffing levels would be concurrently associated with better patient outcomes (H3), and higher RN turnover rates at time t − 1 and t would be associated with lower RN staffing levels at time t (H4). Although we tested the possibility of RN staffing mediation while hypothesizing H4, little is known about whether RN staffing affects RN turnover, or vice versa. Based on this concern, we also tested whether RN staffing at time t − 1 or t would have an effect on RN turnover rates at time t (H5).
Hospital and Unit Characteristics
Hospital and unit characteristics, such as Magnet™ status, hospital size, teaching status, Medicare Case Mix Index (CMI), and unit type, have been used as important control variables in outcomes research (Aiken et al. 2002; Mark and Belyea 2009; Blegen et al. 2011). Magnet hospitals have shown better patient outcomes than non-Magnet hospitals (Lake et al. 2010). Teaching hospitals may provide better quality of care than non-teaching hospitals, adjusting for patient and hospital characteristics (Allison et al. 2000; Ayanian and Weissman 2002); however, teaching hospitals typically have more beds (Allison et al. 2000). Thus, teaching status and hospital size may be confounded with each other. CMI has been used as a proxy measure of hospital-level severity of patient illness, on the assumption that hospitals with more severe patients and a higher CMI level have more demand for nursing care and have poorer patient outcomes (Kovner et al. 2002; Mark and Harless 2010). Unit type was included in our models because rates of pressure ulcers, nurse staffing, and turnover typically differ by unit type.
While testing the hypotheses presented above after controlling for hospital and unit characteristics, we examined (1) the concurrent and lagged effects of RN turnover on pressure ulcer rates using longitudinal, unit-level data, and (2) whether the effects of RN turnover on pressure ulcer rates were mediated by RN staffing levels. As a patient outcome attributable to nursing care, pressure ulcers are an adverse patient condition that has yet to be studied in relation to nurse turnover. Pressure ulcers prolong hospital length of stay, increase in-hospital mortality and costs (Allman et al. 1999; Russo, Steiner, and Spector 2008), and represent one of the patient outcome indicators endorsed by the National Quality Forum (NQF 2004) for public reporting. In addition, pressure ulcers are among the hospital-acquired conditions ineligible for reimbursement by the Centers for Medicare and Medicaid Services (CMS 2012) and are a quality indicator measurable at the unit level.
Despite the important role of RNs in reducing pressure ulcers, the findings of previous studies have been inconsistent regarding the beneficial effect of RN staffing on pressure ulcer rates. Some researchers found a significant relationship between higher RN staffing and lower pressure ulcer rates (Blegen, Goode, and Reed 1998; Blegen et al. 2011), whereas other researchers reported no beneficial effect of staffing on pressure ulcers (Needleman et al. 2002; Cho et al. 2003). Our study using unit-level longitudinal analysis and accounting for RN turnover effects could provide a better understanding of the relationship between RN staffing and pressure ulcers.
Methods
Data Sources and Sample
This longitudinal, observational study used hospital administrative data obtained from the National Database of Nursing Quality Indicators (NDNQI®). Our sample included NDNQI member hospitals that reported data on nurse turnover and pressure ulcers for each quarter from 2008 through 2010. We limited our sample to four major types of units (step-down, medical, surgical, and medical-surgical combined) with adult patients. We excluded intensive care, rehabilitation, psychiatric, and obstetric units as these units provide specialized patient care. Unit-level data on nurse turnover, staffing, pressure ulcers, and unit characteristics were matched with NDNQI facility-level information on hospital characteristics. The final analytic sample included a multilevel panel of 10,935 unit-quarter observations (from 2,294 units in 465 hospitals from 47 states) that had values of turnover and pressure ulcers for the previous quarter (i.e., no missing values for the lagged variables).
Compared with 2010 American Hospital Association (AHA) survey data (6,268 hospitals, response rate about 85 percent), our sample differed in terms of hospital size, location, and Magnet status. Specifically, about 55 percent of hospitals in our sample had 200 staffed beds or less as compared with the 74 percent of hospitals in the AHA sample. Furthermore, our sample included more hospitals with Magnet designation (23 vs. 6 percent) and more hospitals located in metropolitan areas (83 vs. 65 percent) than the AHA sample. Most hospitals in our sample (88 percent) were not-for-profit as compared with the AHA sample (50 percent).
Measures
A pressure ulcer is a localized lesion of skin and/or underlying tissue resulting from pressure or pressure combined with shear (NPUAP/EPUAP 2009). Data on pressure ulcer prevalence, hospital-acquired pressure ulcers, and unit-acquired pressure ulcers are gathered quarterly by nursing staff in NDNQI-affiliated hospital units through direct inspection of the patient's skin. The NDNQI requires participating hospital staff to be trained in pressure ulcer identification and staging prior to collecting pressure ulcer data. Findings from two reliability studies on the NDNQI pressure ulcer indicator showed moderate to substantial agreement in pressure ulcer staging from direct inspection of the patient's skin (Kappa statistics of 0.60–0.68), moderate to near perfect agreement in pressure ulcer staging from web-based testing with pictures (Kappa statistics of 0.59–0.81), and near perfect agreement in pressure ulcer identification (pressure ulcer/not pressure ulcer) from web-based testing with pictures (Kappa statistics of 0.83–0.84) (Hart et al. 2006; Bergquist-Beringer et al. 2011). For this study, we used the NDNQI data on unit-acquired pressure ulcers that reflect the proximal point of nursing care services better than hospital-acquired pressure ulcers. A unit-acquired pressure ulcer was defined as a new pressure ulcer that developed after arrival on the hospital unit. We measured the proportion of patients with a unit-acquired pressure ulcer of any stage among patients surveyed on the units each quarter.
The NDNQI database includes information on nurse turnover at the unit level. We measured nurse turnover based on unit RNs who provide direct patient care for greater than 50 percent of their time. Average quarterly turnover rates were computed by dividing the total number of RNs on the unit who left their positions for any reason during a given quarter by the average number of RNs on the unit for the quarter.
Unit-level nurse staffing was measured as the number of nursing hours per patient day (HPPD). Only productive hours worked by staff who provided direct patient care for greater than 50 percent of their time were captured. We computed HPPDs for RN and non-RN staffing separately. Non-RN HPPD was calculated by aggregating hours provided by licensed practical nurses and unlicensed assistive personnel.
We included unit and hospital characteristics as control variables. The NDNQI identifies unit type by acuity level, overall age of the patient population, and type of service provided. Only adult step-down, medical, surgical, and medical-surgical units were included in the current study. Hospital size was defined by the number of staffed beds: small (<200 beds), medium (200–399 beds), and large (≥400 beds). Magnet hospitals were defined as those recognized by the American Nurses Credentialing Center's Magnet Recognition Program; non-Magnet hospitals were those that were not. Medicare CMI, which indicated the average diagnostic-related group weight for a hospital's Medicare patient volume, was used to differentiate hospital-level patient case mix.
Data Analysis
Descriptive statistics were used to examine distribution and trends in study variables for the 12-quarter period. We also fit multilevel logistic regression models to examine the effects of unit-level RN turnover and staffing on the odds of a patient having at least one unit-acquired pressure ulcer. Unit-specific and hospital-specific random intercepts were included in each model to account for the clustered structure of the data. We checked autocorrelation of the error term because regression estimates can be biased and inefficient when autocorrelation is present (Greene 2012). Based on results from the Wooldridge test, we confirmed no serial autocorrelation concern in our data. We also confirmed stationarity in our panel data using the Fisher test for unit roots.
While cross-sectional studies investigate concurrent associations between predictors and outcomes based on the assumption of strict exogeneity, under which there is no correlation between the predictors and error term in any time period (Mark, Harless, and McCue 2005), this strict exogeneity assumption can be violated for longitudinal data because changes in the explanatory variables may influence outcomes in the current and subsequent periods. In our models, along with the concurrent effect of RN turnover, we examined lagged effects to link RN turnover in the previous quarter with pressure ulcer outcomes for the current quarter. The correlation between the concurrent and lagged values of RN turnover was not high (r = 0.13). In addition, when we included concurrent and lagged RN turnover simultaneously in the regression model, the variance inflation factor was less than 2, indicating that multicollinearity was not a concern.
Similarly, a lagged effect may exist for RN staffing because the influence of inadequate RN staffing on patient outcomes may be delayed. However, the values of RN staffing were consistent over the study quarters with an extremely high correlation between concurrent and lagged RN staffing (r = 0.93). Thus, the lagged RN staffing was not included in our regression models.
Consequently, several models were created. We first regressed the unit-acquired pressure ulcer rate (UAPUijt) for nursing unit i in hospital j observed in quarter t on RN turnover rates in the previous quarter (Turnover ijt−1, a lagged variable of turnover) and current quarter (Turnoverijt, a concurrent variable of turnover) (Model 1). Subsequently, to test whether RN staffing mediated the relationship between RN turnover and unit-acquired pressure ulcers, we fit a second model (Model 2) with RN staffing in the current quarter (Staffingijt) added as a predictor to Model 1. We then fit a model examining a relationship between RN staffing and unit-acquired pressure ulcers without the effects of RN turnover (Model 3).
Additionally, we conducted multilevel regression analyses to determine whether RN turnover rates had an effect on RN staffing or vice versa. By doing that, we could check the role of RN staffing as a mediator in the relationships among turnover, staffing, and UAPUs. For the models regressing RN turnover on staffing, we chose Poisson models, which are commonly used to model count and rate data (McCullagh and Nelder 1989). The count of RN separations in the unit-quarter was assumed to follow the Poisson distribution, and we modeled the rate of turnover by including the count of RNs on the unit as an exposure variable. Because of a high correlation between concurrent and lagged RN staffing values, we fit two separate models, one regressing RN turnover on concurrent RN staffing and the other regressing RN turnover on lagged RN staffing. As in the models of turnover and staffing described above, unit and hospital intercepts were included to account for correlations among repeated measures.
Unit type, non-RN staffing, and hospital characteristics of Magnet status, hospital size, and CMI were included as control variables in all models. In our preliminary analysis, our data showed that teaching hospitals were relatively larger than nonteaching hospitals. We also found that teaching hospitals did not have significantly lower UAPU rates, whereas UAPU rates significantly differed by hospital size. For this reason, our regression models included only hospital size and excluded teaching status to reduce multicollinearity among control variables. In our preliminary findings, we observed an overall decreasing trend in UAPU rates during the study period, although the shape of this trend was not linear. For our regression models, we controlled for time-varying effects on UAPU rates using quadratic terms after testing and comparing linear as well as polynomial growth trends. All analyses were conducted using Stata version 12 (Stata Corporation, College Station, Texas, USA).
Results
Table 1 summarizes the hospital and unit characteristics. Most of the study units were medical-surgical (34.83 percent) and medical (25.89 percent) units. The distribution of hospital Magnet status and number of staffed beds (hospital size) were time-variant but fluctuated little over the study period. Hospital location, teaching status, ownership, and unit-type distributions were time-invariant.
Table 1.
Descriptive Summary of Hospital and Unit Characteristics over Twelve Quarters from 2008 to 2010
| Variables | n | % |
|---|---|---|
| Hospital characteristics (N = 465 Hospitals) | ||
| Magnet status* | ||
| Magnet | 106 | 22.80 |
| Nonmagnet | 359 | 77.20 |
| Hospital size* | ||
| Small (<200 beds) | 254 | 54.62 |
| Medium (200–399 beds) | 159 | 34.19 |
| Large (≥400 beds) | 52 | 11.18 |
| Teaching status | ||
| Teaching | 184 | 39.57 |
| Nonteaching | 281 | 60.43 |
| Location | ||
| Metropolitan | 384 | 82.58 |
| Nonmetropolitan | 81 | 17.42 |
| Ownership | ||
| Not-for-profit | 411 | 88.39 |
| Government | 25 | 5.38 |
| For-profit | 29 | 6.24 |
| Unit characteristics (N = 2,294 units) | ||
| Unit type | ||
| Step-down | 455 | 19.83 |
| Medical | 594 | 25.89 |
| Surgical | 446 | 19.44 |
| Combined medical-surgical | 799 | 34.83 |
| Mean | Standard Deviation | |
| Medicare case mix index | 1.47 | 0.24 |
Based on hospitals' most recent data from the study period.
Table 2 presents means and standard deviations of RN turnover, nurse staffing, and UAPU rates by unit types for the study period. The mean quarterly RN turnover rate across units was 5.81 percent. Step-down and medical units showed higher average turnover rates (6.14 and 6.01 percent, respectively) as compared with surgical (5.41 percent) and combined medical-surgical (5.72 percent) units. No increasing or decreasing trend over time was noted in average quarterly RN turnover. However, a small but steady increase in RN staffing levels was observed, whereas non-RN staffing levels slightly decreased over time. Overall, the rate of UAPUs gradually declined from the first quarter of 2008 through the fourth quarter of 2009, but then increased slightly.
Table 2.
Means and Standard Deviations for RN Turnover, Nurse Staffing, and Unit-acquired Pressure Ulcers by Unit Types from 2008 Quarter 1 through 2010 Quarter 4
| 2008 |
2009 |
2010 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Overall | |
| RN Turnover | |||||||||||||
| Step-down | 6.98 (8.16) | 5.85 (7.31) | 6.12 (8.29) | 5.07 (6.84) | 6.93 (8.61) | 5.08 (8.23) | 6.36 (7.27) | 5.20 (5.63) | 5.04 (5.88) | 6.34 (7.01) | 6.99 (7.11) | 6.85 (8.29) | 6.14 (7.36) |
| Medical | 6.82 (8.83) | 6.95 (9.47) | 7.09 (7.79) | 5.31 (6.82) | 4.78 (5.83) | 4.49 (5.75) | 5.93 (7.51) | 6.33 (9.12) | 5.35 (7.93) | 5.78 (6.18) | 7.20 (9.24) | 6.10 (5.97) | 6.01 (7.59) |
| Surgical | 5.72 (7.63) | 4.55 (6.33) | 6.31 (9.44) | 4.99 (7.22) | 5.21 (7.14) | 4.82 (6.20) | 5.33 (8.36) | 4.98 (5.82) | 4.32 (5.26) | 6.09 (7.16) | 6.22 (7.87) | 5.65 (7.12) | 5.41 (7.13) |
| Medical-surgical | 6.30 (7.02) | 5.98 (8.21) | 6.19 (8.32) | 5.17 (6.55) | 5.87 (8.40) | 4.66 (5.97) | 5.94 (7.79) | 5.18 (7.71) | 5.01 (5.98) | 6.30 (8.31) | 6.63 (8.42) | 5.49 (6.85) | 5.72 (7.52) |
| All units | 6.42 (7.85) | 5.89 (8.06) | 6.45 (8.41) | 5.15 (6.80) | 5.63 (7.58) | 4.72 (6.45) | 5.89 (7.74) | 5.44 (7.46) | 4.96 (6.38) | 6.13 (7.32) | 6.77 (8.29) | 5.95 (7.04) | 5.81 (7.44) |
| RN HPPD | |||||||||||||
| Step-down | 7.06 (1.62) | 7.32 (1.85) | 7.68 (2.19) | 7.44 (2.19) | 7.13 (1.94) | 7.30 (1.90) | 7.19 (1.78) | 7.26 (1.79) | 7.34 (1.78) | 7.51 (1.71) | 7.49 (1.78) | 7.54 (1.78) | 7.39 (1.83) |
| Medical | 5.06 (1.45) | 5.36 (1.42) | 5.32 (1.27) | 5.42 (1.31) | 5.44 (1.22) | 5.52 (1.24) | 5.53 (1.36) | 5.80 (1.49) | 5.76 (1.47) | 5.79 (1.46) | 5.77 (1.40) | 5.73 (1.30) | 5.63 (1.39) |
| Surgical | 5.40 (1.29) | 5.74 (1.42) | 5.54 (1.36) | 5.69 (1.32) | 5.73 (1.24) | 5.75 (1.90) | 5.76 (1.47) | 5.97 (1.51) | 5.87 (1.37) | 5.95 (1.33) | 5.97 (1.38) | 5.97 (1.30) | 5.84 (1.42) |
| Medical-surgical | 5.15 (1.42) | 5.38 (1.49) | 5.35 (1.33) | 5.44 (1.33) | 5.33 (1.54) | 5.39 (1.40) | 5.48 (1.37) | 5.65 (1.64) | 5.61 (1.46) | 5.74 (1.39) | 5.78 (1.56) | 5.79 (1.36) | 5.59 (1.46) |
| All units | 5.53 (1.61) | 5.79 (1.68) | 5.82 (1.76) | 5.83 (1.67) | 5.77 (1.63) | 5.87 (1.73) | 5.86 (1.60) | 6.04 (1.70) | 6.02 (1.64) | 6.13 (1.61) | 6.15 (1.67) | 6.17 (1.60) | 5.99 (1.66) |
| Non-RN HPPD | |||||||||||||
| Step-down | 2.84 (1.12) | 3.08 (1.34) | 3.16 (1.61) | 2.93 (1.46) | 2.72 (1.10) | 3.03 (1.23) | 2.94 (1.18) | 2.82 (1.08) | 2.62 (1.01) | 2.80 (1.17) | 2.74 (1.18) | 2.70 (1.18) | 2.82 (1.20) |
| Medical | 3.11 (1.07) | 3.08 (0.89) | 3.17 (0.97) | 3.18 (1.04) | 3.06 (1.02) | 3.18 (1.06) | 3.19 (0.97) | 3.10 (0.98) | 2.83 (0.91) | 2.90 (0.86) | 2.95 (0.90) | 2.89 (0.84) | 3.02 (0.95) |
| Surgical | 2.98 (0.87) | 2.99 (0.87) | 3.03 (0.94) | 2.96 (0.86) | 2.87 (0.96) | 3.06 (1.03) | 3.11 (0.96) | 3.00 (1.00) | 2.78 (0.90) | 2.83 (0.97) | 2.84 (1.06) | 2.84 (0.99) | 2.92 (0.97) |
| Medical-surgical | 2.92 (1.02) | 3.15 (1.03) | 3.20 (1.20) | 3.01 (1.26) | 2.87 (1.10) | 3.02 (1.14) | 3.08 (1.10) | 3.03 (1.05) | 2.88 (1.00) | 2.93 (0.98) | 2.95 (1.02) | 2.93 (1.00) | 2.98 (1.06) |
| All units | 2.97 (1.02) | 3.08 (1.02) | 3.15 (1.19) | 3.03 (1.17) | 2.89 (1.05) | 3.07 (1.12) | 3.09 (1.06) | 3.01 (1.03) | 2.80 (0.97) | 2.88 (0.99) | 2.89 (1.04) | 2.85 (1.00) | 2.95 (1.04) |
| UAPU | |||||||||||||
| Step-down | 3.60 (6.31) | 3.69 (6.30) | 4.28 (9.00) | 2.89 (5.46) | 3.98 (7.44) | 3.74 (7.18) | 3.31 (6.07) | 2.84 (4.89) | 2.30 (4.21) | 2.45 (4.52) | 2.70 (5.27) | 2.90 (6.30) | 3.02 (5.91) |
| Medical | 4.69 (5.57) | 3.44 (6.45) | 3.80 (6.08) | 4.53 (6.89) | 3.33 (4.91) | 2.25 (4.05) | 2.52 (4.80) | 2.58 (4.36) | 2.80 (5.05) | 2.68 (5.27) | 2.39 (4.67) | 2.63 (4.57) | 2.89 (5.10) |
| Surgical | 3.35 (5.30) | 2.56 (4.64) | 2.69 (5.30) | 2.39 (4.41) | 2.14 (4.13) | 1.42 (2.96) | 1.73 (3.80) | 1.70 (3.31) | 2.23 (4.77) | 1.82 (3.91) | 1.88 (4.22) | 1.55 (3.98) | 1.98 (4.18) |
| Medical-surgical | 3.65 (6.38) | 2.93 (5.13) | 2.91 (5.66) | 2.69 (4.44) | 2.65 (5.27) | 1.95 (4.42) | 2.08 (4.07) | 1.96 (4.30) | 2.69 (4.84) | 2.20 (4.27) | 1.90 (4.10) | 1.91 (4.02) | 2.28 (4.56) |
| All units | 3.84 (5.93) | 3.11 (5.62) | 3.36 (6.47) | 3.17 (5.44) | 2.98 (5.47) | 2.28 (4.84) | 2.35 (4.67) | 2.22 (4.27) | 2.55 (4.77) | 2.30 (4.54) | 2.18 (4.53) | 2.23 (4.73) | 2.52 (4.93) |
Note. Standard deviations of the variables are in parentheses. The sample size used for this descriptive analysis was 10,935 observations from 2,294 units in 465 hospitals. HPPD, hours per patient day; Non-RN, non-registered nurse; RN, registered nurse; UAPU, unit-acquired pressure ulcers.
Associations between RN Turnover, Staffing, and UAPU
The results of the multilevel logistic models for UAPUs are presented in Table 3. No statistically significant association was found between concurrent RN turnover and UAPU (no support for H1). However, the lagged effect of RN turnover on UAPUs was significant with and without the adjustment for RN staffing levels, indicating that H2 was supported (see Models 1 and 2). In Model 1, the odds ratio (OR) for lagged RN turnover was 1.004 (p = .038), indicating that for every 10 percentage-point increase in the RN turnover rate in a quarter, the odds of a patient having a UAPU were expected to increase by 4 percent in the next quarter. The change in RN turnover ORs was very minimal, both with and without the adjustment for RN staffing.
Table 3.
Estimations of Multilevel Logistic Regressions of Unit-acquired Pressure Ulcers
| Model 1 |
Model 2 |
Model 3 |
||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Lagged RN turnover | 1.004 (1.000, 1.008) | .038 | 1.004 (1.000, 1.008) | .044 | ||
| RN turnover | 1.002 (0.998, 1.006) | .394 | 1.002 (0.998, 1.006) | .442 | ||
| Non-RN staffing | 1.052 (1.001, 1.106) | .047 | 1.049 (0.997, 1.103) | .063 | 1.053 (1.002, 1.107) | .043 |
| RN staffing | 0.952 (0.916, 0.989) | .011 | 0.950 (0.914, 0.987) | .009 | ||
| Case mix index | 1.059 (0.711, 1.577) | .777 | 1.110 (0.746, 1.654) | .606 | 1.116 (0.748, 1.663) | .591 |
| Unit type | ||||||
| Step-down (Reference) | ||||||
| Medical | 0.971 (0.851, 1.107) | .655 | 0.893 (0.772, 1.034) | .130 | 0.890 (0.769, 1.030) | .119 |
| Surgical | 0.726 (0.629, 0.837) | <.001 | 0.669 (0.573, 0.782) | <.001 | 0.665 (0.569, 0.777) | <.001 |
| Medical-surgical | 0.732 (0.644, 0.832) | <.001 | 0.672 (0.582, 0.777) | <.001 | 0.670 (0.580, 0.774) | <.001 |
| Magnet status | ||||||
| Non magnet (Reference) | ||||||
| Magnet | 0.826 (0.692, 0.986) | .034 | 0.837 (0.702, 0.999) | .049 | 0.833 (0.698, 0.995) | .044 |
| Hospital size | ||||||
| <200 beds (Reference) | ||||||
| 200–399 beds | 0.969 (0.812, 1.156) | .724 | 0.947 (0.793, 1.130) | .545 | 0.947 (0.793, 1.130) | .545 |
| ≥400 beds | 0.902 (0.678, 1.199) | .478 | 0.888 (0.668, 1.180) | .412 | 0.888 (0.668, 1.181) | .415 |
| Year-quarter | 0.892 (0.856, 0.931) | <.001 | 0.894 (0.857, 0.933) | <.001 | 0.890 (0.853, 0.928) | <.001 |
| Year-quarter2 | 1.004 (1.001, 1.007) | .011 | 1.004 (1.001, 1.007) | .010 | 1.004 (1.001, 1.007) | .005 |
| Full model Wald χ2 | 209.90 | 216.05 | 211.21 | |||
| Log likelihood | −9,691.41 | −9,688.12 | −9,690.36 | |||
Note. All models were based on 10,935 observations (from 2,294 units in 465 hospitals) that did not have missing values for the lagged variables. In Model 1, unit-acquired pressure ulcer rates were regressed on RN turnover rates in the previous and current quarter after adjusting for controls. Model 2 was regressed by adding the adjustment for RN staffing levels to Model 1. Model 3 examined a relationship between RN staffing and pressure ulcers without the effects of RN turnover. For lagged variables, a one-quarter lag was used. CI, confidence interval; HPPD, hours per patient day; Non-RN, nonregistered nurse; OR, odds ratio; RN, registered nurse.
Unit-level RN staffing had a significant effect on UAPU outcomes (support for H3). More RN hours per patient day were associated with lower UAPU rates, controlling for other variables (OR = 0.952, p = .011; see Model 2). In addition, the significant effect of RN staffing on UAPUs remained without the RN turnover variables included as predictors (OR = 0.950, p = .009; see Model 3). Higher non-RN staffing was significantly related to higher UAPU rates in Models 1 and 3. In all models, quadratic-time effects were statistically significant.
Associations between Hospital and Unit Characteristics and UAPU
Magnet status was significantly associated with UAPU outcomes (Table 3). The UAPU odds were about 16 percent lower among units in Magnet hospitals compared to units in non-Magnet hospitals, holding other factors constant (see Model 2). Step-down units tended to have higher UAPU rates than surgical and combined medical-surgical units. Hospital size and CMI were not statistically associated with UAPU rates in nursing units.
Associations between RN Staffing and Turnover
Regression analysis revealed significant effects of concurrent and lagged RN turnover rates on RN staffing levels, supporting H4 (see Table 4). Higher rates of RN turnover in prior and current quarters were associated with lower levels of RN staffing in the current quarter. However, the concurrent and lagged levels of RN staffing did not have a statistically significant effect on RN turnover rates (no support for H5).
Table 4.
Regression Results for RN Staffing and RN Turnover
| Coefficient (95% CI) | p-Value | |
|---|---|---|
| (a) Regression of RN staffing on RN turnover (Full model Wald χ2 (12) = 1,666.12, p < .001) | ||
| Lagged RN turnover | −0.004 (−0.005, −0.002) | <.001 |
| Concurrent RN turnover | −0.002 (−0.004, −0.001) | .007 |
| (b) Regression of RN turnover on RN staffing (Full model Wald χ2 (11) = 112.74, p < .001) | ||
| RN staffing | −0.008 (−0.027, 0.012) | .435 |
| (c) Regression of RN turnover on lagged RN staffing (Full model Wald χ2 (11) = 102.91, p < .001) | ||
| Lagged RN staffing | −0.006 (−0.026, 0.013) | .519 |
Note. All models were based on 10,935 observations (from 2,294 units in 465 hospitals) that did not have missing values for the lagged variables. All three models were adjusted for non-RN staffing, unit type, case mix index, Magnet status, hospital size, year-quarter, and squared year-quarter. Multilevel mixed linear regression was used for Model (a). Multilevel Poisson regression models were used for Models (b) and (c). For lagged variables, a one-quarter lag was used. CI, confidence interval; RN, registered nurse.
Discussion
Nurse turnover is inevitable even under the best of work environments. Some nurse turnover can be beneficial by replacing poorly performing staff with new hires who bring fresh ideas and new practices to a unit. However, these potential benefits are outweighed by the results of nurse turnover: reductions of individual and organizational effectiveness, productivity, and quality of care (Buchan 2010). We used longitudinal analyses to examine the effects of unit-level RN turnover and staffing on UAPUs. We hypothesized that high RN turnover and low RN staffing would be associated with higher UAPU rates on nursing units; we found support for these relationships in this study.
Specifically, our findings showed that nursing units with higher RN turnover in a quarter were more likely to have higher UAPU rates in the next quarter. However, no concurrent relationship was found between RN turnover and UAPUs. We conclude that the effect of higher RN turnover on UAPUs was delayed until the next quarter rather than immediately observed. Based on this, we suggest that RN turnover can impede the provision of high-quality patient care during the transition period for the remaining and new RN staff on units.
Past studies have reported inconsistent findings on the relationship between nurse staffing and pressure ulcers (Cho et al. 2003; Unruh 2003; Blegen et al. 2011). However, our regression findings from unit-level longitudinal analyses add to the empirical evidence in support of the relationship between higher RN staffing levels and lower UAPU rates. Our descriptive analysis also showed a trend toward slightly increasing RN staffing and decreasing UAPU rates over the study period. Based on our regression results, the decreasing trend in UAPU rates was non-linear over 12 quarters from 2008 through 2010, holding other factors constant.
RN staffing was significantly related to UAPU outcomes regardless of whether RN turnover was also included in the model. As hypothesized, we found that RN turnover in a quarter affected RN staffing levels in both the current and subsequent quarter, while RN staffing levels did not affect turnover rates. However, the significant effect of lagged RN turnover on UAPUs did not change after adjusting for RN staffing. Based on these results, we concluded that there was no evidence for the mediation effect of RN staffing on the relationship between lagged RN turnover and UAPUs.
Instead of RN staffing, job satisfaction might be a potential mediator for the relationship between RN turnover and patient outcomes because high turnover on a unit can lead to low job satisfaction of the remaining staff, resulting in poorer patient outcomes. However, in this study, we could not check this mediation effect because NDNQI collects job satisfaction data annually rather than quarterly. Moreover, many hospitals do not provide job satisfaction data, and limiting the sample to units with for which these data were available would have led to an extreme reduction in the sample size. Future researchers should examine the mediation effect of job satisfaction with a different study design or data.
Although some studies have found no association between patient outcomes and non-RN staffing (Needleman et al. 2002; Park et al. 2012), we found that higher levels of non-RN staffing were associated with higher UAPU rates on nursing units when RN staffing levels and unit and hospital characteristics were held constant. This is consistent with the positive association between non-RN staffing and patient falls observed by Lake et al. (2010).
In the current study, Magnet-designated hospitals showed lower UAPU rates than non-Magnet hospitals. This finding was similar to that of previous studies that found better patient outcomes, such as lower fall rates, in Magnet hospitals (Dunton et al. 2007; Lake et al. 2010).
Despite our efforts to minimize weaknesses in the study's design, there are limitations. First, although collecting data from a large sample of hospitals nationwide was a study strength, the sample included mostly not-for-profit, large hospitals in metropolitan areas as compared with the AHA sample. Second, we analyzed one-quarter lags for RN turnover and UAPUs because UAPUs were measured quarterly, making a lag of one quarter the shortest possible time increment. However, we might have estimated more precise lagged effects on outcomes if we could have obtained measures on a monthly basis. Third, although the NDNQI's pressure ulcer indicator has strength in that it is collected by direct observation of patient skin and previous studies support its reliability (Hart et al. 2006; Bergquist-Beringer et al. 2011), the data on pressure ulcers were gathered during quarterly surveys that were performed on one calendar day at each nursing unit. Pressure ulcer rates computed from each quarterly survey may overestimate or underestimate actual pressure ulcer rates on nursing units for the quarter; however, more frequent tracking of pressure ulcers using this data collection method is expensive and time-consuming. Thus, using the data on pressure ulcers from the quarterly surveys was our only feasible method to measure pressure ulcer rates. Finally, unit-level information on interventions to prevent pressure ulcers and accessible resources for these activities was not available for this study analysis. Although we controlled for unit and hospital characteristics in addition to the adjustment for unit- and hospital-specific random intercepts and time trends, our adjustment might not be enough to account for unmeasured factors related to patient acuity or quality of care on nursing units, such as having more patients at higher risk for pressure ulcers, the lack of health care professionals who specialize in skin and wound care, or poor support systems to improve quality of care.
This study contributes to understanding the association between RN turnover and UAPUs. Based on our findings, we suggest that RN turnover is an important factor that negatively influences RN staffing levels needed for high-quality care and also adversely affects UAPU outcomes regardless of staffing levels. Higher RN turnover may be detrimental to a unit's capability to deliver high-quality care due to loss of clinical expertise, productivity, effectiveness, and teamwork. We also suggest that although RN staffing may not mediate the relationship between RN turnover and UAPUs, higher RN staffing is critical to improving UAPU outcomes relative to non-RN staffing. Thus, organizational efforts to maintain a stable and adequate RN workforce are needed for better outcomes of UAPUs on units.
Although pressure ulcers are one of the most common and costly adverse events on nursing units (Russo, Steiner, and Spector 2008), they can be prevented by nurses' efforts to improve quality of care (Bergquist-Beringer, Derganc, and Dunton 2009). We suggest that nursing administrators can reduce the occurrence of pressure ulcers by using managerial strategies and other interventions to promote a positive work environment to maintain a stable and adequate RN workforce on the units, developing a program for pressure ulcer prevention, and creating environments in which nursing and wound care teams can work closely. Given the high rates of RN turnover, we also suggest that administrators should prepare for the negative effect on patient outcomes that may occur at a later time and anticipate the possibility of an upcoming shortage of RNs on their hospital units.
To our knowledge, this is the first study to link RN turnover with pressure ulcer outcomes using unit-level longitudinal data. Our longitudinal analyses made it possible to evaluate time-lagged effects on a single patient outcome. Our unit-level study was also able to capture the associations among RN turnover, staffing, and patient outcomes on nursing units where turnover events occur and nursing care is delivered. Further research using multiple patient outcome indicators is needed to better understand the relationship between unit-level RN turnover and patient outcomes.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Support for this study was provided through a contract with the American Nurses Association (ANA).
Disclosures: At the time the study was conducted, the authors were personnel at the NDNQI, established by the ANA. The views expressed in this article are those of the authors and do not necessarily represent the views of the ANA and NDNQI.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
References
- Aiken LH, Clarke SP, Sloane DM, Sochalski JA, Busse R, Clarke H, Giovannetti P, Hunt J, Rafferty AM. Shamian J. “Nurses' Reports on Hospital Care in Five Countries”. Health Affairs. 2001;20(3):43–53. doi: 10.1377/hlthaff.20.3.43. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski JA. Silber JH. “Hospital Nurse Staffing and Patient Mortality, Nurse Burnout, and Job Dissatisfaction”. Journal of the American Medical Association. 2002;288(16):1987–93. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Allison JJ, Kiefe CI, Weissman NW, Person SD, Rousculp M, Canto JG, Bae S, Williams OD, Farmer R. Centor RM. “Relationship of Hospital Teaching Status with Quality of Care and Mortality for Medicare Patients with Acute MI”. Journal of the American Medical Association. 2000;284(10):1256–62. doi: 10.1001/jama.284.10.1256. [DOI] [PubMed] [Google Scholar]
- Allman RM, Goode PS, Burst N, Bartolucci AA. Thomas DR. “Pressure Ulcers, Hospital Complications, and Disease Severity: Impact on Hospital Costs and Length of Stay”. Advances in Wound Care. 1999;12(1):22–30. [PubMed] [Google Scholar]
- Ayanian JZ. Weissman JS. “Teaching Hospitals and Quality of Care: A Review of the Literature”. Milbank Quarterly. 2002;80(3):569–93. doi: 10.1111/1468-0009.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bae SH, Mark B. Fried B. “Impact of Nursing Unit Turnover on Patient Outcomes in Hospitals”. Journal of Nursing Scholarship. 2010;42(1):40–9. doi: 10.1111/j.1547-5069.2009.01319.x. [DOI] [PubMed] [Google Scholar]
- Baernholdt M. Mark BA. “The Nurse Work Environment, Job Satisfaction and Turnover Rates in Rural and Urban Nursing Units”. Journal of Nursing Management. 2009;17(8):994–1001. doi: 10.1111/j.1365-2834.2009.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beecroft PC, Dorey F. Wenten M. “Turnover Intention in New Graduate Nurses: A Multivariate Analysis”. Journal of Advanced Nursing. 2008;62(1):41–52. doi: 10.1111/j.1365-2648.2007.04570.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergquist-Beringer S, Derganc K. Dunton N. “Embracing the Use of Skin Care Champions”. Nursing Management. 2009;40(12):19–24. doi: 10.1097/01.NUMA.0000365465.01722.4b. [DOI] [PubMed] [Google Scholar]
- Bergquist-Beringer S, Gajewski B, Dunton N. Klaus S. “The Reliability of the National Database of Nursing Quality Indicators Pressure Ulcer Indicator: A Triangulation Approach”. Journal of Nursing Care Quality. 2011;26(4):292–301. doi: 10.1097/NCQ.0b013e3182169452. [DOI] [PubMed] [Google Scholar]
- Blegen MA, Goode CJ. Reed L. “Nurse Staffing and Patient Outcomes”. Nursing Research. 1998;47(1):43–50. doi: 10.1097/00006199-199801000-00008. [DOI] [PubMed] [Google Scholar]
- Blegen MA, Goode CJ, Spetz J, Vaughn T. Park SH. “Nurse Staffing Effects on Patient Outcomes: Safety-Net and Non-Safety-Net Hospitals”. Medical Care. 2011;49(4):406–14. doi: 10.1097/MLR.0b013e318202e129. [DOI] [PubMed] [Google Scholar]
- Buchan J. “Reviewing the Benefits of Health Workforce Stability”. Human Resources for Health. 2010;8(1):29. doi: 10.1186/1478-4491-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buerhaus PI, Auerbach DI. Staiger DO. “The Recent Surge in Nurse Employment: Causes and Implications”. Health Affairs. 2009;28(4):w657–68. doi: 10.1377/hlthaff.28.4.w657. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (CMS) 2012. Hospital-Acquired Conditions [accessed on October 31, 2013]. Available at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalAcqCond/Hospital-Acquired_Conditions.html.
- Cho SH, Ketefian S, Barkauskas VH. Smith DG. “The Effects of Nurse Staffing on Adverse Events, Morbidity, Mortality, and Medical Costs”. Nursing Research. 2003;52(2):71–9. doi: 10.1097/00006199-200303000-00003. [DOI] [PubMed] [Google Scholar]
- Dunton N, Gajewski B, Klaus SF. Pierson B. “The Relationship of Nursing Workforce Characteristics to Patient Outcomes”. Online Journal of Issues in Nursing. 2007;12(3):3. [Google Scholar]
- Gardner JK, Thomas-Hawkins C, Fogg L. Latham CE. “The Relationships between Nurses' Perceptions of the Hemodialysis Unit Work Environment and Nurse Turnover, Patient Satisfaction, and Hospitalizations”. Nephrology Nursing Journal. 2007;34(3):271–81. [PubMed] [Google Scholar]
- Greene WH. Econometric Analysis. Upper Saddle River, NJ: Prentice Hall; 2012. [Google Scholar]
- Hart S, Bergquist S, Gajewski B. Dunton N. “Reliability Testing of the National Database of Nursing Quality Indicators Pressure Ulcer Indicator”. Journal of Nursing Care Quality. 2006;21(3):256–65. doi: 10.1097/00001786-200607000-00011. [DOI] [PubMed] [Google Scholar]
- Hayes LJ, O'Brien-Pallas L, Duffield C, Shamian J, Buchan J, Hughes F, Laschinger HK. North N. “Nurse Turnover: A Literature Review – An Update”. International Journal of Nursing Studies. 2012;49(7):887–905. doi: 10.1016/j.ijnurstu.2011.10.001. [DOI] [PubMed] [Google Scholar]
- HSM Group. “Acute Care Hospital Survey of RN Vacancy and Turnover Rates in 2000”. Journal of Nursing Administration. 2002;32(9):437–9. doi: 10.1097/00005110-200209000-00001. [DOI] [PubMed] [Google Scholar]
- Jones CB. “Staff Nurse Turnover Costs, Part I: A Conceptual Model”. Journal of Nursing Administration. 1990;20(4):18–23. [PubMed] [Google Scholar]
- Jones CB. “The Costs of Nurse Turnover, Part 2: Application of the Nursing Turnover Cost Calculation Methodology”. Journal of Nursing Administration. 2005;35(1):41–9. doi: 10.1097/00005110-200501000-00014. [DOI] [PubMed] [Google Scholar]
- Kovner C, Jones C, Zhan C, Gergen PJ. Basu J. “Nurse Staffing and Postsurgical Adverse Events: An Analysis of Administrative Data from a Sample of U.S. Hospitals, 1990-1996”. Health Services Research. 2002;37(3):611–29. doi: 10.1111/1475-6773.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET, Shang J, Klaus S. Dunton NE. “Patient Falls: Association with hospital Magnet Status and Nursing Unit Staffing”. Research in Nursing & Health. 2010;33(5):413–25. doi: 10.1002/nur.20399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiter MP, Harvie P. Frizzell C. “The Correspondence of Patient Satisfaction and Nurse Burnout”. Social Science & Medicine. 1998;47(10):1611–7. doi: 10.1016/s0277-9536(98)00207-x. [DOI] [PubMed] [Google Scholar]
- LeVasseur SA, Wang CY, Mathews B. Boland M. “Generational Differences in Registered Nurse Turnover”. Policy, Politics, Nursing, & Practice. 2009;10(3):212–23. doi: 10.1177/1527154409356477. [DOI] [PubMed] [Google Scholar]
- Mark BA. Belyea M. “Nurse Staffing and Medication Errors: Cross-Sectional or Longitudinal Relationships?”. Research in Nursing & Health. 2009;32(1):18–30. doi: 10.1002/nur.20305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark BA. Harless DW. “Nurse Staffing and Post-Surgical Complications using the Present on Admission Indicator”. Research in Nursing & Health. 2010;33(1):35–47. doi: 10.1002/nur.20361. [DOI] [PubMed] [Google Scholar]
- Mark BA, Harless DW. McCue M. “The Impact of HMO Penetration on the Relationship between Nurse Staffing and Quality”. Health Economics. 2005;14(7):737–53. doi: 10.1002/hec.988. [DOI] [PubMed] [Google Scholar]
- McCullagh P. Nelder JA. Generalized Linear Model. London: Chapman & Hall; 1989. [Google Scholar]
- National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel (NPUAP/EPUAP) Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Washington, DC: NPUAP; 2009. [Google Scholar]
- National Quality Forum (NQF) National Voluntary Consensus Standards for Nursing-Sensitive Care: An Initial Performance Measure Set. Washington, DC: NQF; 2004. [Google Scholar]
- Needleman J, Buerhaus P, Mattke S, Stewart M. Zelevinsky K. “Nurse-Staffing Levels and the Quality of Care in Hospitals”. New England Journal of Medicine. 2002;346(22):1715–22. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- O'Brien-Pallas L, Griffin P, Shamian J, Buchan J, Duffield C, Hughes F, Spence Laschinger HK, North N. Stone PW. “The Impact of Nurse Turnover on Patient, Nurse, and System Outcomes: A Pilot Study and Focus for a Multicenter International Study”. Policy, Politics, Nursing, & Practice. 2006;7(3):169–79. doi: 10.1177/1527154406291936. [DOI] [PubMed] [Google Scholar]
- O'Brien-Pallas L, Murphy GT, Shamian J, Li X. Hayes LJ. “Impact and Determinants of Nurse Turnover: A Pan-Canadian Study”. Journal of Nursing Management. 2010;18(8):1073–86. doi: 10.1111/j.1365-2834.2010.01167.x. [DOI] [PubMed] [Google Scholar]
- Park SH, Blegen MA, Spetz J, Chapman SA. De Groot H. “Patient Turnover and the Relationship between Nurse Staffing and Patient Outcomes”. Research in Nursing & Health. 2012;35(3):277–88. doi: 10.1002/nur.21474. [DOI] [PubMed] [Google Scholar]
- Russo CA, Steiner C. Spector W. Hospitalizations Related to Pressure Ulcers among Adults 18 Years and Older, 2006: HCUP Statistical Brief #64. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [PubMed] [Google Scholar]
- Shortell SM, Zimmerman JE, Rousseau DM, Gillies RR, Wagner DP, Draper EA, Knaus WA. Duffy J. “The Performance of Intensive Care Units: Does Good Management Make a Difference?”. Medical Care. 1994;32(5):508–25. doi: 10.1097/00005650-199405000-00009. [DOI] [PubMed] [Google Scholar]
- Spetz J. Given R. “The Future of the Nurse Shortage: Will Wage Increases Close the Gap?”. Health Affairs. 2003;22(6):199–206. doi: 10.1377/hlthaff.22.6.199. [DOI] [PubMed] [Google Scholar]
- Staiger DO, Auerbach DI. Buerhaus PI. “Registered Nurse Labor Supply and the Recession: Are We in a Bubble?”. New England Journal of Medicine. 2012;366(16):1463–5. doi: 10.1056/NEJMp1200641. [DOI] [PubMed] [Google Scholar]
- Tai TW, Bame SI. Robinson CD. “Review of Nursing Turnover Research, 1977-1996”. Social Science & Medicine. 1998;47(12):1905–24. doi: 10.1016/s0277-9536(98)00333-5. [DOI] [PubMed] [Google Scholar]
- Unruh L. “Licensed Nurse Staffing and Adverse Events in Hospitals”. Medical Care. 2003;41(1):142–52. doi: 10.1097/00005650-200301000-00016. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Health Services (DHHS) Health Resources and Services Administration Bureau of Health Professions. 2002. Projected Supply, Demand, and Shortages of Registered Nurses: 2000-2020 [accessed on October 31, 2013]. Available at http://www.ask.hrsa.gov/detail_materials.cfm?ProdID=4313.
- Veterans Health Administration (VHA) Center for Research and Innovation. 2002. The Business Case for Workforce Stability [accessed on October 31, 2013]. Available at http://www.healthleadersmedia.com/pdf/white_papers/wp_vha_120103.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


