Abstract
Aims
Our goal was to evaluate the association between antidepressant use and the risk of coronary heart disease (CHD) among subjects with no history of coronary heart disease.
Methods
A search of Medline, EMBASE, PsycINFO and the Cochrane Library was performed in January 2013. Two authors independently reviewed and selected eligible observational studies, based on predetermined selection criteria. Pooled relative risks (RRs) with confidence intervals (CIs) were calculated using random-effects or fixed-effects models.
Results
Sixteen observational studies (seven case–control studies and nine cohort studies) were included in the final analysis. There was no association between selective serotonin reuptake inhibitor use and the risk of CHD overall [odds ratio (OR), 0.93; 95% CI, 0.65–1.33] or in subgroup meta-analysis of case–control studies (OR, 0.91; 95% CI, 0.60–1.37) and cohort studies (RR, 0.96; 95% CI, 0.59–1.55). The use of tricyclic antidepressant was associated with an increased risk of CHD overall (OR, 1.51; 95% CI, 1.07–2.12), but it was observed only in case–control studies (OR, 1.56; 95% CI, 1.24–1.96) and low-quality studies (OR, 1.49; 95% CI, 1.20–1.85) in the subgroup meta-analyses.
Conclusions
This meta-analysis of observational studies in subjects with no history of CHD suggests that neither selective serotonin reuptake inhibitor nor tricyclic antidepressant use is associated with an increased risk of CHD.
Keywords: antidepressant, coronary heart disease, meta-analysis, myocardial infarction, selective serotonin reuptake inhibitor, tricyclic antidepressant
What is Already Known about this Subject
Antidepressants are among the most frequently prescribed drugs in the world.
Several randomized controlled studies and meta-analyses have evaluated the association between antidepressant use and the risk of coronary heart disease (CHD) in populations with pre-existing CHD at baseline.
Little is known about the association between antidepressants and CHD in subjects without underlying CHD, and existing results have been controversial.
What this Study Adds
There was no association between selective serotonin reuptake inhibitor antidepressant use and risk of CHD in the overall analysis and subgroup analyses by study design.
Tricyclic antidepressant use was associated with an increased risk of CHD only in case–control studies and low-quality studies.
Introduction
Antidepressants are among the most frequently prescribed drugs in the world, and the use of antidepressants has increased dramatically in the past decade [1,2]. However, little is known about whether antidepressant use is related to coronary heart disease (CHD). Although multiple epidemiological studies have sought to identify the association between antidepressant use and CHD risk, their variable study populations and difference in methodology have hindered the production of conclusive results. Several observational studies, for instance, reported an increased risk of CHD associated with antidepressants. The increased risk was observed mainly in patients using tricyclic antidepressant (TCA) [3–8], while there have also been reports of increased risk with selective serotonin reuptake inhibitor (SSRI) use [8–10]. Conversely, some studies found protective effects of antidepressants [11,12], whereas others found no such association [13–20].
Interestingly, multiple randomized controlled studies and meta-analyses have evaluated the association of antidepressants and the risk of CHD in populations with pre-existing CHD at baseline, while subjects without CHD have not been able to attract much attention [21]. There has been no randomized controlled trial addressing antidepressant use and its effect on CHD in patients without pre-existing CHD. However, identifyication of the association between antidepressants and CHD risk in an otherwise healthy population is crucial, because the use of antidepressants is increasing not only for depression but also for a variety of conditions.
As such, the purpose of this study was to investigate the association between antidepressant use and the risk of CHD among subjects with no history of CHD, by conducting a meta-analysis of observational studies.
Methods
Search strategy
We conducted Medline (PubMed), EMBASE, PsycINFO and Cochrane Library searches in January 2013 using the following MeSH keywords: ‘antidepressive agents’, ‘serotonin reuptake inhibitors’ and ‘antidepressive agents, tricyclic’ for exposure factors, and ‘cardiovascular diseases’, ‘myocardial ischaemia’, ‘acute coronary syndrome’, ‘angina pectoris’, ‘myocardial infarction’ and ‘coronary heart disease’ for outcome factors. The searches were performed by two of the authors (JK and S-WO) and confirmed by another (S-KM). Bibliographies of relevant articles were reviewed to identify potentially relevant studies.
Eligibility criteria
We included case–control studies and cohort studies that examined the association between antidepressant use and the risk of CHD by using odds ratios (ORs) or relative risks (RRs). Only articles written in English were reviewed. We excluded studies with no available data for outcome measure, those with the same population as other studies (in this case, we included the first published or the more comprehensive study in the analysis), those with data on mortality only, and those that used standardized incidence ratios.
Definition of antidepressants
An SSRI user was defined as a subject who was exposed to at least one SSRI (fluoxetine, fluvoxamine, paroxetine, sertraline, citalopram and escitalopram). A TCA user was defined as a subject who was exposed to at least one of the following antidepressants: amitriptyline, clomipramine, imipramine, trimipramine, desipramine, nortriptyline, protriptyline, amoxapine, dothiepin, doxepin and maprotiline.
Main outcome
The primary outcome of this study was CHD. Coronary heart disease was defined as acute myocardial infarction (MI), CHD death including fatal MI and other ischaemic heart disease.
Data extraction
Data extraction and evaluation of bibliographies were performed independently by two authors (JK and S-WO). Discrepancies were resolved by consensus or through consultation with the other authors (S-KM and D-HY). Among the articles found in the three databases, duplicate articles and those that did not meet the selection criteria were excluded.
We extracted the following data from the selected studies: study name (first author and year of publication), study design, country, year of enrolment, characteristics of study population, exposure assessment, category of antidepressant, definition of use, OR or RR with 95% confidence interval (CI) and adjustment for severity of depression.
We assessed the methodological quality of the included studies by the nine-star Newcastle–Ottawa Scale (NOS) for quality of nonrandomized studies in meta-analyses. The rating was also performed by two evaluators, and discrepancies were resolved by consensus, as was study selection. Given that there are no standard criteria to define a high-quality study, we considered a high-quality study as one that had more stars than the average among the included studies with the same study design.
Statistical analysis
Adjusted data (adjusted OR or RR with 95% CI) were used for the meta-analysis. We performed subgroup analyses by quality of study methodology, study design type (case–control studies vs. cohort studies; a nested case–control study was classified as a case–control study), outcome adjusted for severity of depression, elderly population (age ≥65 years), depressed population and gender (female or male).
The extent of heterogeneity among study results was assessed using the Higgins I2, which is a percentage measure of total variation across the studies. The value of I2 is calculated as follows:
where Q is Cochran's heterogeneity statistic and d.f. is degrees of freedom. Negative values of I2 are set to zero, so that I2 lies between 0% (no observed heterogeneity) and 100% (maximal heterogeneity). An I2 value >50% is considered to show substantial heterogeneity. Both fixed-effects and random-effects models were used to calculate the pooled OR or RR with a 95% CI. The pooled estimate based on the fixed-effects model was calculated when substantial heterogeneity was not found (i.e. I2 ≤ 50%). In contrast, the pooled estimate based on the random-effects model was calculated when substantial heterogeneity was found (i.e. I2 > 50%).
We used the Woolf method (inverse variance method) for the fixed-effects analysis [22], and the DerSimonian and Laird method for the random-effects analysis [23]. Publication bias was assessed using Begg's funnel plot and Egger's test. Publication bias was considered to be present if the funnel plot was asymmetrical or Egger's test P value was <0.05. The Stata SE version 10.0 software package (StataCorp, College Station, TX, USA) was used for the statistical analysis.
Results
Literature search
Sixteen studies (seven case–control studies and 11 cohort studies) published between January 1995 and January 2013 were included in the final analysis. Figure 1 shows the flow diagram for the identification of the relevant studies.
Figure 1.
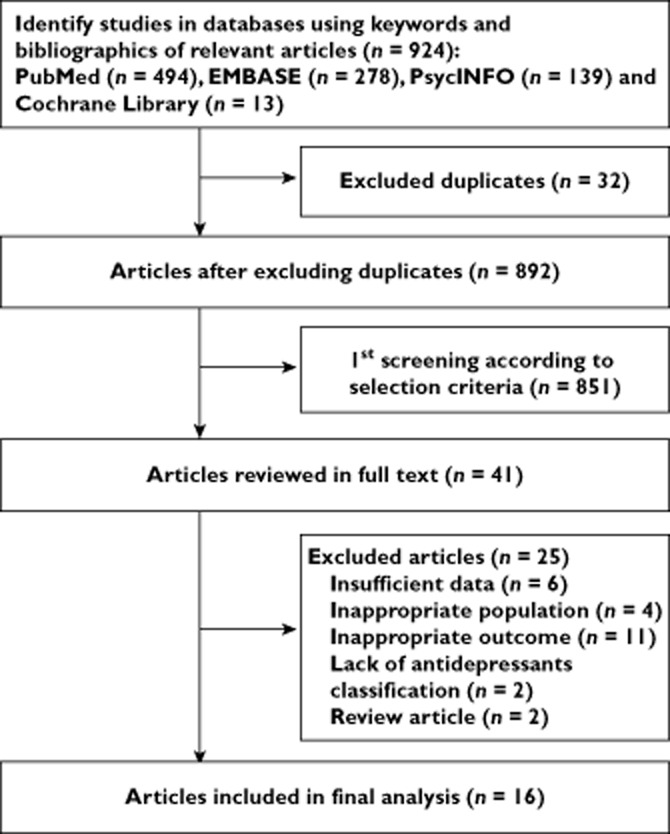
Flow diagram of identification of relevant studies
We identified 924 articles by searching the three databases and relevant bibliographies. After the exclusion of duplicates (n = 32), the titles and abstracts of all the remaining articles screened (n = 892) were reviewed. Of the 892 articles, 851 articles did not meet the predetermined selection criteria and were excluded. The full texts of the remaining 41 articles were reviewed, and 16 articles were included in the final analysis. The main reasons of exclusion from the final review (n = 25) were as follows: insufficient data (n = 6) [24–29], inappropriate population (post-MI patients, paediatric population and identical cohorts; n = 4) [30–33], inappropriate outcome (valvular disease, deep vein thrombosis, stroke and mortality only; n = 11) [34–44], lack of antidepressant classification (n = 2) [18,45] and review article (n = 2) [46,47].
Study characteristics
Table 1 shows the main characteristics of all the studies included in the final analysis. The study design types were as follows: population-based case–control studies (n = 6), nested case–control study (n = 1), retrospective cohort study (n = 1) and prospective cohort studies (n = 8). The countries where the studies had been performed were as follows: the USA (n = 8), the UK (n = 5), Denmark (n = 1), Finland (n = 1) and Canada (n = 1). The range of enrolment periods of participants across the studies was 1979 to 2007.
Table 1.
Characteristics of studies of antidepressants and coronary heart disease risk included in the final analysis (n = 16)
| Study (reference) | Country | Years enrolled | Population (age, years) | Exposure assessment | Category of antidepressant | Definition of use (highest category) | Main outcome | OR or RR (95% CI) | Adjustment for depression | |
|---|---|---|---|---|---|---|---|---|---|---|
| Case–control studies | ||||||||||
| 1 | Penttinen & Valonen (1996) [5] | Finland; nested CC | 1979–1980 | 83 cases and 249 controls; men (NA) | Community healthcare unit records | TCA | NA | MI | 5.40 (1.80–16.10) | No |
| 2 | Hippisley-Cox et al. (1998) [14] | UK | 1996 | 327 cases and 897 controls (68.7) | Computerized data | TCA | Use during 5 years preceding the diagnosis | IHD | Men: 3.55 (0.89–14.21) Women: 0.94 (0.37–2.35) |
Yes |
| 3 | Hippisley-Cox et al. (2001) [7] | UK | 1995–1999 | 933 cases and 5516 controls (NA) | Computerized data | TCA SSRI |
Use during 7.5 years preceding the diagnosis | IHD | 1.29 (0.89–1.87) 1.56 (1.18–2.05) |
No |
| 4 | Sauer et al. (2001) [11] | USA | 1995–1997 | 653 cases and 2990 controls (30–65) | Telephone interview | SSRI | Use during the week before the index date | MI | 0.35 (0.18–0.68) | No |
| 5 | Sauer et al. (2003) [55] | USA | 1998–2001 | 1080 cases and 4256 controls (40–75) | Telephone interview | SSRI TCA |
Use during the week before the index date | MI | 0.72 (0.49–1.05) 1.63 (0.89–2.88) |
No |
| 6 | Monster et al. (2004) [16] | Denmark | 1994–2002 | 5238 cases and 77,093 controls (21–102) | Prescription database | SSRI | Prescriptions redeemed in the 30 days before hospitalization | MI | 0.90 (0.67-1.19) | No |
| 7 | Tata et al. (2005) [8] | UK | 1988–2001 | 63,512 cases and 378,886 controls (over 18) | Prescription data | TCA SSRI |
Use during 28 days before index date | MI | 1.41 (1.37–1.45) 1.49 (1.43–1.56) |
No |
| Cohort studies | ||||||||||
| 1 | Lapane et al. (1995) [4] | USA | 1981 | 77 cases among 5998 (35–65) | Interview | TCA | Current use | IHD | 5.70 (2.60–12.80) | No |
| 2 | Pratt et al. (1996) [13] | USA | 1981 | 64 cases among 1551 (over 18) | Interview | TCA | Ever use | MI | 1.30 (0.52–3.29) | Yes |
| 3 | Cohen et al. (2000) [3] | USA | 1991–1992 | 207 cases among 54,997 (25–65) | Prescription data | TCA SSRI |
At least one prescription during the accrual period (1991, 1992) | MI | 2.20 (1.20–3.80) 0.80 (0.20–3.50) |
No |
| 4 | Blanchette et al. (2008) [9] | USA | 1997–2001 | 1052 SSRI users and 10,856 non-antidepressant users (over 65) | Interview | SSRI | Use during the baseline year | MI | 1.85 (1.13-3.04) | Yes |
| 5 | Smoller et al. (2009) [17] | USA | 1993–1998 | 2983 cases among 136,293 women (50–79) | Questionnaire | SSRI TCA |
Current use (first follow-up visit) | MI or CHD death | 0.95 (0.70–1.29) 1.13 (0.77–1.65) |
Yes |
| 6 | Rosenberg et al. (2010) [6] | Canada | 1995 | 147 cases among 970 (61) | Interview | SSRI TCA |
Current use (baseline visit) | IHD | 1.33 (0.49–3.64) 2.10 (1.09–4.06) |
Yes |
| 7 | Hamer et al. (2011) [19] | UK | 1995–2003 | 969 cases among 14,784 (52.4) | Interview | TCA SSRI |
Current use (baseline interview) | MI or CHD death | 1.24 (0.87–1.75) 0.81 (0.49–1.33) |
Yes |
| 8 | Scherrer et al. (2011) [12] | USA; retrospective | 1999–2000 | 93,653 depressed patients (51.5) | Patient records | SSRI TCA |
≥12 weeks of continuous use | MI | 0.48 (0.44–0.52) 0.39 (0.34–0.44) |
Yes |
| 9 | Coupland et al. (2011) [10] | UK | 1996–2007 | 60,746 depressed patients (over 65) | Medical record system | TCA SSRI |
At least one prescription | MI | 1.09 (0.96–1.23) 1.15 (1.04–1.27) |
Yes |
Abbreviations are as follows: CHD, coronary heart disease; CI, confidence interval; IHD, ischaemic heart disease; MI, myocardial infarction; NA, not available; OR, odds ratio; RR, relative risk; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
Quality of study methodologies
Table 2 shows the quality of study methodologies included in the final meta-analysis. The range of quality scores was 6–9; the average score was 7.5. The average scores (SD) of case–control studies and cohort studies were 7.4 (0.96) and 7.6 (0.52), respectively. The high-quality studies (exceeding the average score of each study type) included three of six case–control studies and five of 10 cohort studies.
Table 2.
Methodological quality of studies included in the final analysis, based on the Newcastle–Ottawa Scale for assessing the quality of case–control studies and cohort studies (n = 16)
| Case–control studies (n = 7) | Selection | Comparability | Exposure | Total (0–9) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Adequate definition of cases | Representativeness of cases | Selection of controls | Definition of controls | Control for important factor or additional factor | Ascertainment of exposure (blinding) | Same method of ascertainment for subjects | Nonresponse rate* | ||
| 1 Penttinen & Valonen (1996) [5] | * | * | * | * | * | * | 6 | ||
| 2 Hippisley-Cox et al. (1998) [14] | * | * | * | ** | * | * | * | 8 | |
| 3 Hippisley-Cox et al. (2001) [7] | * | * | * | * | ** | * | * | * | 9 |
| 4 Sauer et al. (2001) [11] | * | * | * | ** | * | * | 7 | ||
| 5 Sauer et al. (2003) [15] | * | * | * | ** | * | * | 7 | ||
| 6 Monster et al. (2004) [16] | * | * | * | ** | * | * | * | 8 | |
| 7 Tata et al. (2005) [8] | * | * | ** | * | * | * | 7 | ||
| Cohort studies (n = 9) | Selection | Comparability | Outcome | Total (0–9) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Outcome of interest not present at start of study | Control for important factor or additional factor | Assessment of outcome | Follow-up long enough for outcomes to occur | Adequacy of follow-up of cohorts | ||
| 1 Lapane et al. (1995) [4] | * | * | * | * | ** | * | * | 8 | |
| 2 Pratt et al. (1996) [13] | * | * | * | * | ** | * | 7 | ||
| 3 Cohen et al. (2000) [3] | * | * | * | ** | * | * | 7 | ||
| 4 Blanchette et al. (2008) [9] | * | * | * | ** | * | * | * | 8 | |
| 5 Smoller et al. (2009) [17] | * | * | * | * | ** | * | * | 8 | |
| 6 Rosenberg et al. (2010) [6] | * | * | * | ** | * | * | 7 | ||
| 7 Hamer et al. (2011) [19] | * | * | * | * | ** | * | * | 8 | |
| 8 Scherrer et al. (2011) [12] | * | * | * | * | ** | * | * | 8 | |
| 9 Coupland et al. (2011) [10] | * | * | * | ** | * | * | 7 | ||
If there was no significant difference in the response rate between both groups by using a χ2 test (P > 0.05), one point was awarded. Each study can be awarded a maximum of one star for each numbered item within the selection and exposure categories, while a maximum of two stars can be given for the comparability category.
Overall use of antidepressants and risk of coronary heart disease
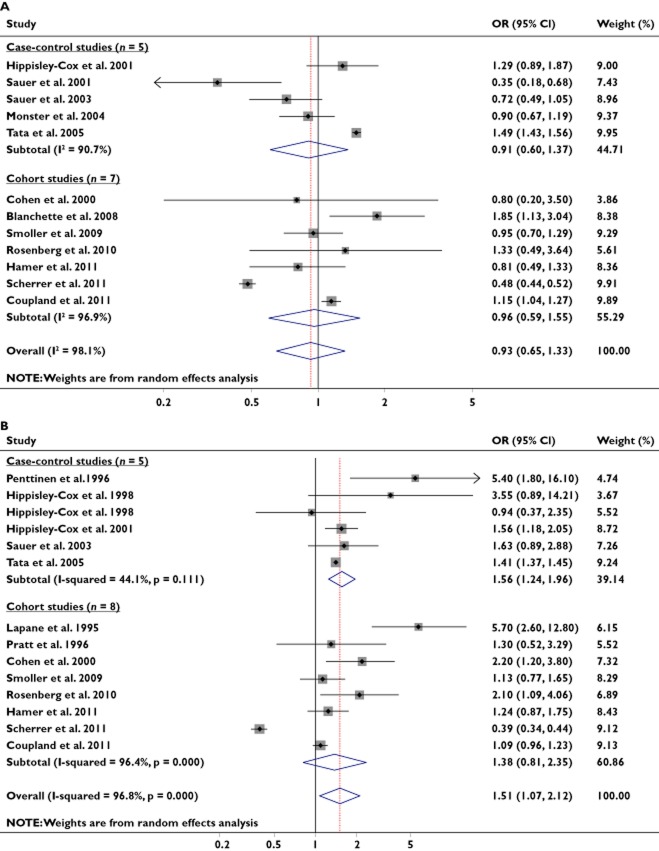
Figure 2 shows the effect of antidepressant use on CHD risk in the meta-analysis of all studies, including both case–control and cohort studies. Thirteen studies (five case–control and eight cohort studies) were included in the meta-analysis of TCA use and CHD risk. Overall, the use of TCAs significantly increased the risk of CHD (OR, 1.51; 95% CI, 1.07–2.12; I2 = 96.8%). In a subgroup meta-analysis by study design, an increased CHD risk with TCA use (OR, 1.56; 95% CI, 1.24–1.96; I2 = 44.1%; fixed-effects model) was observed in case–control studies, while there was no association observed within cohort studies (RR, 1.38; 95% CI, 0.81–2.36; I2 = 96.4%; random-effects model).
Figure 2.
(A) Association of selective serotonin reuptake inhibitor (SSRI) use and risk of coronary heart disease by type of study design. (B) Association of tricyclic antidepressant (TCA) use and risk of coronary heart disease by type of study design
Twelve studies (five case–control and seven cohort studies) were included in the meta-analysis of SSRI use and CHD risk. No association between SSRI use and CHD risk was observed overall (OR, 0.93; 95% CI, 0.65–1.33; I2 = 0.0%), or in subgroup meta-analyses of case–control studies (OR, 0.91; 95% CI, 0.60–1.37; I2 = 90.7%; random-effects model) and cohort studies (RR, 0.96; 95% CI, 0.59–1.55; I2 = 96.9%; random-effects model).
There was no publication bias in the 13 studies on TCA use (Egger's test, P for bias = 0.725) and in the 12 studies on SSRI use (Egger's test, P for bias = 0.401; Figure 3).
Figure 3.
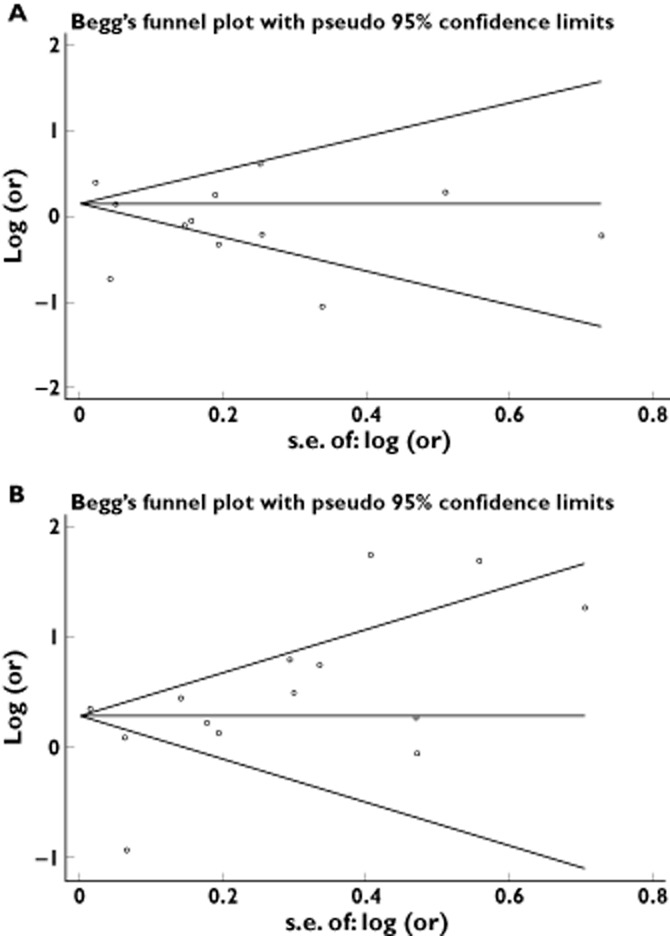
(A) Begg's funnel plot and Egger's test risk for identifying publication bias in the studies on SSRI use (Egger's test, P for bias = 0.401). (B) Begg's funnel plot and Egger's test risk for identifying publication bias in the studies on TCA use (Egger's test, P for bias = 0.725)
Subgroup meta-analyses
Table 3 summarizes the results of the subgroup meta-analyses. Significant association of antidepressant use and the risk of CHD was observed among low-quality studies regarding TCA use (OR, 1.49; 95% CI, 1.20–1.85; I2 = 76.8%; random-effects model), but not among high-quality studies regarding TCA use (OR, 1.38; 95% CI, 0.69–2.80; I2 = 96.1%; random-effects model). Increased risk of CHD was observed in a subgroup of males with TCA use (OR, 4.60; 95% CI, 1.95–10.85; I2 = 0.0%; fixed-effects model), whereas females did not have an increased risk of CHD. There was no association between SSRI use and CHD risk in subgroup meta-analyses, regardless of study quality.
Table 3.
Association between antidepressant use and coronary heart disease risk in subgroup meta-analyses by quality of study methodology, population age, baseline depression status and gender
| Category | No. of studies (reference numbers) | Summary RR (95% CI) | Heterogeneity, I2 (%) | Model used |
|---|---|---|---|---|
| Quality of study methodology | ||||
| High quality, SSRI | 6 [7,9,12,16,17,19] | 0.94 (0.60–1.49) | 93.7 | Random effects |
| Low quality, SSRI | 6 [3,6,8,10,11,15] | 0.99 (0.75–1.31) | 90.3 | Random effects |
| High quality, TCA | 6 [4,7,12,14,17,19] | 1.38 (0.69–2.80) | 96.1 | Random effects |
| Low quality, TCA | 7 [3,5,6,8,10,13,15] | 1.49 (1.20–1.85) | 76.8 | Random effects |
| Outcome adjusted for severity of depression | ||||
| Adjusted for depression, SSRI | 6 [6,9,10,12,17,19] | 0.97 (0.59–1.60) | 97.4 | Random effects |
| Adjusted for depression, TCA | 7 [6,10,12–14,17,19] | 1.13 (0.68–1.89) | 95.7 | Random effects |
| Elderly population | ||||
| ≥65 years old, SSRI | 2 [9,10] | 1.37 (0.87–2.14) | 70.7 | Random effects |
| ≥65 years old, TCA | 1 [10] | 1.09 (0.96–1.23) | ||
| Depressed population | ||||
| Depressed patients, SSRI | 2 [10,12] | 0.69 (0.64–0.73) | 99.4 | Random effects |
| Depressed patients, TCA | 2 [10,12] | 0.67 (0.61–0.73) | 99.2 | Random effects |
| Gender | ||||
| Female, SSRI | 1 [17] | 0.95 (0.70–1.29) | ||
| Female, TCA | 2 [14,17] | 1.10 (0.77–1.56) | 0.0 | Fixed effects |
| Male, TCA | 2 [5,14] | 4.60 (1.95–10.85) | 0.0 | Fixed effects |
Abbreviations are as follows: CI, confidence interval; RR, relative risk; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
There was no association between antidepressant use and CHD risk in subgroup meta-analyses by outcomes adjusted for severity of depression and elderly population (≥65 years old). In contrast, both SSRIs and TCAs had a significant protective effect on CHD in depressed patients (for SSRIs: OR, 0.69; 95% CI, 0.64–0.73; I2 = 99.4%; random-effects model; and for TCAs: OR, 0.67; 95% CI, 0.61–0.73; I2 = 99.2%; random-effects model).
Discussion
The findings from this meta-analysis of epidemiological studies, including case–control and cohort studies, indicate that there is no association between SSRI antidepressant use and CHD risk in the overall analysis and subgroup analyses by study design. Tricyclic antidepressant use was associated with an increased risk of CHD overall. However, in the subgroup meta-analyses by study design, increased risk of CHD with TCA use was observed only in case–control studies, not in cohort studies. Furthermore, only low-quality studies showed a significant association with risk of CHD, whereas high-quality studies did not.
The discordance between the case–control studies and cohort studies can be explained by the difference in important factors, such as the duration of TCA use and the presence of follow-up. Case–control studies deal with exposure data before hospitalization and cohort studies follow patients after initial screening of antidepressant use history; therefore, case–control studies tend to reflect relatively short-term effects of antidepressants in comparison to cohort studies. Three of the six case–control studies included in our meta-analysis defined the exposure to antidepressants as use during a month before the index date. There are conflicting data with regard to the duration of antidepressant exposure and risk of CHD. One study reported a temporarily increased risk of acute MI in the initial 28 days of exposure to antidepressant drugs, which did not persist after this period [8]. Another study suggested that a longer duration of antidepressant use may be associated with a greater risk [9]. Unfortunately, we could not perform subgroup analysis by duration of antidepressant use because of limited data. Further study would be necessary to confirm the short- and long-term effects of antidepressants on CHD.
Several studies have evaluated the association of antidepressant therapy and CHD in patients with previous CHD. Although some studies suggested that antidepressant therapy in depressed patients with CHD may reduce subsequent cardiovascular morbidity and mortality [16,30], other studies reported no significant association [48,49]. A meta-analysis of randomized controlled trials in patients with previous CHD suggested that SSRI use may improve CHD prognoses, such as readmission rate for CHD (RR = 0.63, 95% CI 0.46–0.86) and mortality (RR = 0.56, 95% CI 0.35–0.88) [21]. This protective effect of SSRIs in patients with CHD is inconsistent with the results of our study. The reason for the difference in results could not be ascertained, but several hypotheses can be suggested. First, the benefit of SSRIs in patients with CHD may be related to the increased susceptibility to cardioprotective effects of SSRIs compared with healthy populations. Numerous studies have shown that SSRIs improve endothelial function, decrease inflammatory markers and relieve autonomic dysfunction [50,51]. Second, the methodological quality of individual studies included in the meta-analysis might have affected the result as well. This hypothesis is supported by the fact that patients on SSRIs showed no significant differences in mortality or CHD readmission rates compared with control subjects when only properly randomized trials were considered in the aforementioned meta-analysis [21].
It has long been established that depression itself increases the risk of cardiovascular disease through abnormalities in the autonomic nervous system, enhanced platelet reactivity, endothelial dysfunction and increased thrombus formation [52–54]. Previous studies have suggested that the association between antidepressant use and cardiovascular disease risk is explained by the relief of depressive symptoms and not as a direct effect of the pharmacological agents [55]. In contrast, there have also been reports that antidepressants may expose individuals to an increased risk of CHD despite their theoretical benefit, regardless of depression [19]. In our study, subgroup meta-analysis of outcome adjusted for severity of depression demonstrated no significant association. Interestingly, subgroup analysis of patients with depression showed decreased CHD risk with the use of either SSRI or TCA, which is suggestive of protective effects in depressed patients. This finding requires further investigation, as the potential for confounding bias cannot be excluded.
It is unclear why only males using TCAs had a significantly increased risk of CHD in subgroup meta-analysis. Although only two studies had subgroups based on gender, and one had a significantly higher OR (OR = 5.40, 95% CI 1.80–16.10) compared with the other (OR = 3.55, 95% CI 0.89–14.21), this finding cannot be ignored. The most likely explanation of this finding is the natural difference in cardiovascular risk between men and women. It is well known that cardiovascular disease burden and mortality is significantly higher in males compared with females, and this might have affected the study outcome [56]. However, these findings should be evaluated in the future, due to the small number of studies and populations.
Our meta-analysis has several limitations. First, the definition of antidepressant use was heterogeneous. This term includes various types of antidepressants and different durations and doses of use. We divided antidepressants largely into TCAs and SSRIs by the mechanism of action. However, variations existed among antidepressants included in each group, and several studies did not provide generic names of antidepressants. For instance, Lapane et al. [4] and Penttinen & Valonen [5] included atypical antidepressants in the TCA group, while Blanchette et al. [9] included venlafaxine in the SSRI group. Analysis excluding these studies did not affect the overall outcome of the meta-analysis. (data not shown). Further study should examine specific drugs within the classes of antidepressants as well as their duration of use, dose, substitution within the class, and pattern of starting and stopping. It is also possible that association of antidepressants with CHD may differ based on the mechanism of action of the antidepressants. Unfortunately, we were unable to perform analyses on types of antidepressants other than TCAs and SSRIs due to the dearth of available data. Second, multidrug use in the study population was not adjusted correctly. This could have potentially biased our study outcomes. Third, defining a high-quality study by its superiority in comparison to other studies included in the analysis rather than having a definite standard may affect the interpretation of the study result. Fourth, only observational studies were evaluated, and the definition of CHD was not identical between studies in this meta-analysis, which is therefore not free of potential confounding biases. There has been no randomized control trial addressing antidepressant use and its effect on CHD without pre-existing CHD. Finally, we focused only on studies with the primary outcome of CHD. Thus, it was not feasible to investigate the association of antidepressants with other cardiovascular conditions, including stroke, heart failure or mortality.
In summary, we performed a meta-analysis of observational studies to investigate the association between antidepressant use and the risk of CHD among subjects with no history of CHD. The findings of this meta-analysis indicate that there is no evidence of an association between either TCA or SSRI antidepressant use and the risk of CHD. Tricyclic antidepressant use was associated with an increased risk of CHD overall, but it was observed only in low-quality studies and case–control studies, not in cohort studies, in the subgroup meta-analyses.
Competing Interests
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
This research was supported by grant no. 23-2013-0030 from the SNUH Research Fund.
References
- 1.Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66:848–856. doi: 10.1001/archgenpsychiatry.2009.81. [DOI] [PubMed] [Google Scholar]
- 2.Reid S, Barbui C. Long term treatment of depression with selective serotonin reuptake inhibitors and newer antidepressants. BMJ. 2010;340:c1468. doi: 10.1136/bmj.c1468. [DOI] [PubMed] [Google Scholar]
- 3.Cohen HW, Gibson G, Alderman MH. Excess risk of myocardial infarction in patients treated with antidepressant medications: association with use of tricyclic agents. Am J Med. 2000;108:2–8. doi: 10.1016/s0002-9343(99)00301-0. [DOI] [PubMed] [Google Scholar]
- 4.Lapane KL, Zierler S, Lasater TM, Barbour MM, Carleton R, Hume AL. Is the use of psychotropic drugs associated with increased risk of ischemic heart disease? Epidemiology. 1995;6:376–381. doi: 10.1097/00001648-199507000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Penttinen J, Valonen P. Use of psychotropic drugs and risk of myocardial infarction: a case-control study in Finnish farmers. Int J Epidemiol. 1996;25:760–762. doi: 10.1093/ije/25.4.760. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg LB, Whang W, Shimbo D, Shah A, Shapiro PA, Davidson KW. Exposure to tricyclic antidepressants is associated with an increased risk of incident CHD events in a population-based study. Int J Cardiol. 2010;145:124–125. doi: 10.1016/j.ijcard.2009.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hippisley-Cox J, Pringle M, Hammersley V, Crown N, Wynn A, Meal A, Coupland C. Antidepressants as risk factor for ischaemic heart disease: case-control study in primary care. BMJ. 2001;323:666–669. doi: 10.1136/bmj.323.7314.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tata LJ, West J, Smith C, Farrington P, Card T, Smeeth L, Hubbard R. General population based study of the impact of tricyclic and selective serotonin reuptake inhibitor antidepressants on the risk of acute myocardial infarction. Heart. 2005;91:465–471. doi: 10.1136/hrt.2004.037457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blanchette CM, Simoni-Wastila L, Zuckerman IH, Stuart B. A secondary analysis of a duration response association between selective serotonin reuptake inhibitor use and the risk of acute myocardial infarction in the aging population. Ann Epidemiol. 2008;18:316–321. doi: 10.1016/j.annepidem.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, Hippisley-Cox J. Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ. 2011;343:d4551. doi: 10.1136/bmj.d4551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sauer WH, Berlin JA, Kimmel SE. Selective serotonin reuptake inhibitors and myocardial infarction. Circulation. 2001;104:1894–1898. doi: 10.1161/hc4101.097519. [DOI] [PubMed] [Google Scholar]
- 12.Scherrer JF, Garfield LD, Lustman PJ, Hauptman PJ, Chrusciel T, Zeringue A, Carney RM, Freedland KE, Bucholz KK, Owen R, Newcomer JW, True WR. Antidepressant drug compliance: reduced risk of MI and mortality in depressed patients. Am J Med. 2011;124:318–324. doi: 10.1016/j.amjmed.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 13.Pratt LA, Ford DE, Crum RM, Armenian HK, Gallo JJ, Eaton WW. Depression, psychotropic medication, and risk of myocardial infarction. Prospective data from the Baltimore ECA follow-up. Circulation. 1996;94:3123–3129. doi: 10.1161/01.cir.94.12.3123. [DOI] [PubMed] [Google Scholar]
- 14.Hippisley-Cox J, Fielding K, Pringle M. Depression as a risk factor for ischaemic heart disease in men: population based case-control study. BMJ. 1998;316:1714–1719. doi: 10.1136/bmj.316.7146.1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sauer WH, Berlin JA, Kimmel SE. Effect of antidepressants and their relative affinity for the serotonin transporter on the risk of myocardial infarction. Circulation. 2003;108:32–36. doi: 10.1161/01.CIR.0000079172.43229.CD. [DOI] [PubMed] [Google Scholar]
- 16.Monster TB, Johnsen SP, Olsen ML, McLaughlin JK, Sorensen HT. Antidepressants and risk of first-time hospitalization for myocardial infarction: a population-based case-control study. Am J Med. 2004;117:732–737. doi: 10.1016/j.amjmed.2004.06.027. [DOI] [PubMed] [Google Scholar]
- 17.Smoller JW, Allison M, Cochrane BB, Curb JD, Perlis RH, Robinson JG, Rosal MC, Wenger NK, Wassertheil-Smoller S. Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the Women's Health Initiative study. Arch Intern Med. 2009;169:2128–2139. doi: 10.1001/archinternmed.2009.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whang W, Kubzansky LD, Kawachi I, Rexrode KM, Kroenke CH, Glynn RJ, Garan H, Albert CM. Depression and risk of sudden cardiac death and coronary heart disease in women: results from the Nurses' Health Study. J Am Coll Cardiol. 2009;53:950–958. doi: 10.1016/j.jacc.2008.10.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamer M, David Batty G, Seldenrijk A, Kivimaki M. Antidepressant medication use and future risk of cardiovascular disease: the Scottish Health Survey. Eur Heart J. 2011;32:437–442. doi: 10.1093/eurheartj/ehq438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kimmel SE, Schelleman H, Berlin JA, Oslin DW, Weinstein RB, Kinman JL, Sauer WH, Lewis JD. The effect of selective serotonin re-uptake inhibitors on the risk of myocardial infarction in a cohort of patients with depression. Br J Clin Pharmacol. 2011;72:514–517. doi: 10.1111/j.1365-2125.2011.04008.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pizzi C, Rutjes AW, Costa GM, Fontana F, Mezzetti A, Manzoli L. Meta-analysis of selective serotonin reuptake inhibitors in patients with depression and coronary heart disease. Am J Cardiol. 2011;107:972–979. doi: 10.1016/j.amjcard.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 22.Woolf B. On estimating the relation between blood group and disease. Ann Hum Genet. 1955;19:251–253. doi: 10.1111/j.1469-1809.1955.tb01348.x. [DOI] [PubMed] [Google Scholar]
- 23.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 24.Martinez C, Assimes TL, Mines D, Dell'aniello S, Suissa S. Use of venlafaxine compared with other antidepressants and the risk of sudden cardiac death or near death: a nested case-control study. BMJ. 340:c249. doi: 10.1136/bmj.c249. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salaycik KJ, Kelly-Hayes M, Beiser A, Nguyen AH, Brady SM, Kase CS, Wolf PA. Depressive symptoms and risk of stroke: the Framingham Study. Stroke. 2007;38:16–21. doi: 10.1161/01.STR.0000251695.39877.ca. [DOI] [PubMed] [Google Scholar]
- 26.Surtees PG, Wainwright NW, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Depression and ischemic heart disease mortality: evidence from the EPIC-Norfolk United Kingdom prospective cohort study. Am J Psychiatry. 2008;165:515–523. doi: 10.1176/appi.ajp.2007.07061018. [DOI] [PubMed] [Google Scholar]
- 27.Xue F, Strombom I, Turnbull B, Zhu S, Seeger JD. Cardiovascular events in duloxetine users compared to other depressed and non-depressed subjects. Pharmacoepidemiol Drug Saf. 2009;18:S96. [Google Scholar]
- 28.Pan A, Okereke OI, Sun Q, Logroscino G, Manson JE, Willett WC, Ascherio A, Hu FB, Rexrode KM. Depression and incident stroke in women. Stroke. 2011;42:2770–2775. doi: 10.1161/STROKEAHA.111.617043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xue F, Strombom I, Turnbull B, Zhu S, Seeger J. Treatment with duloxetine in adults and the incidence of cardiovascular events. J Clin Psychopharmacol. 2012;32:23–30. doi: 10.1097/JCP.0b013e31823fb238. [DOI] [PubMed] [Google Scholar]
- 30.Taylor CB, Youngblood ME, Catellier D, Veith RC, Carney RM, Burg MM, Kaufmann PG, Shuster J, Mellman T, Blumenthal JA, Krishnan R, Jaffe AS ENRICHD Investigators. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry. 2005;62:792–798. doi: 10.1001/archpsyc.62.7.792. [DOI] [PubMed] [Google Scholar]
- 31.Chen Y, Guo JJ, Patel NC. Hemorrhagic stroke associated with antidepressant use in patients with depression: does degree of serotonin reuptake inhibition matter? Pharmacoepidemiol Drug Saf. 2009;18:196–202. doi: 10.1002/pds.1699. [DOI] [PubMed] [Google Scholar]
- 32.Winterstein AG, Gerhard T, Kubilis P, Saidi A, Linden S, Crystal S, Zito J, Shuster JJ, Olfson M. Cardiovascular safety of central nervous system stimulants in children and adolescents: population based cohort study. BMJ. 2012;345:e4627. doi: 10.1136/bmj.e4627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Caso V, Santalucia P, Pezzella FR. Depression and stroke risk. Womens Health (Lond Engl) 2012;8:35–37. doi: 10.2217/whe.11.85. [DOI] [PubMed] [Google Scholar]
- 34.Abas M, Hotopf M, Prince M. Depression and mortality in a high-risk population. 11-Year follow-up of the Medical Research Council Elderly Hypertension Trial. Br J Psychiatry. 2002;181:123–128. [PubMed] [Google Scholar]
- 35.Ray JG, Mamdani MM, Yeo EL. Antipsychotic and antidepressant drug use in the elderly and the risk of venous thromboembolism. Thromb Haemost. 2002;88:205–209. [PubMed] [Google Scholar]
- 36.Jick SS, Li L. Antidepressant drug use and risk of venous thromboembolism. Pharmacotherapy. 2008;28:144–150. doi: 10.1592/phco.28.2.144. [DOI] [PubMed] [Google Scholar]
- 37.Mast ST, Gersing KR, Anstrom KJ, Krishnan KR, Califf RM, Jollis JG. Association between selective serotonin-reuptake inhibitor therapy and heart valve regurgitation. Am J Cardiol. 2001;87:989–993. doi: 10.1016/s0002-9149(01)01435-7. [DOI] [PubMed] [Google Scholar]
- 38.Tiihonen J, Lonnqvist J, Wahlbeck K, Klaukka T, Tanskanen A, Haukka J. Antidepressants and the risk of suicide, attempted suicide, and overall mortality in a nationwide cohort. Arch Gen Psychiatry. 2006;63:1358–1367. doi: 10.1001/archpsyc.63.12.1358. [DOI] [PubMed] [Google Scholar]
- 39.Seifert CL, Poppert H, Sander D, Feurer R, Etgen T, Ander KH, Pürner K, Brönner M, Sepp D, Kehl V, Förstl H, Bickel H. Depressive symptoms and the risk of ischemic stroke in the elderly – influence of age and sex. PLoS One. 2012;7:e50803. doi: 10.1371/journal.pone.0050803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Majed B, Arveiler D, Bingham A, Ferrieres J, Ruidavets JB, Montaye M, Appleton K, Haas B, Kee F, Amouyel P, Ducimetiere P, Empana JP PRIME Study Group. Depressive symptoms, a time-dependent risk factor for coronary heart disease and stroke in middle-aged men: the PRIME Study. Stroke. 2012;43:1761–1767. doi: 10.1161/STROKEAHA.111.645366. [DOI] [PubMed] [Google Scholar]
- 41.Castro VM, Gallagher PJ, Clements CC, Murphy SN, Gainer VS, Fava M, Weilburg JB, Churchill SE, Kohane IS, Iosifescu DV, Smoller JW, Perlis RH. Incident user cohort study of risk for gastrointestinal bleed and stroke in individuals with major depressive disorder treated with antidepressants. BMJ Open. 2012;2:e000544. doi: 10.1136/bmjopen-2011-000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li CT, Bai YM, Tu PC, Lee YC, Huang YL, Chen TJ, Chang WH, Su TP. Major depressive disorder and stroke risks: a 9-year follow-up population-based, matched cohort study. PLoS One. 2012;7:e46818. doi: 10.1371/journal.pone.0046818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.D'Cruz S, Sachdev A, Tiwari P. Adverse drug reactions & their risk factors among Indian ambulatory elderly patients. Indian J Med Res. 2012;136:404–410. [PMC free article] [PubMed] [Google Scholar]
- 44.Hung CC, Lin CH, Lan TH, Chan CH. The association of selective serotonin reuptake inhibitors use and stroke in geriatric population. Am J Geriatr Psychiatry. 21:811–815. doi: 10.1016/j.jagp.2013.01.018. 2013. [DOI] [PubMed] [Google Scholar]
- 45.Nabi H, Kivimaki M, Suominen S, Koskenvuo M, Singh-Manoux A, Vahtera J. Does depression predict coronary heart disease and cerebrovascular disease equally well? The Health and Social Support Prospective Cohort Study. Int J Epidemiol. 2010;39:1016–1024. doi: 10.1093/ije/dyq050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schlienger RG, Meier CR. Effect of selective serotonin reuptake inhibitors on platelet activation: can they prevent acute myocardial infarction? Am J Cardiovasc Drugs. 2003;3:149–162. doi: 10.2165/00129784-200303030-00001. [DOI] [PubMed] [Google Scholar]
- 47.Stollerman GH, Bisno AL. Antidepressants and myocardial infarction. Hosp Pract. 2000;35:26–141. [Google Scholar]
- 48.Glassman AH, O'Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT, Jr, Krishnan KR, van Zyl LT, Swenson JR, Finkel MS, Landau C, Shapiro PA, Pepine CJ, Mardekian J, Harrison WM, Barton D, McLvor M. Sertraline Antidepressant Heart Attack Randomized Trial (SADHEART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701–709. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 49.Lespérance F, Frasure-Smith N, Koszycki D, Laliberté MA, van Zyl LT, Baker B, Swenson JR, Ghatavi K, Abramson BL, Dorian P, Guertin MC CREATE Investigators. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;297:367–379. doi: 10.1001/jama.297.4.367. [DOI] [PubMed] [Google Scholar]
- 50.Pizzi C, Mancini S, Angeloni L, Fontana F, Manzoli L, Costa GM. Effects of selective serotonin reuptake inhibitor therapy on endothelial function and inflammatory markers in patients with coronary heart disease. Clin Pharmacol Ther. 2009;86:527–532. doi: 10.1038/clpt.2009.121. [DOI] [PubMed] [Google Scholar]
- 51.Pizzi C, Manzoli L, Mancini S, Bedetti G, Fontana F, Costa GM. Autonomic nervous system, inflammation and preclinical carotid atherosclerosis in depressed subjects with coronary risk factors. Atherosclerosis. 2010;212:292–298. doi: 10.1016/j.atherosclerosis.2010.04.038. [DOI] [PubMed] [Google Scholar]
- 52.Penninx BW, Beekman AT, Honig A, Deeg DJ, Schoevers RA, van Eijk JT, van Tilburg W. Depression and cardiac mortality: results from a community-based longitudinal study. Arch Gen Psychiatry. 2001;58:221–227. doi: 10.1001/archpsyc.58.3.221. [DOI] [PubMed] [Google Scholar]
- 53.Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry. 1998;55:580–592. doi: 10.1001/archpsyc.55.7.580. [DOI] [PubMed] [Google Scholar]
- 54.Zellweger MJ, Osterwalder RH, Langewitz W, Pfisterer ME. Coronary artery disease and depression. Eur Heart J. 2004;25:3–9. doi: 10.1016/j.ehj.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 55.O'Connor CM, Jiang W, Kuchibhatla M, Mehta RH, Clary GL, Cuffe MS, Christopher EJ, Alexander JD, Califf RM, Krishnan RR. Antidepressant use, depression, and survival in patients with heart failure. Arch Intern Med. 2008;168:2232–2237. doi: 10.1001/archinte.168.20.2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet. 1999;353:89–92. doi: 10.1016/S0140-6736(98)10279-9. [DOI] [PubMed] [Google Scholar]