Abstract
Background
Demand management defines any method used to monitor, direct, or regulate patient referrals. Strategies have been developed to manage the referral of patients to secondary care, with interventions that target primary care, specialist services, or infrastructure.
Aim
To review the international evidence on interventions to manage referral from primary to specialist care.
Design and setting
Systematic review.
Method
Iterative, systematic searches of published and unpublished sources public health, health management, management, and grey literature databases from health care and other industries were undertaken to identify recent, relevant studies. A narrative synthesis of the data was completed to structure the evidence into groups of similar interventions.
Results
The searches generated 8327 unique results, of which 140 studies were included. Interventions were grouped into four intervention categories: GP education (n = 50); process change (n = 49); system change (n = 38); and patient-focused (n = 3). It is clear that there is no ‘magic bullet’ to managing demand for secondary care services: although some groups of interventions may have greater potential for development, given the existing evidence that they can be effective in specific contexts.
Conclusions
To tackle demand management of primary care services, the focus cannot be on primary care alone; a whole-systems approach is needed because the introduction of interventions in primary care is often just the starting point of the referral process. In addition, more research is needed to develop and evaluate interventions that acknowledge the role of the patient in the referral decision.
Keywords: demand management, general practice, narrative synthesis, primary care, referral, systematic review
INTRODUCTION
Demand management defines any method used to monitor, direct, or regulate patient referrals, including the methods by which patients are referred from primary care to specialist, non-emergency care provided in hospital. This interface between primary and secondary care is a pivotal organisational feature in many healthcare systems, including the NHS.1
As demand outstrips resources in the UK, the volume and appropriateness of referrals from primary care to specialist services has become a key concern in the NHS. The NHS needs to make recurrent efficiency savings of up to £20 billion over 4 years,2 but current policy direction means that primary care funding is prioritised. This desire to shift resources to primary care means that demand management of secondary care services is needed.
As a result, several strategies have been developed to manage the referral of patients to secondary care. Referral management should not focus solely on reducing demand, but on ensuring that the right patients receive the right care, at the right time.3
A previous Cochrane review 4 in this area was limited to high-quality, controlled studies and found only 17 published papers. The authors concluded that there was insufficient evidence on organisational and financial interventions aimed at primary care, and inconclusive evidence on effective educational interventions. A report by the King’s Fund5 also highlighted the concerns of many with regard to the risks of managing demand without taking account of patient safety, and acknowledging that referral management has the capacity to increase clinical risk, as well as to reduce it. The current study aimed to go beyond previous reviews in the area by conducting an inclusive review of a broad range of evidence (from multiple sources) encompassing all study designs.
METHOD
This research was designed to answer the following question: what can be learned from the international evidence on interventions to manage referral from primary to specialist care? The inclusion criteria were:
Participants: primary care physicians, hospital specialists, and their patients.
Interventions: interventions that aim to influence and/or affect referral from primary care to specialist services by having an impact on the referral practices of the primary physician.
Comparators: the main comparator condition was the usual method of referral practice that is undertaken in the location where the intervention is being implemented. However, alternative comparators have not been excluded. Studies with no concurrent comparator (such as non-controlled before and after studies) were also included.
Outcomes: all outcomes relating to referral were considered including: referral rate, referral quality, appropriateness of referral, impact on existing service provision, costs, mortality and morbidity outcomes, length of stay in hospital, safety, effectiveness, patient satisfaction, patient experience, and process measures (such as referral variation and conversion rates).
Study design: with the increasing recognition in the literature that a broad range of evidence is needed to inform review findings, no restrictions were placed on study design. The criterion for inclusion in the review was that a study was able to answer or inform the research question. However, it has been noted that the quality of the study design and execution may affect the reliability of the results generated.
How this fits in
Demand management defines any method used to monitor, direct or regulate patient referrals, including referral from primary care to hospital. Previous reviews in the area have taken a focused inclusion criteria; this study took an inclusive approach to include all study designs and a broad range of public health, health management, management, and grey literature databases. Despite identifying 140 intervention papers, it is clear that there is no ‘magic bullet’ to managing demand for secondary care services: the perfect solution does not exist. To tackle demand management of primary care services, the focus cannot be on primary care alone: a whole-systems approach is needed because the introduction of interventions in primary care is often just the starting point of the referral process.
Iterative6,7 systematic searches of published and unpublished sources from health care and other industries were undertaken to identify recent, relevant studies. Searches were limited by date (January 2000 to July 2013). An initial search was generated with free text and subject heading terms combined to address the concepts of ‘primary care’ and ‘referral’ (Box 1). A broad range of public health, health management, management, and grey literature databases were searched (Box 2). After the initial search, phrase searches were undertaken for ‘referral management centres’ and ‘patient-focused interventions’ to make sure that papers had not been missed that were relevant to demand management. Citation searches of included articles and systematic reviews, and reference list checking of included articles, were also undertaken.
Box 1. Main search strategy.
Database: Ovid MEDLINE® In-Process & Other Non-Indexed Citations and Ovid MEDLINE® < 1946 to present>
*Primary Health Care/ (31226)
(primary care or general practitioner$ or gp).ti. (38162)
*Family practice/ or *General practitioners/(38225)
1 or 2 or 3 (83924)
(referral or referred or refer).ti. (10316)
demand management.ti,ab. (141)
*”Referral and Consultation”/ (17682)
Specialization/ (20898)
5 or 6 or 7 or 8 (43885)
4 and 9 (4328)
limit 10 to yr = ”2000–Current” (1978)
Box 2. Data sources.
MEDLINE In-Process and Other Non-Indexed Citations and MEDLINE via Ovid <1946 to present>
Cochrane Database of Systematic Reviews
Cochrane Central Register of Controlled Trials
Cochrane Methodology Register
Database of Abstracts of Reviews of Effects
Health Technology Assessment Database
NHS Economic Evaluation Database
All accessed via the Cochrane Library, published by John Wiley and Sons Ltd <from inception>
CINAHL via EBSCO <from inception>
Embase via Ovid <1974 to 2012 November 13 >
PsycINFO via Ovid <1806 to November Week 1 2012>
Science Citation Index, Social Science Citation Index, Science Conference Papers Index, Social Science
Conference Papers Index via Web of Science published by Thomson Reuters <from inception>
Scopus via Elsevier <from inception>
Applied Social Sciences Index and Abstracts (ASSIA) via ProQuest <from inception >
Sociological abstracts via ProQuest <from inception >
Social policy and practice via Ovid <1890s to October 2012>
International Bibliography of the Social Sciences (IBSS) via Proquest <from inception >
HMIC via NHS Evidence <from inception>
Health business Elite via EBSCO <from inception>
Business source premier via EBSCO <from inception >
Emerald management reviews via http://www.emeraldinsight.com/products/reviews/index.htm <from inception>
EPPI Centre databases: Bibliomap, Database of Promoting Health Effectiveness Reviews (DoPHER), Trials
Register of Promoting Health Interventions (TRoPHI) via http://eppi.ioe.ac.uk/ <from inception >
OpenGrey via http://www.opengrey.eu/ <from inception>
Opensource via http://www.greynet.org/greysourceindex.html <from inception>
Google Scholar via http://scholar.google.co.uk/ <from inception >
Titles and abstracts (where available) of papers were independently screened for inclusion by two reviewers, with disputes resolved by consulting other team members. Full paper copies of potentially relevant articles were retrieved for systematic screening. A data extraction form was developed using the previous expertise of the review team, trialled using a small number of papers, and refined for use here. Data extractions were completed by one reviewer and checked by a second. Non-English language articles with English abstracts were considered for translation.
The internal and external validity of studies was assessed using quality appraisal checklists based on work by the Cochrane Collaboration on risk of bias.8 Each paper was assessed by one reviewer and checked for accuracy by a second. Each paper was graded on a 3-point scale as being at higher risk of bias, lower risk of bias, or unclear risk of bias.8 Quality criteria for inclusion in the review were not set because the work was intended to be broad-based and inclusive; however, an account was taken of quality standards in the synthesis and presentation of the evidence as outlined below.
The strength of the evidence was also considered for each element of the intervention typology. Each group of papers was graded as stronger evidence, weaker evidence, inconsistent evidence, or no evidence (using criteria from Hoogendoorn et al ).9
RESULTS
The heterogeneity of the interventions’ aim, design, and outcome measures used preclude a meta-analysis. A narrative synthesis of the data was therefore undertaken to generate a typology of interventions and to explore the evidence for impact (or lack of impact) on outcomes.
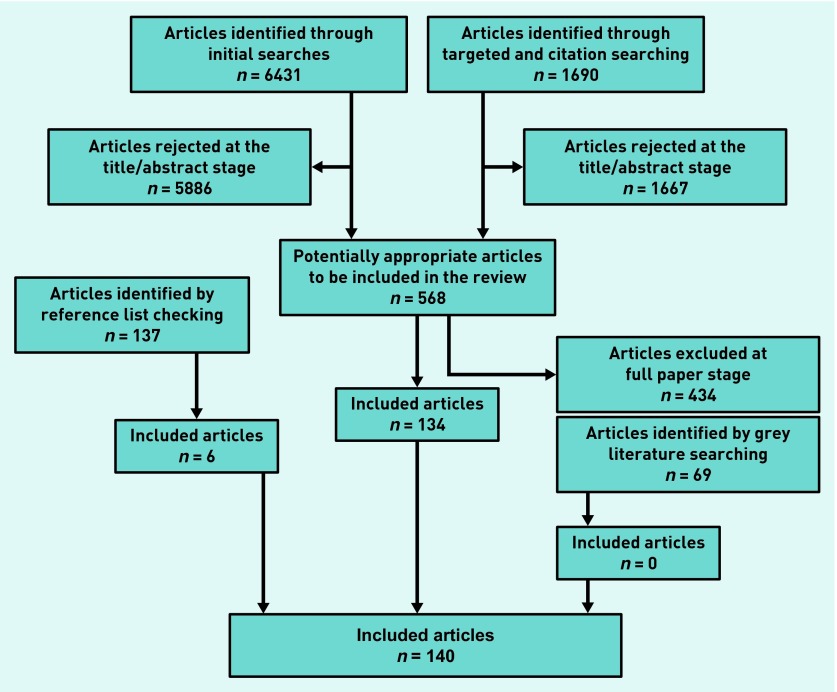
One hundred and forty studies met the inclusion criteria for the review (Figure 1).10–150 Most studies (n = 121) were considered to be at lower risk for bias. Nineteen intervention studies were considered to be at higher (or unclear) risk of bias. The main risks for increased bias were related to a lack of participant details, only narrative results, single-point percentages reported without supporting statistics, data reported as charts only, inconsistencies in data reporting, poor response rates, attrition rate not reported, weak outcome measures, unclear study design, and evaluation tools that asked questions that strongly led responders towards positive answers.
Figure 1.
Quorum diagram of included articles .
Studies included 44 randomised controlled trials (including 19 of cluster design), five non-randomised controlled trials, 43 before and after studies (without a concurrent control group), three controlled before and after studies, one case-control study, one economic analysis, five cohort studies, and 38 evaluation studies (described variably as audits, review, evaluation, and retrospective data analysis). Most were conducted in the UK (n = 83) or the US (n = 20). There were 10 studies from the Netherlands and nine from Australia. Additional studies were conducted in Canada (n = 3), Israel (n = 3), Italy (n = 3), Denmark (n = 2), Spain (n = 2), Finland (n = 1), Norway (n = 1), Hong Kong (n = 1), UK/China (n = 1), and one study where the country of origin was unclear.
The 140 studies were used to create a typology of studies by intervention. The studies were grouped into four intervention categories: GP education (n = 50); process change (n = 49); system change (n = 38); and patient-focused (n = 3). Table 1 gives a summary of the number of papers identified and the quality grading given to the evidence for each type of intervention.
Table 1.
Summary of intervention typology and quality appraisal
| Intervention category | Intervention type | Positive effect (high bias) | No effect (high bias) | Strength of evidence |
|---|---|---|---|---|
| GP education | Peer review and training/feedback | 4 (1) | 0 | i |
| GP training: professional development | 10 (1) | 7 (2) | iii | |
| Guidelines (no training/feedback) | 7 (2) | 5 | iii | |
| Guidelines with training/feedback/specialist support | 11 | 6 | iii | |
|
| ||||
| Process change | Designated appointment slots/fast-track clinic | 4 (1) | 2 | iii |
| Direct access to screening/diagnostic testing | 6 | 3 | iii | |
| Specialist consultation before referral | 11 (3) | 0 | i | |
| Electronic referral | 9 (1) | 1 | i | |
| Decision support tool | 6 | 4 | iii | |
| Waiting list review | 1 | 2 | iii | |
|
| ||||
| System change | Additional primary care staff | 0 | 3 (1) | i (−ve) |
| Community provision of ‘specialist’ services by GPs | 7 | 2 (1) | i | |
| Outreach: community provision by specialists | 8 | 2 (1) | i | |
| Return of inappropriate referrals | 2 (1) | 0 | ii | |
| Gatekeeping | 0 | 4 (1) | iii | |
| Payment system | 1 | 3 (1) | iii | |
| Referral management centre | 3 (2) | 3 | iii | |
|
| ||||
| Patient inventions | Patient education | 1 | 1 | iii |
| Patient concerns and satisfaction | 1 | 0 | iii | |
i = stronger evidence. ii = weaker evidence. iii = conflicting or no evidence (evidence from one study). [–ve] = negative affect on referral outcomes. Adapted from the method of Hoogendoorn et al 1999.
GP education interventions were defined as any intervention with a primary focus on GP education or training. The GP education intervention group included peer review and feedback (n = 4),10–13 interventions which consisted of formal GP training (including continued professional development) (n = 17),14–30 and the issuing of guidelines (without [n = 12]31–42 or with [n = 17]43–59 additional formal training and support for practitioners). The overall picture for interventions that aim to moderate referral processes by educating GPs is mixed, but some groups of interventions with more positive outcomes have been identified, including in particular peer review and feedback interventions (positive effects on referral, expenditure, and referral letter quality), as well as some elements of formal GP training (positive effects on referral rate, appropriate referrals, GP knowledge, consultation quality, and patient waiting time). However, given the variety of interventions reported, more research is needed to identify key successful interventions or particular elements of interventions that are more likely to be successful.
Process changes were defined as small-scale changes to some aspect of the individual referral process that did not involve the movement of staff or relocation of clinics, the methods in which referrals were triaged at hospital, or financial arrangements for referral. Process change interventions included: designated appointment slots and fast-track clinics for primary care referrals (n = 6),60–65 direct access to screening (n = 9),66–74 specialist consultation prior to referral (individual contact between a specialist and GP) (n = 11),75–85 electronic referral systems (n = 10),86–95 decision support tools (n = 10),96–105 and waiting list review or watchful waiting (n = 3).106–108 The overall picture for interventions that aim to moderate referral outcomes by changing an element of the referral process is mixed. Stronger evidence exists for electronic referral interventions (positive effects on referral, appropriate referral, GP satisfaction, reduction in non-attendance, waiting times, and transfer of information) and interventions including specialist consultation prior to referral (positive effects on number of referrals [referrals avoided], time to treatment, accuracy of diagnosis, and patient evaluation of services). These interventions are designed to provide better quality information to the specialist, either before or as part of a formal referral process.
System changes were identified as large changes impacting on all referrals made that involved the movement of staff or relocation clinics, the methods in which all referrals were triaged at hospital, or financial arrangements for referrals. System change interventions included the community provision of specialist services by GPs (n = 9),108–117 outreach or community provision by specialists (whole-scale provision of a hospital service within the community) (n = 10),118–127 return of inappropriate referrals (n = 2),128,129 the provision of additional primary care staff (n = 3),130–132 the addition or removal of gatekeeping systems (requiring a primary care provider to give access to secondary care services) (n = 4),133–136 changes to payment systems (n = 4),137–139 and referral management centre or other major triage systems (n = 6).140–146 The overall picture for interventions that aim to implement large system changes to impact on referral is mixed. Two of the types of interventions for which stronger evidence was identified involved the provision of specialist services in the community: either outreach/community provision by specialists or community provision of specialist services by specially trained GPs (positive effects on referral rate, appropriate referrals, patient satisfaction, and service accessibility). Stronger evidence also existed to suggest that the provision of additional staff in primary care (for example, nurses or counsellors) had a negative effect on referral outcomes. Some system change interventions conducted internationally such as those based on US healthcare payment systems, or where enormous change to the NHS system would be required (such as the removal of gatekeeping to secondary care services) would be impractical to implement in the NHS.
Very few examples were found of patient-focused interventions with outcomes relevant to managing demand. There is of course a large literature on patient education and activation measures, but this reports different outcome measures and was beyond the scope of the current review. The patient-focused interventions included the provision of health information/education (n = 2),146,147 and an intervention to address patient concerns and satisfaction (n = 1).148 The education interventions were graded as inconsistent and the patient concern intervention was graded as no evidence. This highlights a significant lack of evidence for patient-focused interventions, despite the huge potential impact that patients may have on the referral process.
DISCUSSION
Summary
It is clear that there is no ‘magic bullet’ to managing demand for secondary care services: the perfect solution does not exist and issues such as the context of a particular specialty or the location of a service impacts on the generalisability of interventions. In addition, the balance of the evidence is hard to interpret because some interventions that were reported frequently (such as referral guidelines) are supported by a contradictory evidence base and also receive mixed support from GPs and specialists. However, some groups of interventions may have greater potential for development, given the existing evidence that they can be effective in specific contexts.
It appears that GP peer review and feedback within a practice can be successful in changing referral practice and that providing training (or reinforcement) of guidelines can go some way to improving effectiveness. Process changes appear to be most effective when they result in the specialist being provided with more or better quality information about the patient; either electronically or through specialist consultation prior to the formal referral being made. The same is true in the most part for larger system changes. The community provision of specialist services by GPs (having been previously trained by specialists), outreach or community provision by specialists, and the return of inappropriate referrals, all engage the specialist and show the strongest positive effect on referral outcomes.
However, the evidence suggests that the addition of other primary care staff (such as nurses or counsellors) into a GP practice can increase the referral rate and reduce appropriateness of referral (although the amount of evidence was limited). The evidence for gatekeeping systems overall was very inconsistent and appeared to suggest that adding or removing a gatekeeping system had no positive impact on referral (although there were possibly small negative effects), although the evidence here was weaker. The same was true of payment system changes. However, it is also true that most of these US interventions would not be applicable or relevant in the UK within the NHS context.
Despite additional targeted searches, there was a significant lack of an evidence base to support referral management centres or other large triage systems. It was also surprising to find an almost complete lack of patient-focused interventions. This is particularly relevant given the potential impact that the patient may have on the referral decision.
Strengths and limitations
At times it was difficult to establish which outcome measures should be considered as positive, for example where interventions encourage referrals irrespective of their appropriateness, or where quicker referral processes are created, because these have a cost implication.
Deliberately inclusive search criteria were chosen including all study designs and grey literature sources in order to identify the most evidence and to develop the evidence base beyond previously conducted reviews. However, it is important to acknowledge that this creates an evidence base of mixed quality, for example, where study designs differ. This variation in quality has been considered as discussed above.
Although the evidence identified here is international in nature and some of it originates from countries with very different healthcare systems and processes to the UK, most studies have relevance in the UK within an NHS setting. It is likely that differences between specialties, UK demographic variation, and the impact of individual patients and practitioners will have an even stronger impact on the effectiveness of the interventions identified than their country of origin. There are two exceptions to this, namely, the addition or removal of gatekeeping systems and changes to healthcare payment systems. It would not be possible to make these types of changes in the UK; however, very few studies were identified in either of these categories and the evidence in both cases was conflicting.
Comparison with existing literature
The current study builds on previous reviews in the area4,5 by taking much broader inclusion criteria to create a more complete picture of interventions to manage referral from primary to specialist care. An inclusive approach was taken to include all study designs and a broad range of public health, health management, management, and grey literature databases. Consideration of a wider range of evidence helps to explain the mixed outcomes from more carefully controlled evaluations, and demonstrates the complexity and range of types of interventions that might be explored to address the overall problem of how to improve the referral process.
Implications for research and practice
To tackle demand management of primary care services, the focus cannot be on primary care alone; a whole-systems approach is needed because the introduction of interventions in primary care is often just the starting point of the referral process. Patton150 identified a ‘systems perspective as becoming increasingly important in dealing with and understanding real-world complexities’. With the introduction of interventions in primary care there are likely to be implications for secondary care. Furthermore, in a climate of ‘payment by results’, any intervention that reduces secondary care activity means a loss of income to secondary care and the implications of this would require consideration.
There are limitations in adopting this approach to demand management, because of the complexity of health systems. System designers need to be more mindful of the multitude of influencing factors and potential consequences from any given intervention. With this in mind, the authors have developed a logic model to illustrate the complexity of managing this demand.151
More research is needed to develop and evaluate interventions that acknowledge the role of the patient in the referral decision. Demand management is driven by the desire to reduce patient numbers and costs. It is therefore focused on process not outcome. Research is needed to examine what effect interventions focused on patient outcomes may have on demand (for example, would better care lead to less need for services?).
Acknowledgments
The authors would like to acknowledge the members of their steering group for their invaluable contribution to this research: Dr Martin McShane (NHS England), Professor Danuta Kasprzyk (Department of Global Health, University of Washington), Professor Helena Britt (Family Medicine Research Centre, University of Sydney), Ellen Nolte (RAND Corporation Europe/international), Jon Karnon (School of Population Health and Clinical Practice, University of Adelaide), Christine Allmark (Patient and Public Involvement [PPI]), and Brian Hodges (PPI).
Funding
This project was funded by the National Institute for Health Research (Health Service and Delivery Research Programme; project number11/1022/01). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Health Service and Delivery Research Programme, NIHR, the NHS or the Department of Health. This paper represents emerging findings from a larger systematic review and logic model development project (http://www.nets.nihr.ac.uk/projects/hsdr/11102201).
Ethical approval
Ethical approval was not required for the secondary data analysis presented here.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have no competing interests to declare.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.The King’s Fund. An alternative guide to the new NHS in England. London: The King’s Fund; 2013. http://www.kingsfund.org.uk/projects/nhs-65/alternative-guide-new-nhs-england (accessed 15 Oct 2014) [Google Scholar]
- 2.Jones NM, Charlesworth A. The anatomy of health spending 2011/12. London: Nuffield Trust; 2013. http://www.nuffieldtrust.org.uk/sites/files/nuffield/publication/130305_anatomy-health-spending.pdf (accessed 15 Oct 2014) [Google Scholar]
- 3.Lee A, Blank L, Payne N, et al. Demand management: misguided solutions? Br J Gen Pract. 2013 doi: 10.3399/bjgp13X670859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akbari A, Mayhew A, Al-Alawi MA, et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst Rev. 2008;(4):CD005471. doi: 10.1002/14651858.CD005471.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imison C, Naylor C. Referral management: lessons for success. London: The King’s Fund; 2010. http://www.kingsfund.org.uk/sites/files/kf/Referral-management-lessons-for-success-Candace-Imison-Chris-Naylor-Kings-Fund-August2010.pdf (accessed 15 Oct 2014) [Google Scholar]
- 6.Evidence for Policy and Practice Information and Co-ordinating Centre. EPPI-Centre methods for conducting systematic reviews. Updated 2010. http://eppi.ioe.ac.uk/cms/LinkClick.aspx?fileticket=hQBu8y4uVwI%3D&tabid=88 (accessed 15 Oct 2014)
- 7.Grant MJ, Brettle A, Long AF. Developing a review question: a spiral approach to literature searching. Poster presentation 3rd Symposium on Systematic Reviews: Beyond the basics Improving quality and impact; 3–5 July 2000; Oxford. [Google Scholar]
- 8.Higgins JPT, Altman DG. Higgins JPT, Green S, editors. Assessing risk of bias in included studies. Cochrane handbook for systematic reviews of interventions. 2008. Version 5.0.1. The Cochrane Collaboration. http://hiv.cochrane.org/sites/hiv.cochrane.org/files/uploads/Ch08_Bias.pdf (accessed 29 Oct 2014)
- 9.Hoogendoorn WE, van Poppel MN, Bongers PM, et al. Physical load during work and leisure time as risk factors for back pain. Scand J Work Environ Health. 1999;25(5):387–403. doi: 10.5271/sjweh.451. [DOI] [PubMed] [Google Scholar]
- 10.Cooper R. How peer review reduced GP referrals by 25% in two months. Pulse. 2012;72(10):31. [Google Scholar]
- 11.Evans E. The Torfaen referral evaluation project. Qual Prim Care. 2009;17(6):423–429. [PubMed] [Google Scholar]
- 12.Evans E, Aiking H, Edwards A. Reducing variation in general practitioner referral rates through clinical engagement and peer review of referrals: a service improvement project. Qual Prim Care. 2011;19(4):263–272. [PubMed] [Google Scholar]
- 13.Jiwa M, Walters S, Mathers N. Referral letters to colorectal surgeons: the impact of peer-mediated feedback. Br J Gen Pract. 2004;54(499):123–126. [PMC free article] [PubMed] [Google Scholar]
- 14.Ramsay CR, Eccles M, Grimshaw JM, Steen N. Assessing the long-term effect of educational reminder messages on primary care radiology referrals. Clin Radiol. 2003;58(4):319–321. doi: 10.1016/s0009-9260(02)00524-x. [DOI] [PubMed] [Google Scholar]
- 15.Shariff Z, Roshan A, Williams AM, Platt AJ. 2-Week wait referrals in suspected skin cancer: does an instructional module for general practitioners improve diagnostic accuracy? Surgeon. 2010;8(5):247–251. doi: 10.1016/j.surge.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Kousgaard KR, Nielsen JD, Olesen F, Jensen AB. General practitioner assessment of structured oncological information accompanying newly referred cancer patients. Scand J Prim Health Care. 2003;21(2):110–114. doi: 10.1080/02813430310001725. [DOI] [PubMed] [Google Scholar]
- 17.Bennett K, Haggard M, Churchill R, Wood S. Improving referrals for glue ear from primary care: are multiple interventions better than one alone? J Health Serv Res Policy. 2001;6(3):139–144. doi: 10.1258/1355819011927387. [DOI] [PubMed] [Google Scholar]
- 18.Donohoe ME, Fletton JA, Hook A, et al. Improving foot care for people with diabetes mellitus: a randomized controlled trial of an integrated care approach. Diabet Med. 2000;17(8):581–587. doi: 10.1046/j.1464-5491.2000.00336.x. [DOI] [PubMed] [Google Scholar]
- 19.Watson E, Clements A, Yudkin P, et al. Evaluation of the impact of two educational interventions on GP management of familial breast/ovarian cancer cases: a cluster randomised controlled trial. Br J Gen Pract. 2001;51(471):817–821. [PMC free article] [PubMed] [Google Scholar]
- 20.Adams SG, Pitts J, Wynne J, et al. Effect of a primary care continuing education program on clinical practice of chronic obstructive pulmonary disease: translating theory into practice. Mayo Clin Proc. 2012;87(9):862–870. doi: 10.1016/j.mayocp.2012.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhalla RK, Unwin D, Jones TM, Lesser T. Does clinical assistant experience in ENT influence general practitioner referral rates to hospital? J Laryngol Otol. 2002;116(8):586–588. doi: 10.1258/00222150260171542. [DOI] [PubMed] [Google Scholar]
- 22.Ellard R, Gulati A, Hubbard V, et al. The impact of physician education on primary care referrals in dermatology [abstract] Br J Dermatol. 2012;167(Suppl 1):P41. [Google Scholar]
- 23.Emmerson WB, Frost A, Powell JL, et al. Evaluating a GP consultative psychiatric service in an Australian metropolitan hospital district. Australas Psychiatry. 2003;11(2):195–198. [Google Scholar]
- 24.Hands S, Holbrook J. Are one-to-one outpatient teaching sessions a useful way for GPs to undertake their continuing education? Educ Prim Care. 2001;12(4):392–400. [Google Scholar]
- 25.Hilty DM, Yellowlees PM, Nesbitt TS. Evolution of telepsychiatry to rural sites: changes over time in types of referral and in primary care providers’ knowledge, skills and satisfaction. Gen Hosp Psychiatry. 2006;28(5):367–373. doi: 10.1016/j.genhosppsych.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 26.Lam TP, Chow RW, Lam KF, et al. Evaluation of the learning outcomes of a year-long postgraduate training course in community geriatrics for primary care doctors. Arch Gerontol Geriatr. 2011;52(3):350–356. doi: 10.1016/j.archger.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 27.Lester H, Birchwood M, Freemantle N, et al. REDIRECT: cluster randomised controlled trial of GP training in first-episode psychosis. Br J Gen Pract. 2009 doi: 10.3399/bjgp09X420851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rowlands G, Sims J, Kerry S, et al. Within-practice educational meetings and GP referrals to secondary care: an aid to reflection and review of clinical practice. Educ Prim Care. 2003;14(4):449–462. [Google Scholar]
- 29.Suris X, Cerdà D, Ortiz-Santamaría V, et al. A rheumatology consultancy program with general practitioners in Catalonia, Spain. J Rheumatol. 2007;34(6):1328–1331. [PubMed] [Google Scholar]
- 30.Wolters R, Wensing M, Klomp M, et al. Effects of distance learning on clinical management of LUTS in primary care: a randomised trial. Patient Educ Couns. 2005;59(2):212–218. doi: 10.1016/j.pec.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 31.Malik A, Wigney L, Murray S, Gerrand CH. The effectiveness of ‘two-week’ referrals for suspected bone and soft tissue sarcoma. Sarcoma. 2007 doi: 10.1155/2007/23870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Twomey P. Making the best use of a radiology department: an example of implementation of a referral guideline within a primary care organisation. Qual Prim Care. 2003;11(1):53–59. [Google Scholar]
- 33.Cusack CM, Buckley CC. Efficacy of issuing guidelines on acne management to general practitioners. Br J Dermatol. 2005;152(6):1392–1393. doi: 10.1111/j.1365-2133.2005.06641.x. [DOI] [PubMed] [Google Scholar]
- 34.Idiculla JM, Perros P, Frier BM. Do diabetes guidelines influence the content of referral letters by general practitioners to a diabetes specialist clinic? Health Bull (Edinb) 2000;58(4):322–327. [PubMed] [Google Scholar]
- 35.Lucassen A, Watson E, Harcourt J, et al. Guidelines for referral to a regional genetics service: GPs respond by referring more appropriate cases. Fam Pract. 2001;18(2):135–140. doi: 10.1093/fampra/18.2.135. [DOI] [PubMed] [Google Scholar]
- 36.Potter S, Govindarajulu S, Shere M, et al. Referral patterns, cancer diagnoses, and waiting times after introduction of two week wait rule for breast cancer: prospective cohort study. BMJ. 2007;335(7614):288–290. doi: 10.1136/bmj.39258.688553.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Imkampe A, Bendall S, Chianakwalam C. Two-week rule: has prioritisation of breast referrals by general practitioners improved? Breast. 2006;15(5):654–658. doi: 10.1016/j.breast.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 38.Fearn S, Larner AJ. Have Quality and Outcomes Framework Depression Indicators changed referrals from primary care to a dedicated memory clinic? Ment Health Fam Med. 2009;6(3):129–132. [PMC free article] [PubMed] [Google Scholar]
- 39.Hill VA, Wong E, Hart CJ. General practitioner referral guidelines for dermatology: do they improve the quality of referrals? Clin Exp Dermatol. 2000;25(5):371–376. doi: 10.1046/j.1365-2230.2000.00665.x. [DOI] [PubMed] [Google Scholar]
- 40.Matowe L, Ramsay CR, Grimshaw JM, et al. Effects of mailed dissemination of the Royal College of Radiologists’ guidelines on general practitioner referrals for radiography: a time series analysis. Clin Radiol. 2002;57(7):575–578. doi: 10.1053/crad.2001.0894. [DOI] [PubMed] [Google Scholar]
- 41.Melia J, Coulson P, Coleman D, Moss S. Urological referral of asymptomatic men in general practice in England. Br J Cancer. 2008;98(7):1176–1181. doi: 10.1038/sj.bjc.6604291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.West YR, Kendrick BJ, Williamson DM. Evaluation of the impact of orthopaedic guidelines on referrals from primary care to a specialist department. Qual Prim Care. 2007;15(1):27–31. [Google Scholar]
- 43.Banait G, Sibbald B, Thompson D, et al. Modifying dyspepsia management in primary care: a cluster randomised controlled trial of educational outreach compared with passive guideline dissemination. Br J Gen Pract. 2003;53(487):94–100. [PMC free article] [PubMed] [Google Scholar]
- 44.Eccles M, Steen N, Grimshaw J, et al. Effect of audit and feedback, and reminder messages on primary-care radiology referrals: a randomised trial. Lancet. 2001;357(9266):1406–1409. doi: 10.1016/S0140-6736(00)04564-5. [DOI] [PubMed] [Google Scholar]
- 45.Elwyn G, Owen D, Roberts L, et al. Influencing referral practice using feedback of adherence to NICE guidelines: a quality improvement report for dyspepsia. Qual Saf Health Care. 2007;16(1):67–70. doi: 10.1136/qshc.2006.019992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wright J, Harrison S, McGeorge M, et al. Improving the management and referral of patients with transient ischaemic attacks: a change strategy for a health community. Qual Saf Health Care. 2006;15(1):9–12. doi: 10.1136/qshc.2005.014704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Glaves J. The use of radiological guidelines to achieve a sustained reduction in the number of radiographic examinations of the cervical spine, lumbar spine and knees performed for GPs. Clin Radiol. 2005;60(8):914–920. doi: 10.1016/j.crad.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 48.Griffiths CE, Taylor H, Collins SI, et al. The impact of psoriasis guidelines on appropriateness of referral from primary to secondary care: a randomized controlled trial. Br J Dermatol. 2006;155(2):393–400. doi: 10.1111/j.1365-2133.2006.07354.x. [DOI] [PubMed] [Google Scholar]
- 49.Kerry S, Oakeshott P, Dundas D, Williams J. Influence of postal distribution of the Royal College of Radiologists’ guidelines, together with feedback on radiological referral rates, on X-ray referrals from general practice: a randomized controlled trial. Fam Pract. 2000;17(1):46–52. doi: 10.1093/fampra/17.1.46. [DOI] [PubMed] [Google Scholar]
- 50.Robling MR, Houston HL, Kinnersley P, et al. General practitioners’ use of magnetic resonance imaging: an open randomized trial comparing telephone and written requests and an open randomized controlled trial of different methods of local guideline dissemination. Clin Radiol. 2002;57(5):402–407. doi: 10.1053/crad.2001.0864. [DOI] [PubMed] [Google Scholar]
- 51.White T, Marriott S. Using evidence-based dissemination and implementation strategies to improve routine communication between general practitioners and community mental health teams. Psychiatr Bull. 2004;28:8–11. [Google Scholar]
- 52.Julian S, Naftalin NJ, Clark M, et al. An integrated care pathway for menorrhagia across the primary-secondary interface: patients’ experience, clinical outcomes, and service utilisation. Qual Saf Health Care. 2007;16(2):110–115. doi: 10.1136/qshc.2005.016782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Walkowski K, Peel C, Sandy L. Effect of academic detailing on primary care referral patterns to high performing cardiac specialists. J Gen Intern Med. 2007;22(1 Suppl):196–197. [Google Scholar]
- 54.Morrison J, Carroll L, Twaddle S, et al. Pragmatic randomised controlled trial to evaluate guidelines for the management of infertility across the primary care-secondary care interface. BMJ. 2001;322(7297):1282–1284. doi: 10.1136/bmj.322.7297.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wilson BJ, Torrance N, Mollison J, et al. Cluster randomized trial of a multifaceted primary care decision-support intervention for inherited breast cancer risk. Fam Pract. 2006;23(5):537–544. doi: 10.1093/fampra/cml026. [DOI] [PubMed] [Google Scholar]
- 56.Dey P, Simpson CW, Collins SI, et al. Implementation of RCGP guidelines for acute low back pain: a cluster randomised controlled trial. Br J Gen Pract. 2004;54(498):33–37. [PMC free article] [PubMed] [Google Scholar]
- 57.Engers AJ, Wensing M, van Tulder MW, et al. Implementation of the Dutch low back pain guideline for general practitioners: a cluster randomized controlled trial. Spine. 2005;30(6):559–600. doi: 10.1097/01.brs.0000155406.79479.3a. [DOI] [PubMed] [Google Scholar]
- 58.Jiwa M, Skinner P, Coker AO, et al. Implementing referral guidelines: lessons from a negative outcome cluster randomised factorial trial in general practice. BMC Fam Pract. 2006;7:65. doi: 10.1186/1471-2296-7-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Spatafora S, Canepa G, Migliari R, et al. Effects of a shared protocol between urologists and general practitioners on referral patterns and initial diagnostic management of men with lower urinary tract symptoms in Italy: the Prostate Destination study. BJU Int. 2005;95(4):563–570. doi: 10.1111/j.1464-410X.2005.05340.x. [DOI] [PubMed] [Google Scholar]
- 60.Bridgman S, Li X, Mackenzie G, Dawes P. Does the North Staffordshire slot system control demand of orthopaedic referrals from primary care? A population-based survey in general practice. Br J Gen Pract. 2005;55(518):704–709. [PMC free article] [PubMed] [Google Scholar]
- 61.Khan A, Smith DA, Whittaker J, et al. Abstract S26: effectiveness of direct GP referrals to hospital specialist respiratory teams in avoiding acute admissions. Thorax. 2008;63(Suppl 7):A12–A15. [Google Scholar]
- 62.Sved-Williams A, Poulton J. Primary care mental health consultation-liaison: a connecting system for private psychiatrists and general practitioners. Australas Psychiatry. 2010;18(2):125–129. doi: 10.3109/10398560903469783. [DOI] [PubMed] [Google Scholar]
- 63.Hemingway DM, Jameson J, Kelly MJ, Leicester Colorectal Specialist Interest Group Project Steering Committee Straight to test: introduction of a city-wide protocol driven investigation of suspected colorectal cancer. Colorectal Dis. 2006;8(4):289–295. doi: 10.1111/j.1463-1318.2005.00935.x. [DOI] [PubMed] [Google Scholar]
- 64.McNally OM, Wareham V, Flemming DJ, et al. The impact of the introduction of a fast track clinic on ovarian cancer referral patterns. Eur J Cancer Care (Engl) 2003;12(4):327–330. doi: 10.1046/j.1365-2354.2003.00419.x. [DOI] [PubMed] [Google Scholar]
- 65.Prades J, Espinàs JA, Font R, et al. Implementing a Cancer Fast-track Programme between primary and specialised care in Catalonia (Spain): a mixed methods study. Br J Cancer. 2011;105(6):753–759. doi: 10.1038/bjc.2011.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.DAMASK (Direct Access to Magnetic Resonance Imaging: Assessment for Suspect Knees) Trial Team. Cost-effectiveness of magnetic resonance imaging of the knee for patients presenting in primary care. Br J Gen Pract. 2008 doi: 10.3399/bjgp08X342660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shaw IS, Valori RM, Charlett A, McNulty CA. Limited impact on endoscopy demand from a primary care based ‘test and treat’ dyspepsia management strategy: the results of a randomised controlled trial. Br J Gen Pract. 2006;56(526):369–374. [PMC free article] [PubMed] [Google Scholar]
- 68.Simpson GC, Forbes K, Teasdale E, et al. Impact of GP direct-access computerised tomography for the investigation of chronic daily headache. Br J Gen Pract. 2010;60(581):897–901. doi: 10.3399/bjgp10X544069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thomas RE, Grimshaw JM, Mollison J, et al. Cluster randomized trial of a guideline-based open access urological investigation service. Fam Pract. 2003;20(6):646–654. doi: 10.1093/fampra/cmg605. [DOI] [PubMed] [Google Scholar]
- 70.Thomas R, Cook A, Main G, et al. Primary care access to computed tomography for chronic headache. Br J Gen Pract. 2010;60(575):426–430. doi: 10.3399/bjgp10X502146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wong BC, Chan CK, Wong KW, et al. Evaluation of a new referral system for the management of dyspepsia in Hong Kong: role of open-access upper endoscopy. J Gastroenterol Hepatol. 2000;15(11):1251–1256. [PubMed] [Google Scholar]
- 72.Dhillon V, Creiger J, Hannan J, et al. The effect of DXA scanning on clinical decision making by general practitioners: a randomized, prospective trial of direct access versus referral to a hospital consultant. Osteoporos Int. 2003;14(4):326–333. doi: 10.1007/s00198-002-1371-2. [DOI] [PubMed] [Google Scholar]
- 73.Eley KA, Fitzgerald JE. Quality improvement in action. Direct general practitioner referrals to audiology for the provision of hearing aids: a single centre review. Qual Prim Care. 2010;18(3):201–206. [PubMed] [Google Scholar]
- 74.Gough-Palmer AL, Burnett C, Gedroyc WM. Open access to MRI for general practitioners: 12 years’ experience at one institution — a retrospective analysis. Br J Radiol. 2009;82(980):687–690. doi: 10.1259/bjr/88267089. [DOI] [PubMed] [Google Scholar]
- 75.Leggett P, Gilliland AE, Cupples ME, et al. A randomized controlled trial using instant photography to diagnose and manage dermatology referrals. Fam Pract. 2004;21(1):54–56. doi: 10.1093/fampra/cmh112. [DOI] [PubMed] [Google Scholar]
- 76.Eminovic N, de Keizer NF, Wyatt JC, et al. Teledermatologic consultation and reduction in referrals to dermatologists: a cluster randomized controlled trial. Arch Dermatol. 2009;145(5):558–564. doi: 10.1001/archdermatol.2009.44. [DOI] [PubMed] [Google Scholar]
- 77.Whited JD, Hall RP, Foy ME, et al. Teledermatology’s impact on time to intervention among referrals to a dermatology consult service. Telemed J E Health. 2002;8(3):313–321. doi: 10.1089/15305620260353207. [DOI] [PubMed] [Google Scholar]
- 78.McKoy KC, DiGregorio S, Stira L. Asynchronous teledermatology in an urban primary care practice. Telemed J E Health. 2004;10(Suppl 2):S70–S80. [PubMed] [Google Scholar]
- 79.Knol A, van den Akker TW, Damstra RJ, de Haan J. Teledermatology reduces the number of patient referrals to a dermatologist. J Telemed Telecare. 2006;12(2):75–78. doi: 10.1258/135763306776084365. [DOI] [PubMed] [Google Scholar]
- 80.Hockey AD, Wootton R, Casey T. Trial of low-cost teledermatology in primary care. J Telemed Telecare. 2004;10(Suppl 1):44–47. doi: 10.1258/1357633042614221. [DOI] [PubMed] [Google Scholar]
- 81.Nielsen JD, Palshof T, Mainz J, et al. Randomised controlled trial of a shared care programme for newly referred cancer patients: bridging the gap between general practice and hospital. Qual Saf Health Care. 2003;12(4):263–272. doi: 10.1136/qhc.12.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Harrington JT, Dopf CA, Chalgren CS. Implementing guidelines for interdisciplinary care of low back pain: a critical role for pre-appointment management of specialty referrals. Jt Comm J Qual Improv. 2001;27(12):651–663. doi: 10.1016/s1070-3241(01)27055-2. [DOI] [PubMed] [Google Scholar]
- 83.Wallace P, Barber J, Clayton W, et al. Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations. Health Technol Assess. 2004;8(50):1–106. doi: 10.3310/hta8500. [DOI] [PubMed] [Google Scholar]
- 84.Jaatinen PT, Aarnio P, Remes J, et al. Teleconsultation as a replacement for referral to an outpatient clinic. J Telemed Telecare. 2002;8(2):102–106. doi: 10.1258/1357633021937550. [DOI] [PubMed] [Google Scholar]
- 85.Tadros A, Murdoch R, Stevenson JH. Digital image referral for suspected skin malignancy: a pilot study of 300 patients. J Plast Reconstr Aesthet Surg. 2009;62(8):1048–1053. doi: 10.1016/j.bjps.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 86.Nicholson C, Jackson CL, Wright B, et al. Online referral and OPD booking from the GP desktop. Aust Health Rev. 2006;30(3):397–404. doi: 10.1071/ah060397. [DOI] [PubMed] [Google Scholar]
- 87.Kim Y, Chen AH, Keith E, et al. Not perfect, but better: primary care providers’ experiences with electronic referrals in a safety net health system. J Gen Intern Med. 2009;24(5):614–619. doi: 10.1007/s11606-009-0955-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dennison J, Eisen S, Towers M, Ingham Clark C. An effective electronic surgical referral system. Ann R Coll Surg Engl. 2006;88(6):554–556. doi: 10.1308/003588406X130642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chen AH, Kushel MB, Grumbach K, Yee HF., Jr A safety-net system gains efficiencies through ‘eReferrals’ to specialists. Health Aff. 2010;29(5):969–971. doi: 10.1377/hlthaff.2010.0027. [DOI] [PubMed] [Google Scholar]
- 90.Gandhi TK, Sittig DF, Franklin M, et al. Communication breakdown in the outpatient referral process. J Gen Intern Med. 2000;15(9):626–631. doi: 10.1046/j.1525-1497.2000.91119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kim-Hwang JE, Chen AH, Bell DS, et al. Evaluating electronic referrals for specialty care at a public hospital. J Gen Intern Med. 2010;25(10):1123–1128. doi: 10.1007/s11606-010-1402-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Stoves J, Connolly J, Cheung CK, et al. Electronic consultation as an alternative to hospital referral for patients with chronic kidney disease: a novel application for networked electronic health records to improve the accessibility and efficiency of healthcare. Qual Saf Health Care. 2010 doi: 10.1136/qshc.2009.038984. [DOI] [PubMed] [Google Scholar]
- 93.Patterson V, Humphreys J, Chua R. Email triage of new neurological outpatient referrals from general practice. J Neurol Neurosurg Psychiatry. 2004;75(4):617–620. doi: 10.1136/jnnp.2003.024489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Jiwa M, Dhaliwal S. Referral Writer: preliminary evidence for the value of comprehensive referral letters. Qual Prim Care. 2012;20(1):39–45. [PubMed] [Google Scholar]
- 95.Kennedy AM, Aziz A, Khalid S, Hurman D. Do GP referral guidelines really work? Audit of an electronic urgent referral system for suspected head and neck cancer. Eur Arch Otorhinolaryngol. 2012;269(5):1509–1512. doi: 10.1007/s00405-011-1788-3. [DOI] [PubMed] [Google Scholar]
- 96.McGowan J, Hogg W, Campbell C, Rowan M. Just-in-time information improved decision-making in primary care: a randomized controlled trial. PloS ONE. 2008;3(11):e3785. doi: 10.1371/journal.pone.0003785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Junghans C, Feder G, Timmis AD, et al. Effect of patient-specific ratings vs conventional guidelines on investigation decisions in angina: Appropriateness of Referral and Investigation in Angina (ARIA) Trial. Arch Intern Med. 2007;167(2):195–202. doi: 10.1001/archinte.167.2.195. [DOI] [PubMed] [Google Scholar]
- 98.Akbari A, Grimshaw J, Stacey D, et al. Change in appropriate referrals to nephrologists after the introduction of automatic reporting of the estimated glomerular filtration rate. CMAJ. 2012;184(5):E269–E276. doi: 10.1503/cmaj.110678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Emery J, Morris H, Goodchild R, et al. The GRAIDS Trial: a cluster randomised controlled trial of computer decision support for the management of familial cancer risk in primary care. Br J Cancer. 2007;97(4):486–493. doi: 10.1038/sj.bjc.6603897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Knab JH, Wallace MS, Wagner RL, et al. The use of a computer-based decision support system facilitates primary care physicians’ management of chronic pain. Anesth Analg. 2001;93(3):712–720. doi: 10.1097/00000539-200109000-00035. [DOI] [PubMed] [Google Scholar]
- 101.Mariotti G, Meggio A, de Pretis G, Gentilini M. Improving the appropriateness of referrals and waiting times for endoscopic procedures. J Health Serv Res Policy. 2008;13(3):146–151. doi: 10.1258/jhsrp.2008.007170. [DOI] [PubMed] [Google Scholar]
- 102.Greiver M, Drummond N, White D, et al. Angina on the Palm: randomized controlled pilot trial of Palm PDA software for referrals for cardiac testing. Can Fam Physician. 2005;51:382–383. [PMC free article] [PubMed] [Google Scholar]
- 103.Magill MK, Day J, Mervis A, et al. Improving colonoscopy referral rates through computer-supported, primary care practice redesign. J Healthc Qual. 2009;31(4):43–52. doi: 10.1111/j.1945-1474.2009.00037.x. [DOI] [PubMed] [Google Scholar]
- 104.Tierney WM, Overhage JM, Murray MD, et al. Effects of computerized guidelines for managing heart disease in primary care. J Gen Intern Med. 2003;18(12):967–976. doi: 10.1111/j.1525-1497.2003.30635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Slade M, Gask L, Leese M, et al. Failure to improve appropriateness of referrals to adult community mental health services: lessons from a multi-site cluster randomized controlled trial. Fam Pract. 2008;25(3):181–190. doi: 10.1093/fampra/cmn025. [DOI] [PubMed] [Google Scholar]
- 106.Stainkey LA, Seidl IA, Johnson AJ, et al. The challenge of long waiting lists: how we implemented a GP referral system for non-urgent specialist appointments at an Australian public hospital. BMC Health Serv Res. 2010;10:303. doi: 10.1186/1472-6963-10-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.King RHB, Bateman H. Piloting an approach to the identification of avoidable referrals in a general practice with a high referral rate. Journal of Clinical Excellence. 2001;2(4):209–213. [Google Scholar]
- 108.van Bokhoven MA, Koch H, van der Weijden T, et al. The effect of watchful waiting compared to immediate test ordering instructions on general practitioners’ blood test ordering behaviour for patients with unexplained complaints; a randomized clinical trial (ISRCTN55755886) Implement Sci. 2012;7:29. doi: 10.1186/1748-5908-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Callaway P, Frisch L. Does a family physician who offers colposcopy and LEEP need to refer patients to a gynecologist? J Fam Pract. 2000;49(6):534–536. [PubMed] [Google Scholar]
- 110.Standing P, Dent M, Craig A, Glenville B. Changes in referral patterns to cardiac outpatient clinics with ambulatory ECG monitoring in general practice. Br J Cardiol. 2001;8(6):394–398. [Google Scholar]
- 111.van Dijk CE, Verheij RA, Spreeuwenberg P, et al. Minor surgery in general practice and effects on referrals to hospital care: observational study. BMC Health Serv Res. 2011;11:2. doi: 10.1186/1472-6963-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ridsdale L, Doherty J, McCrone P, et al. A new GP with special interest headache service: observational study. Br J Gen Pract. 2008;58(552):478–483. doi: 10.3399/bjgp08X319440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Salisbury C, Noble A, Horrocks S, et al. Evaluation of a general practitioner with special interest service for dermatology: randomised controlled trial. BMJ. 2005;331(7530):1441–1446. doi: 10.1136/bmj.38670.494734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sanderson D. Evaluation of the GPs with special interests (GPwSIs) pilot projects within the Action On ENT Programme: final report. York: Department of Health Modernisation Agency York Health Economics Consortium; 2002. [Google Scholar]
- 115.Sauro A, Scalzitti F, Buono N, et al. Spirometry is really useful and feasible in the GP’s daily practice but guidelines alone are not. Eur J Gen Pract. 2005;11(1):29–31. doi: 10.3109/13814780509178015. [DOI] [PubMed] [Google Scholar]
- 116.Rosen R, Jones R, Tomlin Z, Cavanagh MR. Evaluation of general practitioners with special interests: access, cost evaluation and satisfaction with services. National Institute for Health Research; 2006. http://www.nets.nihr.ac.uk/__data/assets/pdf_file/0005/64445/FR-08-1210-035.pdf (accessed 15 Oct 2014) [DOI] [PubMed] [Google Scholar]
- 117.Levell NJ, Penart-Lanau AM, Garioch JJ. Introduction of intermediate care dermatology services in Norfolk, England was followed by a 67% increase in referrals to the local secondary care dermatology department. Br J Dermatol. 2012;167(2):443–445. doi: 10.1111/j.1365-2133.2012.10850.x. [DOI] [PubMed] [Google Scholar]
- 118.Leiba AM, Martonovits G, Magnezi R, et al. Evaluation of a specialist outreach clinic in a primary healthcare setting: the effect of easy access to specialists. Clinician in Management. 2002;11(3):131–136. [Google Scholar]
- 119.Campbell H, Holloway S, Cetnarskyj R, et al. Referrals of women with a family history of breast cancer from primary care to cancer genetics services in South East Scotland. Br J Cancer. 2003;89(9):1650–1656. doi: 10.1038/sj.bjc.6601348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Felker BL, Barnes RF, Greenberg DM, et al. Preliminary outcomes from an integrated mental health primary care team. Psychiatr Serv. 2004;55(4):442–444. doi: 10.1176/appi.ps.55.4.442. [DOI] [PubMed] [Google Scholar]
- 121.Gurden M, Morelli M, Sharp G, et al. Evaluation of a general practitioner referral service for manual treatment of back and neck pain. Prim Health Care Res Dev. 2012;13(3):204–210. doi: 10.1017/S1463423611000648. [DOI] [PubMed] [Google Scholar]
- 122.Schulpen GJ, Vierhout WP, van der Heijde DM, et al. Joint consultation of general practitioner and rheumatologist: does it matter? Ann Rheum Dis. 2003;62(2):159–161. doi: 10.1136/ard.62.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Vlek JF, Vierhout WP, Knottnerus JA, et al. A randomised controlled trial of joint consultations with general practitioners and cardiologists in primary care. Br J Gen Pract. 2003;53(487):108–112. [PMC free article] [PubMed] [Google Scholar]
- 124.Hughes-Anderson W, Rankin SL, House J, et al. Open access endoscopy in rural and remote Western Australia: does it work? ANZ J Surg. 2002;72(10):699–703. doi: 10.1046/j.1445-2197.2002.02535.x. [DOI] [PubMed] [Google Scholar]
- 125.Hermush V, Daliot D, Weiss A, et al. The impact of geriatric consultation on the care of the elders in community clinics. Arch Gerontol Geriatr. 2009;49(2):260–262. doi: 10.1016/j.archger.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 126.Pfeiffer PN, Szymanski BR, Zivin K, et al. Are primary care mental health services associated with differences in specialty mental health clinic use? Psychiatr Serv. 2011;62(4):422–425. doi: 10.1176/ps.62.4.pss6204_0422. [DOI] [PubMed] [Google Scholar]
- 127.Johnson G, White A, Livingstone R. Do general practices which provide an acupuncture service have low referral rates and prescription costs? A pilot survey. Acupunct Med. 2008;26(4):205–213. doi: 10.1136/aim.26.4.205. [DOI] [PubMed] [Google Scholar]
- 128.Wylie KR, Davies-South D. Returning a referral for erectile dysfunction to the referrer by two different routes. BJU Int. 2001;87(9):846–848. doi: 10.1046/j.1464-410x.2001.02188.x. [DOI] [PubMed] [Google Scholar]
- 129.Tan E, Levell NJ, Garioch JJ. The effect of a dermatology restricted-referral list upon the volume of referrals. Clin Exp Dermatol. 2007;32(1):114–115. doi: 10.1111/j.1365-2230.2006.02273.x. [DOI] [PubMed] [Google Scholar]
- 130.van Dijk CE, Verheij RA, Hansen J, et al. Primary care nurses: effects on secondary care referrals for diabetes. BMC Health Serv Res. 2010;10:230. doi: 10.1186/1472-6963-10-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.White M, Bijlani N, Bale R, Burns T. Impact of counsellors in primary care on referrals to secondary mental health services. Psychiatr Bull. 2000;24(11):418–420. [Google Scholar]
- 132.Simpson S, Corney R, Fitzgerald P. Counselling provision, prescribing and referral rates in a general practice setting. Primary Care Psychiatry. 2003;8(4):115–119. [Google Scholar]
- 133.Schillinger D, Bibbins-Domingo K, Vranizan K, et al. Effects of primary care coordination on public hospital patients. J Gen Intern Med. 2000;15(5):329–336. doi: 10.1046/j.1525-1497.2000.07010.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ferris TG, Chang Y, Blumenthal D, Pearson SD. Leaving gatekeeping behind: effects of opening access to specialists for adults in a health maintenance organization. N Engl J Med. 2001;345(18):1312–1317. doi: 10.1056/NEJMsa010097. [DOI] [PubMed] [Google Scholar]
- 135.Ferris TG, Chang Y, Perrin JM, et al. Effects of removing gatekeeping on specialist utilization by children in a health maintenance organization. Arch Pediatr Adolesc Med. 2002;156(6):574–579. doi: 10.1001/archpedi.156.6.574. [DOI] [PubMed] [Google Scholar]
- 136.Joyce GF, Kapur K, Van Vorst KA, Escarce JJ. Visits to primary care physicians and to specialists under gatekeeper and point-of-service arrangements. Am J Manag Care. 2000;6(11):1189–1196. [PubMed] [Google Scholar]
- 137.McGarry H, Hegarty K, Johnson C, et al. Managing depression in a changing primary mental healthcare system: comparison of two snapshots of Australian GPs’ treatment and referral patterns. Ment Health Fam Med. 2009;6(2):75–83. [PMC free article] [PubMed] [Google Scholar]
- 138.van Dijk CE, Verheij RA, Spreeuwenberg P, et al. Impact of remuneration on guideline adherence: empirical evidence in general practice. Scand J Prim Health Care. 2013;31(1):56–63. doi: 10.3109/02813432.2012.757078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Vardy DA, Freud T, Sherf M, et al. A co-payment for consultant services: primary care physicians’ referral actualization. J Med Syst. 2008;32(1):37–41. doi: 10.1007/s10916-007-9105-9. [DOI] [PubMed] [Google Scholar]
- 140.Iversen T, Lurås H. The effect of capitation on GPs’ referral decisions. Health Econ. 2000;9(3):199–210. doi: 10.1002/(sici)1099-1050(200004)9:3<199::aid-hec514>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 141.Watson E, Clements A, Lucassen A, et al. Education improves general practitioner (GP) management of familial breast/ovarian cancer: findings from a cluster randomised controlled trial. J Med Genet. 2002;39(10):779–781. doi: 10.1136/jmg.39.10.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Whiting M. Introducing a GP-led referral gateway. Pulse. 2011;71(18):29–30. [Google Scholar]
- 143.Maddison P, Jones J, Breslin A, et al. Improved access and targeting of musculoskeletal services in northwest Wales: targeted early access to musculoskeletal services (TEAMS) programme. BMJ. 2004;329(7478):1325–1327. doi: 10.1136/bmj.329.7478.1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kim C, Williamson DF, Herman WH, et al. Referral management and the care of patients with diabetes: the Translating Research Into Action for Diabetes (TRIAD) study. Am J Manag Care. 2004;10(2):137–143. [PubMed] [Google Scholar]
- 145.Cox JM, Steel N, Clark AB, et al. Do referral-management schemes reduce hospital outpatient attendances? Time-series evaluation of primary care referral management. Br J Gen Pract. 2013 doi: 10.3399/bjgp13X668177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ferriter K, Gangopadhyay P, Nilforooshan R, et al. Quality of referrals to old age psychiatry following introduction of the single assessment process. Psychiatr Bull. 2006;30(12):452–453. [Google Scholar]
- 147.Albertson G, Lin CT, Schilling L, et al. Impact of a simple intervention to increase primary care provider recognition of patient referral concerns. Am J Manag Care. 2002;8(4):375–381. [PubMed] [Google Scholar]
- 148.Heaney D, Wyke S, Wilson P, et al. Assessment of impact of information booklets on use of healthcare services: randomised controlled trial. BMJ. 2001;322(7296):1218–1221. doi: 10.1136/bmj.322.7296.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lyon D, Knowles J, Slater B, Kennedy R. Improving the early presentation of cancer symptoms in disadvantaged communities: putting local people in control. Br J Cancer. 2009;101(Suppl 2):S49–S54. doi: 10.1038/sj.bjc.6605390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Patton MQ. Qualitative research and evaluation methods. 3rd edn. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 151.Baxter SK, Blank L, Woods HB, et al. Using logic model methods in systematic review synthesis: describing complex pathways in referral management interventions. BMC Med Res Methodol. 2014;14:62. doi: 10.1186/1471-2288-14-62. [DOI] [PMC free article] [PubMed] [Google Scholar]