Abstract
Patient: Female, 56
Final Diagnosis: Broncho-pleural fistula • empyema • supra-vena cava syndrome
Symptoms: Dyspnea • fever • facial edema
Medication: —
Clinical Procedure: —
Specialty: Oncology and Pulmonology
Objective:
Unusual clinical course
Background:
It is extremely rare for pulmonary hilar lymph node metastasis (PHLNM) of a cancer to be independently lethal. Here, we report an exceedingly rare case of cavitation in PHLNM from breast cancer triggering bronchopleural fistula and empyema (BPFE), complicated with superior vena cava syndrome (SVCS).
Case Report:
A 56-year-old woman who had undergone left segmental mastectomy and axillary lymph node dissection due to left breast cancer was then treated for 1 year with postoperative adjuvant chemotherapy. Recurrence of right PHLNM was observed 2 years after the operation, for which 3 courses of bevacizumab (BEV) and paclitaxel combination chemotherapy were administered. The woman had dyspnea and fever during the washout period, and CT examination revealed fistula formation between the right PHLNM cavitation and right main bronchus, so she was admitted for further treatment. This fistula rapidly progressed to BPFE, and contralateral aspiration was observed to cause pneumonia of the left lung. In addition, edema of both upper limbs and head and neck were observed, and CT examination revealed SVCS caused by re-enlargement of PHLNM. Active treatment was performed, but the recommencement of chemotherapy was not possible, and she died on Day 150 of admission.
Conclusions:
We think that PHLNM deteriorated to central necrosis due to chemotherapy with BEV taking effect, leading to formation of BPFE. The case was also made more difficult due to the complication of SVCS caused by the re-enlarged PHLNM.
MeSH Keywords: Angiogenesis Inhibitors, Breast Neoplasms, Bronchial Fistula, Superior Vena Cava Syndrome
Background
Although pulmonary hilar lymph node metastasis (PHLNM) is frequently observed in breast cancer [1], it is extremely rare for the condition to independently constitute a serious risk for cancer death. Bronchial fistula and superior vena cava syndrome (SVCS) caused by metastasizing or disseminated lesions in the thoracic cavity are serious paraneoplastic syndrome (PNS), the treatment for which often causes much suffering [2]. This report describes an exceedingly rare case of cavitation in PHLNM from breast cancer triggering broncho-pleural fistula and empyema (BPFE) complicated by SVCS.
Case Report
A 56-year-old woman had undergone segmental mastectomy and axillary lymph node dissection in November 2009, with a final diagnosis of T2N0M0 that was estrogen receptor-negative, progesterone receptor-negative, and strongly HER2-positive. She received 6 courses of docetaxel and 12 courses of trastuzumab as postoperative adjuvant chemotherapy. CT examination revealed right PHLNM 2 years after the operation (Figure 1), so chemotherapy was recommenced. The appearance of new lesions had not been observed one year following recommencement of treatment, but the right PHLNM indicated a trend toward enlargement, and bevacizumab (BEV) and paclitaxel combination chemotherapy was commenced. Upon completion of 3 courses of chemotherapy with the same regimen, CT examination revealed PHLNM cavitation. Because she complained of dyspnea and fever during the washout period, she was admitted for further medical treatments.
Figure 1.
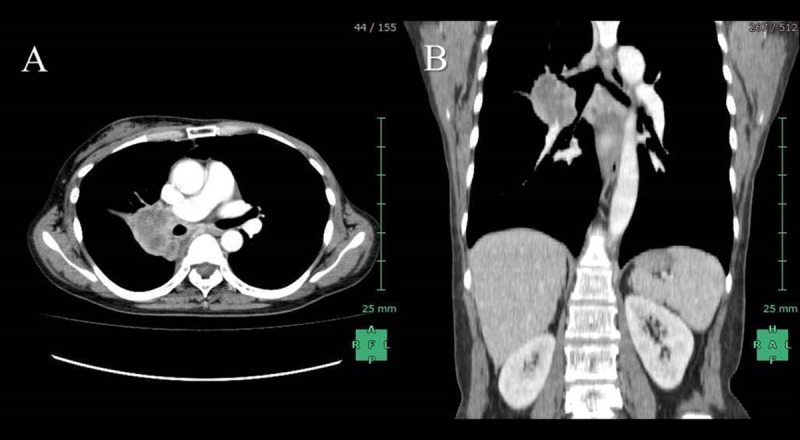
(A) CT examination revealed a 4.5-cm right PHLNM. (B) CT examination in coronal section also revealed the exclusion of lobar bronchi by PHLNM.
Routine blood examination showed a high degree of inflammation, with a leukocyte count of 25 900/μL, CRP of 33.32 mg/dl, and procalcitonin of 14.21 ng/ml. A sputum culture test also detected Staphylococcus aureus. In addition, a CT examination on admission revealed fistula formation between the right PHLNM cavitation and the right main bronchus and its peripheral obstructive pneumonia (Figure 2). Conservative treatment was immediately commenced for the obstructive pneumonia, but a CT examination on Day 7 of admission revealed BPFE accompanying the formation of a fluid collection in the right thoracic cavity. On Day 10 of admission, her condition became worse, complicated by pneumonia of the left lung due to the contralateral aspiration caused by BPFE; therefore, selected intubation using bronchoscopy into the left main bronchus was performed. Tracheotomy was subsequently performed and a double-lumen tracheostomy tube (Tracheopart, Toray Medical Co. Ltd, Tokyo, Japan) was inserted into the left main bronchus via tracheostomy (Figure 3).
Figure 2.

(A) CT examination on admission revealed fistula formation between the right PHLNM cavitation and the right main bronchus. (B) CT examination in coronal section also revealed its peripheral obstructive pneumonia.
Figure 3.
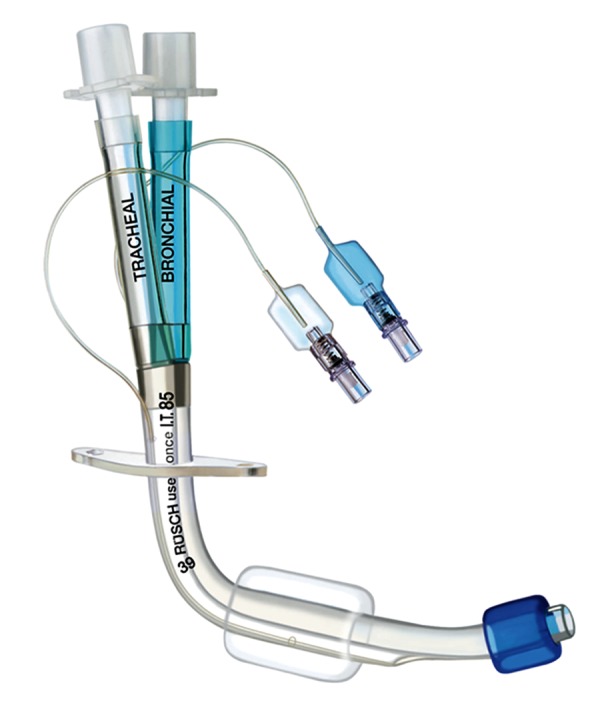
A double-lumen tracheostomy tube for left bronchus. (Tracheopart, Toray Medical Co. Ltd, Tokyo, Japan).
Because the patient had cancer without any distant metastasis or recurrent lesions except for the right PHLNM, and because lethal organ dysfunction brought on by PHLNM is very rare, active treatment was continued. However, on Day 51 of admission, edema of both upper limbs, head, and neck were observed. Contrast CT examination revealed severe narrowing of the superior vena cava due to exclusion and direct invasion by the right PHLNM (Figure 4), and the patient was diagnosed as SVCS. The use of interventional radiology (IVR) for SVCS was considered at this time, but because resolving the SVCS would not improve quality of life (QOL), and compliance with chemotherapy would not be possible, the proposal was abandoned. Ultimately, the patient had no dramatic improvement in symptoms, and died on Day 150 of admission.
Figure 4.
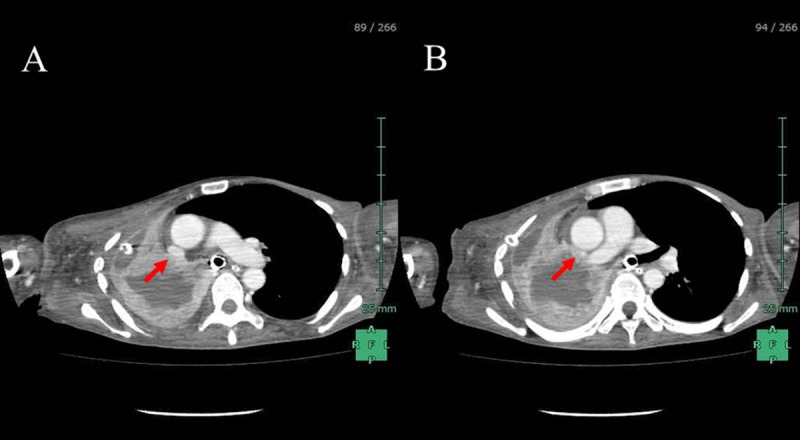
(A, B) Contrast CT examination revealed severe narrowing of the superior vena cava due to exclusion and direct invasion by the right PHLNM (arrow).
Discussion
While pulmonary hilar lymph node metastasis (PHLNM) is frequently observed in breast cancer [1], it is rare for it to be lethal. We treated an extremely rare case in which PHLNM as the first recurring lesion after surgery and adjuvant chemotherapy caused BPFE and SVCS.
Treatment methods for BPFE include surgical methods such as lung decortication, thoracoplasty, pneumonectomy, and plombage [3], and non-surgical treatment methods such as endoscopic cauterization, silver nitrate application, injection of OK-432 into the thoracic cavity, and bronchoscopic plombage with fibrin glue [4]. Because BPFE is refractory and is observed in critically ill patients, treatment for BPFE is sometimes very difficult. If appropriate treatments are not administered during the early stages of BPFE onset, sepsis and acute respiratory failure caused by contralateral aspiration are very likely to occur.
In this case, poor general physical condition (ECOG performance status was 3) made selection of a surgical treatment more difficult. Basic conservative treatment involves drainage of the infected thoracic cavity and proper discharge of bronchial secretions, along with administration of an adequate dose of antibiotics [4]. Here, however, although these conservative treatments for BPFE were appropriately administered, dramatic improvement in the extent of organization of the infectious site was not achieved.
SVCS is a typical PNS of thoracic malignancies [2,5]. Wierecky et al. reported that it occurs in most cases as a result of either superior vena cava invasion by primary malignant tumors (60–90%) or malignant lymphoma (6–25%), with onset due to metastasizing lesions in the thoracic cavity, which is relatively rare [6]. In addition, the 1-year survival rate after onset of SVCS is only around 20–25% [7,8], and patients with SVCS complicated by a malignant tumor generally have a poor prognosis regardless of whether the tumor is a primary or metastasizing lesion. Chemotherapy and radiation therapy are conventionally selected for treatment of SVCS [7], but these methods had no immediate effect, and treatment itself was impossible given that the overall physical condition of the patient was poor.
Since confirmation of the utility of intravascular stent placement with IVR [2,9], it has become the treatment of choice for SVCS [2,9]. In our case, however, the onset of BPFE made cessation of chemotherapy unavoidable, and re-enlargement of the PHLNM during that period might have caused SVCS. Although the indication of IVR for SVCS was discussed, the proposal was abandoned due to poor prospects for improvement in QOL or sequential recommencement of chemotherapy, before even considering stent patency or the rate of complications. Furthermore, although the utility of prophylactic IVR for predicted future SVCS onset due to thoracic or mediastinal tumors has not yet been demonstrated, only IVR could prevent the onset of SVCS.
This case presented several severe paraneoplastic complications triggered by the PHLNM cavitation due to BEV and paclitaxel combination chemotherapy. BEV is a recombinant humanized monoclonal antibody against vascular endothelial growth factor, and it exerts an anti-tumor effect by inhibiting angiogenesis in malignant tumors. The utility of BEV against recurrent breast cancer is well-established by randomized control studies [10], and combination chemotherapy with paclitaxel was selected for this case. Nishino et al. reported tumor cavitation in 14 of 72 cases (19%) of non-small-cell lung cancer treated with BEV combination chemotherapy, in most cases carried out with paclitaxel or carboplatin [11]. Tumor cavitation is thought to occur due to central necrosis caused by the angiogenesis-inhibiting effects of BEV, and this change commonly suggests that the treatment has taken effect [11]. In addition to tumor cavitation as a result of chemotherapy in this case, fistula formation between the PHLNM cavitation and the right bronchus due to an increase of airway and intracavernous pressure was thought to constitute the pathogenesis [12].
Conclusions
This was an extremely rare case in which BPFE and SVCS arose as complications triggered by the PHLNM from breast cancer. It is thought that PHLNM lapsed into central necrosis and cavitation as a result of chemotherapy with BEV taking effect, and ruptured due to additional bronchial fistula formation and excessive intracavernous pressure, forming BPFE. In addition, complications with SVCS arose due to re-enlargement of PHLNM during the period for which a continuation of chemotherapy was impossible, resulting in a series of extremely rare pathological states. There is currently no clear evidence for prophylactic IVR prior to onset of SVCS, but if implemented on the basis of informed consent, it may have been effective in this case.
Acknowledgments
The authors would like to thank Dr. Kazushige Ishida and Dr. Seika Nakamura for helpful discussions.
References:
- 1.Cummings MC, Simpson PT, Reid LE, et al. Metastatic progression of breast cancer: insights from 50 years of autopsies. J Pathol. 2014;232:23–31. doi: 10.1002/path.4288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gwon DI, Ko GY, Kim JH, et al. Malignant superior vena cava syndrome: a comparative cohort study of treatment with covered stents versus uncovered stents. Radiology. 2013;266:979–87. doi: 10.1148/radiol.12120517. [DOI] [PubMed] [Google Scholar]
- 3.Tsai YM, Chen SL, Hsieh CM, et al. Treatment of empyema and bronchopleural fistula by bovine pericardium and latissimus flap. Ann Thorac Surg. 2013;95:e39–40. doi: 10.1016/j.athoracsur.2012.07.071. [DOI] [PubMed] [Google Scholar]
- 4.Boudaya MS, Smadhi H, Zribi H, et al. Conservative management of postoperative bronchopleural fistulas. J Thorac Cardiovasc Surg. 2013;146:575–79. doi: 10.1016/j.jtcvs.2013.04.023. [DOI] [PubMed] [Google Scholar]
- 5.Lepper PM, Ott SR, Hoppe H, et al. Superior vena cava syndrome in thoracic malignancies. Respir Care. 2011;56:653–66. doi: 10.4187/respcare.00947. [DOI] [PubMed] [Google Scholar]
- 6.Wierecky J, Bokemeyer C. Compression syndromes. Internist (Berl) 2005;46:9–18. doi: 10.1007/s00108-004-1318-0. [DOI] [PubMed] [Google Scholar]
- 7.Armstrong BA, Perez CA, Simpson JR, Hederman MA. Role of irradiation in the management of superior vena cava syndrome. Int J Radiat Oncol Biol Phys. 1987;13:531–39. doi: 10.1016/0360-3016(87)90068-x. [DOI] [PubMed] [Google Scholar]
- 8.Mose S, Stabik C, Eberlein K, et al. Retrospective analysis of the superior vena cava syndrome in irradiated cancer patients. Anticancer Res. 2006;26:4933–36. [PubMed] [Google Scholar]
- 9.Fagedet D, Thony F, Timsit JF, et al. Endovascular treatment of malignant superior vena cava syndrome: results and predictive factors of clinical efficacy. Cardiovasc Intervent Radiol. 2013;36:140–49. doi: 10.1007/s00270-011-0310-z. [DOI] [PubMed] [Google Scholar]
- 10.Miller K, Wang M, Gralow J, et al. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N Engl J Med. 2007;357:2666–76. doi: 10.1056/NEJMoa072113. [DOI] [PubMed] [Google Scholar]
- 11.Nishino M, Cryer SK, Okajima Y, et al. Tumoral cavitation in patients with non-small-cell lung cancer treated with antiangiogenic therapy using bevacizumab. Cancer Imaging. 2012;29:225–35. doi: 10.1102/1470-7330.2012.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaudhuri MR. Primary pulmonary cavitating carcinomas. Thorax. 1973;28:354–66. doi: 10.1136/thx.28.3.354. [DOI] [PMC free article] [PubMed] [Google Scholar]


