Abstract
Introduction:
Knee flexion is one of the main problems of the lower extremities in cerebral palsy patients. Many operative procedures are recommended for contractures of the knee in cerebral palsy patients. We performed simple operation and analyzed the results after operative treatment with nine years follow up.
Method:
85 patients with spastic cerebral palsy were treated in period 2001 – 2010. 40 were ambulatory and 45 non ambulatory with ability to stand with support. All of them underwent same surgical procedure with distal hamstrings lengthening. Tenotomies were performed on m. semitendinosus, m. semimembranosus, m. gracillis and biceps femoris. Only m. semitendinosus was tenotomized completely, other muscles were tenotomized only on tendinous part. The patients had a plaster immobilization for five days after the surgery with the knee extended.
Results:
All 85 patients had improvement of the popliteal angle pre and post operative respectively. Improvement in the crouch gait was noticed in the period of rehabilitation. We had no complication with the wound. Three of the patients had overcorrection and achieved recurvatum of the knees.
Conclusion:
We consider this procedure very simple with satisfying improvement of standing, walking and sitting abilities in children with spastic cerebral palsy.
Keywords: Cerebral palsy, knee flexion contracture, distal hamstrings lengthening
1. INTRODUCTION
Knee flexion contracture is one of the main problems of the lower extremities in cerebral palsy patients. The prerequisites for normal gait are: stability in the stance phase of gait, clearance of the foot in the swing phase, proper foot preposition in swing, and an adequate step length. In the stance phase, the knee provides shock absorption and energy conservation; in the swing phase, it allows foot clearance. To accomplish these functions, the knee must extend fully in stance and flex approximately 60 degrees in swing. Consequently, balanced muscle action at the hip, knee, and ankle joints, combined with adequate acceleration from the hip flexor and triceps sure muscles, is essential (1). These prerequisites are not met in patients with spastic cerebral palsy due to the primary neurological condition and therefore are considered as primary reasons for the most common sagittal contractures and deformities in these patients. These conditions in most cases lead even the collaborative patients to relinquish their efforts for walking.
There are many surgical options for treating the flexion contracture of the knee in spastic cerebral palsy patients, some are soft tissue only like distal hamstring lengthening (2, 3), distal hamstring lengthening combined with posterior knee capsulotomy or knee extensor mechanism shortening (4), medial or combined medial and lateral hamstring lengthening procedures (5).
Our approach to this problem is treating these patients with distal hamstrings, medial and lateral, lengthening.
2. PATIENTS AND METHODS
In the period 2001 – 2010, 85 patients with spastic cerebral palsy were treated. 40 were ambulatory and 45 non ambulatory with ability to stand with support. All of them underwent same surgical procedure with distal hamstrings lengthening. Tenotomies were performed on m. semitendinosus, m. semimembranosus, m. gracillis and biceps femoris. Only m. semitendinosus was tenotomized completely, other muscles were tenotomized only on tendinous part. The patients had a plaster immobilization for five days after the surgery with the knee extended. We divided the patients in two groups- ambulatory and non-ambulatory patients. We divided the patients further in four age groups (5-7y, 8-10y, 11-13y and 14-16y) and analyzed the values of the popliteal angle pre-operative and at nine years of follow-up postoperative with chi-square and t-test.
3. RESULTS
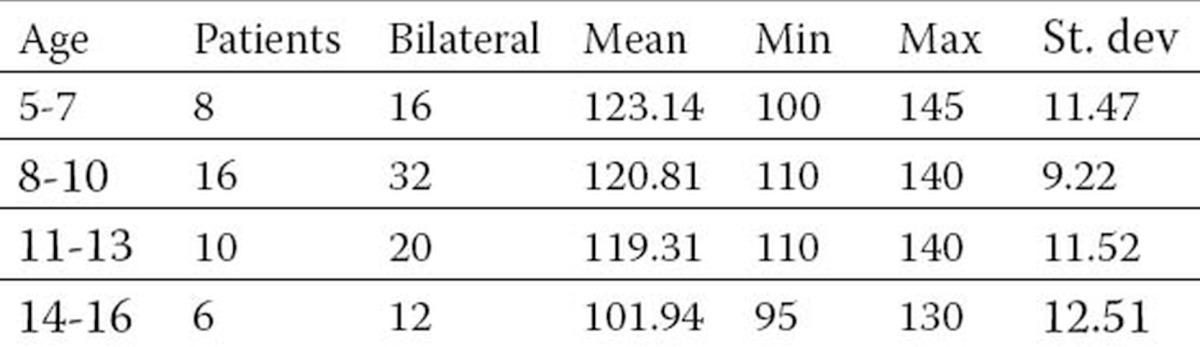
The group of ambulatory patients had total of 40 patients. The average values of the popliteal angle was 76,82 degrees in the group of 5-7y, 70,46 degrees in 8-10y group, 68,13 degrees in 11-13y and 61,35 in 14-16y group (Table 1). At the follow up we found improvement of the values of the popliteal angle in all of the age groups ranging from 123,14 degrees in 5-7y group to 101,94 in 14-16y group (Table 2). We analyzed the data using the chi-square and t-test. These tests confirmed high statistical significance of the postoperative results (p<0,0001) (preoperative values of the popliteal angle compared with postoperative values and also high statistical significance of the results comparing the separate age groups).
Table 1.
Ambulatory patients preoperative popliteal angle
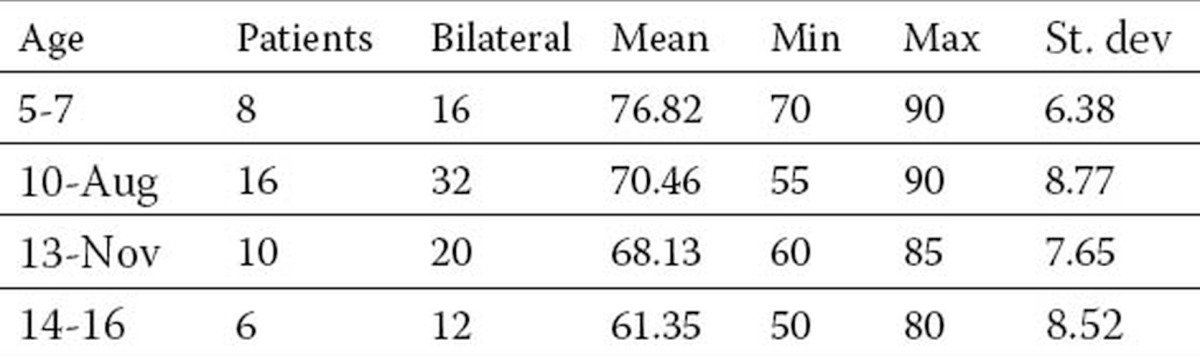
Table 2.
Ambulatory patients postoperative popliteal angle
The group of non-ambulatory patients comprised total of 45 patients with ability to stand with support. The average values of the popliteal angle preoperative was 68,60 degrees in the group of 5-7y, 74,85 degrees in 8-10y group, 64,75 degrees in 11-13y and 58,56 in 14-16y group (Table 3). At the follow up we found improvement of the values of the popliteal angle in all of the age groups ranging from 130,50 degrees in 5-7y group to 107,77 in 14-16y group (Table 4). Using the same statistical test as in the ambulatory patients we found high statistical significance of the postoperative results in the non-ambulatory patients (p<0,0001) (comparing the preoperative values with the postoperative values of the popliteal angle and also high statistical significance of the results comparing the separate age groups).
Table 3.
Non-ambulatory patients preoperative popliteal angle
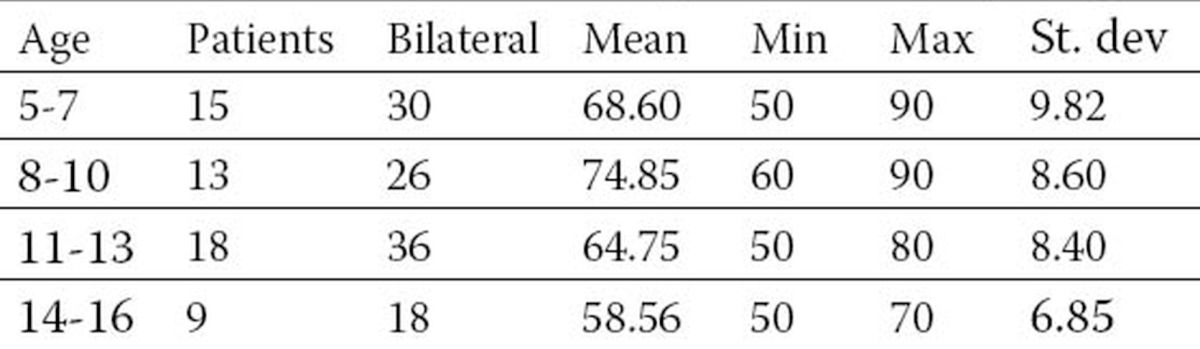
Table 4.
Non-ambulatory patients postoperative popliteal angle
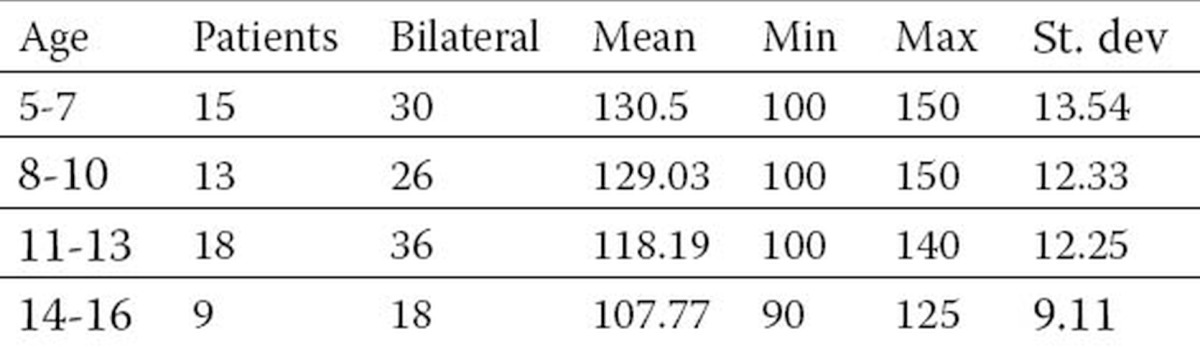
We did not find a statistical significance comparing the postoperative values of the popliteal angle comparing the ambulatory with the non-ambulatory group (p>0,005).
Also we found lower correction of the popliteal angle in the ambulatory patients compared to non-ambulatory in all age groups except in the group of 11-13y (in ambulatory patients group 5-7y 5,6% less, 8-10y 6,3% less, 11-13y 0,9% more, 14-16y 5,4% less).
4. DISCUSSION
Patients with spastic cerebral palsy are highly demanding both for their caregivers and for the clinicians treating these conditions in order to obtain the best possible result with the treatment of this condition. Gait abnormalities in children with cerebral palsy are the consequence of contractures across joints, muscle spasticity, and physically inappropriate muscle action. Though abnormalities involving one of the major joints of the lower extremity will usually have consequences on the function of the other joints, it is possible to recognize certain primary disorders at each joint. The most common gait abnormalities of the knee in patients with cerebral palsy occur in the sagittal plane. Based on the experience gained from performing gait analysis on more than 588 patients with cerebral palsy, four primary gait abnormalities of the knee have been identified: jump knee, crouch knee, stiff knee, and recurvatum knee (6). The treatment options of patients with spastic cerebral palsy range from conservative to surgical treatments depending on the severity of the condition (7, 8). Analyses have been made to understand the relationship between the joint contractures in cerebral palsy patients and their effect on stance and gait (9).
In the treatment of the flexion knee contracture in spastic cerebral palsy patients we focused on the soft tissue procedures. Authors have been describing various soft tissue procedures comprising distal hamstrings lengthening alone or combined with posterior knee capsulotomy and quadriceps mechanism shortening (2, 3, 4, 5). The values of the popliteal angle that we obtained postoperatively with our method of choice are comparable and consistent with the results of the similar studies (10, 11). Improvement of the crouch gait was obtained in the rehabilitation period. We did not find any wound complications. Three of the patients had overcorrection and achieved recurvatum of the knees.
5. CONCLUSION
We consider that, distal hamstrings lengthening is a simple surgical procedure with satisfying and reproducible improvement of the popliteal angle. With this procedure we can achieve improvement of the standing, walking and sitting abilities in children with spastic cerebral palsy.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.Gage JR. Surgical treatment of knee dysfunction in cerebral palsy. Clin Orthop Relat Res. 1990 Apr;(253):45–54. [PubMed] [Google Scholar]
- 2.Atar D, Zilberberg L, Votemberg M, Norsy M, Galil A. Effect of distal hamstring release on cerebral palsy patients. Bull Hosp Jt Dis. 1993;53(1):34–36. Spring. [PubMed] [Google Scholar]
- 3.Grujic H, Aparisi T. Distal hamstring tendon release in knee flexion deformity. Int Orthop. 1982;6(2):103–106. doi: 10.1007/BF00268652. [DOI] [PubMed] [Google Scholar]
- 4.Beals RK. Treatment of knee contracture in cerebral palsy by hamstring lengthening, posterior capsulotomy, and quadriceps mechanism shortening. Dev Med Child Neurol. 2001 Dec;43(12):802–805. doi: 10.1017/s0012162201001451. [DOI] [PubMed] [Google Scholar]
- 5.Kay RM, Rethlefsen SA, Skaggs D, Leet A. Outcome of medial versus combined medial and lateral hamstring lengthening surgery in cerebral palsy. J Pediatr Orthop. 2002 Mar-Apr;22(2):169–172. [PubMed] [Google Scholar]
- 6.Sutherland DH, Davids JR. Common gait abnormalities of the knee in cerebral palsy. Clin Orthop Relat Res. 1993 Mar;(288):139–147. [PubMed] [Google Scholar]
- 7.Chambers HG. Treatment of functional limitations at the knee in ambulatory children with cerebral palsy. Eur J Neurol. 2001 Nov;(8 Suppl 5):59–74. doi: 10.1046/j.1468-1331.2001.00039.x. [DOI] [PubMed] [Google Scholar]
- 8.Temelli Y, Akalan NE. Treatment approaches to flexion contractures of the knee. Acta Orthop Traumatol Turc. 2009 Mar-Apr;43(2):113–20. doi: 10.3944/AOTT.2009.113. doi:10.3944/AOTT.2009.113. [DOI] [PubMed] [Google Scholar]
- 9.Hoffinger SA, Rab GT, Abou-Ghaida H. Hamstrings in cerebral palsy crouch gait. J Pediatr Orthop. 1993 Nov-Dec;13(6):722–726. doi: 10.1097/01241398-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Sharps CH, Clancy M, Steel HH. A long-term retrospective study of proximal hamstring release for hamstring contracture in cerebral palsy. J Pediatr Orthop. 1984 Aug;4(4):443–447. doi: 10.1097/01241398-198408000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Atar D, Zilberberg L, Votemberg M, Norsy M, Galil A. Effect of distal hamstring release on cerebral palsy patients. Bull Hosp Jt Dis. 1993 Spring;53(1):34–36. [PubMed] [Google Scholar]


