Abstract
Introduction:
Diabetes mellitus, the most frequent endocrinology disease is a predisposing factor for infections. Diabetic patients have 4,4 times greater risk of systemic infection than non diabetics. Aim: a) To determine the prevalence and characteristics of acute infectious diseases in hospitalized diabetics; b) To correlate values of blood glucose levels and HbA1c with acute infections in hospitalized diabetics; c) To identify the etiology of infectious diseases.
Material and methods:
The study included 450 diabetic patients hospitalized in the 24-month period in the Intensive care unit of the Clinic for Endocrinology, Diabetes and Metabolic Disorders CCUS. In 204 patients (45,3%) there was an acute infectious condition and the following data was registered: a) gender and age; b) basic illness; c) laboratory parameters of inflammation (Le, CRP); d) blood glucose upon admission, parameters of glucoregulation (HbA1c, fructosamine); e) type of infection; f) verification of etiological agent; g) late complications of diabetes; and h) outcome.
Results:
Out of 204 diabetic patients with infection, there was 35,3% men and 64,7% women. More than half of patients (61%) were in the age group 61-80 years. The most common primary disease was Diabetes mellitus type 2. HbA1c and fructosamine were significantly increased in diabetic patients with acute infection compared to diabetics without acute infection. There is a positive correlation between HbA1c levels and CRP, and blood glucose and CRP in diabetic patients with acute infection. Most frequent infections: urinary tract infection (70,0%), followed by respiratory infections (11,8%), soft tissue infections (10,3%), generalized–bacteremia / sepsis (6,9%). The most common cause of urinary infection and generalized infection was Escherichia colli. The most common bacteria causing soft tissue infections was Staphylococcus aureus.
Conclusion:
Almost half (45,3%) of hospitalized diabetic patients had acute infectious condition. They present most frequently in women, aged 61-80 years, with Type 2 Diabetes mellitus. HbA1c and fructosamine were significantly increased in diabetic patients with acute infection. There is a positive correlation between the parameters of inflammation and glucoregulation in diabetics with acute infection. Most frequent was a urinary tract infection and the most common causative agent was Escherichia coli. The most common cause of soft tissue infections was Staphylococcus aureus. Out of 21 patients with verified soft tissue infections, 18 of them (85,7%) had confirmed diagnosis of diabetic microangiopathy diabetica. A total of 96,1% of patients fully recovered.
Keywords: Diabetes mellitus, blood glucose, acute infection
1. INTRODUCTION
Diabetes mellitus as the most frequent endocrinological disease is also a predisposing factor for common infections, but also those caused by pathogens that are rarely encountered in the general population. Patients with diabetes have 4,4 times greater risk of systemic infection than non-diabetics (1). Many factors increase susceptibility of diabetics to infections. Hyperglycemia has adverse effects on the immune system, causing impaired chemotaxis, adherence of microorganisms to polymorphonuclear leukocytes and lymphocytes, and disruption of phagocytosis. Hyperglycemia reduces the ability of white blood cells to break down phagocited microorganisms. Since the process of phagocytosis is basic defense against bacteria and fungi, the disruption of this process it thought to be responsible for a higher incidence of infections in diabetics.
On the other hand, infections are a major cause hyperglycemic crises in old and newly discovered diabetics. It is sufficient to mention the fact that ketoacidosis in nearly 30% of cases is triggered by infection (2). One of the most important metabolic features of infection is catecholaminemia, and it can disrupt the regulation of blood glucose in 4 ways: a) increased gluconeogenesis (directly or through increased secretion of cortisol, somatotropin hormone and glucagon), b) reduction of the intrinsic secretion of insulin in insulin-dependent diabetes, c) increasing the intrinsic insulin secretion, but also increased resistance to it. This phenomenon is reported in insulin-independent diabetes (the mechanism of resistance occurs in the insulin receptors, primarily skeletal muscle and liver), and d) increased utilization of glucagon, which leads to ketoacidosis.
Intensive care unit of the Clinic for Endocrinology is certainly one of the busiest departments concerning the number of infectious conditions in patients. In this study, urinary, respiratory, soft tissue infections- with emphasis on the diabetic foot, generalized infection (bacteremia, sepsis), and fungal infections were analyzed in patients who were admitted to the Intensive care unit of the Clinic of Endocrinology in the period of 24 months.
2. AIM
To determine prevalence and characteristics of acute infections in hospitalized diabetic patients.
To correlate blood glucose levels and HbA1c with acute infections in hospitalized diabetics.
Relevant microbiological tests to determine the etiology of infectious diseases in hospitalized diabetics.
3. MATERIALS AND METHODS
During the 24-month period (Jan. 2012–Dec. 2013) in the Intensive care unit of the Clinic for Endocrinology, Diabetes and Metabolic Disorders of Clinical center of Sarajevo University, there were 523 hospitalized patients. Seventy-three patients were not diabetics, so the study included 450 patients- diabetics. In 204 patients (45.3%) there was verified acute infectious condition, and 106 of those had confirmation of etiologic agents. In the group of patients with acute infection, the following data were recorded: a) gender and age; b) primary disease (DM type 1, DM type 2); c) laboratory parameters of inflammation (Le, CRP); d) Blood glucose on admission, the parameters of glucoregulation (HbA1C, fructosamine); e) Type of infection; f) etiological agent confirmation; g) Late complications of diabetes (microangiopathy, polyneuropathy) in soft tissue infections; and h) outcome (recovery, transfer to another hospital for further treatment, fatal outcome).
4. RESULTS
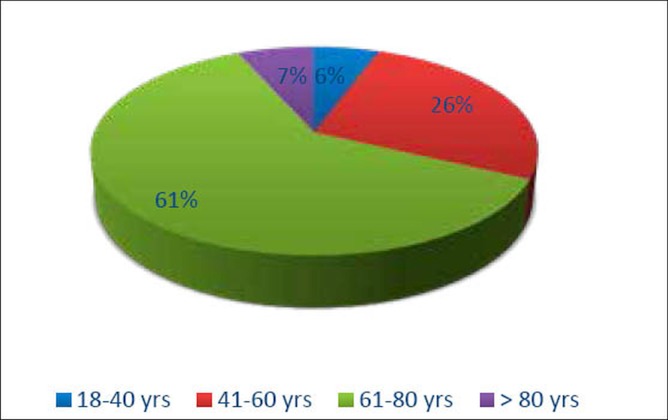
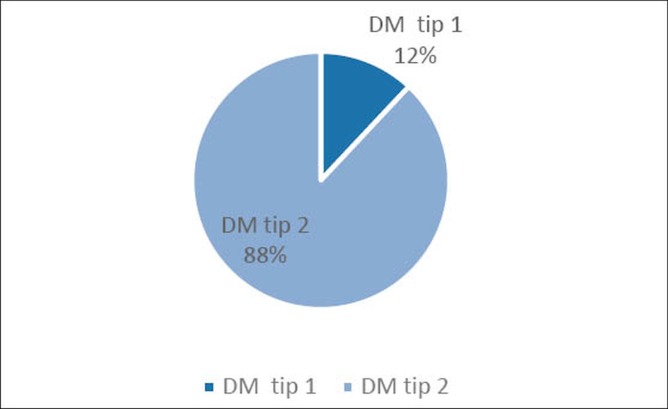
Out of 204 diabetic patients with infection, there were 72 (35,3%) men and 132 (64,7%) women. The age distribution and the primary disease are presented in Figure 1 and 2.
Figure 1.
Age distribution of diabetic patients with acute infection
Figure 2.
Primary disease in patients with acute infectious condition
More than half of patients (61%) were in the group 61-80 years (Figure 1). The most common primary disease was the Diabetes Mellitus Type 2 (Figure 2). In all 204 diabetic patients with acute infection, the laboratory parameters of inflammation and glucoregulation were taken (Table 1. and 2.). The correlation was determined between values of CRP as the most relevant parameter of acute phase of inflammation, and blood glucose and HbA1c values upon admission (Figure 3 and 4).
Table 1.
Parameters of inflammation in diabetic patients with and without acute infection respectively.
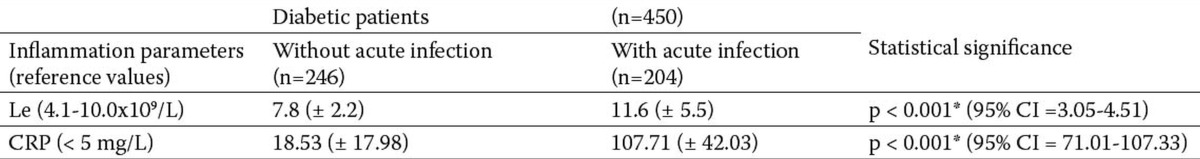
Table 2.
Glycemia and parameters of glucoregulation in diabetics with and without acute infection.
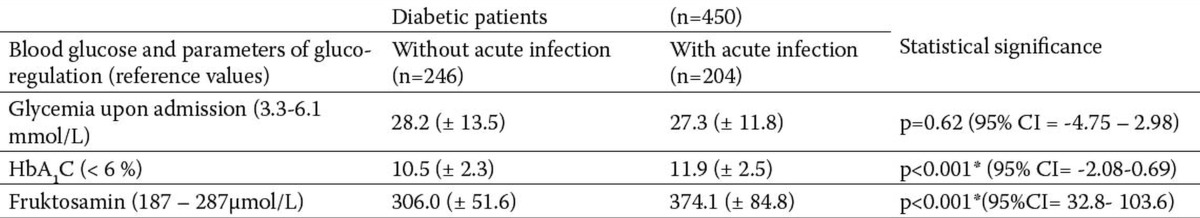
Figure 3.
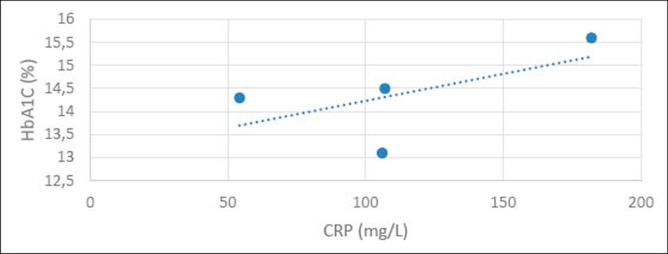
Correlation between HbA1c and CRP in diabetic patients with acute infections.
Figure 4.
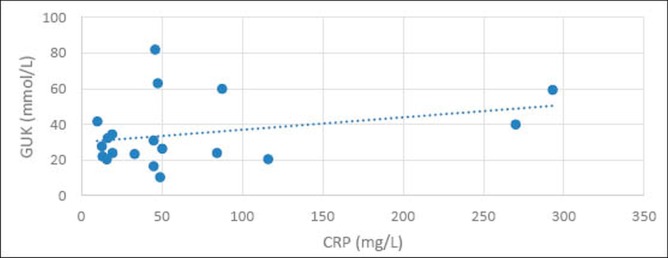
Correlation between glycemia upon admission and CRP in diabeticts with acute infections.
Laboratory parameters of inflammation-WBC and CRP were significantly elevated in diabetic patients with acute infection compared to diabetics without acute infection.
There is no statistically significant difference between levels of blood glucose upon admission in diabetic patients with acute infection and diabetic patients without acute infection. HbA1c and fructosamine were significantly increased in diabetic patients with acute infection.
There is a positive correlation between HbA1C levels and CRP (Figure 3), and glucose values at admission and CRP (Figure 4) in diabetic patients with acute infection.
In hospitalized diabetic patients, most frequent infections were: urinary tract infection (70,0%), followed by respiratory infections (11,8%), soft tissue infections (10,3%), generalized–bacteremia / sepsis (6,9%). Twenty-three patients had more than one infection (e.g. pneumonia and urinary tract infection or soft tissue infections and bacteremia). All kinds of infections were more common in women, except for soft tissue infections that were represented 1,3 times more frequently in men.
Microbiological tests have verified the etiologic agents in 106 hospitalized patients with acute infectious condition. As a material for confirmation were used: urine culture, sputum, blood culture, scrapings of skin/wound. (Figures 6, 7, and 8). The most common cause of urinary infection was Escherichia coli followed by Klebsiella pneumoniae and Pseudomonas aeruginosa (Figure 6).
Figure 6.
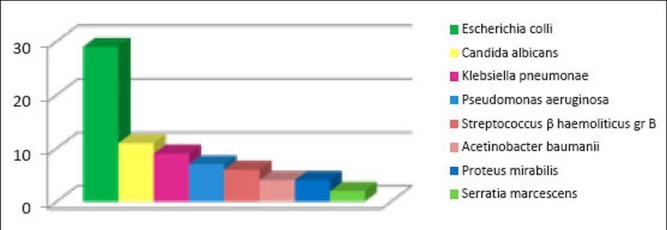
Etiologically verified causes of urinary tract infections.
Figure 7.
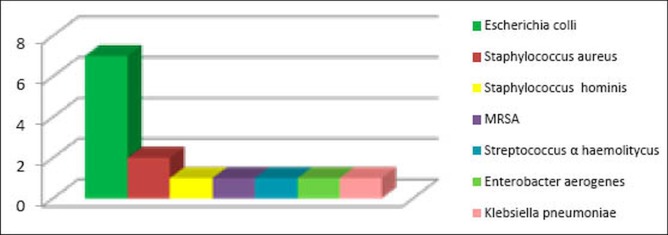
Etiologically verified causes of generalized infection.
Figure 8.
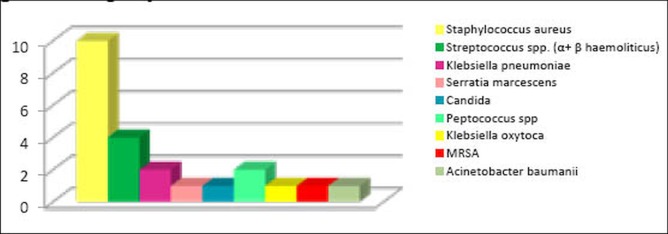
Etiologically verified causes of soft tissue infections.
Figure 5.
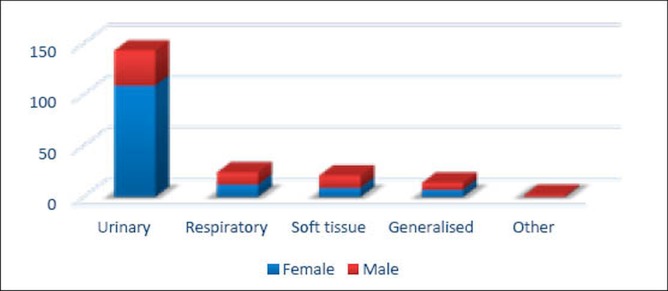
Frequency of certain types of infections in hospitalized diabetic patients.
The most frequent generalized infection was coliform septicemia. Escherichia coli was the cause of generalized infection in 50% of cases. (Figure 7).
The most common cause of soft tissue infections was Staphylococcus aureus (Figure 8). Three patients had soft tissue infection in which there were two or more pathogens. Out of 21 patients with verified soft tissue infections, 18 of them (85,7%) had confirmed diagnosis. Microangiopathia diabetica.
Out of total 204 patients, 196 (96,1%) were discharged from the hospital as recovered, 3 patients (1,4%) had a fatal outcome (two had soft tissue infection), and 5 patients (2,5%) were transferred to another hospital for further treatment (Clinic for Vascular Surgery and Orthopedic Surgery).
5. DISCUSSION
Our study showed that the infectious conditions usually occur in elderly patients with Diabetes mellitus type 2. Females were affected almost twice as often as men. The most common infectious condition in our study was the urinary infection. Hammar and colleagues in their study found that urinary infection occurs more frequently in women with diabetes mellitus type 2, and in older patients of both sexes (3).
C-reactive protein, as the most relevant parameter of the acute phase of infection had a progressive linear correlation with the level of glycemia upon admission and with HbA1c. (Figure 3 and 4). Nevertheless, a statistically significant difference was observed in HbA1c and fructosamine, but not in blood glucose values up on admission of patients with and without acute infection respectively. This finding is only a confirmation of Rueda and associates study, which showed that poorly regulated diabetes predisposes to severe infectious states, but the degree of hyperglycemia at admission is associated with increased risk of infection (4).
The advantage of our study is that attention has been given to certain types of infectious conditions, and was followed by a detailed analysis of the etiologic agents and predisposing conditions. Besides being a major cause of urinary infection, Escherichia coli was also the main cause of generalized bacteremia and sepsis. Michalia and associates found that despite the strict control and regulation of blood glucose, diabetics 1,7 times more likely develop septicemia in the Intensive care unit, in comparison with patients without diabetes (5).
In our study, over 85% of patients with soft tissue infections had predisposing diabetic microangiopathy. More than half of patients with soft tissue infections were men. This finding correlates with the Strba and associates study, who showed that the diabetic foot syndrome was present more often in type-2 diabetics with longer duration of disease, and those on insulin therapy, in men of older age, in diabetics with poor glycemic control and/or chronic micro vascular complications of diabetes (6).
Over 95% of patients in the study were discharged home as recovered. Soft tissue infections were the most common reason for extended hospitalization or transfer to other clinics for further treatment-amputation, and were co-morbidity in a very small percentage of deaths.
6. CONCLUSION
Based on our research, we reached the following conclusions:
* Out of 450 diabetics hospitalized in the ICU, 204 patients (45,3%) had verified acute infection.
* Out of 204 patients, there were 35,3% men and 64,7% women. More than half of patients (61%) were in the age group 61-80 years. In 88% of patients the basic disease was Diabetes Mellitus Type 2.
* Glycemia upon admission was significantly increased in diabetic patients with acute infection.
* HbA1c and fructosamine were significantly increased in diabetic patients with acute infection compared to diabetics without acute infection.
* There was a positive correlation between HbA1c levels and CRP, and blood glucose and CRP in diabetic patients with acute infection.
* The most frequent was urinary tract infection (70,0%) and the most common cause was Escherichia coli. The most common cause of generalized infection was Escherichia coli.
* The most common cause of soft tissue infections was Staphylococcus aureus. In patients with verified soft tissue infections, 85,7% of them had confirmed diagnosis. Microangiopathia diabetica.
* Recovery occurred in 96,1% of patients. Fatal outcome occurred in 1,4%, and 2,5% of patients were transferred to another hospital for further treatment.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.Stoeckle M, Kaech C, Trampuz A, Zimmerli W. The role of diabetes mellitus in patients with bloodstream infections. Swiss Med Wkly. 2008;138(35-36):512–519. doi: 10.4414/smw.2008.12228. [DOI] [PubMed] [Google Scholar]
- 2.Lin SF, Lin JD, Huang YY. Diabetic ketoacidosis: comparisons of patient characteristics, clinical presentations and outcomes today and 20 years ago. Chang Gung Med J. 2009;28(1):24–30. [PubMed] [Google Scholar]
- 3.Hammar N, Farahmand B, Gran M, Joelson S, Andersson SW. Incidence of urinary tract infection in patients with type 2 diabetes. Experience from adverse event reporting in clinical trials. Pharmacoepidemiol Drug Saf. 2010;19(12):1287–1292. doi: 10.1002/pds.2043. [DOI] [PubMed] [Google Scholar]
- 4.Rueda AM, Ormond M, Gore M, Matloobi M, Giordano TP. Hyperglycemia in diabetics and non-diabetics: effect on the risk for and severity of pneumococcal pneumonia. J Infect. 2010;60(2):99–105. doi: 10.1016/j.jinf.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Michalia M, Kompoti M, Koutsikou A, Paridou A, Giannopoulou P, et al. Diabetes mellitus is an independent risk factor for ICU-acquired bloodstream infections. Intensive Care Med. 2009;35(3):448–454. doi: 10.1007/s00134-008-1288-0. [DOI] [PubMed] [Google Scholar]
- 6.Strbová L, Krahulec B, Waczulíková I, Gaspar L, Ambrózy E. Characteristics of foot ulcers in diabetic patients. Vnitr Lek. 2009;55(10):918–924. [PubMed] [Google Scholar]