Abstract
Thyroidectomy is traditionally performed by the transcervical approach. To avoid or reduce visible scarring, diverse innovative surgical trials have been reported. Here we report a patient who underwent endoscopic thyroidectomy via a lateral keloid scar due to a previous traffic accident. A 30-year-old woman presented with a papillary thyroid carcinoma. Total thyroidectomy was performed via a keloid scar incision. The keloid scar was then revised. The total thyroidectomy was successful, resulting in no acute complications, such as neural injury, hematoma, or seroma formation. The keloid scar healed with excellent cosmetic results and the patient remains free of disease 12 months after excision. Endoscopic total thyroidectomy via a lateral keloid scar incision healed not only the physical disease but also the mental disease.
Keywords: Endoscopes, Keloid, Thyroid, Wound healing
INTRODUCTION
The conventional method for performing total thyroidectomy is usually through a 5- to 6-cm skin incision. This is a safe procedure that provides a wide surgical view to operators; however, the procedure sometimes results in an unsatisfactory scar. To avoid or reduce visible scarring, several alternative approaches have been attempted, such as minimally invasive video-assisted thyroidectomy (MIVAT), the transaxillary approach, and the bilateral axillo-breast approach (BABA) technique. Although these approaches have benefits for reducing external scars, they finally do result in damage due to other skin incision [1,2,3,4,5,6].
Hypertrophic scars and keloids are a problem that surgeons often encounter. Particularly in the head and neck region, these lesions are conspicuous and not easy for patients to conceal [7]. In some patients present with cosmetic concerns, thyroid carcinoma should be surgically treated and that can produce esthetic problems because thyroidectomy incision should be conducted trauma at the skin and sometimes made a keloid. In this article, we describe a patient with a previous large keloid scar who underwent total thyroidectomy via keloid scar incision and revision.
CASE REPORT
In November 2012, a 30-year-old woman presented for evaluation of bilateral thyroid masses. A 4×5 cm hypoechoic nodular lesion was detected on the right and a 6×7 cm hypoechoic nodular lesion was detected on the left. The lesions were diagnosed as papillary thyroid carcinoma, and we recommended total thyroidectomy. However, the patient did not wish to undergo total thyroidectomy because she was afraid of the large surgical scar that would remain on her anterior neck. Two years earlier, the patient had been in a traffic accident, as a result of which she had a 10 cm keloid scar on the left lateral neck area (Fig. 1A). For this reason, she had a growing fear of skin incision that we planned to perform endoscopic total thyroidectomy via a keloid scar incision.
Fig. 1.
The photography of serial scar change. (A) Preoperative state. Postoperative (B) 2 days, (C) 2 weeks, and (D) 12 months.
Under general anesthesia, the patient was placed in the supine position. The neck was extended to a greater degree than with the conventional transcervical approach to provide sufficient working space (Fig. 2A). A skin incision was made on the lateral keloid scar about 10 cm in length (Fig. 2B). A skin and subcutaneous dissection was carried out from the incision line toward the thyroid area, carefully retracting the sternocleidomastoid (SCM) muscle (*) inferiorly and strap muscle superiorly (Fig. 2C). We then met the left thyroid gland, preserving the recurrent laryngeal nerve and parathyroid gland around the thyroid (Fig. 2D). Thereafter the left thyroidectomy was done (Fig. 2E). In frozen biopsy, the left thyroid mass was confirmed to be papillary thyroid carcinoma.
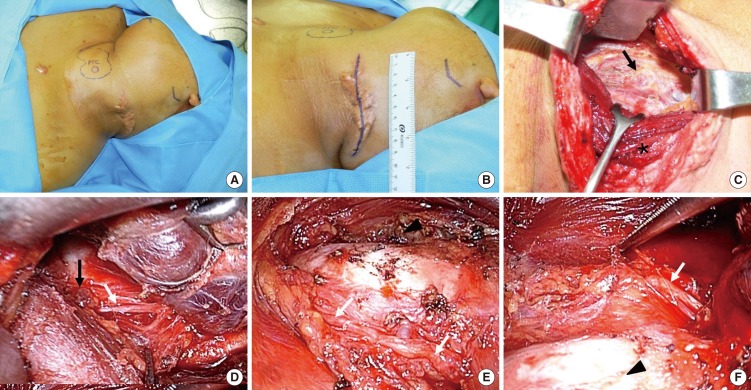
Fig. 2.
The photography of operative view. (A) In operation room, we can see the thyroid marking and left lateral keloid scar. (B) For the revision of keloid scar and surgical pathway, we draw the incision on the keloid scar. (C) The sternocleidomastoid muscle (*) was retracted inferiorly and the skin flap and strap muscle were retracted superiorly. We can see the left thyroid gland (black arrow). (D) The left thyroid was retracted superiorly. The recurrent laryngeal nerve was found (white arrow) and the inferior parathyroid was found (black arrow). (E) The recurrent laryngeal nerve (white arrows) and trachea were found. The right thyroid (arrowhead) was found over the trachea. (F) After right thyroid was removed, the right recurrent laryngeal nerve (white arrow) was found over the trachea (arrowhead).
After that, the subcutaneous flap (including the strap muscle) and the SCM muscle were pulled with a retractor to make a tunnel to approach the right thyroid. As the size of the thyroid was large, it could be identified easily while approaching it laterally. A flexible endoscope (10 mm, 0 degrees; Olympus, Tokyo, Japan) was inserted through a subcutaneous tunnel, which provided a good view of the right thyroid area. The assisting surgeon kept the endoscope in the correct position during the operation, and the main operating surgeon used both hands to move device through the subcutaneous tunnel. After identifying the inferior end of the thyroid, careful dissection between the gland and adjacent tissue was accomplished, minimizing injury to the recurrent laryngeal nerve and parathyroid. In this case, the recurrent laryngeal nerve was easily exposed during the careful dissection and we could safely preserve it by direct identification of the nerve (Fig. 2F).
The superior thyroid artery was identified at the superior border of the thyroid, which was divided and sealed. Thereafter, the thyroid was pulled out through the subcutaneous tunnel. After thyroid was removed, we did central lymph node dissection. A profuse irrigation of the surgical field, the incision line was closed layer by layer, and a negative suction drainage tube was inserted through the incision site. After that, for the prevention of keloids after surgery, intralesional corticosteroids are used during the immediate postoperative period (1 mL per application, once every 2 weeks, for the first 2 months after surgery). This patient was taken for the excision of her keloid, total thyroidectomy and intralesional steroid injection was done. Twelve months later, the scar was very satisfactory (Fig. 1). The excision of scar was diagnosis as keloid.
DISCUSSION
When injured, the skin must consistently and rapidly repair itself in order to maintain its external defense system. The result of wound healing is the formation of a scar at the site of tissue disruption. The rate and quality of scar formation vary among individuals, and alterations in this process may result in the development of a chronic wound or an abnormal scar. Keloids are hypertrophic-appearing scars that continue to evolve over time without a quiescent or regressive phase in the process of wound healing [8,9]. Keloids infiltrate into sur-rounding normal tissue and rarely regress, so that they continue to develop over time [10,11]. Keloids are a problem that affects patients' quality of life, not only for aesthetic reasons, but also primarily due to the associated symptoms (itching, pain, burning sensation, and intolerance to some tissues) [7], making it necessary to utilize an effective, specific treatment approach.
Especially in the head and neck region, these lesions are conspicuous, and patients typically present with cosmetic concerns. The head and neck area and the earlobes are common sites for keloid formation, usually after a surgery, trauma, or ear piercing, with an incidence of approximately 2.5% [12]. The most common difficulty in treating keloids is their recurrence following surgical excision.
Conventional transcervical thyroidectomy leaves neck scars that are easily visible after the operation. This is an unacceptable sequela for some patients, especially young women with keloids. Since the recent application of endoscopic techniques to head and neck surgeries, there have been only a few reports on the transcervical endoscopic approach to the thyroid [13]. In this article, we hypothesized that the endoscopic technique could permit both good visualization and clear identification of the important structures around the thyroid during thyroidectomy via a keloid incision. Because incision length is enough to obtain proper operative field, any type of incision line, from minimal scar to keloid or hypertrophic scar, is feasible for endoscopic thyroidectomy.
Based on our experience, it was difficult to secure a contralateral visual field of the thyroid in the total thyroidectomy, but the visual field could be obtained by using a retractor and flexible 10-mm endoscope. We then wished to identify the superior and inferior thyroid arteries and tie them, and also to preserve the recurrent laryngeal nerve by traction of the tie. However, the recurrent laryngeal nerve was easily exposed during the operation and we could safely preserve it by direct identification of the nerve.
Simple total excision of a keloid stimulates additional collagen synthesis, thus sometimes prompting rapid recurrence of a keloid even larger than the initial one [14,15]. Thus, surgical therapy should be combined with adjuvant treatment such as pressure therapy, corticosteroids, and radiotherapy.
This report suggests a surgical method to avoid the skin incision through lateral neck keloid incision. Endoscopic thyroidectomy via a keloid is technically feasible and secures a better cosmetic outcome.
ACKNOWLEDGMENTS
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT, and Future Planning (2013R1A1A1012542). This research was supported by the Leading Foreign Research Institute Recruitment Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (MEST) (2012K1A4A3053142).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Woo SH. Endoscope-assisted transoral thyroidectomy using a frenotomy incision. J Laparoendosc Adv Surg Tech A. 2014 May;24(5):345–349. doi: 10.1089/lap.2014.0110. [DOI] [PubMed] [Google Scholar]
- 2.Woo SH. Endoscope-assisted intraoral removal of the thyroid isthmus mass using a frenotomy incision. J Laparoendosc Adv Surg Tech A. 2013 Sep;23(9):787–790. doi: 10.1089/lap.2013.0216. [DOI] [PubMed] [Google Scholar]
- 3.Woo SH, Jeong HS, Kim JP, Park JJ, Baek CH. Endoscope-assisted frenotomy approach to median upper neck masses: clinical outcomes and safety (from a phase II clinical trial) Head Neck. 2014 Jul;36(7):985–991. doi: 10.1002/hed.23395. [DOI] [PubMed] [Google Scholar]
- 4.Woo SH, Kim JP, Baek CH. Endoscope-assisted extracapsular dissection of benign parotid tumors using hairline incision. Head Neck. 2014 Oct 28; doi: 10.1002/hed.23901. [Epub]. http://dx.doi.org/10.1002/hed.23901. [DOI] [PubMed] [Google Scholar]
- 5.Kim JP, Park JJ, Lee EJ, Woo SH. Intraoral removal of a thyroglossal duct cyst using a frenotomy incision. Thyroid. 2011 Dec;21(12):1381–1384. doi: 10.1089/thy.2011.0180. [DOI] [PubMed] [Google Scholar]
- 6.Kim JP, Park JJ, Jeon SY, Ahn SK, Hur DG, Kim DW, et al. Endoscope-assisted intraoral resection of external dermoid cyst. Head Neck. 2012 Jun;34(6):907–910. doi: 10.1002/hed.21674. [DOI] [PubMed] [Google Scholar]
- 7.Segev F, Jaeger-Roshu S, Gefen-Carmi N, Assia EI. Combined mitomycin C application and free flap conjunctival autograft in pterygium surgery. Cornea. 2003 Oct;22(7):598–603. doi: 10.1097/00003226-200310000-00003. [DOI] [PubMed] [Google Scholar]
- 8.English RS, Shenefelt PD. Keloids and hypertrophic scars. Dermatol Surg. 1999 Aug;25(8):631–638. doi: 10.1046/j.1524-4725.1999.98257.x. [DOI] [PubMed] [Google Scholar]
- 9.Slemp AE, Kirschner RE. Keloids and scars: a review of keloids and scars, their pathogenesis, risk factors, and management. Curr Opin Pediatr. 2006 Aug;18(4):396–402. doi: 10.1097/01.mop.0000236389.41462.ef. [DOI] [PubMed] [Google Scholar]
- 10.Murray JC. Scars and keloids. Dermatol Clin. 1993 Oct;11(4):697–708. [PubMed] [Google Scholar]
- 11.Nemeth AJ. Keloids and hypertrophic scars. J Dermatol Surg Oncol. 1993 Aug;19(8):738–746. doi: 10.1111/j.1524-4725.1993.tb00418.x. [DOI] [PubMed] [Google Scholar]
- 12.Zuber TJ, DeWitt DE. Earlobe keloids. Am Fam Physician. 1994 Jun;49(8):1835–1841. [PubMed] [Google Scholar]
- 13.Woo SH, Jeong HS, Kim JP, Park JJ, Baek CH. Endoscope-assisted intraoral removal of ectopic thyroid tissue using a frenotomy incision. Thyroid. 2013 May;23(5):605–608. doi: 10.1089/thy.2011.0468. [DOI] [PubMed] [Google Scholar]
- 14.Datubo-Brown DD. Keloids: a review of the literature. Br J Plast Surg. 1990 Jan;43(1):70–77. doi: 10.1016/0007-1226(90)90047-4. [DOI] [PubMed] [Google Scholar]
- 15.Salasche SJ, Grabski WJ. Keloids of the earlobes: a surgical technique. J Dermatol Surg Oncol. 1983 Jul;9(7):552–556. doi: 10.1111/j.1524-4725.1983.tb00853.x. [DOI] [PubMed] [Google Scholar]