Abstract
Background: Heart failure (HF) is a deadly, disabling and often costly syndrome world-wide. Unfortunately, there is a paucity of data describing its economic impact in sub Saharan Africa; a region in which the number of relatively younger cases will inevitably rise.
Methods: Heath economic data were extracted from a prospective HF registry in a tertiary hospital situated in Abeokuta, southwest Nigeria. Outpatient and inpatient costs were computed from a representative cohort of 239 HF cases including personnel, diagnostic and treatment resources used for their management over a 12-month period. Indirect costs were also calculated. The annual cost per person was then calculated.
Results: Mean age of the cohort was 58.0±15.1 years and 53.1% were men. The total computed cost of care of HF in Abeokuta was 76, 288,845 Nigerian Naira (US$508, 595) translating to 319,200 Naira (US$2,128 US Dollars) per patient per year. The total cost of in-patient care (46% of total health care expenditure) was estimated as 34,996,477 Naira (about 301,230 US dollars). This comprised of 17,899,977 Naira- 50.9% ($US114,600) and 17,806,500 naira −49.1%($US118,710) for direct and in-direct costs respectively. Out-patient cost was estimated as 41,292,368 Naira ($US 275,282). The relatively high cost of outpatient care was largely due to cost of transportation for monthly follow up visits. Payments were mostly made through out-of-pocket spending.
Conclusion: The economic burden of HF in Nigeria is particularly high considering, the relatively young age of affected cases, a minimum wage of 18,000 Naira ($US120) per month and considerable component of out-of-pocket spending for those affected. Health reforms designed to mitigate the individual to societal burden imposed by the syndrome are required.
Introduction
Heart failure (HF) has recently emerged as a global health problem [1]. It is a highly symptomatic syndrome that affects 2–3% of the population in high income countries especially in people above the age of 65 years [2], [3]. Approximately 15 million (out of 900 million) Europeans and 5.8 million (out of 300 million) Americans are affected by HF [4], [5]. The burden of HF has increased due to increasing elderly population as well as improved survival of patients with risks of HF such as acute myocardial infarction, hypertension and diabetes mellitus [6], [7]. In response, strategies for the effective management of the disease in the outpatient setting have been developed and applied [5]. This has led to improved survival in some countries [4], [8], [9]. In high-income countries, the economic burden of HF is high because it is associated with frequent hospital admissions [10], [11]. Moreover, management of HF places significant financial burden on patients, their families/care-givers and, as indicated, society as a whole [10], [12], [13].
Until recently, little was known about the emerging problem of non-communicable forms of HF supplementing traditional pathways to the syndrome in sub-Saharan Africa. Contemporary studies from South Africa[14], [15] and Nigeria[16]–[19] have built on historical reports to demonstrate that the aetiology, natural history and indeed case profile of HF (i.e. more women and younger individuals affected in the prime of their life) is different from high-income countries. As such, HF is now responsible for 7–10% of medical admissions in the region [16], [19], [20]. Significantly, given its potential enormous cost implications (both related to direct health care costs and economic burden on affected individuals and their families) there is virtually no data on the economic burden of HF in sub-Saharan African countries and major populaces such as Nigeria.
Study Aims & Objectives
The aim of this study, therefore, was to determine the consumption of health care resources for the treatment of HF in Abeokuta, Nigeria and to estimate overall healthcare costs associated with its management in a large and representative cohort of affected cases. Data were used to estimate the annual cost of HF in the region to inform health care policy towards efficient use of resources to mitigate the individual to societal impact of the syndrome.
Material and Methods
Ethics Statement
This study was approved by the Federal Medical Center Abeokuta and University of Witwatersrand Health Research Ethics Review Committees and all the participants provided informed consent in writing, in accordance with the Declaration of Helsinki [21].
Study site
The study was undertaken at the Federal Medical Centre, Abeokuta, Ogun state, southwest Nigeria. The state has a population of about 3,751,140 inhabitants [22]. Abeokuta is the state capital and has a population of about a million people [23]. As described previously [19], Federal medical center Abeokuta is a tertiary institution that receives referrals from primary and secondary health facilities within and outside the state. All the patients that were discharged alive were given monthly appointments for clinical review as well as for refill of their medications. Patients pay out of pocket and many may not be able to buy medication that will last for longer period. Home based nursing care is not in existence in the city and in many parts of the country. Patients are often taken care of by their relations. Healthcare cost in the city of Abeokuta and in most parts of Nigeria is generally borne by the patient through out of pocket payment payments.
Only a small proportion of the Nigerian population has access to social health insurance [24]–[26]. However, there exist very strong family bonding and extended family systems where poor patients are assisted by their wealthy or well-to-do family members. The limited coverage of social health insurance in Nigeria is a very big challenge to the achievement of universal health coverage and health care delivery in the country.
Study design and sample
As described previously [19], the Abeokuta HF registry was a hospital based, prospective, observational registry that ran from January 2009 to December 2010 which was established to determine the current clinical profile of HF in the city as well as to assess typical clinical outcomes and healthcare costs (the focus of this report) associated with HF. A more detailed description of the registry has been documented [19]. Briefly, all cases of HF presenting to the hospital were captured into the database. Private health facilities, primary health centres as well as health workers were sensitized on the existence of the registry with good response. To a large extent, the sample was fully representative of the population. During the period, HF was responsible for 9% of total medical admission [19] a figure that is consistent with equivalent reports from other parts of Africa [14], [18], [20].
Data collection
A specific data extraction proforma was developed and used to obtain data on resource consumption in those cases enrolled in the Abeokuta HF registry. The clinical diagnostic criteria employed in the diagnosis of HF have been described elsewhere [19]. Clinical diagnoses were coded using the International Classification of Diseases (ICD-10) coding system [27]. The proforma was used to extract the following direct outpatient and inpatient cost categories as shown in the textbox below.
Health Care Expenditure
Direct Health Care Costs
The inpatient costs include the cost of medical and nursing care, cost of investigations and drugs ( Table 1 ). It also includes the cost of surgery and procedures as well transportation to and from the hospital. Personnel costs include the opportunity cost of medical care, nursing as well as ancillary support by other health workers. The wages of these health workers were derived from the Federal Government of Nigeria salary scales. This included their basic salary; call duty allowance, hazard allowance and housing allowance. We did not capture cost associated with purchase of medications over the counter, cost of alternative medical care which is common in Africa, aids, home modifications etc. We assume that these categories are likely to represent a very small percentage of the total costs identified from this study. We also did not capture capital costs.
Table 1. Shows summary of the cost components.
| Cost component |
| A. |
| B. In-patient care |
| i. Direct cost |
| Hospital care (Medical consultation) |
| Nursing care, utility fees, accommodation and feeding and ward consumables including oxygen) |
| Medications |
| Medications |
| Surgery and procedures |
| Transportation |
| Surgery and procedures |
| ii. Indirect cost- the days of lost work (productivity loss) |
| B. Out-patient care |
| i. Direct cost |
| Clinic visits |
| Laboratory investigations |
| Medications |
| Transportation |
| ii. Indirect cost-the days of lost work (productivity loss) |
Indirect Health Care Costs
For indirect costs, the days of lost work (productivity loss) were calculated and the minimum wage used to monetize them.
In-patient cost
The standard costing table (unit costs) of the Federal Medical Center, Abeokuta for the year 2010 was used for computing the cost of consultations, hospital admissions, medical consumables, medical investigations, and drug therapy ( Table 1 ). It was assumed that the cost of single hospital admission covers the cost of treatment in the emergency room as well as in the medical ward. The cost of medications was taken as a whole. We assumed that the cost of medications had remained unchanged throughout the year.
Out-patient costs
This was also grouped into direct and indirect costs. All the patients that were discharged alive were given monthly appointments for clinical review as well as for refill of their medications ( Table 1 ).
Specific costs
Cost of drugs
The cost of drugs was based on the hospital's price list (which includes the tender prices plus a 10% mark up or dispensing fee). The frequency of use of the various categories of drugs was based on the findings from the HF registry. The most frequent dosage was used for cost calculation. We did not account for increase or reduction in dose of the drugs during the course of treatment. We assumed that substitution of one class or brand of medication occurred without additional costs.
Cost of Laboratory and diagnostic tests
The cost of all laboratory and diagnostic tests (haematological, biochemical, microbiological, chest radiography, electrocardiography and echocardiography) were based on the price list of the hospital in 2010. The rate of consumption of these items was also garnered from the HF registry.
Cost of Surgery and Procedures
The cost of surgeries and procedures were obtained from the Lagos State University Teaching Hospital (LASUTH), as well the Reddington multi-specialist hospital, Lagos where majority of the surgeries and procedures were performed [28], [29]. The surgeries and procedures include valve surgeries, coronary angioplasty/stenting, pericardiectomies etc. Total cost was multiplied by the frequency of the surgeries and procedures.
Estimation of indirect costs
The human capital approach was used to estimate the indirect cost. The average annual earning of the patients was estimated based on their occupational group. These were used to calculate their average daily earnings. The product of the working days lost and average daily earnings provided the productivity losses associated with HF in the study and these were assigned monetary values.
Cost analyses
All available costs (as detailed above) associated with in-patient care, out-patient care as well as the opportunity costs associated with HF management in the city were computed for the year 2010. An annual, prevalence based approach was employed in estimating the cost of the resources used for the management HF [10]–[12], [30]. Healthcare costs were then expressed in the local currency-Naira, (and converted to US Dollar [$US] at a rate of 150 Nigerian Naira to $US1 in 2010).
Results
Outpatient and inpatient costs were computed from a representative cohort of 239 HF cases over a 12-month period for the year 2010. Table 2 provides a summary of the study cohort used to derive all HF-related health care activities. Mean age was 58.0±15.1 years, 46.9% were female and around one third were aged ≤55 years and in the prime of their potential working life.
Table 2. Sociodemographic profile of the HF subjects seen in 2010.
| Variable | Value |
| Gender | |
| Male (n/%) | 127(53.1) |
| Female (n/%) | 112(46.9) |
| Mean age (years) | 58.0(15.1) |
| Median age(years) | 60 |
| Age range (years) | |
| <24 | 8(3.3) |
| 25–34 | 15(6.3) |
| 35–44 | 21(8.8) |
| 45–54 | 40(16.7) |
| 55–64 | 59(24.7) |
| 65–74 | 63(26.4) |
| > = 75 | 33(13.8) |
| Marital status | |
| Single | 32(13.4) |
| Married | 168(70.3) |
| Widow/widower | 5(2.1) |
| Separated/Divorced | 34(14.2) |
| Educational level | |
| No formal education | 88(36.8) |
| Primary (< = 6 years) | 60(25.1) |
| Secondary (6–12 years) | 44(18.4) |
| Post-Secondary/University/Postgraduate (>12years) | 47(19.7) |
| Occupation | |
| Unemployed | 20(8.4) |
| Unskilled labour | 146(61.1) |
| Skilled labour | 18(7.5) |
| Professional | 24(10.0) |
| Pensioner/Retiree | 31(13.0) |
| Place of residence | |
| Within Abeokuta city | 138(57.7) |
| Outside Abeokuta but within Ogun State | 53(22.2) |
| Outside Abeokuta and outside Ogun State | 48(20.1) |
| Monthly Income of subjects in Naira(Median value) | |
| Unemployed* | 18000(120USD) |
| Unskilled labour | 90,000(600USD) |
| Skilled labour | 240,000(1600USD) |
| Professional | 480,000(3200USD) |
| Pensioner/Retiree | 330,000(2200USD) |
| Aetiology of HF | |
| Hypertensive HF | 195(81.6) |
| Dilated Cardiomyopathy | 14(5.9) |
| Pericardial Diseases | 8(3.3) |
| Rheumatic Heart Disease | 4(1.7) |
| Others | 4(1.7) |
| Co-morbidities | |
| Hypertension | 185(77.4) |
| Osteoarthritis | 49(20.9) |
| Atrial fibrillation | 37(15.5) |
| Diabetes Mellitus | 24(10.0) |
| Chronic Obstructive pulmonary disease | 7(2.9) |
| Others | 6(2.4) |
*Allocated minimum wage in the country.
Cost of components of in-patient care
Cost of hospital care
The following were computed for the subjects: medical consultation (N300/day), nursing care (N200/day), utility fees(N400/day), accommodation and feeding (N900/day) and average cost of ward consumables/patient/admission (N3500/patient)The estimated cost of hospital care for the year was about 5.5 million naira (about $U36,500).
Cost of laboratory investigations
The laboratory investigations considered in the costing is as shown in Table 3(A) .The estimated cost was approximately 3.8 million naira (about $US28, 000).
Table 3. Cost of investigations (In-patient).
| A. In-patient Investigations | |||||
| Investigation | Cost per test | Percent | Number | Cost (Naira) | Cost (US Dollars) |
| Urinalysis | 200 | 88 | 225 | 45000 | 300.0 |
| Full blood count | 1350 | 96 | 229 | 309150 | 2061.0 |
| Blood sugar | 400 | 96 | 229 | 91600 | 610.7 |
| Electrolyte and Urea | 2500 | 96 | 229 | 572500 | 3816.7 |
| Lipid profile | 3500 | 65 | 155 | 542500 | 3616.7 |
| Electrocardiography | 2500 | 96 | 229 | 572500 | 3816.7 |
| Echocardiography | 5000 | 92 | 220 | 1100000 | 7333.3 |
| Chest X-Ray | 2000 | 96 | 229 | 458000 | 3053.3 |
| Cardiac enzyme | 5000 | 0.8 | 2 | 10000 | 66.7 |
| INR | 3500 | 10 | 24 | 84000 | 560.0 |
| HIV screening | 500 | 46 | 111 | 55500 | 370.0 |
| Liver function tests | 3000 | 50 | 120 | 360000 | 2400.0 |
| Total Cost | 3840750 | 28005.0 | |||
| B. Out-patient investigations | |||||
| Investigation | Cost per test | Percent* | Number | Cost (Naira) | Cost (US Dollars) |
| Electrocardiography | 2500 | 96 | 197 | 492500 | 3283.3 |
| Electrolyte and Urea | 2500 | 96 | 197 | 492500 | 3283.3 |
| Total | 5000 | 96 | 394 | 985000 | 6566.7 |
Note: Cost based on the hospital costing list for 2009.
Note: Calculation based on those that survived, it is assumed that same proportion on admission.
performed these investigations during follow up.
Cost of medications
This includes cost of standard drugs for the management of HF, as well as other drugs such as antituberculous drugs used for the management of T.B pericarditis. The estimated cost of drugs was N6, 565,527 (about $US43770) (see Table 4 ).
Table 4. In-patient cost of medications.
| Drug | Route | Dose | Dosing | Unit cost (Naira) | Cost per daily dose(Naira) | Total Cost(Naira) | Number of subjects | Total cost in US Dollars |
| Frusemide | IV | 40 mg | 3 | 20 | 60 | 13620 | 227 | 90.8 |
| Frusemide | Oral | 40 mg | 3 | 5 | 15 | 3405 | 227 | 22.7 |
| Amlodipine | Oral | 5 mg | 1 | 15 | 15 | 615 | 41 | 4.1 |
| Lisinopril | Oral | 10 mg | 1 | 15 | 15 | 3330 | 222 | 22.2 |
| Spironolactone | Oral | 25 mg | 1 | 10 | 10 | 2030 | 203 | 13.5 |
| Digoxin | Oral | 0.125 mg | 1 | 5 | 5 | 1015 | 203 | 6.8 |
| Carvedilol | Oral | 6.25 mg | 1 | 25 | 25 | 550 | 22 | 3.7 |
| Hydrallazine | Oral | 25 mg | 1 | 5 | 5 | 90 | 18 | 0.6 |
| Isosorbide dinitrate | Oral | 10 mg | 1 | 220 | 220 | 3960 | 18 | 26.4 |
| Heparin (LMW) | SC | 40 mg | 1 | 1350 | 1350 | 209250 | 155 | 1395.0 |
| Warfarin | Oral | 2.5 mg | 1 | 40 | 40 | 1120 | 28 | 7.5 |
| Atorvastatin | Oral | 10 mg | 1 | 180 | 180 | 7380 | 41 | 49.2 |
| Amiodarone | Oral | 200 mg | 2 | 20 | 40 | 200 | 5 | 1.3 |
| Antibiotics (Augmentin) | IV | 600 mg | 3 | 600 | 1800 | 399600 | 222 | 2664.0 |
| Antibiotics (Augmentin) | Oral | 625 mg | 2 | 170 | 340 | 75480 | 222 | 503.2 |
| Prednisolone | Oral | 30 mg | 1 | 30 | 30 | 7170 | 239 | 47.8 |
| Anti-tuberculous therapy | Oral | Multiple drugs | 1 | 60 | 60 | 480 | 8 | 3.2 |
| Aspirin | Oral | 75 mg | 1 | 2 | 2 | 208 | 104 | 1.4 |
| Total | 729503 | 4863.4 | ||||||
| Grand Total | 6565527 | 43770.2 |
Source: Federal Medical Centre, Abeokuta costing list, Median length of hospital stay = 9 days, 1 US Dollar = 150 naira (2010).
Cost of Surgery/Procedures
As stated earlier, we estimated the cost of surgery/procedures for the few patients who were able to afford them. This was estimated to cost N1, 092, 000 (about $US72800) – see Table S1.
Cost of transportation
This was calculated to cost N216, 600 (about $US1, 444) see Table S2.
Indirect in-patient care cost
This was estimated to cost N17, 806,500 Naira ($US118, 710) – see Table 5A .
Table 5. Indirect cost (In-patient/outpatient).
| A. Indirect in-patient care cost | |||||||
| Occupation | Monthly Income | Daily income | Daily income(Dollars) | No of Subjects | Total Income lost/day(Naira) | Income lost (Naira)** | Income lost (Dollar)** |
| Unemployed* | 18000 | 900 | 6 | 20 | 18000 | 162000 | 1080 |
| Unskilled | 90000 | 4500 | 30 | 146 | 657000 | 5913000 | 39420 |
| Skilled | 240000 | 12000 | 80 | 18 | 216000 | 1944000 | 12960 |
| Professional | 480000 | 24000 | 160 | 24 | 576000 | 5184000 | 34560 |
| Pensioners | 330000 | 16500 | 110 | 31 | 511500 | 4603500 | 30690 |
| Total | 1158000 | 57900 | 386 | 239 | 1978500 | 17806500 | 118710 |
| B. Indirect out-patient care cost | |||||||
| Occupation | Monthly Income | Daily income | Daily income(Dollars) | No of Subjects | Total Income lost/day(Naira) | Income lost (Naira)** | Income lost (Dollar)** |
| Unemployed* | 18000 | 900 | 6 | 14 | 12600 | 151200 | 1008 |
| Unskilled | 90000 | 4500 | 30 | 130 | 585000 | 7020000 | 46800 |
| Skilled | 240000 | 12000 | 80 | 15 | 180000 | 2160000 | 14400 |
| Professional | 480000 | 24000 | 160 | 21 | 504000 | 6048000 | 40320 |
| Pensioners | 330000 | 16500 | 110 | 25 | 412500 | 4950000 | 33000 |
| Total | 1158000 | 57900 | 386 | 205 | 1694100 | 20329200 | 135528 |
Note: Income loss was based on 5 working days in a week, **Income loss was based on median Los of 9 days.
Note: *Assigned the minimum wage in Nigeria, Income loss was based on 5 working days in a week,
Because most mortality occurred early, it was assumed that 205 subjects completed follow up, 1dollar = 150Nigerian Naira.
Cost of components of out-patient care
Out-patient clinic visit
This was based on the cost of medical consultations (N250/visit) and nursing/ancillary services (N200/visit). The calculated total cost was N29, 700 ($US198 US dollar) – see Table S3.
Cost of out-patient investigations
This was calculated for subjects who survived initial hospital admission. It was assumed that the proportion of subjects who had these tests during admission were also able to have them done during the follow up period. It was estimated to cost N985, 000 ($US 6567 – see Table 3B .
Cost of outpatient medications
This is shown in Table S4. It was estimated to cost N9, 154,168 ($US61, 028).
Cost of outpatient transportation
This constituted a greater proportion of the out-patient care cost. It was calculated as N9, 717, 000 ($US 64,780) – see Table S5.
Indirect out-patient care cost
This was estimated to cost about 20,329,200 Naira ($US135, 528) – see - Table 5B .
Summary of in-patent and out-patient care cost
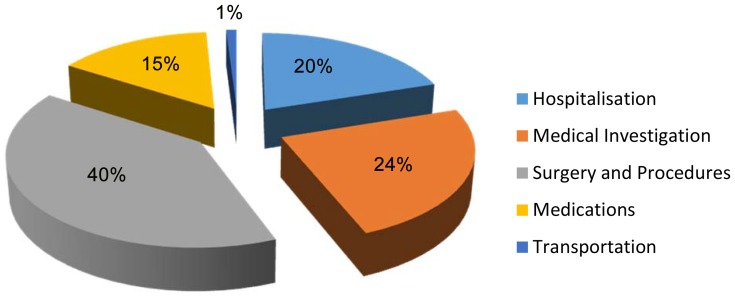
The total cost of in-patient care was estimated as N34, 996, 477 ($US301, 230). This comprised of N17, 899, 977 (50.9%, $US114, 600) and N17, 806,500 (49.1%, $US118, 710) for direct and in-direct costs respectively. Direct costs were responsible for 61% of in-patient care costs. About 40% of the direct cost was due to surgery/procedures. Hospitalization, medical investigations, drug therapy, and transportation accounted for 20%, 24%, 15%, and 1% respectively, of costs –see Table 6 (A) and Figure 1 .
Table 6. Summary of various aspects of costs of in-patient/out-patient care.
| A. Summary of various aspects of costs of in-patient care | ||
| Item | Total cost (in Naira) | Total Cost in US Dollars |
| Hospitalization | 5475100 | 36500.7 |
| Investigations | 3840750 | 28005 |
| Medications | 6565527 | 43770.2 |
| Surgery and procedures | 10920000 | 72800 |
| Transportation | 216600 | 1444 |
| Total Direct Cost | 17189977 | 114600 |
| Total Indirect Cost | 17806500 | 118710 |
| Grand total | 34996477 | 233310 |
| B. Summary of various aspects of costs of out-patient care | ||
| Item | Total cost (in Naira) | Total Cost in US Dollars |
| Clinic visit | 1107000 | 7380 |
| Investigations | 985000 | 6567 |
| Medications | 9154168 | 61028 |
| Transportation | 9717000 | 64780 |
| Total Direct cost | 20963168 | 139754 |
| Indirect cost | 20329200 | 135528 |
| Grand total | 41292368 | 275282 |
Figure 1. Components of direct cost (In-patient).
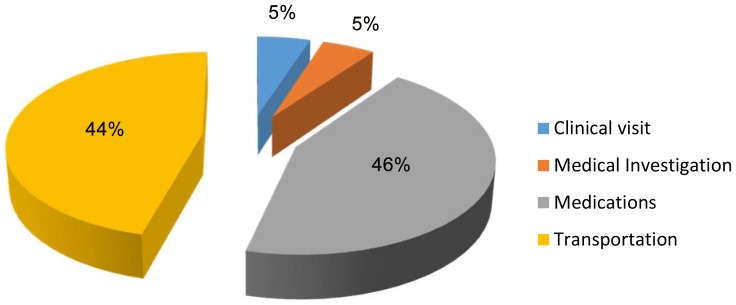
Table 6(B) summarizes the components and total estimated cost of out-patient care. It was estimated as N41, 292, 368 ($US 275,282 UD dollars). Direct and in-direct costs were N20, 963,168 ($US139, 754) and N20, 329,200 ($US135, 528) respectively, constituting 51% and 49% of total out-patient care costs. Transportation, medications, clinic visits and medical investigations contributed 46%, 44%, 5% and 5% respectively to these costs - see ( Figure 2 ).
Figure 2. Components of direct cost (out-patient).
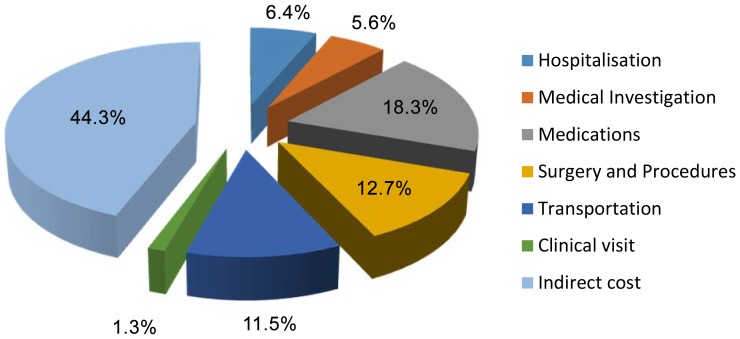
Total cost
The total estimated cost of care of HF in Abeokuta for the year 2010 was N76, 288,845 ($US508, 595) translating to N319, 200 ($US2, 128) per patient per year. The proportional contribution of in-patient and out-patient cost were 46% and 54% respectively. The contribution of various components to the total cost is shown in Figure 3 .
Figure 3. Percentage contribution of different components to total cost.
Discussion
To our knowledge this is the first systematic attempt at estimating the cost of HF in Nigeria; a major populace of sub-Saharan Africa. We have calculated the cost from an individual perspective whilst calculating the total cost per annum overall from a societal perspective. Effort was made to capture all the HF patients in the city of Abeokuta during the study period. All cases of HF presenting to the two major hospitals in the city were captured into the database. Private health facilities, primary health centres as well as health workers were sensitized on the existence of the registry with good response. To a large extent, the sample was representative of the population. During the period, HF was responsible for 9% of total medical admission similar to earlier report from other parts of Africa [14], [18], [20]. The main findings of the study are - 1. The total cost of HF or cost per patient per year is enormous considering the context of a developing economy where out-of-pocket expenses is the main means of health care financing;2. Furthermore the estimated cost of HF was fairly distributed between in-patient and out-patient care; 3. A large proportion of direct cost for in-patient care was due to surgery and medical procedures and; 4. Out-patient medications and transportation was responsible for 90% of direct cost of out-patient care. The huge cost of HF has been well documented by several reports both at the individual and population levels. Data from the National Heart and Lung Institute of the United Kingdom shows that the cost of HF per person is approximately 8500 Pounds. At the national level HF costs about 39.2 billion US dollars in America (about 2% of US healthcare budget) [31]. Similar data have been reported from other countries [10], [11] [12], [32].
The distribution of cost of HF in our setting is different from that observed in high income countries [10], [11], [32] but similar to one report from Brazil [12]. There has not been any report from Africa to compare our findings with. The contribution of hospital care cost in these countries ranged from 53–75%. Cost of outpatient care was in the range of 4–31% while the cost of drug therapy was between 6–8% of the total cost of care. The pattern of heart diseases as well as level of technological development influences the mode of care as well as utilization of sophisticated and expensive medical equipment, procedures and consumables which are obviously needed for the care of HF patients. The consumption of these is higher in high income countries than in our setting. This is clearly shown by the impact of surgery/procedures on the cost of hospital care. The few cases (out of the many that needed this) that had surgery for valvular diseases or coronary interventions escalated the hospital care cost in our study.
Other determinants of hospital cost will also include length of hospital stay [10], [13]. (in which our report is similar to European data but longer than the mean length of hospital stay in the USA) Cost of management of co-morbidities has also been shown to account for higher cost of hospitalization in high income countries. In one report on Medicare claims, HF accounted for only15% of the total in-patient cost while 57% were associated with other co-morbid conditions [33]. This may probably be responsible for the huge cost of hospitalization in high income countries compared to our environment.
Due to lack of community based or nurse-led or home care of HF patients in our setting, our patients are given shorter out-patient appointments in order to refill their medications. This is responsible for the high cost attributable to transportation in our report. Because of the younger age of our subjects, HF in our setting is, therefore, associated with longer disability adjusted life years and by extension a huge cost to the society at large.
With the changing demographic and epidemiological landscape in Nigeria coupled with the rising burden of cardiovascular risk factors and non-communicable diseases (especially hypertension) in the country, the rate of HF is predicted to rise if preventive measures are not put in place at all levels. This will put a lot of strain in an already weak health system. The high cost of surgical interventions and procedures is out of the reach of the average Nigerian. Prevention of conditions requiring this mode of care such as rheumatic heart disease, tuberculosis (because of pericarditis) and coronary artery disease should be a priority for the country at large. Furthermore the need for a functional, effective and efficient social health insurance system in the country cannot be overemphasized considering the fact that majority of those afflicted by HF are poor and are not likely to sustain the treatment of their illness for a long time. There is also need to develop community based HF care in the country as this will reduce the cost of outpatient care which is largely contributed by the cost of frequent transport to-and-from the health facility.
Limitations
This is a hospital based study. Although we tried as much as possible to capture all the HF cases in the city during the study period, there is still the possibility that mild cases may have been missed out especially those that were managed in the out-patient clinic.
We also did not assess cost based on the severity of HF (NYHA class). Studies have shown that those in NYHA class IV were 8–30 times more expensive to manage compared to those in NYHA class II [30], [34], [35]. Age and sex-specific cost analysis was also not carried out. We also did not include the cost of co-morbidities neither did we capture cost due to alternative medicines (which is common in Africa), over the counter purchases, capital cost and indirect cost by care givers as well as the general cost to the society. These are potential areas of research in our community in the future.
Conclusion
Our data shows the profound impact and importance of HF as a major public health problem in a developing economy like Nigeria that is still battling with communicable diseases. The annual individual cost of HF is high coupled with the fact that of pocket expenses in the country is over 90%. There is therefore need to reduce this expenditure through control of risk factors for HF in the society especially high blood pressure, reduction in hospital as well as out-patient care cost through the development of community HF care programmes in the country.
Supporting Information
Cost of procedures (In-patient).
(DOCX)
Cost of transport (In-patients).
(DOCX)
Cost of clinic visits (Out-patient).
(DOCX)
Cost of medications (Out-patient).
(DOCX)
Cost of transport (Out-patient).
(DOCX)
Acknowledgments
All authors had full access to all the data in the study. Okechukwu.S Ogah is a Doctoral Student at the University of the Witwatersrand, South Africa. Simon Stewart is supported by the National Health and Medical Research Council of Australia.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors would like to acknowledge support from the BMBF (Ministry of Research and Education, Germany) and the Sir Maurice Hatter Foundation for funding the travel of OSO to Cape Town, South Africa, in May 2014. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Cook C, Cole G, Asaria P, Jabbour R, Francis DP (2014) The annual global economic burden of heart failure. Int J Cardiol 171:368–376. [DOI] [PubMed] [Google Scholar]
- 2. Redfield MM, Jacobsen SJ, Burnett JC Jr, Mahoney DW, Bailey KR, et al. (2003) Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 289:194–202. [DOI] [PubMed] [Google Scholar]
- 3. Mosterd A, Hoes AW, de Bruyne MC, Deckers JW, Linker DT, et al. (1999) Prevalence of heart failure and left ventricular dysfunction in the general population; The Rotterdam Study. Eur Heart J 20:447–455. [PubMed] [Google Scholar]
- 4. Wijeysundera HC, Machado M, Wang X, Van Der Velde G, Sikich N, et al. (2010) Cost-effectiveness of specialized multidisciplinary heart failure clinics in Ontario, Canada. Value Health 13:915–921. [DOI] [PubMed] [Google Scholar]
- 5. McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Bohm M, et al. (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 33:1787–1847. [DOI] [PubMed] [Google Scholar]
- 6.Nagamine M, Jiang HJ, Merrill CT (2006) Trends in Elderly Hospitalizations, 1997–2004: Statistical Brief #14. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD).
- 7.Hines A, Stranges E, Andrews RM (2006) Trends in Hospital Risk-Adjusted Mortality for Select Diagnoses by Patient Subgroups, 2000–2007: Statistical Brief #98. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD). [PubMed]
- 8. MacIntyre K, Capewell S, Stewart S, Chalmers JW, Boyd J, et al. (2000) Evidence of improving prognosis in heart failure: trends in case fatality in 66 547 patients hospitalized between 1986 and 1995. Circulation 102:1126–1131. [DOI] [PubMed] [Google Scholar]
- 9. Schaufelberger M, Swedberg K, Koster M, Rosen M, Rosengren A (2004) Decreasing one-year mortality and hospitalization rates for heart failure in Sweden; Data from the Swedish Hospital Discharge Registry 1988 to 2000. Eur Heart J 25:300–307. [DOI] [PubMed] [Google Scholar]
- 10. Stewart S, Jenkins A, Buchan S, McGuire A, Capewell S, et al. (2002) The current cost of heart failure to the National Health Service in the UK. Eur J Heart Fail 4:361–371. [DOI] [PubMed] [Google Scholar]
- 11. Ryden-Bergsten T, Andersson F (1999) The health care costs of heart failure in Sweden. J Intern Med 246:275–284. [DOI] [PubMed] [Google Scholar]
- 12. Araujo DV, Tavares LR, Verissimo R, Ferraz MB, Mesquita ET (2005) [Cost of heart failure in the Unified Health System]. Arq Bras Cardiol 84:422–427. [PubMed] [Google Scholar]
- 13. Stewart S (2005) Financial aspects of heart failure programs of care. Eur J Heart Fail 7:423–428. [DOI] [PubMed] [Google Scholar]
- 14. Stewart S, Wilkinson D, Hansen C, Vaghela V, Mvungi R, et al. (2008) Predominance of heart failure in the Heart of Soweto Study cohort: emerging challenges for urban African communities. Circulation 118:2360–2367. [DOI] [PubMed] [Google Scholar]
- 15. Sliwa K, Wilkinson D, Hansen C, Ntyintyane L, Tibazarwa K, et al. (2008) Spectrum of heart disease and risk factors in a black urban population in South Africa (the Heart of Soweto Study): a cohort study. Lancet 371:915–922. [DOI] [PubMed] [Google Scholar]
- 16. Ojji D, Stewart S, Ajayi S, Manmak M, Sliwa K (2013) A predominance of hypertensive heart failure in the Abuja Heart Study cohort of urban Nigerians: a prospective clinical registry of 1515 de novo cases. Eur J Heart Fail 15:835–842. [DOI] [PubMed] [Google Scholar]
- 17. Ojji DB, Alfa J, Ajayi SO, Mamven MH, Falase AO (2009) Pattern of heart failure in Abuja, Nigeria: an echocardiographic study. Cardiovasc J Afr 20:349–352. [PMC free article] [PubMed] [Google Scholar]
- 18. Laabes EP, Thacher TD, Okeahialam BN (2008) Risk factors for heart failure in adult Nigerians. Acta Cardiol 63:437–443. [DOI] [PubMed] [Google Scholar]
- 19. Ogah OS, Stewart S, Falase AO, Akinyemi JO, Adegbite GD, et al. (2014) Contemporary Profile of Acute Heart Failure in Southern Nigeria: Data From the Abeokuta Heart Failure Clinical Registry. JACC Heart Fail 2:250–259. [DOI] [PubMed] [Google Scholar]
- 20. Oyoo GO, Ogola EN (1999) Clinical and socio demographic aspects of congestive heart failure patients at Kenyatta National Hospital, Nairobi. East Afr Med J 76:23–27. [PubMed] [Google Scholar]
- 21. Rits IA (1964) Declaration of Helsinki. Recommendations Guidings Doctors in Clinical Research. World Med J 11:281. [PubMed] [Google Scholar]
- 22.Ogun State. Available: http://en.wikipedia.org/wiki/Ogun_State. Accessed 2014 August 10
- 23.Abeokuta. Available: http://en.wikipedia.org/wiki/Abeokuta. Accessed 2014 August 10
- 24.Soyibo A, Olaniyan O, Lawanson OA National health accounts: Structure, trends and sustainability of health expenditure in Nigeria. African Journal of Economic Policy 14.
- 25. Lawanson AO, Olaniyan O, Soyibo A (2012) National Health Accounts estimation: lessons from the Nigerian experience. Afr J Med Med Sci 41:357–364. [PubMed] [Google Scholar]
- 26.Atlas of African Health Statistics. Available: http://www.aho.afro.who.int/en/publication/63/atlas-african-health-statistics-2012-health-situation-analysis-african-region. Accessed 2014 August 10.
- 27.International Statistical Classification of Diseases and Related Health Problems 10th Revision. Available: http://www.who.int/classifications/icd/en/. Accessed 2014 August 10.
- 28. Falase B, Sanusi M, Majekodunmi A, Ajose I, Idowu A, et al. (2013) The cost of open heart surgery in Nigeria. Pan Afr Med J 14:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Johnson A, Falase B, Ajose I, Onabowale Y (2014) A Cross-sectional study of stand-alone Percutaneous Coronary Intervention in a Nigerian Cardiac Catheterization Laboratory. BMC Cardiovasc Disord 14:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Czech M, Opolski G, Zdrojewski T, Dubiel JS, Wizner B, et al. (2013) The costs of heart failure in Poland from the public payer's perspective. Polish programme assessing diagnostic procedures, treatment and costs in patients with heart failure in randomly selected outpatient clinics and hospitals at different levels of care: POLKARD. Kardiol Pol 71:224–232. [DOI] [PubMed] [Google Scholar]
- 31. Writing Group M, Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, et al. (2010) Heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation 121:e46–e215. [DOI] [PubMed] [Google Scholar]
- 32. Fagnani F, Buteau L, Virion JM, Briancon S, Zannad F (2001) [Management, cost and mortality of a cohort of patients with advanced heart failure (the EPICAL study)]. Therapie 56:5–10. [PubMed] [Google Scholar]
- 33. Whellan DJ, Greiner MA, Schulman KA, Curtis LH (2010) Costs of inpatient care among Medicare beneficiaries with heart failure, 2001 to 2004. Circ Cardiovasc Qual Outcomes 3:33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. McMurray J, Davie A (1996) The pharmacoeconomics of ACE inhibitors in chronic heart failure. Pharmacoeconomics 9:188–197. [DOI] [PubMed] [Google Scholar]
- 35. McMurray JJ, Hart W, Rhodes G (1993) An evaluation of the cost of heart failure to the National Health Service in the UK. Br J Med Econ 6:91–98. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Cost of procedures (In-patient).
(DOCX)
Cost of transport (In-patients).
(DOCX)
Cost of clinic visits (Out-patient).
(DOCX)
Cost of medications (Out-patient).
(DOCX)
Cost of transport (Out-patient).
(DOCX)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.