Abstract
Introduction:
Pathogenesis of kidney stones includes many factors, whereas uroliths, as a generic term for kidney stones, are of a different composition. In pathogenesis of calcium urolithiasis hypercalcemia/hypercalciuria takes a significant place. Hypercalcemia exists when the serum calcium is of increased values, along with measurement and calculation of physiologically active calcium, when there are differences in the Ph of the blood or albumin.
Goal:
the goal of this research is to determine the correlation of values of the serum (CaS) and ionized calcium (Ca++) in patients with the calcium nephrolithiasis, whom have been established not to have hyperparathyroidism and malign diseases.
Material and methods:
the research was prospective and implemented at the Clinical Center in Banja Luka, at the Urology Clinic, in the period between 1st April 2012 – 1st January 2013 and it included 120 patients with the calcium lithiasis of the upper part of the urinary tract, divided into three age categories. Diagnosis of the calcium lithiasis of the upper part of the urinary tract was established on the basis of the ultrasonography of the urinary tract as well as native urinary tract/intravenous urography and chemical analysis of the stone in patients with spontaneous stone emission or after some of the methods for active removal of the stone. Chemical laboratory analysis of the serum and ionized calcium was done for all the patients, with 3ml of blood being taken for establishing the aforementioned parameters (1-2 ml of the serum) in vacuumed test tubes or glass tubes of capillary blood. Increased parathormone values (PHT) and history of malignity were excluding factors.
Results:
out of the 120 patients observed, Cs(S) had the value in the reference interval with most of them, that is, in 110 patients (91.7%). Those, whose value was out of the interval, are of an older age (all above 40). Average value of this parameter amounted to 2.3017, with an average difference (the standard deviation) of 0.11391. Observing the value of Ca++, the value within the reference interval was found in 106 patients (88.3%). Out of the remaining 14 patients, only two simultaneously had the value of Ca(S) out of the permitted interval. The majority of this group consisted of older patients (a half of those whose values were outside the interval was over 60). Average value of Ca++ amounted to 1.22 mmol/L with an average difference of 0.06454. In the 2 aforementioned patients, who simultaneously had increased values of CaS and Ca++, the blood Ph was within the referential value limits, which suggests that, in line with the hyporcalcemia definition, only 2 patients with nephrolithiasis, in the total sample of 120 patients of our research sample, could have had a true hypercalcemia.
Conclusion:
the biggest number of patients with the calcium urolithiasis, who do not have hyperparathyroidism and history of malign diseases, do not have a real hypercalcemia.
Keywords: the upper part of the urinary tract, calcium urolithiasis, serum calcium, ionized calcium
1. INTRODUCTION
Urolithiasis presents morbidity, which significantly participates in the costs of national health systems throughout the world, having in mind that the patients have a high percentage of hospitalization with indirect costs related to the decrease of their work abilities and loss of work days (1). Urolithiasis incidence has been on the increase in the last three decades, both in adult population as well as in children. This fact suggests that the change of external factors take a significant place in the risk of occurrence of kidney stones, even though there are many indications that genetic components present a significant cause of occurrence of this pathological condition (2). Uroliths, as a generic term for kidney stones, are of different composition. Pathogenesis of the kidney stones includes many factors: age, gender, obesity, hypertension, hyperparathyroidism, gastrointestinal diseases, genetically caused urolithiasis, medicines associated and anatomic anomalies associated with the occurrence of uroliths, as well as different external factors, such as profession (occupation), physical activities, diets, geographical location of residence place (3-8). Generally, in pathogenesis of the calcium urolithiasis, hypercalcemia/hypercalciuria takes a significant place. As a consequence of hypercalcemia, what happens in the bones is generalized demineralization and subperiosteal bone resorption with the loss of cortex, whereas the kidney changes get manifested with the recidive occurrence of nephrolithiasis, nephrocalcinosis and damage of the kidney function. Hypercalciuria, i.e. increased excretion of calcium through urine is also frequent. Basically, there are three principle organs for maintaining of the calcium homeostasis: the kidneys, intestines and bones (9). Generally, the kidneys have a key role in the control of the calcium balance. Each day, about 10 g of calcium gets filtered through kidneys: about 1.5% of this quantity gets excreted into urine, whereas the rest gets reabsorbed. The stone kidneys occur when it comes to their crystallization in urine and formation of solid forms. According to the EAU, the basic laboratory analysis of the patients with renal/ureteral colic implies the application of urine analysis (urinary sediment/dipstick test), serum analysis of creatinine, uric acid, ionized calcium, sodium, potassium, blood cell count and C-reactive protein (CRP). Evaluation of high-risk stone formers also requires having a metabolic evaluation of 24 h urine samples of urinary excretion calcium, citrate, cystine, oxalate, urate (excretion), as well as additional serum analysis of ionograph and blood gas analysis. Hypercalcemia exists when the serum calcium values are increased, together with measuring and calculation of physiologically active calcium when there are differences in the Ph of blood or albumin (10). Measuring of the serum calcium with asymptomatic patients often leads to inaccurately-positive increased values caused by random errors or changes in the level of active calcium because of differences of the blood Ph or albumin serum (11). Even though calcium is a predominant crystalline constituent of kidney stones in 80% of cases, it is necessary to emphasize that the calcium nephrolithiasis occurs both in hypercalcemia/hypercalciuria patients and in normocalcemia/normokalciuria patients (12).
2. GOAL OF RESEARCH
The goal of this research is to determine the correlation of values of the serum and ionized calcium in patients with the calcium nephrolithiasis, who have been identified as not suffering from hyperparathyroidism and malign diseases.
3. MATERIAL AND METHODS
The research was prospective and implemented at the Clinical Center in Banja Luka, at the Urology Clinic, in the period from 1st January 2012 – 1st January 2013 and it has included 120 patients with the calcium lithiasis of the upper part of the urinary tract, which were divided into three age categories, with their age being 20-40, 40-60 and older than 60. Diagnosis of calcium lithiasis of the upper part of the urinary tract was set on the basis of ultrasonography of the urinary tract, as well as native urinary tract/intravenous urography and chemical analysis of stones in patients suffering from spontaneous emission of the stone or after some of the methods for an active stone removal. Ultrasound examinations were conducted using the sonograph LOGIQ 5 PRO, with a transabdominal proble of 3.5 MHz. Generally, untrasound examination provides detection of all the stones, regardless of their chemical composition. Pathognomonic sign of calcium urolithiasis on native scan of the urinary tract shows the presence of mineral shadow of calcium intensity. Intervenous urography has also, in addition to pathognomonic sign of calcium urolithiasis on the RTG scan, given insight into the functionality status of the kidney, as well as morphological overview of pielocaliceal system of the kidney, ureter and bladder, with the defining of whether there was an obstruction in the derivation of urine in the sense of anatomic or functional obstruction, which could have presented a cause behind the urolithiasis. Excluding factors were anatomic and functional disturbances of the urinary tract, the consequence of which is obstructive uropathy, hyperthyroidism and history of malignity. Laboratory analysis of the serum and ionized calcium was done for all the patients at the central laboratory of the Clinical Center. For determining the aforementioned parameters, 3 ml of blood (1-2 ml of serum) were taken in vacuumed test tubes or glass tubes of capillary blood and processed with equipment COBAS C 501 (CaS) and acidobasic device ABL 800 (Ca++). Normal values of the serum ionized calcium for adults, older than 18 years of age, at the aforementioned instruments amount to 1.15-1.29 mmol/L, while of the serum (unionized) calcium it is 2.2-2.65 mmol/L.
4. RESULTS
Demographically observed, the working sample included 120 patients, who were categorized in three age categories: 20-40, 40-60 and over 60. Each age group had 40 patients.
Average age amounted to 50.19 years, with a standard deviation of 15.60, while, on the other side, the sex structure was not complete balanced, as the sample included 52.5% of men and 47.5% of women.
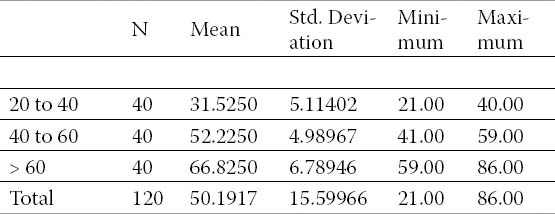
Basic descriptive measures, depending on the age category (average, minimum, maximum, difference), were given in Table 1.
Table 1.
Demographic characteristics of working sample by age categories.
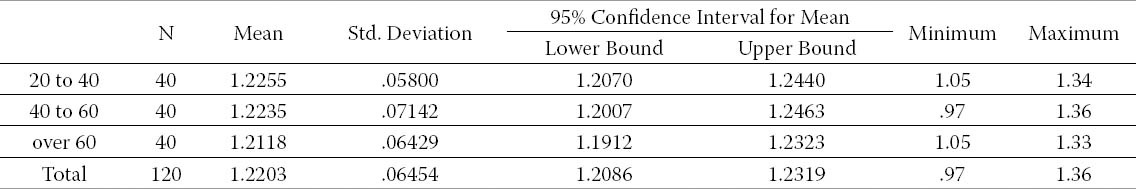
Values of the serum and ionized calcium in relation to the age category are shown in Tables 2 and 3.
Table 2.
Values of CaS by age groups
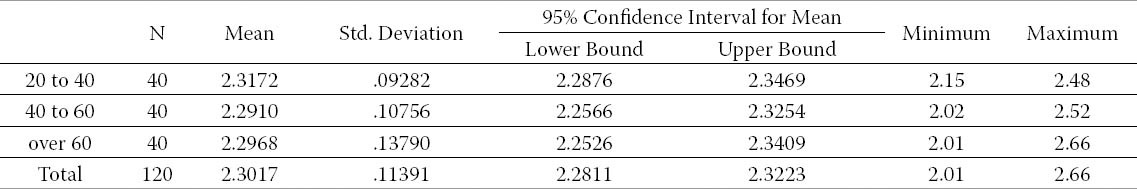
Table 3.
Value of Ca++ by age groups.
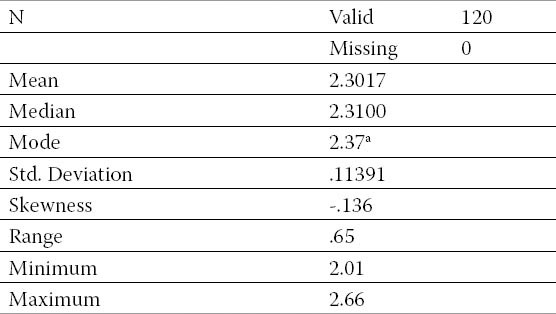
Out of the observed 120 patients, calcium – Ca(S) had the value within the expected interval in most of them, that is, in 110 patients (91.7%). Those, whose value was out of the referential interval, were of older age (all were over 40 years of age). Average value of this parameter amounted to 2.3017, with an average difference (standard deviation) of 0.11391. As there is a small percentual difference, we may accept an average data as representative. It should be pointed out that data have been distributed in a normal manner, which is confirmed by the asymmetry coefficient (Skewness = -0.113), but also the approximate value of the central tendency measure. The other descriptive measures, which are related to the serum calcium, are shown in Table 4.
Table 4.
Descriptive measures of CaS
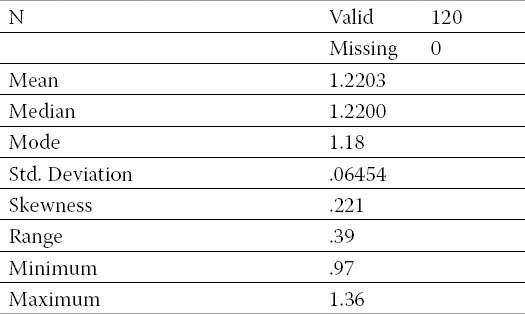
Observing the values of ionized calcium (Ca++), 106 patients (88.3%) had the values within the referential interval. Out of the remaining 14 patients, only two simultaneously had the value of CaS outside the permitted interval.
The majority of this group consists of older patients (a half of those whose value was outside the interval was over 60). Average value, together with all the other descriptive measures, was shown in Table 5. It may be seen that this is a normal distribution, as well as that the average is a representative measure on the basis of which conclusions can be made.
Table 5.
Descriptive measures Ca ++
5. DISCUSSION
Urolithiasis is a multifactoral disease, which occurs by an inter-reaction between the genetic inheritance and environmental exposure. In the pathogenesis of calcium urolithiasis, hypercalcemia/hypercalciuria take a significant place. Hypercalcemia with hypercalciuria cause the occurrence of calcium nephrolithiasis, by increasing the urinary saturation of calcium salts and by binding negatively charged inhibitors of stone formation (13,14). Between 35% and 65% of hypercalciuric stome formers and up to 70% of subjects with hypercalciuria have relatives with nephrolithiasis (15,16). Calcium stones are also associated with several monogenic mendelian traits, many of which affect ion channels and membrane transporters (16). Goodman et all concluded that stone formers have a relative risk of having abnormal calciemia and calciuria 9,18 times more than do nonstone formers (17).
Having in mind the previously stated facts, it is necessary to emphasize that, regardless to the calcium being a predominant constituent of kidney stones, the calcium nephrolithiasis occurs in both hypercalcemic/hypercalciuric patients as well as with normocalcemic/normocalciuric patients. Sakhaee K. and associates have come up with a conclusion that increased fracture risk may be evident in both hypercalciuric and normocalciuric kidney stone-forming subjects as low BDM is present in each population (18).
The results of our study have shown that, out of the observed 120 patients with calcium urolithiasis, calcium CaS was within referential values for most of them, that is, for 110 patients (91.7%). Those, whose value was out of the referential interval, are of older age (all being over 40). Average value of this parameter amounted to 2.3017, with an average difference (standard deviation) of 0.11391.
Hypercalcemia is defined with an increased values of the serum calcium, with measuring and calculation of phyisiologically active calcium when there are differences in the blood or albumin Ph. Nominal exact values of the serum ionized calcium for adults older than 19 may vary from laboratory to laboratory, while usage of the ABL 800 at the laboratory of our Clinical Center amounts to 1.15-1.29 mmol/L (10). It is known that metabolic acidosis reduces also reabsorption of calcium in the kidneys, causing hypercalciuria, which participates in the occurrence of kidney stones (19,20). Our research has shown that 106 patients (88.3%) had the values of ionized calcium, Ca++, within the referential interval. Average values of ionized calcium amounted to 1.22 mmol/L. Out of the remaining 14 (11.7%) patients, only two simultaneously had the value of CaS outside the permitted interval. The majority of this group consisted of older patients (a half of those whose value was outside the interval was over 60). As for the aforementioned 2 patients, who simultaneously had increased values of the serum and ionized calcium, the blood Ph was within the referential values, as well as the values of the serum albumin, which suggests that, by definition of hypercalcemia, only 2 patients with the calcium nephrolithiasis, in the total sample of 120 patients who underwent our research, could have had a true hypercalcemia. Reference data show that measuring of the serum calcium, which is used in the cases of hypertension, generally resulted in the epidemics of incidental hypercalcemia, without a confirmed calcium nephrolithiasis (9).
6. CONCLUSION
Having in mind the definition of urolithiasis, as a multifactoral disease on one side and the fact on the other side that calcium is the most frequent constituent of uroliths, the biggest number of patiens with the calcium urolithiasis do not suffer from hyperthyroidism and have a history of malign diseases, there is no real hypercalcemia, which indirectly suggests that external exposure factors take a significant place in the risk of occurrence of calcium kidney stones.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Pearle MS, Calhoun E, Curhan GC. Urolithiasis. In: Litwin MS, Saigal CS, editors. Urologic disease in America. Washington D.C: US Department of Health and Human Services, Public Health Service, National Institute of Health, National Institute of Diabetes and Digestive and Kidney Disease. NIH Publicationb. No. 07-5512. US Government Printing Office; 2007. pp. 282–319. [Google Scholar]
- 2.Massimo A. The genetic components of idiopathic nephrolithiasis. Pediatr Nephrol. 2011;26:337–346. doi: 10.1007/s00467-010-1562-6. [DOI] [PubMed] [Google Scholar]
- 3.Keoghane S, Walmsley B, Hodgson D. The natural history of untreated renal tract calculi. BJU Int. 2010;105(12):1627–1629. doi: 10.1111/j.1464-410X.2010.09389.x. [DOI] [PubMed] [Google Scholar]
- 4.Hesse AT, Tiselius HG, Siener R, Basel S, Karger AG, et al., editors. 3rd edn. 2009. Urinary stones, Diagnosis, Treatment and Prention of Recurrence. ISBN 978-3-8055-9149-2. [Google Scholar]
- 5.Basiri A, Shakhssalim N, Khoshdel AR, et al. Familial relations and recurrence pattern in nephrolithiasis: new words about old subjects. Urol J. 2010;7(2):81–86. [PubMed] [Google Scholar]
- 6.Goldfarb DS, Fischer ME, Keich Y, et al. A twin study of genetic and dietary influences on nephrolithiasis: a report from the Vietnam Era Twin (VET) Registry. Kidney Int. 2005;67(3):1053–1061. doi: 10.1111/j.1523-1755.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 7.Durrani O, Morrisroe S, Jackman S, et al. Analysis of stone disease in morbidly obese patients undergoing gastric bypass surgery. J Endourol. 2006;20(10):749–752. doi: 10.1089/end.2006.20.749. [DOI] [PubMed] [Google Scholar]
- 8.Asplin JR, Coe FL. Hyperoxaluria in kidney stone formers treated with modern bariatric surgery. J Urol. 2007;177(2):565–569. doi: 10.1016/j.juro.2006.09.033. [DOI] [PubMed] [Google Scholar]
- 9.Neher O. How should you evaluate elevated calcium in an asymptomatic patient? Clinical Inquires. 2008;57(4):267. [PubMed] [Google Scholar]
- 10.Amanzadeh J, Gitomer WL, Zerwekh JE, et al. Effect of high protein diet on stone-forming propensity and bone loss in rats. Kidney International. 2013;64:2142–2149. doi: 10.1046/j.1523-1755.2003.00309.x. [DOI] [PubMed] [Google Scholar]
- 11.Sharma B, Hitchcock K. Make sure it is true hypercalcemia. Clinical Ingquires. 2008;57(4):267–269. [Google Scholar]
- 12.Devuyst O, Pirson Y. Genetics of hypercalciuric stone forming disease. 2007;72:1065–1072. doi: 10.1038/sj.ki.5002441. [DOI] [PubMed] [Google Scholar]
- 13.Pak CYC, Holt K. Nucleation and growth of brushite and calcium oxalate in urine of stone formers. Metabolism. 1976;25:665–673. doi: 10.1016/0026-0495(76)90064-0. [DOI] [PubMed] [Google Scholar]
- 14.Zerwekh JE, Hwang TIS, Pundexter J, et al. Modulation by calcium of inhibitor activity of naturally occurring urinary inhibitors. Kidney Int. 1988;33:1005–1008. doi: 10.1038/ki.1988.100. [DOI] [PubMed] [Google Scholar]
- 15.Polito C, Manna A, Nappi B, Villiani J, Di Toro R. Idiopathic hypercalciuria and hyperuricosuria: family prevalence of nephrolithiasis. 2000;14:1102–1104. doi: 10.1007/s004670000323. [DOI] [PubMed] [Google Scholar]
- 16.Stechman MJ, Loh NY, Thakker RV. Genetics of hypercalciuric nephrolithiasis: renal stone disease. Ann NY Acad Sci. 2007;1116:461–484. doi: 10.1196/annals.1402.030. [DOI] [PubMed] [Google Scholar]
- 17.Goodman HO, Holmes RP, Assimov DG. Genetic factors in calcium oxalate stone disease. J Urol. 1995;153:301–307. doi: 10.1097/00005392-199502000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Sakhae K, Maalouf NM, Kumar R, Pasch A, Moe OW. Nephro-lithiasis-associated bone disease: pathogenesis and treatment options. Kidney Int. 2011;79:393–403. doi: 10.1038/ki.2010.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hutton E. Evaluation and management of hypercalcemia. JAAPA. 2005;18(6):30–35. doi: 10.1097/01720610-200506000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Moe OW. Kidney stones: pathophisiology and medical treatment. Lancet. 2006;367:333–344. doi: 10.1016/S0140-6736(06)68071-9. [DOI] [PubMed] [Google Scholar]


