Abstract
Introduction:
Heart murmurs can be functional (innocent) and pathological (organic). Although it is not considered a major sign of heart disease, it may be a sign of a serious heart defect. In most cases the noise is initiation for cardiac treatment. Is it possible to differentiate on the basis of auscultation innocent from pathological heart murmur? In this article we present the results of ultrasonography of newborns with positive auscultation finding of the heart in the neonatal and early infancy period.
Goal:
To determine the role of murmurs in the heart detected by routine clinical examination in the neonatal period and early infancy, and to establish the legitimacy of cardiology consultation and ultrasound of the heart.
Methods:
A retrospective review of medical records in the period from January 1 to December 31, 2011 at the Maternity ward of Cantonal Hospital in Bihac 1899 children was born. In 32 neonates was registered a heart murmur, in the period from birth up to 6 weeks of life. All children with positive auscultation finding of the heart were examined echocardiography by ultrasound ALOCA 2000, multifrequency probe from 3.5 to 5 MHz, and used M-mode, 2-D, continuous, pulsed and color Doppler.
Results:
Of the 32 examined children regular echocardiographic findings had two children (6.25%), aberrant bunch of left ventricle 11 (34.37%), patent foramen ovale 5 (15.62%), atrial septal defect 3 children (9.37%), ventricular septal defect 8 children (25%), cyanogen anomaly 2 children (6.25%), stenosis of the pulmonary artery 1 child (3.12%). We see that 14 children (43.75%) had a structural abnormality of the heart that requires further treatment and monitoring.
Conclusion:
Echocardiography is necessary to set up or refute the diagnosis of structural heart defect in children with positive auscultation finding in the neonatal period.
Keywords: newborn, echocardiographic review, heart murmur
1. INTRODUCTION
Congenital heart anomalies (CHA) are the most common congenital anomalies and emerge with a fairly constant incidence from 0.8 to 1% per 1000 live births (1,2). Given that the CHA are leading cause of death among congenital anomalies, their early detection would greatly enhance the therapeutic procedures, and therefore the ultimate outcome of the disease (3). Previous methods of CHA screening (ultrasonography in the second trimester of pregnancy, postnatal clinical examination) had a low rate of CHA detection, and a significant number of children have been released from the maternity hospital with unrecognized CHA (4,5,6). This information is even more important if it is seen in the light of today’s trend of earlier discharge from the maternity hospital (before 24h), when most of the CHA is not manifested.
According to data from previous studies, the routine clinical examination fails to diagnose more than half of the children with the CHA (5). For diagnostics of CHA, in addition to clinical examination, so far have been used electrocardiography and chest radiogram. Although electrocardiography and radiogram does not contribute much to diagnosing heart murmur (7,8,9). Ultrasonography is a unique approach in the diagnosis of cardiac anomalies, but is considered to be limiting to be used as a screening method for the detection of CHA due to the cost of that service.
Although wrongly considered the leading sign of heart disease, a heart murmur is still in the highest percentage a reason for cardiac treatment (10). Heart murmurs can be innocent (physiological) and organic (pathological). The physiological bases of these are benign causes that do not endanger the child. In organic noises in the background there is a heart defect.
Auscultation is performed at certain points (ictus, mesocardia, second intercostal space, right and left). Character of the murmur is objectively assessed based on auscultation. The examiner assesses the intensity of the murmur. For the evaluation of the intensity of the murmur is commonly used Levine Harvey scale. By the same scale as the first stage murmur are evaluated these noise, audible only in apnea. The murmur of the second degree is the audible also in the other phases of the respiratory cycle. The third degree will be assessed to a moderately loud murmur, with or without a thrill. The fourth level of murmur indicates a loud murmur followed by a thrill. The sound of the fifth degree is a strong and audible over the entire precordium. The sound of the sixth degree is audible even at a distance of 1 cm from the chest wall (11,12). After determining existence of murmur, evaluated is the punctum maximum (strongest place of hearing) and the existence of propagation in the environment.
Whether based on auscultation can determine whether it is case of innocent or pathological murmur? There are characteristics of the murmur on the basis of which can be roughly differentiated innocent from pathological. For example, innocent murmur intensity changes with the phases of the respiratory cycle or with change of the body posture. It is short, without accompanying phenomena, confined to systole. Audible on a small area without propagation.
Neonates are the most sensitive categories of children and detection of CHA in this age is of great importance. Heart murmurs in these children may mean a serious heart defect, even some the potentially life threatening (13,14). It may also be a result of the transitional circulation of the newborn or the result of some benign structures.
2. GOAL
To determine the significance of a heart murmur detected by routine clinical examination in the neonatal and early infancy period.
Establish justification for cardiology consultation and ultrasound of the heart in infants with a positive auscultation finding the heart.
3. METHODOLOGY
From January 1 to December 31, 2011 on the maternity ward of Cantonal Hospital Bihac was born 1899 babies. Retrospective analysis of medical records, determined by the positive auscultatory findings at the heart of a child in 32 cases, with or without other characteristics that contribute to heart disease. The study included children who were moved to the department of neonatology with suspicion of potential life threatening heart defect, as well as children wellbeing, which, after consultation cardiac examination the patients was discharged, with subsequent ultrasound of the heart over a period of 6 weeks after birth. Children were examined by ultrasound machine, ALOKA 2000, with multifrequency probe from 3.5 to 5 MHz. We used M-mode, 2-D, continuous and pulsed Doppler. The results were statistically analyzed and graphically displayed.
4. RESULTS
During the study period in Bihac Cantonal Hospital was born 1899 children. Of these, 32 children had positive auscultatory findings of the heart, with or without other supporting features of a heart defect. These children are subjected to cardiac treatment and echocardiography. From those, 14 children (43.75%) had a structural defect of the heart, and 18 children (56.25%) had normal or non-significant findings (Figure 1).
Figure 1.

Results of the ultrasonography
From the total number of live births during the tested year (1899 children), murmurs was registered in 32 neonates. The percentage is 1.68% of the children. In children with positive auscultation finding cardiac evaluation is required. Two children had normal findings (6.25%). Five neonates had a patent foramen ovale (15, 62%), 11 children (34.37%) as a cause of murmurs had aberrant horde in the pulp chamber in left ventricle, 8 neonates had a defect of ventricle compartments (25%) of which are in two children was a perimembranous defect, while in other children it was a muscular ventricular septal defect. Three children had a defect of paraventricular parts (9.37%). One child had stenosis of pulmonary artery (3.12%). Two children (6.25%) in the background had a serious heart defect (cyanogen anomaly) (Figure 2).
Figure 2.
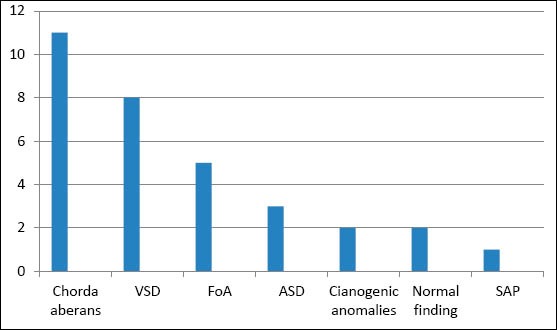
Results of the ultrasonography
5. DISCUSSION
Of the total number of live births in the studied period, in 32 cases was registered a heart murmur or 1.68%. Approximately 1% of newborn children have a heart murmur and the presence of a heart defect as the cause of it, exist is a wide range of 30 to 85% of cases (15,16). In this study it is a somewhat larger proportion of children with audible murmurs. Although other authors state variations ranging from 0.6 to 1.8%, all depending on the number of small muscular defects of descending barriers involved in the study, as well as other trivial lesions (17). In addition, among cardiologists are not harmonized criteria for differentiation of small atrial septal defect (ASD) from the Foramen ovale Apertum (FoA) (18). In this study, the defect of periventricular partition is designated the same as ASD measured 6 mm and more. ASD is diagnosed in 3 patients (9.37%). FoA was diagnosed in 5 patients (15.62%). From the results we can see that compared to the total number of required consultations, with 14 children (43.75%) basically existed structural defect of the heart. For some of them it was very likely, on the basis of clinical examination that it is a cardiac anomaly. However, the final confirmation is mandatory echocardiography, which is in most cases the last in establishing the diagnosis of cardiac anomalies.
Two children had cyanogen, potentially life threatening anomaly. Such anomalies are not necessarily manifested by the heart murmurs as the first manifestation of heart disease. On the contrary, there is a great danger of releasing such a child from a maternity hospital with unrecognized heart disorder, because the symptoms of some serious heart defects are manifested only after 48h or more (19). Between 10-30% of child deaths in the first year of life as a consequence of unrecognized CHA (20,21). Making a diagnosis in such child only after discharge from the maternity hospital has often resulted in poor general condition of the child and poor preoperative condition that is closely linked with poorer postoperative outcome and a number of complications. Eight patients had septal defect in ventricular partitions. Two children had perimembranous VSD, while in six children was a muscular VSD. Reference to the normal incidence of VSD’s 30-35% compared to the total number of CHA (22), we can see a larger number of VSD in our study. Of the 14 children with structural heart defect, 8 of them have VSD. In addition, eight children with VSD infection, with 6 children (75%) registered a muscular VSD, although usually in 80% of cases are perimembranous VSD. For muscular defects is known that more than half of small defects prone to spontaneous closure (23).
In our study we included all septal defects that are diagnosed in the period from birth to the age of 6 weeks of life. This may explain the slightly higher incidence of CHA during the test period, and therefore a greater number of muscular VSD. Prognosis and significance of early diagnosis in children with VSD infection depend on the location, size of the defect and the degree of LD shunt at the level of the defect. Although usually not a life threatening anomaly in the first days of life, it is certainly better to diagnose these types of cardiac anomalies have in the past. As for adequate monitoring of the child and the prevention of septic endocarditis and the optimal time to plan a possible surgical treatment. It is feasible for some anomalies in later life, but it was later followed by a higher rate of mortality and postoperative complications. In addition, we should bear in mind the potential risk of developing pulmonary hypertension, when correction surgery is no longer feasible. Of the 56.25% of respondents who did not have a structural defect of the heart, ultrasound was normal in two children (6.25%). 5 children had a patent foramen ovale Apertum (15.62%). 11 children had registered aberrant horde in the pulp chamber of the left ventricle (34.37%). It is a fibromuscular structures that extend through the left ventricular cavity, with no connections with the heart valves.
Long been regarded as normal structures, although today there is a great interest cardiologist for them, because of their potential association with innocent murmurs (24). He even believes that they may have to do with ventricular arrhythmias. According to some authors, it is possible, because except those containing fibrous and muscular and the conduction tissue. In our study, there are a significant number of children with aberrant and positive auscultation finding of the heart. One study showed an extreme variability of the presence of these structures in echocardiography studies (0.2 to 71%). The wide range is interpreted partly by varying degrees of examiners skill and partly by population based differences (25).
6. CONCLUSION
A significant number of children with audible murmurs in the neonatal period have a structural defect of the heart. Based on the auscultative characteristics of the murmurs cannot be with certainty differentiate innocent from organic heart murmur. For the diagnosis or exclusion of congenital heart anomalies ultrasound of the heart is essential.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Botto LD, Correa A, Erricson JD. Racial and temporal violations in the prevalence of heart defects. Pediatrics. 2001;107(3):E32. doi: 10.1542/peds.107.3.e32. Available from: http://pediatrics.aappublications.org/content/107/3/e32.full.Html . [DOI] [PubMed] [Google Scholar]
- 2.Talner CN. Report of the New England Regional Infant Cardiace Program by Donald C Fyler, MD. Pediatrics. 1980;65:375–461. Pediatrics 1998; 102(1 pt 2): 258-259. [PubMed] [Google Scholar]
- 3.Brown KL, Ridout DA, Hoskote A, Verhulst L, Ricci M, Bull C. Deleyed diagnosis of congenital heart disease worsens preoperative condition and outcome of surgery in neonates. Heart. 2006;92:298–302. doi: 10.1136/hrt.2005.078097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abu-Harb M, Wyllie J, Hey E, Richmond S, Wren C. Presentation of obstructive left heart malformations in infancy. Arch Dis Child. 1994;71:F179–F183. doi: 10.1136/fn.71.3.f179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wren C, Richmond S, Donaldson L. Presentation of congenital heart disease in infancy: implications for routine examination. Arch Dis Child Fetal Neonatal Ed. 1999;80:F49–F53. doi: 10.1136/fn.80.1.f49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bull C for the British Paediatric Cardiac Association. Current and potential impact of fetal diagnosis on prevalence and spectrum of serious congenital heart disease at term in the UK. Lancet. 1999;354:1242–1247. doi: 10.1016/s0140-6736(99)01167-8. [DOI] [PubMed] [Google Scholar]
- 7.Danford DA. Effective use of the consultant, laboratory testing, and echocardiography for the pediatric patient with heart murmur. Pediatr Ann. 2000;29(8):482–488. doi: 10.3928/0090-4481-20000801-07. [DOI] [PubMed] [Google Scholar]
- 8.Poddar B, Basu S. Approach to a child with a heart murmur. Indian J Pediatr. 2004;71(1):63–66. doi: 10.1007/BF02725659. [DOI] [PubMed] [Google Scholar]
- 9.Yi MS, Kimball TR, Tsevat J, Mrus JM, Kotagal UR. Evaluation of heart murmurs in children: cost-effectiveness and practical implications. J Pediatr. 2002;141(4):504–511. doi: 10.1067/mpd.2002.127502. [DOI] [PubMed] [Google Scholar]
- 10.Pelech AN. Evaluation of the pediatric patient with a cardiac murmur. Pediatr Clin North Am. 1999;46(2):167–188. doi: 10.1016/s0031-3955(05)70111-5. [DOI] [PubMed] [Google Scholar]
- 11.Pelech AN. The physiology of cardiac auscultation. Pediatr Clin North Am. 2004;51(6):1515–1535. doi: 10.1016/j.pcl.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Uner A, Doğan M, Bay A, Cakin C, Kaya A, Sal E. The ratio of congenital heart disease and innocent murmur in children in Van city, the Eastern Turkey. Anadolu Kardiyol Derg. 2009;9(1):29–34. [PubMed] [Google Scholar]
- 13.Ainsworth S, Wyllie JP, Wren C. Prevalence and clinical significance of cardiac murmurs in neonates. Arch Dis Child Fetal Neonatal Ed. 1999;80(1):F43–F45. doi: 10.1136/fn.80.1.f43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azhar AS, Habib HS. Accuracy of the initial evaluation of heart murmurs in neonates: do we need an echocardiogram? Pediatr Cardiol. 2006;27(2):234–237. doi: 10.1007/s00246-005-1122-1. [DOI] [PubMed] [Google Scholar]
- 15.Bansal M, Jain H. Cardiac murmur in neonates. Indian Pediatr. 2005;42(4):397–398. [PubMed] [Google Scholar]
- 16.Rein AJ, Omokhodion SI, Nir A. Significance of a cardiac murmur as the sole clinical sign in the newborn. Clin Pediatr (Phila) 2000;39(9):511–520. doi: 10.1177/000992280003900902. [DOI] [PubMed] [Google Scholar]
- 17.Wren C, Richmond S, Donaldson L. Temporal variability in birth prevalence of cardiovascular malformations. Heart. 2000;83:414–419. doi: 10.1136/heart.83.4.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Laas E, Lelong N, Thieulin AC, Houyel L, Bonnet D, Yves Ancel P, Kayem G, Goffinet F, Khoshnood B. Preterme Birth and Congenital Heart Defects-A population based Study. Pediatrics. 2012 doi: 10.1542/peds.2011-3279. originaly published online September 3 2012. [DOI] [PubMed] [Google Scholar]
- 19.Kuehl KS, Loffredo CA, Ferencz C. Failure to diagnostic congenital heart defects in infancy. Pediatrics. 1999;103:743–747. doi: 10.1542/peds.103.4.743. [DOI] [PubMed] [Google Scholar]
- 20.Abu-Harb M, Hey E, Wren C. Death in infancy from unrecognized congenital heart disease. Arch Dis Child. 1994;71:3–7. doi: 10.1136/adc.71.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leonard H, Derrick G, O’Sullivan J, Wren C. Natural and unnatural history of pulmonary atresia. Heart. 2000;84:499–503. doi: 10.1136/heart.84.5.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Samanek M, Yoriskova M. Congenital heart disease among 815.569 children born between 1980 and 1990 and their 15-year survival: a prospective Bohemia survival study. Pediatr Cardiol. 1999;20(6):411–417. doi: 10.1007/s002469900502. [DOI] [PubMed] [Google Scholar]
- 23.Hiraishi S, Agata Y, Nowatari M, Oguchi K, Misawa H, Hirota H, et al. Incidence and natural course of trabecular ventricular septal defect: two-dimensional echocardiography and color Doppler flow imaging study. J Pediatr. 1992;120(3):409–415. doi: 10.1016/s0022-3476(05)80906-0. [DOI] [PubMed] [Google Scholar]
- 24.Saji Philip, Kottureth Mammen Cherion, Mei-Hwan Wu, Hung-Chi Lue. Left Ventricular False Tendons: Echocardiographic, Morphologic and Histopathologic Studies and Review of the Literature. Pediatrics and Neonatology. 2011;52:279–286. doi: 10.1016/j.pedneo.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 25.Cocchieri M, Bardelli G. False chordae tendineae. Minerva Cardioangiol. 1992;40:353–358. [PubMed] [Google Scholar]


