Abstract
Objectives Nasal endoscopic approaches to the sphenoid sinus are challenging. Variations in septation, shape, and dimensions have a critical impact on surgical planning of the skull base. Previous anatomical studies have small numbers or a limited description of this complex structure. The present study is a radiographic analysis of the septation and dimensions of the sphenoid sinus.
Design and Methods High-resolution surgical-guidance computed tomography images of the sinuses from 90 patients at a tertiary care medical center between 2002 and 2007 were studied. Multiple anatomical measurements from axial and sagittal images were obtained and analyzed with imaging and statistical software.
Results Of the 90 patients studied, 9% had presellar, 37% sellar, and 54% postsellar pneumatization. In 34%, the posterior extent of the intersinus septum involved the bony covering of the carotid artery. The average presellar width of the sinus was 1.3 cm, the average midline presellar depth was 1.4 cm, and the average infrasellar midline depth was 2.6 cm.
Conclusions Approaching the skull base through the sphenoid sinus requires a tailored process based on anatomy. Septal involvement of the carotid artery occurs frequently. Pneumatization patterns are potentially disorienting, and awareness of the sinus's posterior and lateral extensions is critical.
Keywords: endoscopic surgery, skull base, sphenoid
Introduction
The sphenoid bone is of central importance to skull base surgery. It allows the endoscopic surgeon to safely approach the sella turcica, optic nerve, planum sphenoidale, tuberculum, and the lateral sellar orbital junction for various skull base lesions and cerebrospinal fluid leaks. As compared with rhinosinusitis, which requires a widefield sphenoidotomy with little intervention of the intersinus septum and skull base, neuroendoscopy often requires the removal of bone within the sphenoid sinus to access the skull base.
The sphenoid sinus is present only in primates and develops postnatally, reaching its adult size usually by age 12 in humans.1 The extent of pneumatization is highly variable and potentially jeopardizing to surrounding structures including the optic, vidian, maxillary, oculomotor, trochlear, and abducent nerves, the cavernous sinuses, and the internal carotid arteries.2 3 4 5 Furthermore, injury to the lateral, posterior, or superior walls of the sphenoid sinus could lead to inadvertent cerebrospinal fluid (CSF) leak.6 Although attempts have been made to describe the pneumatization patterns of the sphenoid sinus, little has been done to examine the variability of the complex intersinus septum.7
The purpose of this study was to further characterize the septation pattern of the sphenoid sinus in a high-resolution computed tomography (CT) database, and review and add to the literature in describing the anatomy of the sphenoid sinus. Sinus dimensions and intersinus septum variability were classified. The extent of pneumatization in relation to the sella was categorized. A preoperative review of the sphenoid anatomy should allow for safer endoscopic management of skull base pathology.
Materials and Methods
Deidentified high-resolution surgical-guidance CT images of the sinuses and skull base were obtained from a single tertiary care medical center. Approval for the study was received with a waiver from the University of Cincinnati's Internal Review Board. Images were analyzed and measurements performed using OsiriX software (Geneva, Switzerland). Axial and sagittal images were obtained and analyzed from 98 adult patients between 2002 and 2007 undergoing neuronavigation imaging for various pathologies. Various pathologies included mastoid and petrous tumors and inflammatory disease, isolated maxillary and frontal sinus inflammatory disease, and imaging for the detection of CSF rhinorrhea. Of the 98 patients, 8 were excluded for disease or tumors involving the sphenoid sinus that may have altered normal anatomical landmarks. Axial and midsagittal images were evaluated to measure the width and depth of the sella at defined anatomical points.
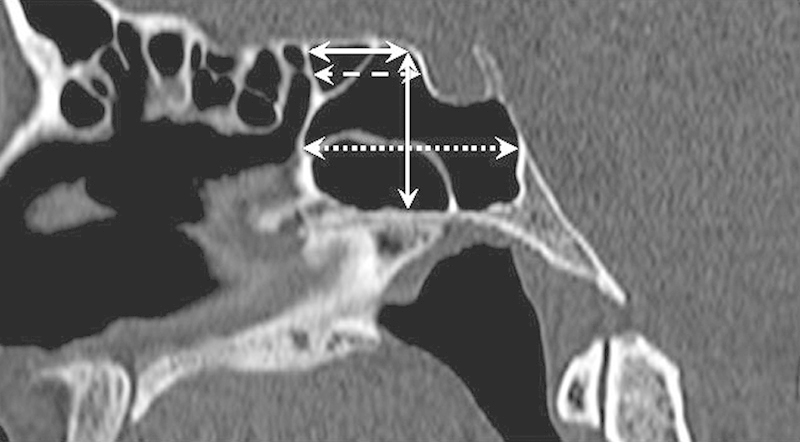
A total of six parameters were measured: two in the axial plane and four in the sagittal plane. Axial plane measurements, shown in Figs. 1 and 2, were the presellar width of the sphenoid sinus and the maximum width of the sphenoid sinus. Sagittal plane measurements, demonstrated in Fig. 3, were (1) height of the sinus, measured from the superior extent of the sellar face to the floor of the sinus; (2) suprasellar depth at the most superior extent of the sinus; (3) presellar depth at the vertical midpoint of the anterior face of the sella turcica; and (4) maximum infrasellar depth to the most posterior extent of the sphenoid sinus. Depth was measured parallel to the planum sphenoidale, and height was measured perpendicularly.
Fig. 1.

Measurement of presellar width (arrows). Sellar termination of intersinus septum is depicted.
Fig. 2.

Measurement of maximum width (arrows).
Fig. 3.
Measurements of the suprasellar (solid line), presellar (dashed line), and infrasellar depths (dotted line). Presellar height was also measured in the midsagittal plane (solid line).
The pattern of septation was determined from axial images. Septation was described as absent, single, double, and/or diverging. An example of a diverging intersinus septum is shown in Fig. 4. Posterior termination of the septum was described as sellar, involving the bony covering of the carotid, or lateral (anterior to the bony covering of the carotid). Right or left deviation of the septum was noted when present.
Fig. 4.

Example of diverging intersinus septum (arrows).
The extent of pneumatization posteriorly was determined from sagittal images. Pneumatization was described as presellar if there was no pneumatization past the anterior margin of the sella, sellar if the pneumatization terminated directly inferior to the sella, and postsellar if the pneumatization extended beyond a vertical line through the posterior margin of the sella, as previously described by Hamid et al.8 A postsellar example is shown in Fig. 3. Pneumatization of the dorsum sellae, shown in Fig. 5, was noted when present.
Fig. 5.
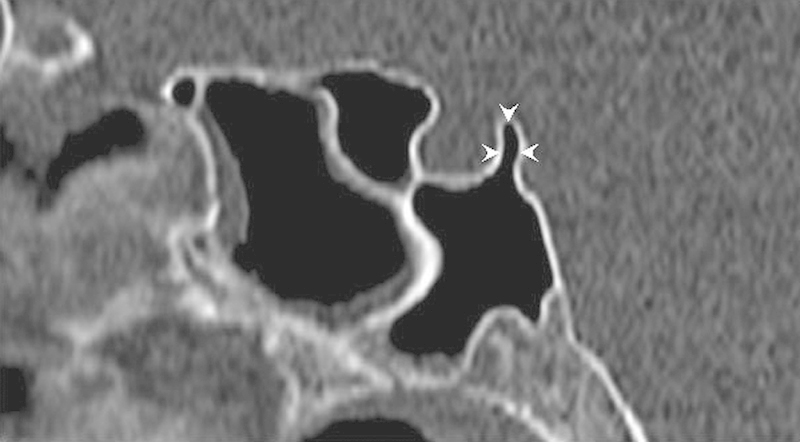
Example of postsellar pneumatization of the dorsum sellae (arrowheads).
Average distances and standard deviations were calculated using Excel software (Microsoft Corp., Redmond, Washington, United States).
Results
Table 1 shows the results of the measurements. The immediate presellar width of the sphenoid sinus was 1.3 cm (0.4–2.5 cm), with a maximum width of 3.5 cm (1.9–7 cm). The height was 2.3 cm (1.2–3.6 cm). The suprasellar depth was 1.3 cm (0.4–2.8 cm), the presellar depth was 1.4 cm (0.4–2.6 cm), and the infrasellar depth was 2.6 cm (0.6–4 cm).
Table 1. Average, standard deviation, and range for measured parameters.
| Parameter | Average, cm | Standard deviation | Minimum, cm | Maximum, cm |
|---|---|---|---|---|
| Presellar width | 1.3 | 0.34 | 0.4 | 2.5 |
| Maximum width | 3.5 | 0.98 | 1.9 | 7 |
| Presellar height | 2.3 | 0.45 | 1.2 | 3.6 |
| Suprasellar depth | 1.3 | 0.47 | 0.4 | 2.8 |
| Presellar depth | 1.4 | 0.4 | 0.4 | 2.6 |
| Infrasellar depth | 2.6 | 0.71 | 0.6 | 4 |
Septation patterns are listed in Tables 2 and 3. Of the 90 patients studied, in 4 the septum was absent (4%), in 75 one septum was present (83%), in 3 there were two septa (3%), and in 8 the septum diverged posteriorly (9%). Of these, in 8 the septum terminated left laterally (9%), and in 14 it terminated right laterally (16%). In 20, the septum terminated on the bony covering of the left internal carotid artery (22%), and in 11 it terminated on the bony covering of the right internal carotid artery (12%). In 43 patients it terminated exclusively on the sella turcica (48%).
Table 2. Presence of septa.
| Type of septa | No. (%) of studies |
|---|---|
| Absent | 4 (4) |
| Single | 75 (83) |
| Double | 3 (3) |
| Diverging | 8 (9) |
Table 3. Posterior termination of septuma .
| Termination | Left (%) | Right (%) | Total (%) |
|---|---|---|---|
| Lateral | 8 (9) | 14 (16) | 22 (25) |
| Carotid | 20 (22) | 11 (12) | 31 (34) |
| Sellar | 43 (48) |
Percentages reflect a denominator of total number of patients, and because total septa exceed the number of studies, the total percentage exceeds 100%.
Conchal pneumatization was not observed in the data population. Presellar pneumatization was found in 8 of the patients (9%), sellar pneumatization was found in 33 (37%), and postsellar pneumatization was found in 49 (54%). Pneumatization of the dorsum sellae was noted in 7 patients (8%).
Discussion
The anatomy of the sphenoid sinus is highly variable. Significant variability exists regarding the dimensions of the sphenoid sinus, attachment of the intersinus septum, number of septa, and pneumatization of the sphenoid bone. This variability has a direct impact on surgical planning for endoscopic skull base cases.
Various studies measuring the dimensions of the sphenoid sinus have previously been performed. Table 4 summarizes the data in comparison with the present study. Elwany and colleagues used plain radiographs of 100 living patients and 100 dried skulls, in addition to 50 cadaveric dissections, to measure the widths and depths of the sinus.9 Zada and coworkers used magnetic resonance imaging (MRI) studies from 100 healthy adults.10 Mutlu and colleagues used high-resolution CT images of the temporal bone from 69 patients.11 The present study has the dual benefit of a large number of patients and the precision of high-resolution CT images for obtaining measurements. In spite of relying on plain radiographs and MRIs, which are not ideal for distinguishing the mucosal/bony boundary, the measurements obtained in the studies by Elwany et al and Zada et al show remarkable similarity to the Mutlu et al and the present study. We sought to add to the literature by providing a complete collection of the primary dimensions of the sphenoid sinus.
Table 4. Comparison of measurements in previous studies.
| Study | Presellar width, cm | Maximum width, cm | Presellar depth, cm | Infrasellar depth, cm |
|---|---|---|---|---|
| Elwany et al9
(n = 250) |
1.2 | – | 1.6 | 3.1 |
| Mutlu et al11
(n = 69) |
– | 3.177 | – | 2.761 |
| Zada et al10
(n = 100) |
1.27 | 3.01 | – | – |
| Present study (n = 90) |
1.3 | 3.5 | 1.4 | 2.6 |
In the present study, the average presellar width of 1.3 cm was nearly identical to the suprasellar depth of 1.3 cm and the presellar depth of 1.4 cm. The variability of the presellar width, interpreted by standard deviation, was found to be slightly less than that of the suprasellar and presellar depths (0.34 cm versus 0.47 cm and 0.4 cm, respectively). The maximum width of the sinus, almost without exception, occurs inferior to the plane through the floor of the sella turcica. Of note, the width of the sellar face is approximately the same distance that the face itself is from the ostia of the sinus.
Septation of the sphenoid sinus also influences surgical planning. Kinnman found that of 80 acromegalic patients, 41.9% had a midline septum, 35.5% had a rightward deviation, and 22.4% had a leftward deviation.12 Of the 80 patients, the septum could not be identified in 4. The study was limited by its reliance on plain radiographs, which provide less detail than CT images; nor did not consider anatomical changes possible from growth hormone secretion in acromegalic patients. Hamid and coworkers later found that in 296 patients with pituitary adenomas, 10.8% had no septum, 71.6% had a single septum, 10.8% had an accessory septum, and 8.7% had multiple septa.8 Similarly, Ramakrishnan and colleagues, in a CT-based study of 106 patients with pituitary adenomas, found 85.8% of patients to have a single septum and 14.2% to have two or more septa.13 As compared with the present data, these studies relied on patients with pituitary pathology, allowing tumor expansion to potentially confound the data. Furthermore, although the number of septa is important, neither study analyzed the anatomical site of attachment of the septa, which gives more clinically relevant information for surgical planning in skull base surgery.
The present study was based on patients without evidence of sphenoid rhinosinusitis or pituitary pathology, and additionally it described the percentage of septa that involve critical surrounding structures of the sinus. Although images were selected without sphenoid, sellar, or parasellar pathology, we cannot discount the possibility that inflammatory disease of the maxillary, frontal, and ethmoid sinus or of the petrous and mastoid air spaces influenced the anatomy of the sphenoid sinus, influencing the measurements and observations in the current study population. Although we found the septum predominantly terminated posteriorly onto the sellar face (48%), a significant number of individuals had septa that involved the bony covering of the internal carotid artery (34%) or the lateral walls of the sinus anterior to the carotids (25%). Furthermore, the removal of a single septum may not be sufficient. In a significant number of individuals the septum bifurcated posteriorly (9%), and in others two distinct septa were present (3%). Awareness of this variability is important for preoperative planning to decrease the likelihood of intraoperative morbidity and increase surgical exposure when necessary.
Hamberger and coworkers divided the pneumatization of the sphenoid sinus into conchal, presellar, and sellar.14 Using this classification, Kinnman, in 80 sphenoid sinuses studied, found that 11.2% were presellar and 88.8% had a sellar configuration.12 As previously mentioned, the study was limited by relying on plain radiographs in acromegalic patients. Elwany and colleagues applied the same classification Kinnman used, although they referred to “postsellar” instead of the Hamberger “sellar.” They found 29.2% to have a presellar and 70.8% to have postsellar pneumatization.9 Although the study provided greater numbers, the resolution available with CT imaging should allow for more precise measurements.
Hamid and coworkers, in the previously mentioned cross-sectional study of 296 patients receiving surgical intervention for pituitary adenomas, divided the Hamberger classification of “sellar” into two categories: “sellar” and “postsellar.”8 The division between sellar and postsellar was a vertical line through the posterior margin of the sella. Using this criteria, 2% were conchal, 21% were presellar, 54.7% had a sellar pattern of pneumatization, and 22.3% had a postsellar pattern. Again, this study was limited by patients known to have pituitary pathology.
In our study using the Hamid classification, 9% were presellar, 37% were sellar, and 54% had postsellar pneumatization. For postsellar pneumatization, the extent can be such that the clivus is vulnerably thin. Care must be taken to avoid unintentional exploration of the basilar plexus. Pneumatization may also be pervasive to the extent that the dorsum sellae is involved. Hamid and coworkers found this in 13.5% of individuals; we found this in 8%.8 Although the present study did not reveal any patients with conchal pneumatization, this is not surprising given the low incidence of that pattern in adults.
Conclusions
Dimensions and septation patterns of the sphenoid sinus from 90 high-resolution CT images of patients without sinus pathology were analyzed. Pneumatization was described according to previously reported studies. The use of thin-cut image-guided radiographs in patients without skull base pathology and sphenoid rhinosinusitis allows for a complete categorization of sphenoid sinus anatomy without pathologic distortion. The data show great variability of sphenoid sinus anatomy and suggest careful preoperative evaluation when approaching the skull base through an endonasal transsphenoidal corridor.
Acknowledgments
The authors would like to thank the staff of the Department of Radiology at the University of Cincinnati for their time in acquiring the imaging studies used in this manuscript.
Conflicts of Interest The authors have nothing to disclose. Financial Disclosures The authors have nothing to disclose.
Notes
Presented as a poster at the American Rhinologic Society meeting; Fall 2013; Vancouver, BC, Canada.
References
- 1.Vidić B. The postnatal development of the sphenoidal sinus and its spread into the dorsum sellae and posterior clinoid processes. Am J Roentgenol Radium Ther Nucl Med. 1968;104(1):177–183. doi: 10.2214/ajr.104.1.177. [DOI] [PubMed] [Google Scholar]
- 2.DeLano M C, Fun F Y, Zinreich S J. Relationship of the optic nerve to the posterior paranasal sinuses: a CT anatomic study. AJNR Am J Neuroradiol. 1996;17(4):669–675. [PMC free article] [PubMed] [Google Scholar]
- 3.Lewin J S, Curtin H D, Eelkema E, Obuchowski N. Benign expansile lesions of the sphenoid sinus: differentiation from normal asymmetry of the lateral recesses. AJNR Am J Neuroradiol. 1999;20(3):461–466. [PMC free article] [PubMed] [Google Scholar]
- 4.Kazkayasi M, Karadeniz Y, Arikan O K. Anatomic variations of the sphenoid sinus on computed tomography. Rhinology. 2005;43(2):109–114. [PubMed] [Google Scholar]
- 5.Cho J H, Kim J K, Lee J G, Yoon J H. Sphenoid sinus pneumatization and its relation to bulging of surrounding neurovascular structures. Ann Otol Rhinol Laryngol. 2010;119(9):646–650. doi: 10.1177/000348941011900914. [DOI] [PubMed] [Google Scholar]
- 6.Aust M R, McCaffrey T V, Atkinson J. Transnasal endoscopic approach to the sella turcica. Am J Rhinol. 1998;12(4):283–287. doi: 10.2500/105065898781390028. [DOI] [PubMed] [Google Scholar]
- 7.Renn W H, Rhoton A L Jr. Microsurgical anatomy of the sellar region. J Neurosurg. 1975;43(3):288–298. doi: 10.3171/jns.1975.43.3.0288. [DOI] [PubMed] [Google Scholar]
- 8.Hamid O, El Fiky L, Hassan O, Kotb A, El Fiky S. Anatomic variations of the sphenoid sinus and their impact on trans-sphenoid pituitary surgery. Skull Base. 2008;18(1):9–15. doi: 10.1055/s-2007-992764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elwany S, Yacout Y M, Talaat M, El-Nahass M, Gunied A, Talaat M. Surgical anatomy of the sphenoid sinus. J Laryngol Otol. 1983;97(3):227–241. doi: 10.1017/s0022215100094056. [DOI] [PubMed] [Google Scholar]
- 10.Zada G, Agarwalla P K, Mukundan S Jr, Dunn I, Golby A J, Laws E R Jr. The neurosurgical anatomy of the sphenoid sinus and sellar floor in endoscopic transsphenoidal surgery. J Neurosurg. 2011;114(5):1319–1330. doi: 10.3171/2010.11.JNS10768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mutlu C, Unlu H H, Goktan C, Tarhan S, Egrilmez M. Radiologic anatomy of the sphenoid sinus for intranasal surgery. Rhinology. 2001;39(3):128–132. [PubMed] [Google Scholar]
- 12.Kinnman J. Surgical aspects of the anatomy of the sphenoidal sinuses and the sella turcica. J Anat. 1977;124(Pt 3):541–553. [PMC free article] [PubMed] [Google Scholar]
- 13.Ramakrishnan V R, Suh J D, Lee J Y, O'Malley B W Jr, Grady M S, Palmer J N. Sphenoid sinus anatomy and suprasellar extension of pituitary tumors. J Neurosurg. 2013;119(3):669–674. doi: 10.3171/2013.3.JNS122113. [DOI] [PubMed] [Google Scholar]
- 14.Hamberger C A, Hammer G, Norlen G, Sjogren B. Transantrosphenoidal hypophysectomy. Arch Otolaryngol. 1961;74:2–8. doi: 10.1001/archotol.1961.00740030005002. [DOI] [PubMed] [Google Scholar]


