Abstract
Background
Diabetes mellitus (DM) is associated with poor outcome after surgery. The prevalence of DM in hospitalised patients is up to 40%, meaning that the anaesthesiologist will encounter a patient with DM in the operating room on a daily basis. Despite an abundance of published glucose lowering protocols and the known negative outcomes associated with perioperative hyperglycaemia in DM, there is no evidence regarding the optimal intraoperative glucose lowering treatment. In addition, protocol adherence is usually low and protocol targets are not simply met.
Recently, incretins have been introduced to lower blood glucose. The main hormone of the incretin system is glucagon-like peptide–1 (GLP-1). GLP-1 increases insulin and decreases glucagon secretion in a glucose-dependent manner, resulting in glucose lowering action with a low incidence of hypoglycaemia.
We set out to determine the optimal intraoperative treatment algorithm to lower glucose in patients with DM type 2 undergoing non-cardiac surgery, comparing intraoperative glucose-insulin-potassium infusion (GIK), insulin bolus regimen (BR) and GPL-1 (liragludite, LG) treatment.
Methods/Design
This is a multicentre randomised open label trial in patients with DM type 2 undergoing non-cardiac surgery. Patients are randomly assigned to one of three study arms; intraoperative glucose-insulin-potassium infusion (GIK), intraoperative sliding-scale insulin boluses (BR) or GPL-1 pre-treatment with liraglutide (LG). Capillary glucose will be measured every hour. If necessary, in all study arms glucose will be adjusted with an intravenous bolus of insulin. Researchers, care givers and patients will not be blinded for the assigned treatment. The main outcome measure is the difference in median glucose between the three study arms at 1 hour postoperatively. We will include 315 patients, which gives us a 90% power to detect a 1 mmol l−1 difference in glucose between the study arms.
Discussion
The PILGRIM trial started in January 2014 and will provide relevant information on the perioperative use of GLP-1 agonists and the optimal intraoperative treatment algorithm in patients with diabetes mellitus type 2.
Trial registration
ClinicalTrials.gov, NCT02036372
Keywords: Diabetes mellitus type 2, Perioperative management, GLP-1 agonist
Background
It is expected that the worldwide prevalence of diabetes will increase from 220 million people now, to 300 million people in 2025 [1]. Type 2 diabetes mellitus (DM) is most common and accounts for 80% of the diabetic cases in the Western World [2]. Because DM is accompanied by macro- and microvascular complications, people with DM are more likely to be admitted to the hospital than people without DM. Twenty-two percent of in-hospital days are occupied by patients with DM, who are especially over-represented in the surgical population [3–5]. The prevalence of DM in hospitalised patients is up to 40% [3], thus the anaesthesiologist will encounter a patient with DM in the operating room on a daily basis.
Patients with DM have an increased risk of developing hyperglycaemia during and after surgery. The glycaemic control in the first 24 hours after surgery in patients with DM is poor and associated with an increased risk of postoperative infections [6–8]. In addition, hyperglycaemia is associated with increased risk of postoperative complications and length of hospital stay, irrespective of the diagnosis of DM [9–13].
Considering the high prevalence of DM in the operating theatre, the lack of evidence with regard to perioperative glucose regulation in non-cardiac surgery patients with DM is surprising. In contrast, stress hyperglycaemia in the ICU or in cardiac surgery patients has been investigated in a vast number of trials [14–16], but these studies did not focus on DM [17].
For the perioperative glucose regulation multiple protocols have been developed, ranging from intravenous glucose-insulin-potassium infusion to subcutaneous sliding-scale insulin bolus regimens. Despite this abundance of published glucose lowering protocols and the proven negative associations of perioperative hyperglycaemia in DM, there is no evidence to support an optimal perioperative glucose lowering treatment. In addition, DM protocol adherence is surprisingly low and glucose targets are frequently not achieved [18]. Considering only the postoperative period, the reduction of 1 mmol l−1 glucose in the RABBIT 2 surgery trial with a subcutaneous basal-bolus regimen compared to sliding scale algorithm significantly reduced postoperative complications in patients with DM type 2 [19]. These data also suggest that we cannot simply tolerate glucose levels above 10 mmol l−1.
Recently, incretins have been introduced to lower blood glucose. The main hormone of the incretin system is glucagon-like peptide–1 (GLP-1). GLP-1 increases insulin and decreases glucagon secretion in a glucose-dependent manner, resulting in low incidence of hypoglycaemia, which is a major advantage in the perioperative period and may reduce workload, thereby improving compliance. Intravenous administration of GLP-1 after major abdominal surgery normalised blood glucose levels, without causing hypoglycaemic events [20].
In conclusion, DM is a relevant and prevalent disease, which predisposes surgical patients to hyperglycaemia and postoperative complications. Despite being one of the most encountered co-morbidities in the operating theatre, there is a lack of clinical trials regarding the optimal perioperative management of elevated glucose levels. Our primary objective is to investigate the optimal intraoperative treatment algorithm to lower glucose in patients with DM type 2 undergoing non-cardiac surgery, comparing intraoperative GIK infusion, insulin bolus regimen and GPL-1 (liraglutide) treatment.
Methods/Design
Ethical approval
This study protocol was approved by the medical ethical committee of the Academic Medical Centre in Amsterdam and by the central committee on research involving human subjects (CCMO) acting as competent authority. The study protocol adheres to the Declaration of Helsinki and the guidelines of Good Clinical Practice (GCP). The study is registered at http://www.clinicaltrials.gov # NCT02036372.
Trial design
The study is a multicentre open-label randomised controlled trial in adult patients with DM type 2, to evaluate the best treatment algorithm to lower glucose in the intraoperative setting, utilizing three parallel study arms. We will compare a glucose-insulin-potassium (GIK) infusion to an insulin bolus regimen and to treatment with the GLP-1 agonist liraglutide. The consort flow diagram of the trial is shown in Figure 1.
Figure 1.
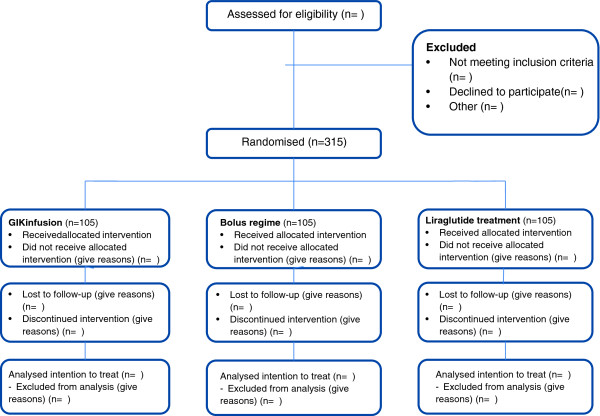
Consort flow diagram of PILGRIM trial.
Eligibility criteria
Patients with DM type 2, treated with oral glucose lowering tablets or a moderate dose of insulin, scheduled for non-cardiac surgery will be eligible for inclusion. This is also in concordance with the population studied in the RABBIT 2 surgery trial [19], showing a reduction in postoperative complications when lowering glucose by 1 mmol l−1. Further inclusion and exclusion criteria are listed below. We set a maximum of insulin dose per day, as we do not expect clinical effect from the GLP-1 agonist treatment when patients are treated with a daily dose of insulin >1 IU kg−1 bodyweight. Patients with a planned postoperative stay at the intensive care unit (ICU) will be excluded, as the participating ICU’s use a stricter glycaemic target, compared to the wards. Considering the suggested increased risk of pancreatitis when using GLP-1 analogues, patients with a history of acute or chronic pancreatitis are excluded. This point is more extensively addressed in the discussion section.
Inclusion criteria
Signed informed consent
known diabetes mellitus type 2 for >3 months
aged 18–75 years
scheduled for elective non-cardiac surgery
daily insulin dosage of <1 IU kg−1 body weight
Exclusion criteria
Oral corticosteroid use
Treatment with long acting GLP-1 agonist or DDP-4 inhibitor
Planned for day-care (ambulatory) surgery
Planned ICU stay post-operatively
Planned bowel surgery
History of chronic pancreatitis or idiopathic acute pancreatitis
Impaired liver function, defined as alanine aminotransferase (ALAT) ≥2.5 times upper normal limit
Impaired renal function defined as serum-creatinine ≥133 μmol l−1 for males and ≥115 μmol l−1 for females
Females of child bearing potential who are pregnant, breast-feeding or intend to become pregnant or are not using adequate contraceptive methods (adequate contraceptive measures as required by local law or practice)
Known or suspected allergy to trial product(s) or related products
Any condition that the local investigator feels would interfere with trial participation or the evaluation of results
Study outline
The patients will be recruited during a pre-assessment visit at the anaesthesiology department, where written and oral information will be provided to each patient. Written informed consent will be obtained either at the pre-assessment visit or prior to surgery. For each patient, age, weight, length, relevant medical history and current medication use will be recorded. During the trial, prophylactic dexamethasone treatment for postoperative nausea and vomiting (PONV) is not allowed, as it is unknown to what extent dexamethasone influences glucose in patients with DM. The anaesthetic details will be noted and the grade of nausea and vomiting will be evaluated 1 hour before surgery and 4 hours after surgery using the PONV intensity scale [21] and numeric rating scale (NRS). Thirty days postoperatively, all patients will be called for the assessment of postoperative complications (Tables 1, 2 and 3) and we will review the charts of the patients. Patients will be called at least at three different dates and times to minimize bias due to lost to follow up. All the data will be entered in a digital, good clinical practice (GCP) approved database. During the whole study period, all (serious) adverse events will be recorded and reviewed by the Principal Investigator, according to the GCP guidelines. If it is determined that a medication related serious adverse event presents an unreasonable risk to patients, we will terminate the study or part of the study presenting that risk. The trial will be monitored by an independent monitor.
Table 1.
Composite endpoint major complications
| Major complications | Definition |
|---|---|
| Death | 30- day mortality of any cause |
| Re-admission | Unplanned admission within 30 days after discharge |
| ICU-admission | Unplanned ICU-admission within 30 days after discharge |
| Re-operation | Unplanned surgical intervention within 30 days after discharge |
| Deep wound infection | CDC definition [23] |
| Pneumonia | CDC definition [23] |
| Sepsis/bacteremia | CDC definition [23] |
| Myocardial infarction | ECG changes/elevated troponine T and/or CK-MB enzymes |
| Cerebrovascular event | Diagnosed by CT-scan |
| Deep venous thrombosis | Diagnosed by Doppler and treatment started |
| Lung embolus | Diagnosed by spiral CT-scan |
| Stent thrombosis | Requiring surgical intervention |
| Bleeding | Requiring intervention or transfusion of RBC’s |
| Respiratory failure | Requiring intubation/ventilator assistance >24 hours |
| Renal failure | Requiring dialysis |
ICU = intensive care unit, CDC = centre for disease control, CXR = chest X-ray, ECG = electrocardiogram, RBC = red blood cells.
Table 2.
Composite endpoint minor complications
| Minor Complications | Definition |
|---|---|
| Cystitis or urinary tract infection | CDC definition [23] |
| Superficial wound infection/wound leakage | CDC definition [23]/leakage of the wound requiring longer duration of hospital stay |
| Pancreatitis | Clinical diagnosis/Elevated amylase or lipase |
| Ileus | Lasting more than 72 hours |
| Delirium | Clinical diagnosis |
| Length of hospital stay | In days |
CDC = centre for disease control.
Table 3.
Composite endpoint diabetes related complications
| Diabetes related complications | Definition |
|---|---|
| Hypoglycaemia | For which assistance was required |
| Diabetic Ketoacidosis | For which admission was required |
| Seeking medical help | Unplanned appointment with physician or DM nurse |
| Change in medication | Change in dose or medication stopped within 30 days of surgery |
| New medication | Additional diabetes medication started within 30 days of surgery |
Randomisation
If eligible, patients will be randomised into one of the three study arms. The randomisation will be 1:1:1 for each study arm, with stratification for insulin use. We will use block randomisation with random block sizes, ranging from 3 to 12. The randomisation will be performed with a computer based randomisation application (TENALEA Clinical Trial Data Management System). Patients and investigators are not blinded for the treatment allocation. All patients randomised will be included in the intention to treat analysis.
Study procedures/interventions
In all patients, capillary glucose will be measured every 60 minutes, starting 30 min prior to surgery. The target range for plasma glucose for all study arms is 6–8 mmol l−1. An intravenous bolus of insulin will be administered according to treatment algorithm (Table 4). Capillary glucose will be measured using the Accu-Chek Inform (Roche diagnostics, Indianapolis, IL, USA).
Table 4.
Treatment algorithm
| Glucose measurement* | Insulin 1st bolus | If glucose increases after 1st bolus | If glucose increases after 2nd bolus |
|---|---|---|---|
| 4-8 mmol/l | - | - | - |
| 8-9 mmol/l | 2 IU | 4 IU | 6 IU |
| 9-10 mmol/l | 3 IU | 5 IU | 7 IU |
| 10-11 mmol/l | 4 IU | 8 IU | 12 IU |
| 11-12 mmol/l | 5 IU | 9 IU | 13 IU |
| 12-13 mmol/l | 6 IU | 12 IU | 18 IU |
| 13-14 mmol/l | 7 IU | 13 IU | 19 IU |
| 14-15 mmol/l | 8 IU | 15 IU | 20 IU |
| 15-16 mmol/l | 9 IU | 16 IU | 21 IU |
| > 16 mmol/l** | 10 IU | 17 IU | 22 IU |
*If glucose is <4 mmol l−1, give 4 g glucose iv (20 ml glucose 20%) measure again after 10 minutes and consult research physician. If glucose is <2.3 mmol l−1 give 50 g glucose iv. (100 ml glucose 50%) measure again after 10 minutes and consult research physician. **Consult research physician. (multiply by 18 for mg dl−1).
Subjects in the glucose-insulin-potassium arm (GIK) will receive:
The day before surgery, the evening dose of long acting insulin will be reduced with 50%.
On the day of surgery, the regular insulin dose, if applicable, and the oral glucose lowering tablets will be withheld.
- GIK infusion: 10 mmol potassium-chloride and a calculated insulin dose are added to a 500 ml glucose 5% solution. The infusion is started 30 minutes before surgery at 83 ml/hr. The insulin dose in the GIK infusion will be calculated according to the formula:
- ○ I = (PG-7)/(200/W) + 8 I = Insulin amount, PG = glucose 30 minutes preoperative, W = body weight in kg.
- Measure glucose every 60 minutes after start of surgery, start 30 min prior to surgery
- ○ If glucose is 4–6 mmol l−1 stop infusion and measure again in 30 minutes
- ○ If glucose is <4 mmol l−1, give 4 g glucose iv. (20 ml glucose 20%),
- ○ measure again after 10 minutes and consult research physician.
-
○ If glucose is <2.3 mmol l−1, give 50 g glucose iv. (100 ml glucose 50%),measure again after 10 minutes and consult research physician.
- ○ If glucose is >8 mmol l−1, treat according to algorithm.
Subjects in the insulin Bolus Regimen arm (BR) will receive:
The day before surgery, the evening dose of long acting insulin will be reduced by 50%.
- On the day of surgery:
- ○ If patients are using mealtime and longacting insulin/NPH: mealtime morning dose will be withheld.
- ○ If patients are using only long acting insulin/NPH: the dose of long-acting or NPH insulin will be reduced by 50%
- ○ If patients are using glucose lowering tablets: glucose lowering tablets will be withheld on the morning of surgery.
Measure glucose every 60 min, start 30 min prior to surgery
Adjust glucose according to treatment algorithm
Subjects in the liraglutide arm (LG) will receive:
On the day before surgery 0.6 mg liraglutide will be administered subcutaneously (s.c.) at 17.00 hr (5 pm). The dose of long acting and mealtime insulin will be reduced by 50% from the start of liraglutide treatment.
On the day of surgery own insulin and oral glucose lowering tablets will be withheld.
In case of nausea graded higher than minimal, the second gift of liraglutide will be omitted. Otherwise, treatment will be continued with 1.2 mg liraglutide s.c. on the morning of surgery.
Measure glucose every 60 min, start 30 min prior to surgery
Adjust glucose according to treatment algorithm
Postoperatively
The assigned treatment will be continued up to 4 hours postoperatively. The patient will stay at the recovery room and will remain fasted. The treatment protocol will end 4 hours postoperatively. Hereafter, glucose will be monitored and treated according to the hospital protocol.
Laboratory measurements
HbA1c, potassium and fasting serum glucose will be determined 1 h prior to surgery. Fasting serum glucose and potassium will be determined 1 hour, 4 hours and on day 1 postoperatively. When the patient has an arterial catheter during the surgical procedure, arterial glucose will be measured.
Postoperative complications
The occurrence of postoperative complications will be assessed one month postoperatively. This will be determined via chart review and telephone contact. We will use a composite endpoint of postoperative complications derived from the RABBIT 2 surgery trial [19] and DelIT trial [22]. The definition of major and minor complications is shown in Tables 1 and 2. We used the definition of the centre for disease control (CDC) for the various infectious complications [23]. The occurrence of nausea and vomiting during hospital admission will be assessed and scored on the NRS scale. Diabetes related complications are shown in Table 3.
Outcome measures
Our primary outcome measure is the difference in median serum glucose between the GIK, BR and LG arm 1 hour after surgery.
The secondary outcome measures are the difference in median serum glucose between the three study arms at 4 hours and 1 day postoperatively, the difference in the amount of insulin administered and difference in the occurrence of major, minor and diabetes related complications. the hourly measurements will be used to determine the perioperative area under the curve of the area outside the target range. In addition, the occurrence of mild or severe hypoglycaemia (glucose <4.0 mmol l−1 and <2.3 mmol l−1, respectively), hypokalaemia (<3.5 mmol l−1) or hyperkalaemia (>5.0 mmol l−1) is assessed. The difference in glucose variability, described as mean absolute glucose change (MAG), between study arms will be calculated [24]. The MAG is calculated by adding the absolute differences of the glucose values, divided by the time over which the measurements were taken.
Statistical analyses
Sample size calculation
A 1 mmol l−1 decrease in glucose resulted in a relevant decrease in postoperative complications (8.7 mmol l−1 ± 1.8 and 9.7 ± 2.4) in the RABBIT 2 surgery trial [10]. We used the following formula to calculate the sample size:  . Assuming a power of 90%, a significance level of 5% and a drop-out rate of 10%, we will need 105 patients per treatment group to detect a relevant difference of 1 mmol l−1 between treatment groups. Thus in total, we will need 315 patients.
. Assuming a power of 90%, a significance level of 5% and a drop-out rate of 10%, we will need 105 patients per treatment group to detect a relevant difference of 1 mmol l−1 between treatment groups. Thus in total, we will need 315 patients.
Analyses
Statistical analyses will be performed using SPSS version 21.0 (SPSS Inc., Chicago, IL, USA). All data will be analysed according to an intention-to-treat analysis. No interim analysis is planned. Glucose is not normally distributed, thus the between group difference in median glucose at 1 hour, 4 hours and 1 day postoperatively will be tested with the Kruskal-Wallis test and post-hoc testing using the Mann–Whitney U test. In case of missing glucose at one hour, the last glucose measured during surgery will be carried forward. Change in glucose will be analysed using repeated measurements ANOVA, with time as fixed effect and baseline glucose, time and the interaction between treatments as covariates. Furthermore a per-protocol analysis will be performed next to the intention-to-treat analysis. Finally, the between group differences of the secondary outcomes will be tested with the ANOVA, Kruskal-Wallis, student t, Mann–Whitney U and the Chi-square test, where appropriate.
Discussion
Insulin infusion has been a long established regime for the treatment of DM in the perioperative period and is frequently combined with glucose and potassium for safety reasons [5, 25]. Moreover, a continuous infusion of glucose might reduce peripheral insulin resistance [26]. An alternative for the GIK infusion is an intravenous insulin bolus regime. Although no difference was seen in perioperative glucose control in insulin naïve- and insulin-dependent patients, an intravenous bolus regime might be less time consuming than a GIK infusion plus bolus regime [27, 28]. GLP-1 agonists have potential advantages over established DM treatments with insulin during the intraoperative period, due to the low risk of hypoglycaemia. For proper execution of all regimes, perioperative glucose measurements are mandatory.
Since the start of GLP-1 treatment, it has been suggested that the use of GLP-1 agonists is associated with an increased risk of pancreatitis [29]. However, patients with DM type 2 and obesity, regardless of treatment, have an increased risk of developing pancreatitis compared to patients without DM [30]. A recent meta-analysis of 55 randomized controlled trials (n = 33,350) showed no increased risk for pancreatitis in patients using GLP-1 agonists (OR 1.05, 95% CI 0.37 to 2.94) [31]. Also in a large observational trial with over 20,000 new incretin users, no increased risk for pancreatitis was found when compared to patients with DM using sulfonylureas, HR 1.00, 95% CI 0.59 to 1.70 [32]. Although these studies do not completely exclude the possibility of a slightly elevated risk of pancreatitis when using GLP-1 agonists, they are reassuring and an encouragement for more clinical trials using these new substances.
We think that the combination of perioperative use of GLP-1 agonists compared with more established perioperative treatment regimes, makes this a relevant trial on the optimal intraoperative treatment of DM during non-cardiac surgery.
Acknowledgements
We acknowledge the European Foundation for the Study of Diabetes (EFSD) for the research grant from the EFSD/Sanofi Fellowship 2012 #94653. We would like to acknowledge A. Zamanbin for her help with data recruitment.
Abbreviations
- DM
Diabetes mellitus
- GIK
Glucose-insulin-potassium
- BR
Bolus regime
- LG
Liraglutide
- GLP-1
Glucagon like peptide-1
- ICU
Intensive care unit
- CRF
Case report form
- NPH
Neutral protamine Hagedorn
- OR
Odds ratio
- HR
Hazard ratio
- CI
Confidence interval.
Footnotes
Competing interests
JHD is an advisor for Novo Nordisk in the field of GLP-1.
Authors’ contributions
JP drafted the manuscript and JH co-authored the writing. JHD and BP provided statistical and methodological advice. All authors participated in the design of the study during several meetings. All authors have read, commented on and approved the final manuscript.
Contributor Information
Jorinde AW Polderman, Email: j.a.polderman@amc.uva.nl.
Peter L Houweling, Email: phouweling@diakhuis.nl.
Markus W Hollmann, Email: m.w.hollmann@amc.uva.nl.
J Hans DeVries, Email: j.h.devries@amc.uva.nl.
Benedikt Preckel, Email: b.preckel@amc.uva.nl.
Jeroen Hermanides, Email: j.hermanides@amc.uva.nl.
References
- 1.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21(9):1414–1431. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 2.Akhtar S, Barash PG, Inzucchi SE. Scientific principles and clinical implications of perioperative glucose regulation and control. Anesth Analg. 2010;110(2):478–497. doi: 10.1213/ANE.0b013e3181c6be63. [DOI] [PubMed] [Google Scholar]
- 3.Levetan CS, Passaro M, Jablonski K, Kass M, Ratner RE. Unrecognized diabetes among hospitalized patients. Diabetes Care. 1998;21(2):246–249. doi: 10.2337/diacare.21.2.246. [DOI] [PubMed] [Google Scholar]
- 4.Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, Inzucchi SE, Ismail-Beigi F, Kirkman MS, Umpierrez GE, American Association of Clinical Endocrinologists, American Diabetes Association American association of clinical endocrinologists and American diabetes association consensus statement on inpatient glycemic control. Endocr Practice Off J Am College Endocrinol Am Assoc Clinical Endocrinol. 2009;15(4):353–369. doi: 10.4158/EP09102.RA. [DOI] [PubMed] [Google Scholar]
- 5.Robertshaw HJ, Hall GM. Diabetes mellitus: anaesthetic management. Anaesthesia. 2006;61(12):1187–1190. doi: 10.1111/j.1365-2044.2006.04834.x. [DOI] [PubMed] [Google Scholar]
- 6.Blondet JJ, Beilman GJ. Glycemic control and prevention of perioperative infection. Curr Opin Crit Care. 2007;13(4):421–427. doi: 10.1097/MCC.0b013e32826388a1. [DOI] [PubMed] [Google Scholar]
- 7.Frisch A, Chandra P, Smiley D, Peng L, Rizzo M, Gatcliffe C, Hudson M, Mendoza J, Johnson R, Lin E, Umpierrez GE. Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care. 2010;33(8):1783–1788. doi: 10.2337/dc10-0304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pomposelli JJ, Baxter JK, 3rd, Babineau TJ, Pomfret EA, Driscoll DF, Forse RA, Bistrian BR. Early postoperative glucose control predicts nosocomial infection rate in diabetic patients. JPEN J Parenter Enteral Nutr. 1998;22(2):77–81. doi: 10.1177/014860719802200277. [DOI] [PubMed] [Google Scholar]
- 9.Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, Hirsch IB, American Diabetes Association Diabetes in Hospitals Writing C Management of diabetes and hyperglycemia in hospitals. Diabetes Care. 2004;27(2):553–591. doi: 10.2337/diacare.27.2.553. [DOI] [PubMed] [Google Scholar]
- 10.Eshuis WJ, Hermanides J, van Dalen JW, van Samkar G, Busch OR, van Gulik TM, DeVries JH, Hoekstra JB, Gouma DJ. Early postoperative hyperglycemia is associated with postoperative complications after pancreatoduodenectomy. Ann Surg. 2011;253(4):739–744. doi: 10.1097/SLA.0b013e31820b4bfc. [DOI] [PubMed] [Google Scholar]
- 11.Finney SJ, Zekveld C, Elia A, Evans TW. Glucose control and mortality in critically ill patients. JAMA J Am Med Assoc. 2003;290(15):2041–2047. doi: 10.1001/jama.290.15.2041. [DOI] [PubMed] [Google Scholar]
- 12.Ponce BA, Menendez ME, Oladeji LO, Soldado F. Diabetes as a risk factor for poorer early postoperative outcomes after shoulder arthroplasty. J Shoulder Elbow Surgery/Am Shoulder Elbow Surg [et al] 2014;23(5):671–678. doi: 10.1016/j.jse.2014.01.046. [DOI] [PubMed] [Google Scholar]
- 13.Smiley DD, Umpierrez GE. Perioperative glucose control in the diabetic or nondiabetic patient. South Med J. 2006;99(6):580–589. doi: 10.1097/01.smj.0000209366.91803.99. [DOI] [PubMed] [Google Scholar]
- 14.Gandhi GY, Nuttall GA, Abel MD, Mullany CJ, Schaff HV, O'Brien PC, Johnson MG, Williams AR, Cutshall SM, Mundy LM, Rizza RA, McMahon MM. Intensive intraoperative insulin therapy versus conventional glucose management during cardiac surgery: a randomized trial. Ann Intern Med. 2007;146(4):233–243. doi: 10.7326/0003-4819-146-4-200702200-00002. [DOI] [PubMed] [Google Scholar]
- 15.Investigators N-SS, Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hebert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283–1297. doi: 10.1056/NEJMoa0810625. [DOI] [PubMed] [Google Scholar]
- 16.van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–1367. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- 17.Siegelaar SE, Devries JH, Hoekstra JB. Patients with diabetes in the intensive care unit; not served by treatment, yet protected? Crit Care. 2010;14(2):126. doi: 10.1186/cc8881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ley SCFR, Bossenroth E, Schlack WS, Preckel B. Datenlage zur perioperativen Diabetesbetreuung in einem universitatsklinikum. Diabetologe. 2008;4:13–19. doi: 10.1007/s11428-007-0187-2. [DOI] [Google Scholar]
- 19.Umpierrez GE, Smiley D, Jacobs S, Peng L, Temponi A, Mulligan P, Umpierrez D, Newton C, Olson D, Rizzo M. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery) Diabetes Care. 2011;34(2):256–261. doi: 10.2337/dc10-1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meier JJ, Weyhe D, Michaely M, Senkal M, Zumtobel V, Nauck MA, Holst JJ, Schmidt WE, Gallwitz B. Intravenous glucagon-like peptide 1 normalizes blood glucose after major surgery in patients with type 2 diabetes. Crit Care Med. 2004;32(3):848–851. doi: 10.1097/01.CCM.0000114811.60629.B5. [DOI] [PubMed] [Google Scholar]
- 21.Wengritzky R, Mettho T, Myles PS, Burke J, Kakos A. Development and validation of a postoperative nausea and vomiting intensity scale. Br J Anaesth. 2010;104(2):158–166. doi: 10.1093/bja/aep370. [DOI] [PubMed] [Google Scholar]
- 22.Abdelmalak B, Maheshwari A, Mascha E, Srivastava S, Marks T, Tang WW, Kurz A, Sessler DI. Design and organization of the Dexamethasone, light anesthesia and tight glucose control (DeLiT) trial: a factorial trial evaluating the effects of corticosteroids, glucose control, and depth-of-anesthesia on perioperative inflammation and morbidity from major non-cardiac surgery. BMC Anesthesiol. 2010;10:11. doi: 10.1186/1471-2253-10-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309–332. doi: 10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 24.Hermanides J, Vriesendorp TM, Bosman RJ, Zandstra DF, Hoekstra JB, Devries JH. Glucose variability is associated with intensive care unit mortality. Crit Care Med. 2010;38(3):838–842. doi: 10.1097/CCM.0b013e3181cc4be9. [DOI] [PubMed] [Google Scholar]
- 25.Thomas DJ, Platt HS, Alberti KG. Insulin-dependent diabetes during the peri-operative period. An assessment of continuous glucose-insulin-potassium infusion, and traditional treatment. Anaesthesia. 1984;39(7):629–637. doi: 10.1111/j.1365-2044.1984.tb06469.x. [DOI] [PubMed] [Google Scholar]
- 26.Ljungqvist O, Nygren J, Soop M, Thorell A. Metabolic perioperative management: novel concepts. Curr Opin Crit Care. 2005;11(4):295–299. doi: 10.1097/01.ccx.0000166395.65764.71. [DOI] [PubMed] [Google Scholar]
- 27.Hemmerling TM, Schmid MC, Schmidt J, Kern S, Jacobi KE. Comparison of a continuous glucose-insulin-potassium infusion versus intermittent bolus application of insulin on perioperative glucose control and hormone status in insulin-treated type 2 diabetics. J Clin Anesth. 2001;13(4):293–300. doi: 10.1016/S0952-8180(01)00276-8. [DOI] [PubMed] [Google Scholar]
- 28.Raucoules Aime M, Labib Y, Levraut J, Gastaud P, Dolisi C, Grimaud D. Use of i.v. insulin in well-controlled non-insulin-dependent diabetics undergoing major surgery. Br J Anaesth. 1996;76(2):198–202. doi: 10.1093/bja/76.2.198. [DOI] [PubMed] [Google Scholar]
- 29.Butler PC, Elashoff M, Elashoff R, Gale EA. A critical analysis of the clinical use of incretin-based therapies: Are the GLP-1 therapies safe? Diabetes Care. 2013;36(7):2118–2125. doi: 10.2337/dc12-2713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nauck MA. A critical analysis of the clinical use of incretin-based therapies: The benefits by far outweigh the potential risks. Diabetes Care. 2013;36(7):2126–2132. doi: 10.2337/dc12-2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li L, Shen J, Bala MM, Busse JW, Ebrahim S, Vandvik PO, Rios LP, Malaga G, Wong E, Sohani Z, Guyatt GH, Sun X. Incretin treatment and risk of pancreatitis in patients with type 2 diabetes mellitus: systematic review and meta-analysis of randomised and non-randomised studies. BMJ. 2014;348:g2366. doi: 10.1136/bmj.g2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Faillie JL, Azoulay L, Patenaude V, Hillaire-Buys D, Suissa S. Incretin based drugs and risk of acute pancreatitis in patients with type 2 diabetes: cohort study. BMJ. 2014;348:g2780. doi: 10.1136/bmj.g2780. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pre-publication history
- The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2253/14/91/prepub


