Abstract
Background
Although individuals with lower socioeconomic status may develop functional disability at younger ages, little is known about the prevalence and correlates of functional disability among late middle-aged and older patients admitted to safety-net hospitals.
Objectives
To determine the prevalence of pre-admission functional disability among late middle-aged and older safety-net inpatients, and to identify characteristics associated with functional disability by age.
Design
Cross-sectional analysis.
Setting
Safety-net hospital in San Francisco, California.
Participants
English, Spanish, and Chinese-speaking community-dwelling patients aged 55 and older admitted to a safety-net hospital with anticipated return to the community (N = 699).
Measurements
At hospital admission, patients reported their need for help performing 5 activities of daily living (ADLs) and 7 instrumental activities of daily living (IADLs) 2 weeks before admission. ADL disability was defined as needing help performing 1 or more ADLs and IADL disability as needing help performing 2 or more IADLs. Participant characteristics were assessed, including sociodemographics, health status, health-related behaviors, and health-seeking behaviors.
Results
Overall, 28.3% of participants reported that they had an ADL disability 2 weeks prior to admission and 40.4% reported an IADL disability. The prevalence of pre-admission ADL disability was 28.9% among those 55-59 years, 20.7% among those 60-69 years, and 41.2% among those aged 70 and older (P<.001). The prevalence of IADL disability had a similar distribution. The characteristics associated with functional disability differed by age: among adults aged 55-59, African Americans had a higher odds of ADL and/or IADL disability, while among participants aged 60-69 and aged 70 and older, inadequate health literacy was associated with functional disability.
Conclusion
Pre-admission functional disability is common among patients aged 55 and older admitted to a safety-net hospital. Late middle-aged patients admitted to safety-net hospitals may benefit from models of acute care currently used for older patients that prevent adverse outcomes associated with functional disability.
Keywords: disability, physical function, middle-aged, aged
Introduction
For many older adults, hospitalization leads to adverse outcomes including functional decline and the subsequent inability to live independently.1 Older adults who have functional disability before hospital admission – defined as needing help performing activities of daily living (ADL) or instrumental activities of daily living (IADLs) – are at increased risk for further functional decline during hospitalization,2-4 discharge to long-term care,5,6 and death.7 Studies of functional disability among hospitalized patients have focused on adults 70 years and older and show that about 30% of community-dwelling older adults have ADL disability prior to admission.3 However, functional disability develops in some middle-aged adults; low socioeconomic status is an important risk factor for earlier onset of disability.8 Earlier onset of disability may lead to increased societal costs, including higher health care spending.9
Little is known about the rate of functional disability among patients who receive care in safety-net health systems in the United States. These health systems provide medical care to patients who are uninsured, underinsured, or insured by Medicaid.10 Many patients at safety-net hospitals have poor health status and high rates of chronic conditions.10 Patients in safety-net hospitals tend to be younger than those in non-safety-net hospitals, with a higher proportion of adults aged 50-64 years, and a lower proportion aged 65 or older.11,12
This study determined the prevalence of functional disability prior to hospitalization in community-dwelling patients aged 55 and older admitted to an urban safety-net hospital, and identified the characteristics associated with functional disability in participants by age group. We hypothesized that the rate of pre-admission functional disability among patients aged 55-59 and 60-69 would be similar to that of community-dwelling patients aged 70 and older hospitalized at non-safety-net hospitals, and that participant characteristics associated with functional disability would be similar to those identified previously in the general population.
Methods
Design overview
We interviewed patients admitted to San Francisco General Hospital and Trauma Center (SFGH), an urban safety-net hospital with 590 licensed beds and over 100,000 patient visits per year.13 These interviews were part of the enrollment interview for the Support from Hospital to Home for Elders study, a randomized controlled trial which compared a nurse-led intervention to improve the quality of care during the peri-discharge period to usual care (clinicaltrials.gov Identifier NCT01221532).
Setting and participants
Patients were eligible for enrollment if they were admitted to the medicine, family medicine, cardiology, or neurology services of SFGH and spoke English, Spanish, or Chinese (Cantonese or Mandarin). Between July 2010 and March 2011, study staff recruited patients aged 60 and older. Because the number of eligible patients was lower than projected, the age eligibility was expanded to include patients aged 55 and older between March 2011 and August 2012. Potential participants were excluded if they were transferred from an outside hospital or skilled nursing facility; were admitted for a planned hospitalization; were expected by the admitting physician to be discharged to a nursing home, rehabilitation center or hospice; could not provide written informed consent for any reason (e.g., severe cognitive impairment or mental illness, delirium); had metastatic cancer; or were unable to participate in telephone follow-up due to aphasia, severe hearing impairment, or lack of access to a telephone. Study staff enrolled participants 6 days per week, Monday through Saturday. Patients admitted on Sunday were recruited the following day. Staff received a daily list of hospitalized patients meeting the age and admitting service criteria, and then approached the patient's attending physician to ask permission to recruit the patient and to determine if the patient met all eligibility criteria. Participants who completed the baseline interview received a $10 pharmacy or grocery store gift certificate. The Institutional Review Board of the University of California, San Francisco approved the study.
Measures
At study enrollment, participants underwent in-person interviews conducted by trained study staff in English, Spanish, or Chinese. Interviews were conducted using questionnaires translated by a native speaker of Chinese (both Cantonese and Mandarin) or Spanish from English to the other language. For each language, a second person then back-translated into English, and the research team revised the original translation as needed to conform with the original meaning. Staff completed interviews at the participant's bedside during hospitalization.
Functional status
To assess pre-admission function, participants were asked to report their functional status 2 weeks before the current admission. Participants reported their need for help performing 5 Activities of Daily Living (ADLs; bathing, dressing, eating, transferring, toileting),14 and 7 Instrumental Activities of Daily Living (IADLs; telephone use, transportation, shopping, meal preparation, light housework, medication management, money management).15 ADL disability was defined as needing help performing 1 or more ADLs 2 weeks prior to hospital admission, and IADL disability as needing help performing 2 or more IADLs 2 weeks prior to hospital admission.
Participant characteristics
Sociodemographic variables
Demographic characteristics were assessed, including age, sex, race/ethnicity, and primary language. Race/ethnicity was categorized as white non-Latino, African American, Asian, Latino, or other/refused. English was defined as the primary language if participants reported speaking English ‘well’ or ‘very well’ (vs. ‘not well’ or ‘not at all’). To measure socioeconomic status, years of education and total household income were assessed. Health literacy was measured using a validated instrument composed of 3 questions, each scored on a 5-point Likert scale: “How confident are you filling out medical forms?”; “How often do you have problems learning about your medical condition because of difficulty understanding written information?”; and “How often do you have someone help you read hospital materials?” (range, 3-15; inadequate health literacy defined as a score ≥9).16 Homelessness during the past year was defined as sleeping in the street, a homeless shelter, or a place not ordinarily used as a sleeping accommodation, and housing instability during the past year was defined as doubling-up with friends or family, staying in a single-room occupancy hotel, or living in more than 4 different places.17
Health status
To measure physical and mental health status, the 12-item Short Form Health Survey (SF-12) was used(range 0-100 for physical and mental health subscales).18 To assess comorbidity burden, the Charlson Comorbidity Index was calculated using International Classification of Diseases, Ninth Revision (ICD-9) codes extracted from administrative data recorded during hospital admission (scores 0, 1-2, 3-4, and ≥5; higher scores indicate higher mortality risk).19,20 Major depression was defined as a score ≥10 on the 9-item Patient Health Questionnaire (range, 0-27).21
Health-related behaviors
To assess alcohol use, the World Health Organization Alcohol, Smoking and Substance Involvement instrument was used (range, 0-39; scores of 0-10, 11-26, and ≥27 correspond to low, moderate, and high risk alcohol use, respectively).22 Illicit drug use was defined as self-reported use of cocaine, amphetamines, or non-prescribed opioids in the past 3 months. Tobacco use was measured by self-reported smoking status (former, current, or never).
Health-seeking behaviors
Hospital administrative data were used to determine the participant's health insurance upon hospitalization (Medicare, Medicaid, County-funded health plan for the uninsured, private, or uninsured).
Statistical analyses
Functional disability and participant characteristics were described using means and standard deviations or medians and interquartile ranges for continuous variables and frequencies and proportions for categorical variables. Rates of functional disability were initially examined in 5-year prevalence bands (e.g., ages 55-59, 60-64, 65-69). As the prevalence of functional disability was similar among those aged 60-64 and 65-69, these groups were recombined to maintain power and describe rates of disability by decade. Chi-square tests were used to test for differences in rates of functional disability among participants aged 55-59, 60-69, and 70 and older. To test for differences in participant characteristics across age groups, ANOVA was used for continuous variables, tests for trend for binary variables, and chi-square tests for categorical variables with more than 2 levels.
To identify the characteristics associated with functional disability in these age groups, age-stratified logistic regression models were examined for both ADL and IADL disability. Covariates for bivariable analyses were selected a priori to incorporate risk factors for functional disability identified in previous research.23,24 To allow for comparisons of the adjusted associations between age groups, covariates with a P value <.20 were included in bivariable analyses for any age group in the final age-stratified multivariable models. All analyses were conducted using SAS version 9.2 (SAS Institute, Cary, North Carolina).
Results
Sample
We identified 6,384 admissions of patients who met age criteria and were admitted to eligible services. Of these patients, 4,603 were excluded prior to screening based on pre-specified criteria (non-study language (n=466); planned admission (n=101); screened out by primary team (n=917); previously enrolled in trial (n=551); previously refused (n=82); less than 24-hour stay (n=1350); discharged before assessment (n=94); transferred to other service (n=233); transferred to/from institution (n=809)). Of the 1781 eligible patients whom we approached, 700 were enrolled and 1081 were excluded upon screening (no phone (n=583); lives elsewhere (n=46); left hospital before enrollment completed (n=111); unable to provide informed consent (n=96); declined (n=169); other (n=76)). One patient withdrew prior to the baseline assessment, for a total of 699 participants.
Participant characteristics
The mean age of the cohort was 66.2 years (standard deviation (SD) 9.0 years) (Table 1). The mean age of participants aged 55-59 years, 60-69 years, and 70 years and older was 57.2 years (SD 1.2), 63.5 years (SD 2.5), and 78.7 years (SD 6.4), respectively. The percentage of male participants decreased over the age groups, as did the percentage of white participants, African American participants, and participants who spoke English as a primary language. The percentage of participants who had 6 or fewer years of education increased, as did the percentage of participants with inadequate health literacy.
Table 1. Baseline characteristics of 699 patients admitted to an urban safety-net hospital.
| Characteristic | All participants (N=699) |
55-59 years (N=166) |
60-69 years (N=339) |
≥70 years (N=194) |
P valuea |
|---|---|---|---|---|---|
| Sociodemographic variables | |||||
| Age, mean years (standard deviation) | 66.2 (9.0) | 57.2 (1.2) | 63.5 (2.5) | 78.7 (6.4) | <.001 |
| Male, No. (%) | 394 (56.4) | 105 (63.3) | 197 (58.1) | 93 (47.9) | .003 |
| Race/ethnicity, No. (%) | <.001 | ||||
| White, non-Latino | 132 (18.9) | 40 (24.1) | 68 (20.1) | 25 (12.9) | |
| African American, non-Latino | 171 (24.5) | 55 (33.1) | 81 (24.0) | 35 (18.0) | |
| Asian | 225 (32.2) | 32 (19.3) | 110 (32.4) | 83 (42.8) | |
| Latino | 137 (19.6) | 32 (19.3) | 65 (19.2) | 40 (20.6) | |
| Other, don't know, or refused | 33 (4.7) | 7 (4.2) | 15 (4.4) | 11 (5.7) | |
| Education, years, No. (%) | <.001 | ||||
| 0-6 years | 154 (22.1) | 19 (11.4) | 61 (18.0) | 74 (38.1) | |
| 7-11 years | 140 (20.1) | 39 (23.5) | 61 (18.0) | 40 (20.6) | |
| 12 years | 172 (24.6) | 49 (29.5) | 92 (27.1) | 32 (16.5) | |
| >12 years | 232 (33.2) | 59 (35.5) | 125 (36.9) | 48 (24.7) | |
| Total household income, No. (%) | <.001 | ||||
| ≤$5,000/year | 147 (21.6) | 47 (29.0) | 74 (22.3) | 26 (14.0) | |
| $5,001-20,000/year | 457 (67.3) | 88 (54.3) | 220 (66.3) | 150 (80.6) | |
| ≥$20,001/year | 75 (11.0) | 27 (16.7) | 38 (11.4) | 10 (5.4) | |
| Foreign-born | 358 (51.4) | 54 (32.5) | 173 (51.5) | 131 (67.5) | <.001 |
| Language spoken at home, No. (%) | <.001 | ||||
| English | 368 (52.7) | 117 (70.5) | 175 (51.6) | 77 (39.7) | |
| Cantonese or Mandarin | 153 (21.9) | 20 (12.0) | 75 (22.1) | 58 (29.9) | |
| Spanish | 112 (16.0) | 19 (11.4) | 55 (16.2) | 38 (19.6) | |
| Tagalog | 28 (4.0) | 5 (3.0) | 17 (5.0) | 6 (3.1) | |
| Other | 37 (5.3) | 5 (3.0) | 17 (5.0) | 15 (7.7) | |
| Primary language English, No. (%)b | 439 (62.9) | 130 (78.3) | 218 (64.3) | 92 (47.4) | <.001 |
| Inadequate health literacy, No. (%)c | 350 (51.6) | 60 (37.3) | 164 (49.8) | 126 (67.0) | <.001 |
| Housing status, past year, No. (%) | |||||
| Homelessness | 29 (4.2) | 15 (9.0) | 10 (3.0) | 4 (2.1) | .001 |
| Housing instability | 129 (18.5) | 52 (31.3) | 60 (17.8) | 17 (8.8) | <.001 |
| Health status variables | |||||
| Health status (SF-12), mean score (standard deviation) | |||||
| Mental component | 45.4 (11.6) | 42.9 (11.9) | 45.3 (11.7) | 47.8 (10.6) | <.001 |
| Physical component | 36.1 (10.7) | 34.5 (11.2) | 36.9 (10.4) | 36.2 (10.5) | <.001 |
| Depression, No (%)d | 235 (33.9) | 74 (44.6) | 105 (31.3) | 56 (29.0) | .002 |
| Charlson comorbidity score, median (interquartile range) | 2.0 (1.0, 3.0) | 2.0 (1.0, 3.0) | 2.0 (1.0, 3.0) | 2.0 (1.0, 3.0) | .06 |
| Charlson comorbidity score, No (%) | |||||
| 0 | 93 (13.3) | 23 (13.9) | 45 (13.4) | 25 (12.9) | .17 |
| 1-2 | 353 (50.6) | 91 (54.8) | 175 (51.9) | 87 (44.8) | |
| 3-4 | 155 (22.2) | 28 (16.9) | 70 (20.8) | 57 (29.4) | |
| ≥5 | 96 (13.8) | 24 (14.5) | 47 (13.9) | 25 (12.9) | |
| Health-related behaviors | |||||
| High or moderate risk alcohol use, No. (%)e | 72 (10.3) | 31 (18.7) | 33 (9.8) | 8 (4.1) | <.001 |
| Illicit drug use, No. (%)f | 54 (7.7) | 28 (16.9) | 25 (7.4) | 1 (0.5) | <.001 |
| Tobacco use, No. (%) | <.001 | ||||
| Current | 165 (23.7) | 55 (33.1) | 92 (27.4) | 18 (9.3) | |
| Former | 275 (39.5) | 68 (41.0) | 126 (37.5) | 81 (41.8) | |
| Health-seeking behaviors variables | |||||
| Health insurance, No. (%) | <.001 | ||||
| Medicare | 295 (42.4) | 20 (12.0) | 107 (31.8) | 168 (87.0) | |
| Medicaid | 116 (16.7) | 45 (27.1) | 58 (17.3) | 13 (6.7) | |
| County-funded health plan for uninsured | 146 (21.0) | 51 (30.7) | 92 (27.4) | 3 (1.6) | |
| Private | 8 (1.2) | 4 (2.4) | 2 (0.6) | 2 (1.0) | |
| Uninsured | 122 (17.6) | 44 (26.5) | 71 (21.1) | 7 (3.6) | |
| Other government insurance | 8 (1.2) | 2 (1.2) | 6 (1.8) | 0 (0.0) |
Abbreviations: SF-12, 12-item Short Form Health Survey.
P value calculated using ANOVA for continuous variables, tests for trend for binary variables, and chi-square tests for categorical variables with more than 2 levels.
Primary language other than English defined as speaking English ‘not at all’ or ‘not well.’
Inadequate health literacy defined as a score ≥9 on a 3-item instrument.
Depression defined as a 9-item Patient Health Questionnaire Score ≥10.
High or moderate risk alcohol use defined as a World Health Organization Alcohol, Smoking and Substance Involvement score ≥11.
Illicit drug use defined as use of cocaine, amphetamines, or non-prescribed opioids during the past 3 months.
The distribution of Charlson comorbidity scores was similar between the 3 age groups. The most common comorbidities in the overall cohort were diabetes (38.1%), chronic pulmonary disease (28.7%), congestive heart failure (25.0%), liver disease (24.6%), and kidney disease (19.8%). Depression prevalence decreased with age. Participants aged 55-59 had higher rates of substance use than older age groups, including high or moderate risk alcohol use, illicit drug use, and current tobacco use.
The percentage of participants who lacked insurance decreased with age, as did the percentage of participants insured by Medicaid; the percentage of participants insured by Medicare increased across age groups (Table 1).
Functional disability
Overall, 28.3% of participants reported that they had an ADL disability 2 weeks prior to admission and 40.4% reported an IADL disability (Figure 1; Table 2). The prevalence of pre-admission ADL disability was 28.9% among those 55-59 years, 20.7% among those 60-69 years, and 41.2% among those aged 70 years and older (P<.001). The prevalence of IADL disability had a similar distribution. The most commonly-reported ADL disabilities were bathing and dressing, and the most common IADL disabilities were shopping, meal preparation, and housework.
Figure 1.
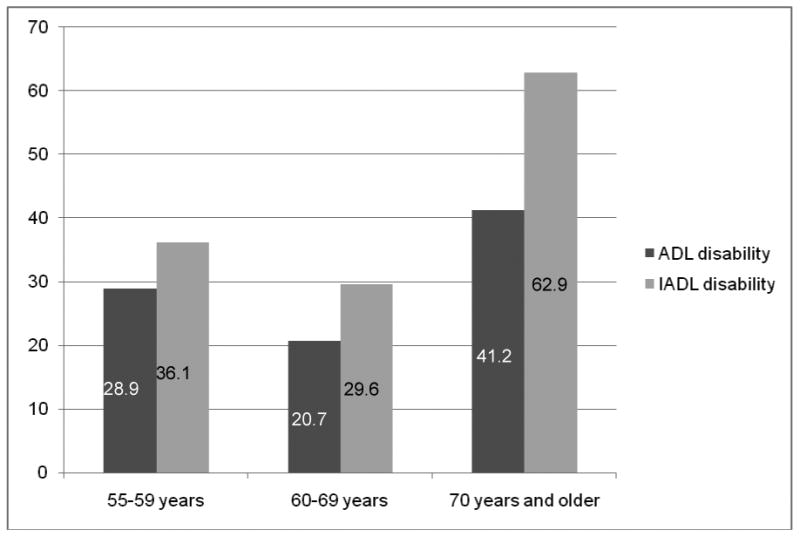
Prevalence of functional disability among 699 patients admitted to a safety-net hospital.
Abbreviations: ADL, activity of daily living; IADL, instrumental activity of daily living. ADL disability defined as need for help performing ≥1 ADLs 2 weeks prior to hospital admission, and IADL disability as need for help performing ≥2 IADLs 2 weeks prior to hospital admission. P<.001 for difference in prevalence of both ADLs and IADLs across age groups.
Table 2. Functional disability among 699 patients admitted to an urban safety-net hospital.
| All participants (N=699) |
55-59 years (N=166) |
60-69 years (N=339) |
≥70 years (N=194) |
P valueb | |
|---|---|---|---|---|---|
| ADL disability, No. (%)a | 198 (28.3) | 48 (28.9) | 70 (20.7) | 80 (41.2) | <.001 |
| Bathing | 142 (20.3) | 35 (21.1) | 51 (15.1) | 56 (29.2) | <.001 |
| Dressing | 139 (19.9) | 34 (20.5) | 46 (13.6) | 59 (30.4) | <.001 |
| Transferring | 117 (16.8) | 24 (14.5) | 43 (12.8) | 50 (25.9) | <.001 |
| Eating | 85 (12.2) | 15 (9.0) | 34 (10.1) | 36 (18.6) | .006 |
| Toileting | 58 (8.3) | 16 (9.6) | 21 (6.2) | 21 (10.8) | 0.14 |
| IADL disability, No. (%)c | 354 (50.6) | 60 (36.1) | 100 (29.6) | 122 (62.9) | <.001 |
| Shopping | 260 (37.7) | 53 (32.5) | 97 (29.1) | 110 (57.0) | <.001 |
| Light housework | 235 (34.1) | 49 (30.6) | 83 (25.1) | 102 (53.4) | <.001 |
| Meal preparation | 228 (33.0) | 49 (30.1) | 79 (23.7) | 100 (51.8) | <.001 |
| Transportation | 186 (26.7) | 35 (21.1) | 62 (18.3) | 88 (46.1) | <.001 |
| Medication management | 135 (21.0) | 31 (20.7) | 45 (14.8) | 59 (31.4) | <.001 |
| Money management | 122 (17.7) | 28 (16.9) | 39 (11.8) | 55 (28.7) | <.001 |
| Using the telephone | 42 (6.0) | 12 (7.2) | 11 (3.3) | 19 (9.8) | .007 |
Abbreviations: ADL, activity of daily living; IADL, instrumental activity of daily living.
ADL disability defined as need for help performing ≥1 ADLs.
P value calculated using chi-square tests.
IADL disability defined as need for help performing ≥2 IADLs.
Association of participant characteristics and functional disability
ADL disability
In multivariable analyses, among participants aged 55-59, African Americans had a higher odds of ADL disability (adjusted odds ratio (AOR), 3.2 [95% CI, 1.0-10.2]), as did persons with fewer than 12 years of education (AOR, 3.7 [95% CI, 1.4-9.8]) (Table 3). Neither of these variables was associated with elevated odds in the older age groups. Inadequate health literacy was associated with a higher odds of ADL disability among participants aged 70 and older, but not participants in other age groups (AOR, 2.9 [95% CI, 1.2-7.3]).
Table 3. Characteristics associated with pre-admission disability in activities of daily livinga among 699 patients admitted to a safety-net hospital.
| Adjusted Odds Ratios (95% CI) | |||
|---|---|---|---|
| Characteristics | 55-59 years | 60-69 years | ≥70 years |
| Female | 1.3 (0.5-3.2) | 1.9 (1.0-3.7) | 1.8 (0.8-3.8) |
| Race/ethnicity | |||
| White, non-Latino | 1.0 | 1.0 | 1.0 |
| African American, non-Latino | 3.2 (1.0-10.2) | 1.5 (0.6-4.0) | 0.7 (0.2-2.7) |
| Asian | 1.8 (0.3-10.9) | 1.5 (0.5-4.7) | 2.0 (0.5-7.9) |
| Latino | 1.0 (0.2-4.5) | 1.2 (0.4-4.0) | 0.9 (0.2-4.0) |
| Other, don't know, or refused | 2.6 (0.3-20.9) | 1.6 (0.4-7.1) | 2.0 (0.3-13.2) |
| <12 years of education | 3.7 (1.4-9.8) | 1.2 (0.6-2.7) | 0.9 (0.4-2.0) |
| Income ≤$20,000 per year | 3.6 (0.7-18.1) | 1.5 (0.6-4.3) | 1.2 (0.3-5.9) |
| Primary language Englishb | 2.9 (0.6-14.3) | 2.9 (0.9-8.3) | 1.1 (0.4-3.2) |
| Inadequate health literacyc | 1.5 (0.6-3.9) | 1.4 (0.7-2.9) | 2.9 (1.2-7.3) |
| Depressiond | 3.8 (1.5-9.4) | 2.6 (1.4-4.8) | 3.8 (1.7-8.4) |
| Charlson comorbidity score | |||
| 0 | 1.0 | 1.0 | 1.0 |
| 1-2 | 3.3 (0.6-18.1) | 3.1 (0.7-14.4) | 0.6 (0.2-1.7) |
| ≥3 | 3.5 (0.6-20.9) | 7.1 (1.5-33.0) | 1.7 (0.6-5.3) |
Disability in activities of daily living (ADLs) defined as needing help to perform ≥1 ADLs.
Primary language other than English defined as speaking English “not at all” or “not well.”
Inadequate health literacy defined as a score ≥9 on a 3-item instrument.
Depression defined as a 9-item Patient Health Questionnaire Score ≥10.
Model also adjusted for high or moderate risk alcohol use (defined as a World Health Organization Alcohol, Smoking and Substance Involvement score ≥11) and illicit drug use (defined as use of cocaine, amphetamines, or non-prescribed opioids during the past 3 months).
Depression was associated with ADL disability in all age groups (55-59 years, AOR, 3.8 [95% CI 1.5-9.4]), 60-69 years, AOR, 2.6 [95% CI 1.4-4.8], 70-79 years, AOR, 3.8 [95% CI 1.7-8.4]). A Charlson comorbidity score of ≥3 was significantly associated with ADL disability only among participants aged 60-69 (7.1 [95% CI, 1.5-33.0]); the direction of association was similar in the other 2 age groups but did not reach significance.
IADL disability
The multivariable models of IADL disability showed a pattern of associations similar to those of the ADL models in terms of depression and Charlson scores (Table 4). However, the associations of race/ethnicity and education differed between the ADL and IADL models for adults aged 55-59. Asians had a lower odds of IADL disability in this age group, but in contrast to the ADL models, neither African Americans nor participants with lower educational attainment had a higher odds of IADL disability. Speaking English as a primary language was associated with IADL disability among participants aged 60-69, and inadequate health literacy was associated with IADL disability among participants 60-69 years and 70 years and older.
Table 4. Characteristics associated with pre-admission disability in instrumental activities of daily livinga among 699 patients admitted to a safety-net hospital.
| Adjusted Odds Ratios (95% CI) | |||
|---|---|---|---|
| Characteristics | 55-59 years | 60-69 years | ≥70 years |
| Female | 2.0 (0.8-4.9) | 2.2 (1.2-3.9) | 2.4 (1.1-5.3) |
| Race/ethnicity | |||
| White, non-Latino | 1.0 | 1.0 | 1.0 |
| African American, non-Latino | 1.7 (0.6-4.8) | 1.4 (0.6-3.3) | 0.6 (0.1-2.1) |
| Asian | 0.1 (0.01-1.0) | 0.5 (0.2-1.5) | 1.7 (0.4-6.7) |
| Latino | 0.3 (0.1-1.2) | 0.7 (0.3-2.1) | 2.2 (0.5-9.6) |
| Other/refused | 2.0 (0.3-14.9) | 0.9 (0.2-3.5) | 0.9 (0.1-5.9) |
| <12 years of education | 1.9 (0.7-5.0) | 1.3 (0.6-2.7) | 1.1 (0.5-2.5) |
| Income ≤$20,000 per year | 1.9 (0.6-6.5) | 1.9 (0.7-4.8) | 1.5 (0.3-8.7) |
| Primary language Englishb | 0.5 (0.1-2.6) | 2.9 (1.0-8.3) | 1.2 (0.4-3.8) |
| Inadequate health literacyc | 1.1 (0.4-2.9) | 2.1 (1.0-4.3) | 4.9 (2.0-12.2) |
| Depressiond | 5.6 (2.3-13.4) | 2.9 (1.6-5.2) | 3.5 (1.4-8.5) |
| Charlson comorbidity score | |||
| 0 | 1.0 | 1.0 | 1.0 |
| 1-2 | 2.3 (0.5-9.5) | 2.0 (0.6-6.3) | 1.1 (0.3-3.5) |
| ≥3 | 2.4 (0.5-11.0) | 4.2 (1.3-13.5) | 2.9 (0.8-9.7) |
Disability in instrumental activities of daily living (IADLs) defined as needing help to perform ≥2 IADLs.
Primary language other than English defined as speaking English “not at all” or “not well.”
Inadequate health literacy defined as a score ≥9 on a 3-item instrument.
Depression defined as a 9-item Patient Health Questionnaire Score ≥10.
Model also adjusted for high or moderate risk alcohol use (defined as a World Health Organization Alcohol, Smoking and Substance Involvement score ≥11) and illicit drug use (defined as use of cocaine, amphetamines, or non-prescribed opioids during the past 3 months).
Discussion
This study demonstrates that the prevalence of pre-admission functional disability was high among community-dwelling adults aged 55 and older admitted to a safety-net hospital. The rate of ADL disability among patients aged 55-59 in this cohort was similar to documented rates among community-dwelling adults aged 70 and older admitted to a non-safety-net hospital (28.9% vs. 27%), while the rate of ADL disability in patients aged 70 years and older was higher (41.2%).3 These findings suggest that interventions to prevent hospital-associated functional decline that are restricted to patients aged 65 and older, such as Acute Care for Elders (ACE) units,25 may miss a large segment of at-risk adults hospitalized in safety-net settings.
In contrast to the high prevalence of ADL disability in participants 55-59 years, the prevalence of IADL disability within this age group was substantially lower than that of participants 70 years and older. The relatively lower rate of IADL disability among late middle-aged participants is consistent with research showing that disability in middle-aged adults develops through different pathways than it does in older adults. Older adults are thought to develop disability through a multifactorial process including the gradual accumulation of comorbid conditions, physiological changes related to aging, and deconditioning. This disabling process has been shown to result in a hierarchical loss of independence in IADLs followed by ADLs.26,27 In contrast, adults in their fifties and sixties are thought to become disabled through an isolated event such as an illness or trauma, such that ADL disability may develop independently of IADL disability.28
In thiscohort, the prevalence of ADL and IADL disability showed a U-shaped distribution across age groups, with rates of disability highest among participants 55-59 years and 70 years and older. The U-shaped distribution was unexpected, as previous studies in the general population show that rates of disability increase with age.29 This pattern of disability likely reflects shifts in the characteristics of the safety-net population across age groups. Compared to the older age groups, a higher percentage of participants aged 55-59 were African American, a characteristic associated with a higher odds of ADL disability in our cohort. This finding is consistent with previous work showing that African Americans have higher rates of disability across the adult lifespan compared to whites, and that these disparities peak in middle age.30-33
Compared to the younger participants, the oldest participants included a higher percentage of foreign-born individuals, consistent with previous research.34,35 Older immigrants may seek care at safety-net hospitals because they lack Medicare36 or because they are less able to navigate non-safety-net institutions compared to non-immigrants. Furthermore, American-born individuals who obtain Medicare may leave the safety-net to seek care at other hospitals. While younger immigrants have lower rates of disability than other groups (the so-called “healthy migrant” effect),37 older immigrants at safety-net hospitals may represent a more vulnerable group, with a history of poor access to health care,36 poorly-controlled chronic illness, and higher rates of functional disability. The association of inadequate health literacy with functional disability in this age group may reflect a history of poor access to care, which is thought to mediate the association between lower health literacy and poorer health outcomesamong older adults.38
The relatively lower prevalence of ADL and IADL disability observed among participants aged 60-69 may reflect several converging factors. A growing body of research shows that disparities in health status by both race/ethnicity and socioeconomic status peak in middle age,33,39,40 possibly because vulnerable populations experience accumulated exposures to socioeconomic disadvantage earlier in life.41 These disparities then decline in older age, likely due to a survival effect and the availability of age-linked benefits including Medicare.41 Both of these factors are likely at play in this study. The sickest persons aged 55-59 years, including both African Americans and those with substance use problems, may die at younger ages.42,43
The high rate of functional disability found in this study has important implications for the acute care of patients in safety-net hospitals. Acute Care for Elders (ACE) units have been shown to be effective in identifying functional disability in older adults and preventing associated functional decline and discharge to long-term care.25 ACE units in safety-net hospitals might consider broadening their reach to include patients age 55 and older. As correlates of disability appear to differ by age, it is not clear whether the same interventions that have proven effective in improving functional status among hospitalized older adults will be appropriate for hospitalized younger adults. It is possible that those who are younger than age 70 and have functional disabilities may have different post-hospitalization trajectories and require different interventions than those currently offered. This hypothesis deserves exploration.
The study has several limitations. Because the age eligibility was changed during enrollment, the age distribution in thecohort does not reflect the source population. However, this change does not affect the validity of the within-study age comparisons. The rate of self-reported difficulty eating was unexpectedly high for a cohort of patients admitted from the community, raising the issue of the question's validity in non-English speaking participants. Although the Katz ADL and Lawton IADL scales are widely used in other languages including Spanish and Chinese, relatively little is known about the cross-cultural validity of these scales.44,45 The study used standard practices for adapting self-report measures for cross-cultural use, including translation and back-translation.46 It is also possible that the relatively high rate of difficulty eating reflects that participants in this study experienced a different pathway to disability, in which disability results from a single disabling event, such as a stroke, rather than through the gradual accumulation of deficits typically observed among older adults. The rate of functional disability in this cohort likely underestimates the true rate of disability among patients admitted to safety-net hospitals, as the study excluded members of safety-net populations who also have the highest rates of disability, including residents of nursing homes,47 persons with severe dementia,48 and people without access to telephones, many of whom were homeless.49 We did not include measures of cognitive status in our models, as cognition was not assessed prior to hospital admission, and chart diagnoses of cognitive impairment frequently underestimate its true prevalence.50 Admission diagnoses for participants were not collected. However, comorbid conditions were collected using ICD-9 codes extracted from administrative data recorded during hospital admission and are reported instead. Because this study was conducted at a single safety-net hospital, its findings may not be generalizable to other hospitals.
In conclusion, our findings show that pre-admission functional disability is common in community-dwelling adults aged 55 and older admitted to a safety-net hospital. Patients aged 55 and older admitted to safety-net hospitals may benefit from models of acute care, such as ACE units, that prevent adverse outcomes associated with functional disability. As the correlates of disability differ by age, hospital-based interventions may need to be adapted to meet the unique needs of patients in late middle age.
Acknowledgments
This study was presented as a poster at the Society for General Internal Medicine 36th Annual Meeting on April 24, 2013 in Denver, Colorado, and at the American Geriatrics Society 2013 Annual Scientific Meeting on May 3, 2013 in Grapevine, Texas.
Funding sources and related paper presentations: Funding sources and related paper presentations: This work was funded in part by the Gordon and Betty Moore Foundation (Mr. Guzman and Drs. Kessell, Goldman, Sarkar, Schneidermann, Critchfield, and Kushel), by grant K23 AG045290 from the National Institute on Aging at the National Institutes of Health (Dr. Brown), by grant KL2TR000143 from the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-Clinical and Translational Sciences Institute (Dr. Brown), by grant T32 AG000212 from the National Institute on Aging at the National Institutes of Health (Dr. Brown), and by grant P30AG044281 from the National Institute on Aging at the National Institutes of Health (Dr. Brown). These funding sources had no role in the preparation, review, or approval of the manuscript. Dr. Brown is an employee of the VA medical Center. The opinions expressed in this manuscript may not represent those of the Department of Veterans Affairs.
Sponsor's Role: The funding sources had no role in the design or conduct of the study; in the collection, analysis, or interpretation of the data; in the preparation, review, or approval of the manuscript; or in the decision to submit the manuscript for publication.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Dr. Pierluissi is Medical Director of the Acute Care for Elders Unit at the San Francisco General Hospital and Trauma Center.
Author Contributions: Drs. Brown and Kushel had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Brown, Pierluissi, Kushel.
Acquisition of data: Kessell, Goldman, Sarkar, Schneidermann, Critchfield, Kushel.
Statistical analysis: Guzman.
Analysis and interpretation of data: Brown, Pierluissi, Guzman, Kessell, Goldman, Sarkar, Schneidermann, Critchfield, Kushel.
Drafting of the manuscript: Brown, Kushel.
Critical revision of the manuscript for important intellectual content: Brown, Pierluissi, Guzman, Kessell, Goldman, Sarkar, Schneidermann, Critchfield, Kushel.
References
- 1.Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I'm not sure”. JAMA. 2011;306:1782–1793. doi: 10.1001/jama.2011.1556. [DOI] [PubMed] [Google Scholar]
- 2.Inouye SK, Wagner DR, Acampora D, et al. A predictive index for functional decline in hospitalized elderly medical patients. J Gen Intern Med. 1993;8:645–652. doi: 10.1007/BF02598279. [DOI] [PubMed] [Google Scholar]
- 3.Sager MA, Franke T, Inouye SK, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med. 1996;156:645–652. [PubMed] [Google Scholar]
- 4.Mehta KM, Pierluissi E, Boscardin WJ, et al. A clinical index to stratify hospitalized older adults according to risk for new-onset disability. J Am Geriatr Soc. 2011;59:1206–1216. doi: 10.1111/j.1532-5415.2011.03409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fortinsky RH, Covinsky KE, Palmer RM, et al. Effects of functional status changes before and during hospitalization on nursing home admission of older adults. J Gerontol A Biol Sci Med Sci. 1999;54:M521–526. doi: 10.1093/gerona/54.10.m521. [DOI] [PubMed] [Google Scholar]
- 6.Fried LP, Guralnik JM. Disability in older adults: Evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997;45:92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- 7.Covinsky KE, Palmer RM, Counsell SR, et al. Functional status before hospitalization in acutely ill older adults: Validity and clinical importance of retrospective reports. J Am Geriatr Soc. 2000;48:164–169. doi: 10.1111/j.1532-5415.2000.tb03907.x. [DOI] [PubMed] [Google Scholar]
- 8.Minkler M, Fuller-Thomson E, Guralnik JM. Gradient of disability across the socioeconomic spectrum in the United States. N Engl J Med. 2006;355:695–703. doi: 10.1056/NEJMsa044316. [DOI] [PubMed] [Google Scholar]
- 9.Martin LG, Freedman VA, Schoeni RF, et al. Trends in disability and related chronic conditions among people ages fifty to sixty-four. Health Aff (Millwood) 2010;29:725–731. doi: 10.1377/hlthaff.2008.0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Institute of Medicine. America's Health Care Safety Net: Intact but Endangered. Washington, D.C.: National Academies Press; 2000. [PubMed] [Google Scholar]
- 11.Hall MJ, DeFrances CJ, Williams SN, et al. National Hospital Discharge Survey: 2007 summary. Natl Health Stat Report. 2010;29:1–20. 24. [PubMed] [Google Scholar]
- 12.National Association of Public Hospitals and Health Systems. America's safety net hospitals and health systems, 2010: Results of the annual NAPH hospital characteristics survey. [Accessed June9, 2014]; http://essentialhospitals.org/wp-content/uploads/2013/12/NPH214.pdf.
- 13.San Francisco Department of Public Health. San Francisco General Hospital and Trauma Center. [Accessed June9, 2014]; http://www.sfdph.org/dph/comupg/oservices/medSvs/sfgh/default.asp.
- 14.Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged: The index of ADL. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 15.Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 16.Sarkar U, Schillinger D, Lopez A, et al. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J Gen Intern Med. 2011;26:265–271. doi: 10.1007/s11606-010-1552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kushel MB, Gupta R, Gee L, et al. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21:71–77. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 20.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 21.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction. 2002;97:1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- 23.Stuck AE, Walthert JM, Nikolaus T, et al. Risk factors for functional status decline in community-living elderly people: Asystematic literature review. Soc Sci Med. 1999;48:445–469. doi: 10.1016/s0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- 24.McCusker J, Kakuma R, Abrahamowicz M. Predictors of functional decline in hospitalized elderly patients: Asystematic review. J Gerontol A Biol Sci Med Sci. 2002;57:M569–577. doi: 10.1093/gerona/57.9.m569. [DOI] [PubMed] [Google Scholar]
- 25.Landefeld CS, Palmer RM, Kresevic DM, et al. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338–1344. doi: 10.1056/NEJM199505183322006. [DOI] [PubMed] [Google Scholar]
- 26.Spector WD, Katz S, Murphy JB, et al. The hierarchical relationship between activities of daily living and instrumental activities of daily living. J Chronic Dis. 1987;40:481–489. doi: 10.1016/0021-9681(87)90004-x. [DOI] [PubMed] [Google Scholar]
- 27.Kempen GI, Myers AM, Powell LE. Hierarchical structure in ADL and IADL: Analytical assumptions and applications for clinicians and researchers. J Clin Epidemiol. 1995;48:1299–1305. doi: 10.1016/0895-4356(95)00043-7. [DOI] [PubMed] [Google Scholar]
- 28.Ferrucci L, Guralnik JM, Cecchi F, et al. Constant hierarchic patterns of physical functioning across seven populations in five countries. Gerontologist. 1998;38:286–294. doi: 10.1093/geront/38.3.286. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Census Bureau. Americans with Disabilities: 2010. Washington, DC: U.S. Census Bureau; 2012. [Google Scholar]
- 30.Mendes de Leon CF, Fillenbaum GG, Williams CS, et al. Functional disability among elderly blacks and whites in two diverse areas: The New Haven and North Carolina EPESE. Am J Public Health. 1995;85:994–998. doi: 10.2105/ajph.85.7.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kington RS, Smith JP. Socioeconomic status and racial and ethnic differences in functional status associated with chronic diseases. Am J Public Health. 1997;87:805–810. doi: 10.2105/ajph.87.5.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clark DO. US trends in disability and institutionalization among older Blacks and Whites. Am J Public Health. 1997;87:438–440. doi: 10.2105/ajph.87.3.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nuru-Jeter AM, Thorpe RJ, Jr, Fuller-Thomson E. Black-white differences in self-reported disability outcomes in the U.S.: Early childhood to older adulthood. Public Health Rep. 2011;126:834–843. doi: 10.1177/003335491112600609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cordasco KM, Asch SM, Franco I, et al. Health literacy and English language comprehension among elderly inpatients at an urban safety-net hospital. J Health Hum Serv Adm. 2009;32:30–50. [PubMed] [Google Scholar]
- 35.Gaskin DJ, Hadley J. Population characteristics of markets of safety-net and non-safety-net hospitals. J Urban Health. 1999;76:351–370. doi: 10.1007/BF02345673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mold JW, Fryer GE, Thomas CH. Who are the uninsured elderly in the United States? J Am Geriatr Soc. 2004;52:601–606. doi: 10.1111/j.1532-5415.2004.52169.x. [DOI] [PubMed] [Google Scholar]
- 37.Thomson EF, Nuru-Jeter A, Richardson D, et al. The Hispanic Paradox and older adults' disabilities: Is there a healthy migrant effect? Int J Environ Res Public Health. 2013;10:1786–1814. doi: 10.3390/ijerph10051786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: An updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 39.House JS, Kessler RC, Herzog AR. Age, socioeconomic status, and health. Milbank Q. 1990;68:383–411. [PubMed] [Google Scholar]
- 40.Herd P. Do functional health inequalities decrease in old age? Educational status and functional decline among the 1931-1941 birth cohort. Res Aging. 2006;28:375–392. [Google Scholar]
- 41.Adler NE, Stewart J. Health disparities across the lifespan: Meaning, methods, and mechanisms. Ann N Y Acad Sci. 2010;1186:5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- 42.Ventura SJ, Peters KD, Martin JA, et al. Births and deaths: United States, 1996. Month Vital Stat Rep. 1997;46(1 suppl 2):1–40. [PubMed] [Google Scholar]
- 43.McGinnis JM, Foege WH. Mortality and morbidity attributable to use of addictive substances in the United States. Proc Assoc Am Physicians. 1999;111:109–18. doi: 10.1046/j.1525-1381.1999.09256.x. [DOI] [PubMed] [Google Scholar]
- 44.Ng TP, Niti M, Chiam PC, et al. Physical and cognitive domains of the Instrumental Activities of DailyLiving: Validation in a multi ethnic population of Asian older adults. J Gerontol A Biol Sci Med Sci. 2006;61:726–735. doi: 10.1093/gerona/61.7.726. [DOI] [PubMed] [Google Scholar]
- 45.Tennant A, Penta M, Tesio L, et al. Assessing and adjusting for cross-cultural validity of impairment and activity limitation scales through differential item functioning within the framework of the Rasch model: The PRO-ESOR project. Med Care. 2004;42(1 Suppl):I37–148. doi: 10.1097/01.mlr.0000103529.63132.77. [DOI] [PubMed] [Google Scholar]
- 46.Beaton DE, Bombardier C, Guillemin F, et al. Recommendations for the Cross-Cultural Adaptation of Health Status Measures. Rosemont (IL): American Academy of Orthopedic Surgeons; 2002. [Google Scholar]
- 47.Jones AL, Dwyer LL, Bercovitz AR, et al. The National Nursing Home Survey: 2004 overview. Vital Health Stat. 2009;13:1–155. [PubMed] [Google Scholar]
- 48.Agüero-Torres H, Fratiglioni L, Guo Z, et al. Dementia is the major cause of functional dependence in the elderly: 3-year follow-up data from a population-based study. Am J Public Health. 1998;88:1452–1456. doi: 10.2105/ajph.88.10.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brown RT, Kiely DK, Bharel M, et al. Geriatric syndromes in older homeless adults. J Gen Intern Med. 2012;27:16–22. doi: 10.1007/s11606-011-1848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Quan H, Parsons GA, Ghali WA. Validity of information on comorbidity derived from ICD-9-CCM administrative data. Med Care. 2002;40:675–685. doi: 10.1097/00005650-200208000-00007. [DOI] [PubMed] [Google Scholar]


