Abstract
Objectives
Functional abdominal pain (FAP) in youth is associated with substantial impairment in functioning and prior research has shown that overprotective parent responses can heighten impairment. Little is known about how a range of parental behaviors in response to their child’s pain (overprotection, minimizing and/or encouragement) interact with child coping characteristics (e.g., catastrophizing) to influence functioning in youth with FAP. In this study, it was hypothesized that the relationship between parenting factors and child disability would be mediated by children’s level of maladaptive coping (i.e., pain catastrophizing).
Methods
Seventy-five patients with FAP presenting to a pediatric pain clinic and their caregivers participated. Youth completed measures of pain intensity (Numeric Rating Scale), pain catastrophizing (Pain Catastrophizing Scale), and disability (Functional Disability Inventory). Caregivers completed measures of parent pain catastrophizing (Pain Catastrophizing Scale), and parent responses to child pain behaviors (Adult Responses to Child Symptoms: protection, minimizing, and encouragement/monitoring subscales).
Results
Increased functional disability was significantly related to higher child pain intensity, increased child and parent pain catastrophizing, and higher levels of encouragement/monitoring and protection. Parent minimization was not related to disability. Child pain catastrophizing fully mediated the relationship between parent encouragement/monitoring and disability and partially mediated the relationship between parent protectiveness and disability.
Conclusions
The impact of parenting behaviors in response to FAP on child disability is determined in part by the child’s coping style. Findings highlight a more nuanced understanding of the parent-child interaction in determining pain-related disability levels, which should be taken into consideration in assessing and treating youth with FAP.
Keywords: functional abdominal pain, pediatric, catastrophizing, parent responses
Functional abdominal pain (FAP) in children, is a set of recurrent pain conditions without an organic cause (1), is highly prevalent and can lead to substantial impairment including decreased involvement in social, academic, and other daily activities (2–4). Based on Rome-III criteria, subtypes of FAP include functional dyspepsia, irritable bowel syndrome, and abdominal migraine (1). Youth with FAP who have the greatest level of impairment may be characterized by anxiety, expressed as maladaptive thinking about pain, or other family risk factors (i.e., overprotective parenting) that are potentially modifiable with behavioral intervention (5).
Greater impairment has been associated with the child’s use of poor psychological coping strategies such as catastrophic thinking about pain [e.g., belief that pain will not resolve or get worse, (6)] as well as parental responses to pain, such as overprotection (i.e., checking in repeatedly about pain symptoms) or minimizing/criticism (7). Understanding how children develop maladaptive coping strategies in response to FAP involves recognition of the caregiving environment in which these coping behaviors develop (8). A recent community-based study found that the impact of child catastrophizing on disability was less pronounced in the context of high levels of adaptive parenting behaviors (e.g., promotion of children’s well behaviors) in generally healthy schoolchildren dealing with occasional pain (9). There is emerging evidence that the joint impact of parenting factors and child pain catastrophizing is relevant for understanding impairment in samples of youth with mixed chronic pain conditions (10, 11) and in youth with organic causes of abdominal pain, such as Inflammatory Bowel Disease (12)
Multiple studies in pediatric chronic pain have documented the impact of parenting factors in children’s adjustment to pain. For example, parent protection and criticism have been implicated in predicting disability in youth with an array of chronic pain conditions (13–15) and more specifically in children with FAP (16–20). Some research suggests that parental overprotectiveness (i.e., limiting the child’s normal activities and/or giving the child special attention secondary to pain) and/or minimizing (i.e., criticism) uniquely influence FAP-related disability (16, 18) whereas other research did not find evidence of such relationships (20). Given the tendency for pain conditions to occur in families, it is conceivable that parents’ catastrophizing may be related to the expression of disability in youth with FAP, though this research has generally focused on the role of parent catastrophizing about their own pain versus their child’s pain (17), though there are several recent exceptions (12, 21). In youth with Inflammatory Bowel Disease, parent catastrophizing about their child pain partially explained the relationship between child pain behavior and parental protective responses; however, the relationship between these factors and child impairment was not examined (12). Yet another recent investigation has found support for the role of child pain catastrophizing underlying the association between parent catastrophizing about their child’s pain and pain related disability in a school-based sample of adolescents (21). However, it is unclear if child pain catastrophizing is related to disability in the presence of other parental responses to child pain (i.e., overprotection, criticism, or symptom monitoring) in youth with FAP. Thus, investigating multiple parenting behaviors can be beneficial to fully capture the range of responses that children with FAP may receive from their caregivers.
In general, models examining the simultaneous influence of child and parenting factors in predicting impairment in youth with chronic pain have focused on mixed pediatric pain samples, youth with IBD, or healthy controls and have shown mixed results (10, 13, 15, 22, 23), with some support that catastrophizing may mediate the relationship between parenting factors and disability, particularly in youth with chronic musculoskeletal pain (10, 15). Guite and colleagues also found that child pain catastrophizing may account for the relationship between pain intensity and disability (10); thus, it may be valuable to examine if these variables operate similarly in youth with FAP. Thus, the purpose of this study is to examine how pain catastrophizing in children and parental responses to their child’s pain interact to affect disability in a clinical sample of youth with FAP. We predict that child pain catastrophizing will mediate the relationship between parental responses to pain (i.e., protectiveness, encouragement/symptom monitoring, and minimization) and disability, consistent with prior literature. We also investigated the role of child pain catastrophizing in mediating the relationship between pain intensity and disability to assess whether these factors operate similarly in predicting disability in our sample as compared to prior research in youth with musculoskeletal pain (10). We undertook exploratory analysis examining the role of parent pain catastrophizing about the child’s pain in relation to parent responses to pain and disability. This project is the first part of an ongoing research program in developing tailored interventions for youth with FAP and their caregivers.
Materials and Methods
Participants
Participants were youth and their parent/s presenting to a multidisciplinary pediatric pain clinic between July 2010 and March 2014. Participants completed a set of questions as part of a broader research study examining psychosocial factors in youth with chronic pain for which they provided informed consent/assent (see procedures section for additional information). Approximately 70% of youth and their families presenting to pain clinic agreed to participate in the study. Of the 441 patients who were recruited from a broad pediatric pain sample, 75 patients who were diagnosed with FAP and their parents, typically mothers, were included in the current study (See Figure 1). Inclusion criteria were: patients between the ages of 8 and 18; a primary complaint of chronic or recurrent abdominal pain of functional, or likely functional (i.e., cause unknown after medical evaluation) etiology; patient and parent ability to read and comprehend written English. Patients were ineligible for participation if they had an organic cause of pain such as Inflammatory Bowel Disease, any other documented major pain complaints (i.e., neuropathic pain, wide-spread musculoskeletal pain), pain for less than 2 months, or significant developmental delays or impairments. Patients were primarily referred by their other pediatric subspecialty clinics such as gastroenterology or their primary care providers.
Figure 1. Study Flow Diagram.
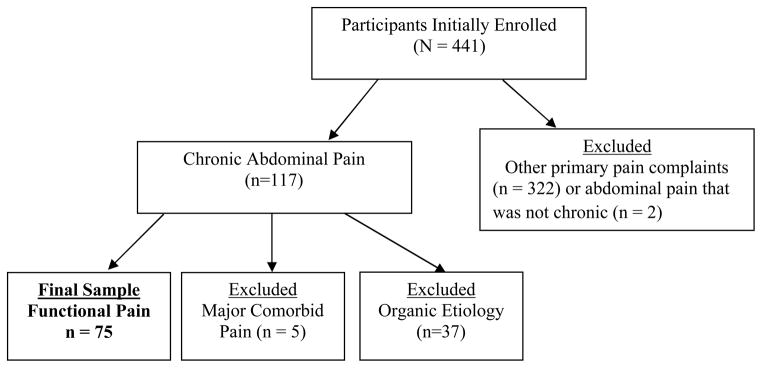
Note. Patients enrolled from July 2010 to April 2014; Major Comorbid Pain includes widespread musculoskeletal pain and neuropathic pain. Chronic abdominal pain is defined as pain onset for 2 months or greater.
Procedures
Patients and their families were invited to participate in an optional research study during their initial visit at a multidisciplinary pain center. If agreeable, consent and assent were obtained by research staff prior to completion of any measures. Patients then completed a battery of measures assessing a wide range of psychological variables, as a part of a larger Institutional Review Board (IRB) approved protocol aimed at investigating psychosocial factors related to chronic pain in a pain management clinic. Research pertaining to this broader pediatric pain sample has been published in previous investigations examining the impact of child and parent pain catastrophizing on pain, functioning, and pain behavior (24).
Measures
Demographic Information
Detailed demographic and background information including race, ethnicity, age, gender, and socioeconomic status were collected from caregivers, as well as parent pain history (number of pain conditions endorsed on a checklist).
Numeric Rating Scale (NRS) Pain Intensity
The NRS pain rating scale assesses average child-reported pain intensity (0–10 scale) over the last two weeks, with “0” indicating no pain, and “10” reflecting worst possible pain. This measure was used as a predictor variable in the current study. The NRS pain intensity scale has been validated in pediatric pain samples and is recommended for use in clinical studies of pain in school-age children (25).
Functional Disability Inventory-child report (FDI-C)
The FDI is a validated measure which assesses physical functioning and difficulty completing activities due to pain (26, 27). Response to items are categorized via 5-point Likert scale, from 0 (no trouble) to 4 (impossible), and are summed to create a total disability score. Scores range from 0–60, with 0–12 indicating no/minimal disability, 13–29 indicating moderate disability, and 30 or higher indicating severe disability (28). The Cronbach’s alpha indicating internal consistency reliability for the current sample was 0.92
Pain Catastrophizing Scales Child and Parent Versions (PCS-C/P)
The child and parent versions of the PCS each contain 13 items related to thoughts and feelings about pain experienced by the child (PCS-C) or by the parent (PCS-P) when the child is in pain. Response items range from not at all (0), mildly (1), moderately (2), severely (3), and extremely (4). Total scores range from 0–52, with higher scores reflecting greater catastrophizing. Subscales on the PCS include rumination, magnification, and helplessness. Total catastrophizing scores were used for analyses in this study. The PCS-C/P have been validated in pediatric pain samples (29, 30). Cronbach’s alphas in the current sample were 0.93 (PSC-C) and 0.93 (PSC-P).
Adult Responses to Children’s Symptoms (ARCS)
The ARCS is a 29-item measure that assesses parent-reported reactions to children’s pain. Item responses that range on a 5-point Likert scale, from 0 (Never) to 4 (Always), are summed to create subscale scores falling into three categories: Protect (placing the child in a passive or sick role), Minimize (punitive or critical responses to the child’s pain), and Encourage and Monitor (having the child engage in normal activities while monitoring symptom intensity). This measure has been validated in pediatric pain samples (31). Cronbach’s alphas in the current sample were 0.83 for Protect, 0.73 for Minimize, and 0.76 for Encourage/Monitor, consistent with the internal consistencies reported in the validation study.
Statistical Analysis
Data were analyzed using SPSS 22.0 for descriptive statistic and Mplus 7.20 for correlational analysis and for constructing mediation models (32). Missing data ranged from 1.3% to 22.7% and was handled with maximum likelihood parameter estimation using 3–6 missing data auxiliary correlate variables to increase the likelihood of the missing at random (MAR) assumption being met (33). First, descriptive data were computed for all demographic variables and measures of pain, functional disability, pain catastrophizing, and adult responses to children’s symptoms. Bivariate correlations were conducted to examine the relationship between child reported disability and pain intensity, child/parent pain catastrophizing, and parental responses to child pain (i.e. protect, minimize, encouragement/monitor). Next, we constructed a single mediation model in which parent reported responses to child pain and child pain intensity were linked directly with functional disability and indirectly via child pain catastrophizing to test our hypothesis that child pain catastrophizing would mediate the relationship between parenting factors/pain intensity and disability (See Figure 2). The following empirically supported fit indices were used to determine optimal model fit: model chi-square values with p>0.05, RMSEA values <0.06, SRMR values <0.08, CFI values >0.95, and TLI values > 0.90. (34) All path models demonstrated adequate fit based on the above criteria. We examined the significance of each path in the models. To test the significance of the indirect effects associated with the mediator, we used bias correction and bootstrapping [n = 5000 bootstrap resamples, (35)] which reduces the probability of type 1 error. A 90% confidence interval (CI) around the joint (a* β) indirect pathway that does not include zero represents significant mediation. We used a 90% confidence interval rather than a 95% confidence error in order to reduce type II error. Finally, to determine the degree to which child pain catastrophizing serves as a mechanism linking parenting factors and functional disability, we calculated the percentage of variance in the relation between parenting factors and functional disability accounted for by catastrophizing (36). In other words, we calculated how much of parental responses to pain could be explained by the variability in children’s catastrophic thinking about pain.
Figure 2.
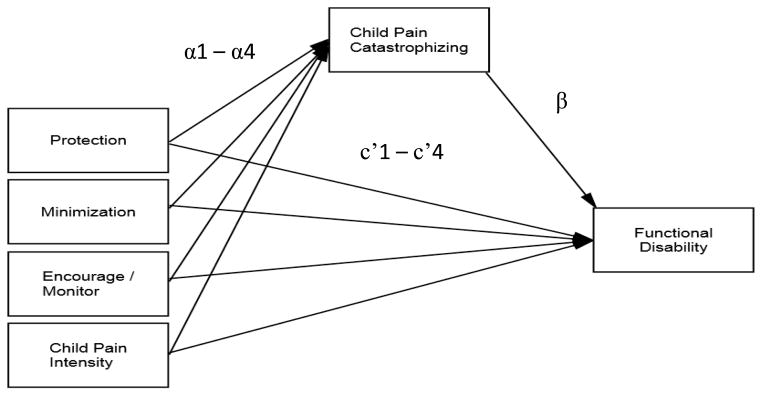
Catastrophizing mediates the relationship between parental responses to pain, pain intensity, and child disability
For our exploratory analysis, we also examined parent pain catastrophizing as a mechanism underlying the relationship between pain responses to pain and child disability.
Results
Patient Characteristics
The sample consisted of 75 patients (ages 9 to 18, mean=13.84, SD=2.62) seen in a multidisciplinary pediatric pain clinic and diagnosed with FAP. The majority of the patients were female and Caucasian (see Table 1 for additional sociodemographic information). This patient profile parallels those reported in prior studies of youth with FAP (19). The majority of parent informants were mothers. On average, parent informants reported a lifetime history of 3.75 (SD = 2.75) prior pain complaints (i.e., headache, back pain). Pain duration, patient sex, parent pain history, and patient age were not significantly associated with outcome variables. The sample was characterized by moderate levels of pain and disability (See Table 2).
Table 1.
Sample Characteristics (n = 75)
| Age | ||
|---|---|---|
| Mean | SD | |
| N | % | |
| Sex (female) | 58 | 77.3 |
| Ethnicity (white) | 62 | 82.7 |
| Parent Reporter (Mother) | 63 | 84 |
| Pain Duration | N | % |
| < 3 months | 10 | 13.3 |
| 3–6 months | 15 | 20.0 |
| 7–11 months | 8 | 10.7 |
| 1–3 years | 28 | 37.3 |
| > 3 years | 14 | 18.7 |
| Pain Category | ||
| Functional Dyspepsia | 34 | 45.3 |
| Irritable Bowel Syndrome | 14 | 18.7 |
| Other functional abdominal pain | 27 | 36.0 |
Note. Patients with pain less than 3 months had pain symptoms for at least 2 months.
Table 2.
Descriptive data and correlations of pain, catastrophizing, parent pain responses, and disability
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | Mean | SE | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Pain Intensity (0–10) | - | 5.48 | 0.25 | ||||||
| 2. Child Pain Catastrophizing (0–52) | .44** | - | 14.89 | 1.18 | |||||
| 3. Parent Pain Catastrophizing (0–52) | .46** | .51** | - | 27.31 | 1.37 | ||||
| 4. Encourage/Monitor (0–4) | .13 | .34* | .43** | - | 2.93 | 0.07 | |||
| 5. Minimize (0–4) | −.14 | −.02 | −.01 | −.19 | - | 0.68 | 0.07 | ||
| 6. Protection (0–4) | .24^ | .43** | .49** | .46** | .00 | - | 1.65 | 0.07 | |
| 7. Functional Disability (0–60) | .44** | .53** | .29* | .31* | .07 | .48** | - | 19.60 | 1.44 |
Note. (range),
p < 0.001,
p < 0.01,
p < 0.05.
Relationship between pain intensity, catastrophizing, and parent responses of pain to disability
As shown in Table 2, bivariate correlations suggest increased functional disability was significantly related to higher child pain intensity, higher levels of parent protection, higher level of parent encouragement/monitoring, increased child pain catastrophizing, and increased parent paincatastrophizing (all p’s <0.05). There was no direct relationship between parent minimizing responses and disability.
Mediation Analysis
We tested a mediated path analysis (Figure 2) consisting of the direct and indirect associations among parenting pain responses, pain intensity and functional disability (Table 3).
Table 3.
Child pain catastrophizing as a mediator of independent variables (parent pain responses and pain intensity) and disability
| IV | M | DV | IV on M (Path a) | M on DV (Path b) | Indirect Effect (a × b) | Direct Effects (Path c′) | |||
|---|---|---|---|---|---|---|---|---|---|
| Est b (β) | SE | Est b (β) | SE | Est b (β) | (90% CI) | Est b (β) | |||
| Parent pain behaviors | |||||||||
| Encourage/Monitor | Catastrophizing | FDI | 3.10(0.18) | 1.72† | 0.33(0.28) | 0.19† | 1.03(0.05) | (0.12, 3.79) | 1.64(0.80) |
| Minimization | Catastrophizing | FDI | 1.10 (0.06) | 1.75 | 0.33(0.28) | 0.19† | 0.37(0.02) | (−0.30, 2.03) | 2.23(0.11) |
| Protection | Catastrophizing | FDI | 4.62(0.26) | 2.14^ | 0.33(0.28) | 0.19† | 1.54(0.07) | (0.10, 4.17) | 5.14(0.25)† |
| Child Pain Intensity | Catastrophizing | FDI | 1.67(0.36) | 0.49** | 0.33(0.28) | 0.19† | 0.56(0.10) | (0.06, 1.38) | 1.56(0.28)^ |
Note.
p < 0.001,
p<0.01,
p < 0.05.
p<0.10.
Parent Protection
Increased parental protection in response to child pain was associated with higher child pain catastrophizing. Further, the indirect path between higher parent protectiveness and higher child reported disability associated with pain was significant (αβ = 1.54; 90% CI = [0.10, 4.17]). In the presence of catastrophizing as a mediator, the direct effect of parental protectiveness on child reported disability remained significant (i.e., c′ =5.14, p < .10). Thus, child pain catastrophizing partially mediated the relationship between child pain intensity and child disability. The indirect effect of child pain catastrophizing in this model explained 23% of the variance of the association between parent protectiveness and child reported functional disability.
Parent encouragement/Monitoring
Increased parental encouragement/monitoring was associated with higher child pain catastrophizing. The indirect path between higher parent encouragement/monitoring and higher child reported disability associated with pain was significant (αβ = 1.03; 90% CI = [.12, 3.79]). In the presence of catastrophizing as a mediator, the direct effect of parental encouragement/monitoring on child reported disability was not significant (i.e., c′ = 1.64, p = .55). Thus, child pain catastrophizing fully mediated the relationship between parent encouragement/monitoring and child disability. The indirect effect of child pain catastrophizing in this model explained 39% of the variance of the association between parent encouragement/monitoring and functional disability.
Parent Minimization
Child pain catastrophizing was not found to mediate the relationship between parent minimization and disability.
Pain Intensity
We also examined the role of child pain catastrophizing in the relationship between pain intensity and disability. Increased pain intensity was associated with higher child pain catastrophizing, and the indirect path between higher pain intensity and higher child reported disability was significant (αβ = 0.56; 90% CI = [.06, 1.38]). In the presence of child pain catastrophizing as a mediator, the direct effect of pain intensity on child reported disability remained significant (i.e., c′ = 1.56, p < 0.05). Thus, child pain catastrophizing was a partial mediator of pain and disability and accounted for 26% of the variation in the association between child reported pain intensity and disability. These findings are consistent with prior research in youth with chronic musculoskeletal pain (10),
Exploratory Analysis
Parent pain catastrophizing about the child’s pain was not found to be a significant mediator of parent responses to pain (protection, minimization, encouragement/monitoring) and disability.
Discussion
The purpose of this study was to examine the relationship between parental responses to pain (protection, minimize, encouragement/monitor) as well as the role of catastrophizing (both parent and child) in accounting for impairment in youth with FAP. Parental responses (specifically protective parental responses) and pain catastrophizing have previously been examined in relation to impairment in mixed samples of youth with chronic pain conditions (10, 11, 15), school-based samples (21) and in youth with organic causes of abdominal pain, such as Inflammatory Bowel Diseases (12). However, examining the role of pain catastrophizing in relation to multiple parent responses (including protection, minimizing and encouragement/ monitoring) in youth with FAP has not previously been investigated. It is valuable to examine youth with FAP in particular, given that FAP is a common pediatric pain condition (37) in which parent factors have been well-studied and are known to influence outcomes (5, 16–18). Further, physicians often encounter this pain complaint and observe an array of parenting styles as families try to cope with and manage symptom-related impairment. Whereas past studies have focused on parent and child factors separately, it is now recognized that the interaction between various parent responses and child characteristics or behaviors (such as the interaction between protectiveness and/or encouragement/monitoring and child pain catastrophizing) may be more important in determining functional outcomes than any single factor alone (9, 10). Certainly, the parent-child dyadic response to pain is important including the context of the parenting environment and the coping characteristics of the child.
A unique contribution of this study is the finding that child pain catastrophizing fully accounts for the relationship between parent support/monitoring of pain symptoms and child disability. Thus, even in the presence of a conceptually adaptive parent response to pain (i.e., encouragement of well behaviors), the impact on a child who is prone to pain catastrophizing may lead to increased impairment in youth with FAP regardless of how presumably adaptive the parental response. These findings suggest that parental encouragement/monitoring is not necessarily adaptive for children who remain vigilant and anxious about their symptoms. For these children, any additional monitoring or attention may still signal that something is wrong. It is noteworthy that parent encouragement of activities while monitoring pain symptoms is also directly linked to higher levels of child disability. This may be because the monitoring of pain symptoms may exacerbate attention to pain and inadvertently increase or maintain disability. By monitoring pain symptoms, the parent may unintentionally confirm to the already anxious child that there is something bad that needs to be watched or monitored, as also seen in the parent protective response to pain. Support for this hypothesis is noted in the significant correlation between protection and support/monitoring.
Our study also found that the influence of parental protectiveness on disability is influenced in part by child catastrophizing in youth with FAP, which is consistent with results from two recent studies in samples of youth with chronic musculoskeletal pain (10, 15). In other words, an overprotective parental response to pain was more likely to be associated with increased disability when the child had a catastrophic coping response to pain. One might speculate about the reasons for this type of dyadic interaction and how it works to affect disability. For example, it is possible that the child’s maladaptive coping in the form of increased worry and anxiety may create a level of child distress that parents find inherently difficult to ignore and thereby elicit natural but ultimately counterproductive protective responses from the parent (6). Alternatively, parent protectiveness (and the attention to symptoms that it likely promotes) may increase catastrophic thinking about pain in their children, which in turn may promote increased disability.
Our analyses also indicated that child pain catastrophizing also partially accounted for the relationship between child pain intensity and disability in youth with FAP. That is, increased pain may exacerbate maladaptive cognitions about pain, which in turn disrupts functioning for youth with functional abdominal pain. These findings are consistent with a prior investigation of youth with musculoskeletal pain (10) and allow for some confidence in generalizing the results of this investigation to youth with functional abdominal pain more broadly in spite of a relatively small (n = 75) sample size.
These findings add to the literature by providing additional support to the idea of a more complex relationship between child pain catastrophizing and parental responses to pain in relation to disability in youth with FAP. These findings may begin to disentangle the emotional and behavioral interplay between parent and child observed by physicians, and validate their clinical impressions that some of these families may have a difficult recovery from FAP given the complexity of the family dynamics. Thus, these findings suggest a complex parent-child dynamic may serve as an indicator for physicians that the family may benefit from psychosocial support to improve their coping/adjustment. While parent pain catastrophizing and parent pain history may be important to consider, we did not find clear evidence that they served as meaningful mechanisms underlying the relationship between parent responses to pain and child functioning. Further study of parent catastrophizing about their own pain and how they cope with their own pain is needed to more fully understand the drivers of parental behaviors towards their child’s pain, while taking into account the child’s tendency for catastrophic thinking.
Results should be interpreted in the context of a few limitations to the current study. First, this investigation is a cross sectional study and therefore a true predictive model could not be tested. Second, other psychological variables such as a broad measure of child anxiety which have been shown to have a significant relationship to disability in youth with FAP (5) were not available for examination in the current study. However, it should be noted that pain catastrophizing can be considered a cognitive expression of anxiety, which reduces concern that a significant factor has been entirely overlooked. Additionally, the patients in this study presented to a pediatric pain clinic, and thus may not completely represent youth with FAP in community settings, primary care, or other specialized medical settings. Instead, the patients in the current investigation may represent the most complex of youth with FAP as they did not respond to conventional treatment and may be likely to be the most highly distressed. Finally, we did not collect data on other sites of pain (e.g., co-occurring headaches, muscle pain, etc.) which may be useful to examine in future research. Also of note, we relied primarily on maternal report of parenting factors in the current investigation. Examination of other parent pain factors, such as parent disability or fear of their own pain, may be beneficial.
Based on these results, it may be useful to screen patients with FAP and their families during medical office visits, specifically for parent responses to pain and especially child pain catastrophizing. The tools required for screening are brief and may be readily incorporated into a busy medical setting (See Table 4 for links to study measures). Such screening could highlight those patients and parents with higher levels of distress and overprotection or excessive focus on pain symptom monitoring that may predispose the patient to increased disability. The benefits of early screening for maladaptive parenting factors in youth with FAP are consistent with other pediatric pain (i.e., juvenile fibromyalgia) investigations, which have suggested that a controlling family environment may be related to poor outcomes in adulthood (38). Early identification of families at higher risk for child disability may streamline and enhance care by guiding care plans towards educational or behavioral interventions designed to alter a potentially vicious cycle that may lead to increasing disability in youth over time. In addition, as the current investigation focused primarily on maternal reports of child functioning, future research in this area should aim to examine the role of both mothers and fathers, the congruence between their parenting styles and the influence on the child’s pain related disability. It may be that the fathers’ parenting style could dampen or magnify the effect on child catastrophizing. Additionally, the role of parenting factors that were associated with disability in our correlation analyses, such as encouragement/monitoring and parent pain catastrophizing, may warrant additional attention in future research.
Table 4.
Links to study measures
| Measure Title | Link |
|---|---|
| Adult Responses to Child Symptoms | http://www.ncbi.nlm.nih.gov/pubmed/20473048 |
| Pain Catastrophizing Scale-Child/Parent Versions | http://www.midss.org/content/pain-catastrophizing-scale-child-version-and-parent-version |
| Functional Disability Inventory, Child Version | http://www.commondataelements.ninds.nih.gov |
It may be beneficial for medical providers to refer families to a psychologist with a specialty in pediatric behavioral medicine/pediatric pain who can address parental behaviors as well as teach the child adaptive pain coping skills in an effort to reduce disability and facilitate return to normal activities. In a similar vein, these findings may be important for ultimately developing tailored treatments for patients and their families to optimize outcomes for these youth. Current psychological treatments for pediatric pain teach a blend of cognitive and behavioral strategies to reduce the child’s maladaptive coping (i.e., child pain catastrophizing) (39). While parent behaviors are usually addressed in a general fashion, targeting the dyadic interaction of parent responses to pain (i.e., protectiveness and pain symptom monitoring) while specifically taking into account the child’s level of catastrophizing may be an important consideration in promoting positive outcomes for youth with FAP.
Acknowledgments
Preparation of this paper was supported in part by NIH grant # K24 AR056687, a midcareer mentorship award to the last author (Kashikar-Zuck).
References
- 1.Drossman DA, Dumitrascu DL. Rome III: New standard for functional gastrointestinal disorders. Journal of Gastrointestinal and Liver Diseases. 2006;15(3):237–41. [PubMed] [Google Scholar]
- 2.Campo JV, Di Lorenzo C, Chiappetta L, Bridge J, Colborn DK, Gartner JC, Jr, et al. Adult outcomes of pediatric recurrent abdominal pain: do they just grow out of it? Pediatrics. 2001;108(1):E1. doi: 10.1542/peds.108.1.e1. [DOI] [PubMed] [Google Scholar]
- 3.Campo JV, Bridge J, Ehmann M, Altman S, Lucas A, Birmaher B, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics. 2004;113(4):817–24. doi: 10.1542/peds.113.4.817. [DOI] [PubMed] [Google Scholar]
- 4.Claar RL, Walker LS. Functional assessment of pediatric pain patients: psychometric properties of the functional disability inventory. Pain. 2006;121(1–2):77–84. doi: 10.1016/j.pain.2005.12.002. Epub 2006/02/17. S0304-3959(05)00610-X [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cunningham NR, Lynch-Jordan A, Mezoff AG, Farrell MK, Cohen MB, Kashikar-Zuck S. Importance of Addressing Anxiety in Youth With Functional Abdominal Pain: Suggested Guidelines for Physicians. Journal of Pediatric Gastroenterology and Nutrition. 2013;56(5):469–74. doi: 10.1097/MPG.0b013e31828b3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17(1):52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Walker LS, Smith CA, Garber J, Claar RL. Appraisal and coping with daily stressors by pediatric patients with chronic abdominal pain. J Pediatr Psychol. 2007;32(2):206–16. doi: 10.1093/jpepsy/jsj124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palermo TM, Eccleston C. Parents of children and adolescents with chronic pain. Pain. 2009;146(1–2):15–7. doi: 10.1016/j.pain.2009.05.009. Epub 2009/06/02. S0304-3959(09)00273-5 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vervoort T, Huguet A, Verhoeven K, Goubert L. Mothers’ and fathers’ responses to their child’s pain moderate the relationship between the child’s pain catastrophizing and disability. Pain. 2011;152(4):786–93. doi: 10.1016/j.pain.2010.12.010. http://dx.doi.org/10.1016/j.pain.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Guite JW, McCue RL, Sherker JL, Sherry DD, Rose JB. Relationships among pain, protective parental responses, and disability for adolescents with chronic musculoskeletal pain: the mediating role of pain catastrophizing. Clin J Pain. 2011;27(9):775–81. doi: 10.1097/AJP.0b013e31821d8fb4. [DOI] [PubMed] [Google Scholar]
- 11.Sieberg CB, Williams SE, Simons LE. Do parent protective responses mediate the relation between parent distress and child functional disability among children with chronic pain? J Pediatri Psychol. 2011;36(9):1043–51. doi: 10.1093/jpepsy/jsr043. [DOI] [PubMed] [Google Scholar]
- 12.Langer SL, Romano JM, Mancl L, Levy RL. Parental catastrophizing partially mediates the association between parent-reported child pain behavior and parental protective responses. Pain Research & Treatment. 2014;2014:9. doi: 10.1155/2014/751097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simons LE, Claar RL, Logan DL. Chronic pain in adolescence: parental responses, adolescent coping, and their impact on adolescent’s pain behaviors. J Pediatr Psychol. 2008;33(8):894–904. doi: 10.1093/jpepsy/jsn029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Logan DE, Scharff L. Relationships between family and parent characteristics and functional abilities in children with recurrent pain syndromes: an investigation of moderating effects on the pathway from pain to disability. J Pediatr Psychol. 2005;30(8):698–707. doi: 10.1093/jpepsy/jsj060. [DOI] [PubMed] [Google Scholar]
- 15.Welkom JS, Hwang WT, Guite JW. Adolescent pain catastrophizing mediates the relationship between protective parental responses to pain and disability over time. J Pediatr Psychol. 2013;38(5):541–50. doi: 10.1093/jpepsy/jst011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walker LS, Levy RL, Whitehead WE. Validation of a measure of protective parent responses to children’s pain. Clinical Journal of Pain. 2006;22(8):712–6. doi: 10.1097/01.ajp.0000210916.18536.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Langer SL, Romano JM, Levy RL, Walker LS, Whitehead WE. Catastrophizing and Parental Response to Child Symptom Complaints. Child Health Care. 2009;38(3):169–84. doi: 10.1080/02739610903038750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Tilburg MA, Venepalli N, Ulshen M, Freeman KL, Levy R, Whitehead WE. Parents’ worries about recurrent abdominal pain in children. Gastroenterol Nurs. 2006;29(1):50–5. doi: 10.1097/00001610-200601000-00009. quiz 6–7. [DOI] [PubMed] [Google Scholar]
- 19.Walker LS, Garber J, Greene JW. Psychosocial correlates of recurrent childhood pain: a comparison of pediatric patients with recurrent abdominal pain, organic illness, and psychiatric disorders. J Abnorm Psychol. 1993;102(2):248–58. doi: 10.1037//0021-843x.102.2.248. [DOI] [PubMed] [Google Scholar]
- 20.Wendland M, Jackson Y, Stokes LD. Functional disability in paediatric patients with recurrent abdominal pain. Child Care Health Dev. 2010;36(4):516–23. doi: 10.1111/j.1365-2214.2010.01087.x. [DOI] [PubMed] [Google Scholar]
- 21.Wilson AC, Moss A, Palermo TM, Fales JL. Parent pain and catastrophizing are associated with pain, somatic symptoms, and pain-related disability among early adolescents. Journal Of Pediatric Psychology. 2013 doi: 10.1093/jpepsy/jst094. Epub December 24, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Claar RL, Baber KF, Simons LE, Logan DE, Walker LS. Pain coping profiles in adolescents with chronic pain. Pain. 2008;140(2):368–75. doi: 10.1016/j.pain.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peterson CC, Palermo TM. Parental reinforcement of recurrent pain: the moderating impact of child depression and anxiety on functional disability. J Pediatr Psychol. 2004;29(5):331–41. doi: 10.1093/jpepsy/jsh037. [DOI] [PubMed] [Google Scholar]
- 24.Lynch-Jordan AM, Kashikar-Zuck S, Szabova A, Goldschneider KR. The Interplay of Parent and Adolescent Catastrophizing and Its Impact on Adolescents’ Pain, Functioning, and Pain Behavior. Clin J Pain. 2013 doi: 10.1097/AJP.0b013e3182757720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGrath PJ, Walco GA, Turk DC, Dworkin RH, Brown MT, Davidson K, et al. Core outcome domains and measures for pediatric acute and chronic/recurrent pain clinical trials: PedIMMPACT recommendations. Journal of Pain. 2008;9(9):771–83. doi: 10.1016/j.jpain.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 26.Walker LS, Greene JW. The functional disability inventory: measuring a neglected dimension of child health status. J Pediatr Psychol. 1991;16(1):39–58. doi: 10.1093/jpepsy/16.1.39. [DOI] [PubMed] [Google Scholar]
- 27.Kashikar-Zuck S, Goldschneider KR, Powers SW, Vaught MH, Hershey AD. Depression and functional disability in chronic pediatric pain. Clin J Pain. 2001;17(4):341–9. doi: 10.1097/00002508-200112000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Kashikar-Zuck S, Flowers SR, Claar RL, Guite JW, Logan DE, Lynch-Jordan AM, et al. Clinical utility and validity of the Functional Disability Inventory (FDI) among a multicenter sample of youth with chronic pain. Pain. 2011;152(7):1600–7. doi: 10.1016/j.pain.2011.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goubert L, Eccleston C, Vervoort T, Jordan A, Crombez G. Parental catastrophizing about their child’s pain. The parent version of the Pain Catastrophizing Scale (PCS-P): a preliminary validation. Pain. 2006;123(3):254–63. doi: 10.1016/j.pain.2006.02.035. [DOI] [PubMed] [Google Scholar]
- 30.Crombez G, Bigttebier P, Eccleston C, Mascagni T, Mertens G, Goubert L, et al. The child version of the pain catastrophizing scale (PSC-C): a preliminary validation. Pain. 2003;104(3):639–46. doi: 10.1016/S0304-3959(03)00121-0. [DOI] [PubMed] [Google Scholar]
- 31.Van Slyke DA, Walker LS. Mothers’ responses to children’s pain. Clin J Pain. 2006;22(4):387–91. doi: 10.1097/01.ajp.0000205257.80044.01. [DOI] [PubMed] [Google Scholar]
- 32.Muthen B, Asparouhov T. Bayesian structural equation modeling: a more flexible representation of substantive theory. Psychol Methods. 2012;17(3):313–35. doi: 10.1037/a0026802. [DOI] [PubMed] [Google Scholar]
- 33.Enders CK. Applied missing data analysis. New York: Guilford; 2010. [Google Scholar]
- 34.MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–31. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 36.MacKinnon DP. Introduction to statistical mediation analysis. New York: Erlbaum; 2008. [Google Scholar]
- 37.Chitkara DK, Rawat DJ, Talley NJ. The epidemiology of childhood recurrent abdominal pain in Western countries: a systematic review. Am J Gastroenterol. 2005;100(8):1868–75. doi: 10.1111/j.1572-0241.2005.41893.x. [DOI] [PubMed] [Google Scholar]
- 38.Sil S, Lynch-Jordan A, Ting TV, Peugh J, Noll J, Kashikar-Zuck S. Influence of Family Environment on Long-Term Psychosocial Functioning of Adolescents With Juvenile Fibromyalgia. Arthritis Care & Research. 2013;65(6):903–9. doi: 10.1002/acr.21921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eccleston C, Palermo TM, de CWAC, Lewandowski A, Morley S, Fisher E, et al. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2012;12:CD003968. doi: 10.1002/14651858.CD003968.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]


