Abstract
Background
Although in-hospital cardiac arrest is common, little is known about readmission patterns and inpatient resource use among survivors of in-hospital cardiac arrest.
Methods and Results
Within a large national registry, we examined long-term inpatient utilization among 6972 adults ≥65 years who survived an in-hospital cardiac arrest. We examined 30-day and 1-year readmission rates and inpatient costs, overall and by patient demographics, hospital disposition (discharge destination), and neurological status at discharge. The mean age was 75.8 ± 7.0 years, 56% were men, and 12% were black. There were a total of 2005 readmissions during the first 30 days (cumulative incidence rate: 35 readmissions/100 patients [95% CI: 33–37]) and 8751 readmissions at 1 year (cumulative incidence rate: 185 readmissions/100 patients [95% CI: 177–190]). Overall, mean inpatient costs were $7,741 ± $2323 at 30 days and $18,629 ± $9411 at 1 year. Thirty-day inpatient costs were higher in patients of younger age (≥85 years: $6052 [reference]; 75–84 years: $7444 [adjusted cost ratio, 1.23 [1.06–1.42]; 65–74 years: $8291 [adjusted cost ratio, 1.37 [1.19–1.59]; both P<0.001]) and black race (whites: $7413; blacks: $9044; adjusted cost ratio, 1.22 [1.05–1.42]; P<0.001), as well as those discharged with severe neurological disability or to skilled nursing or rehabilitation facilities. These differences in resource use persisted at 1 year and were largely due to higher readmission rates.
Conclusion
Survivors of in-hospital cardiac arrest have frequent readmissions and high follow-up inpatient costs. Readmissions and inpatient costs were higher in certain subgroups, including patients of younger age and black race.
Keywords: cardiac arrest, cost, readmission, outcomes research
Among survivors of in-hospital cardiac arrest, little is known about their patterns of readmission and related inpatient resource use after hospital discharge. Although there are an estimated 200,000 in-hospital cardiac arrests annually in the U.S.,1 prior studies have focused on in-hospital outcomes due to the challenge of collecting longitudinal data on survivors. In a recent study, we were able to overcome this challenge and found that most survivors of in-hospital cardiac arrest remained alive at 1 year.2 However, whether cardiac arrest survivors experience multiple readmissions after hospital discharge and the principal reasons for readmissions remain unclear. Moreover, characterizing the prognostic impact of key clinical factors, such as race, sex, hospital disposition and neurological status at discharge, on readmission and inpatient resource use patterns would provide insights into potential opportunities for more aggressive and targeted outpatient surveillance.
To address these gaps in knowledge, we linked data from a large, national in-hospital cardiac arrest registry with Medicare inpatient claims files and examined 30-day and 1-year rates of readmission and inpatient resource use among patients who survived an in-hospital cardiac arrest. Specifically, we examined whether rates of these outcomes differed by demographic characteristics, neurological status and disposition at hospital discharge.
Methods
Data Sources and Linkage
Get With The Guidelines (GWTG)-Resuscitation, formerly the National Registry of Cardiopulmonary Resuscitation, is a large prospective quality-improvement registry of in-hospital cardiac arrests. Hospital participation is voluntary, and the registry’s design has been described in detail previously.3 In brief, trained quality-improvement hospital personnel enroll all patients with cardiac arrest (defined as the absence of a palpable central pulse, apnea, and unresponsiveness) and without do-not-resuscitate orders. Cases are identified by multiple methods, including centralized collection of cardiac arrest flow sheets, reviews of hospital paging system logs, and routine checks of code carts, pharmacy tracer drug records, and hospital billing charges for resuscitation medications.3 The registry uses standardized “Utstein-style” templates to define patient variables and outcomes to facilitate uniform reporting across hospitals.4, 5 Data accuracy is further ensured by rigorous certification of hospital staff and use of standardized software with data checks for completeness and accuracy.6
We linked GWTG-Resuscitation patient-level data from January 1, 2000, through December 31, 2008, with Medicare inpatient files using 6 identifiers: dates of hospital admission and discharge, patient age and sex, admitting hospital (deidentified), and International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes. 2, 7 We selected Medicare records for the linkage if they included a diagnosis code for cardiac arrest (427.5), ventricular fibrillation (427.41), or ventricular flutter (427.42) or a procedure code for cardiopulmonary resuscitation (99.60), defibrillation (99.62), or closed chest massage (99.63). To further optimize the match, we also selected records containing a diagnosis code for acute respiratory failure (518.81) or shock (785.5x) to identify patients who did not have a diagnosis of cardiac arrest in the Medicare claims data but otherwise were uniquely matched on all other identifiers, including hospital. For each linked patient, we obtained Medicare denominator and inpatient files from 2000 through 2010. Denominator files contain information on all Medicare beneficiaries enrolled in a given year while inpatient files contain information on readmission dates, diagnoses, procedures, diagnosis-related group (DRG), and hospital reimbursement.
Study Population
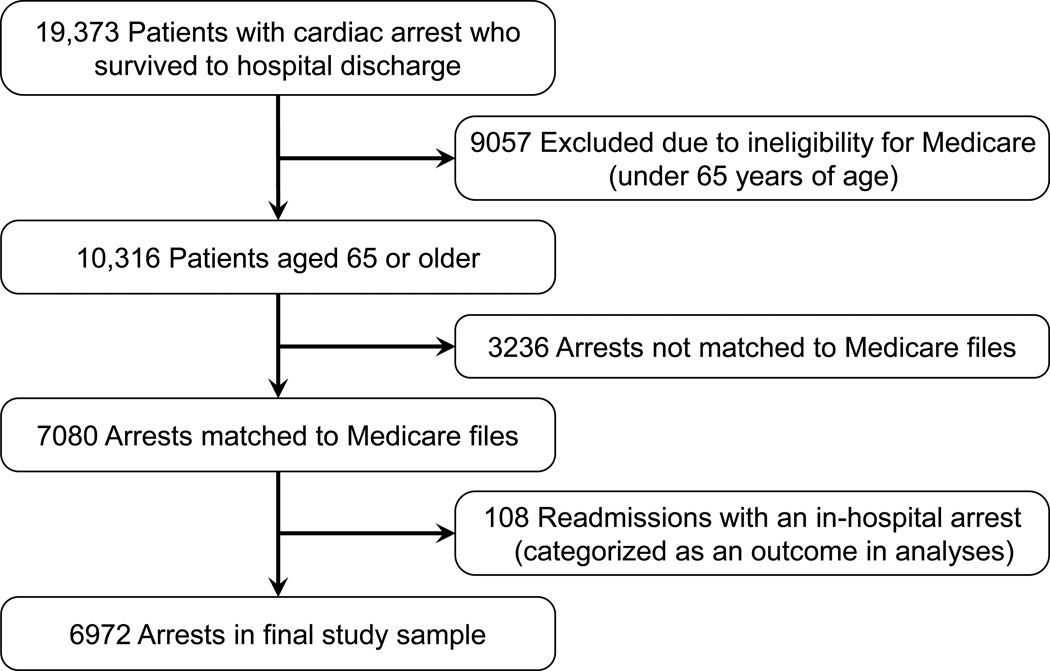
The study cohort included 523 acute-care hospitals that submitted data to GWTG-Resuscitation between January 1, 2000, and December 31, 2008. A total of 19,373 patients 18 years or older had a pulseless in-hospital cardiac arrest and survived to discharge (Figure 1). We excluded 9057 patients younger than 65 years who were not yet entitled to Medicare benefits, leaving 10,316 Medicare age-eligible patients. Using the method described above, we were able to match 7080 (68.6%) eligible patients to Medicare claims data.2 A GWTG-Resuscitation record was not matched to a Medicare hospitalization (n=3236) when a patient 1) was admitted to a non-Medicare hospital (e.g., Veterans Administration hospital), 2) had insurance other than fee-for-service Medicare, 3) was admitted to a hospital with few registry patients (thus precluding a unique match), or 4) lacked a qualifying ICD-9-CM diagnosis or procedure code for cardiac arrest in the Medicare files, as described above. Notably, patients who were and were not linked to Medicare files were found to have similar demographic and clinical characteristics (Supplemental Appendix eTable 1). Finally, for patients who experienced cardiac arrest during multiple hospitalizations, we used the first hospitalization as the index hospitalization and categorized 108 cardiac arrests during subsequent hospitalizations as readmissions. The final study cohort comprised 6972 patients who survived an in-hospital cardiac arrest from 401 hospitals. Notably, these hospitals were geographically distributed throughout the U.S. and represented different hospital bed sizes, with one-half having training programs for residents or fellows and the majority located in urban areas (Supplemental Appendix eTable 2).
Figure 1. Study Cohort.
Study Outcomes
The outcomes of interest were all-cause readmission and inpatient resource use. We examined rates of each outcome at 30 days and 1 year after discharge from an in-hospital cardiac arrest. Readmission was determined from the linked Medicare inpatient files, which contained data as to whether and when a patient was readmitted to a hospital and the ICD-9-CM code for the principal discharge diagnosis for hospitalization. Cost information was also determined from Medicare Part A inpatient files, which provided the actual Medicare payment to hospitals for each readmission.
Statistical Analysis
Baseline characteristics of the study cohort were described using proportions for categorical variables and means with standard deviations for continuous variables. We computed cumulative readmission incidence rates at 30 days and 1 year of follow-up. From these rates, the mean number of readmissions per patient-year of follow-up was determined. To determine the reasons for readmission, hospitalizations were further categorized by common diagnosis groups (e.g., heart failure, myocardial infarction, infection, pneumonia, etc.) using the ICD-9-CM codes for principal discharge diagnosis.
Inpatient resource use for the whole cohort was determined by summing costs for each patient’s rehospitalizations from the linked Medicare inpatient files. We then computed adjusted cost ratios for the following pre-specified subgroups: age, sex, race, initial cardiac arrest rhythm, hospital disposition (discharge destination), and neurological status at discharge. Neurological status at discharge was assessed using commonly-used cerebral performance categories, which distinguished patients with mild to no neurological disability, moderate neurological disability, severe neurological disability, and coma or vegetative state.8
To determine adjusted costs and cost ratios, since some patients had no follow-up inpatient costs, we constructed a two-part model conditional on patients having follow-up inpatient costs, comprised of (1) a logistic regression model predicting the probability of having any follow-up costs,9 and (2) a gamma regression model with a log link for the costs (for those patients with non-zero follow-up costs),10 with both models adjusted for a patient’s characteristics and comorbidities (which are collected by GWTG-Resuscitation using standardized registry definitions). From the model, we calculated adjusted costs for each reference group by performing 1000 bootstrap samples and computing the mean over these 1000 samples. Adjusted cost ratios and 95% confidence intervals for each subgroup were derived also by performing 1000 bootstrap samples, with the 2.5th and 97.5th percentile cost ratios defined as the 95% CI.11 Finally, the adjusted costs for each subgroup strata were obtained by multiplying the adjusted cost ratio for each strata with the adjusted costs for its reference group, with all other covariates fixed at their mean values in the population.
In these models, besides age (65 to 74 years, 75 to 84 years, ≥85 years), sex, race (white, black, other), initial cardiac arrest rhythm (asystole, pulseless electrical activity, ventricular fibrillation, pulseless ventricular tachycardia), hospital disposition (home without assistance, home with home health care, skilled nursing facility, inpatient rehabilitation, hospice), and discharge neurological status, we also adjusted for co-morbidities or medical conditions present prior to cardiac arrest (congestive heart failure, myocardial infarction, or diabetes mellitus; renal, hepatic, or respiratory insufficiency; baseline evidence of motor, cognitive, or functional deficits; acute stroke; pneumonia; hypotension; sepsis; major trauma; metabolic or electrolyte abnormality; metastatic or hematologic malignancy; and requirement for mechanical ventilation or hemodialysis) and therapeutic interventions in place at the time of cardiac arrest (anti-arrhythmic drugs, intravenous vasopressors, dialysis, pulmonary artery catheter, and intra-aortic balloon pump).
Overall, rates of missing data were low. Race was missing for 396 (5.7%) patients, and discharge neurological status was missing for 858 (12.3%) patients. For the multivariable models, we performed multiple imputation with IVEware software (University of Michigan, Ann Arbor).12 Results with and without imputation were not meaningfully different, so we present the former.
For each subgroup analysis of inpatient resource use, we evaluated the null hypothesis of no difference in 30-day and 1-year costs at a 2-sided significance level of 0.05 and calculated 95% confidence intervals (CIs) using robust standard errors. All analyses were performed using SAS version 9.2 (SAS Institute, Cary, North Carolina) and R version 2.10.0 (R Foundation for Statistical Computing, Vienna, Austria).13
The institutional review boards of the Duke University Health System and the Mid America Heart Institute approved the study. Dr. Chan takes responsibility for the accuracy of the data and all analyses, and the final manuscript draft was reviewed and approved by the GWTG-Resuscitation research and publications committee and the American Heart Association’s Executive Database Steering Committee.
Results
Of the 6972 patients who survived an in-hospital cardiac arrest in our study, the mean age was 75.8 ± 7.0 years and 56% were men (Table 1). Approximately 12% of patients were of black race and nearly half (46.4%) had an initial cardiac arrest rhythm of ventricular fibrillation or pulseless ventricular tachycardia that was amenable to defibrillation. One-quarter of patients had an incident myocardial infarction or heart failure exacerbation during the index hospitalization, and nearly one-fifth of patients were hypotensive or on mechanical ventilation at the time of cardiac arrest. The principal diagnoses for the index hospitalization in which in-hospital cardiac arrest occurred are summarized in Supplementary Appendix eTable 3. Cardiovascular diseases comprised more than half of all index hospitalizations for in-hospital cardiac arrest (54.5% [3802/6972]), whereas pneumonia and other infections accounted for 1148 (16.5%) of hospitalizations.
Table 1. Characteristics of the Study Cohort.
| Characteristic | Patients (N=6972) |
|---|---|
| Demographic characteristics | |
| Age — yr | 75.8 ± 7.0 |
| Male sex — no. (%) | 3872 (55.5) |
| Race — no. (%)* | |
| White | 5634 (85.7) |
| Black | 778 (11.8) |
| Other | 164 (2.5) |
| Initial cardiac arrest rhythm — no. (%) | |
| Asystole | 1707 (24.5) |
| Pulseless electrical activity | 2031 (29.1) |
| Pulseless ventricular tachycardia | 1109 (15.9) |
| Ventricular fibrillation | 2125 (30.5) |
| CPC score at discharge — no. (%)† | |
| 1 (mild to no neurological disability) | 2943 (48.1) |
| 2 (moderate neurological disability) | 2097 (34.3) |
| 3 (severe neurological disability) | 879 (14.4) |
| 4 (coma or vegetative state) | 195 (3.2) |
| Preexisting conditions — no. (%) | |
| Acute stroke | 249 (3.6) |
| Baseline depression in CNS function | 736 (10.6) |
| Diabetes mellitus | 2262 (32.4) |
| Heart failure during admission | 1625 (23.3) |
| Heart failure prior to admission | 1848 (26.5) |
| Hepatic insufficiency | 143 (2.1) |
| Hypotension | 1313 (18.8) |
| Major trauma | 113 (1.6) |
| Metabolic or electrolyte abnormality | 770 (11.0) |
| Metastatic or hematologic malignancy | 518 (7.4) |
| Myocardial infarction during admission | 1897 (27.2) |
| Myocardial infarction prior to admission | 1805 (25.9) |
| Renal insufficiency | 1836 (26.3) |
| Respiratory insufficiency | 2368 (34.0) |
| Pneumonia | 725 (10.4) |
| Septicemia | 473 (6.8) |
| Interventions in place at time of cardiac arrest — no. (%) | |
| Mechanical ventilation | 1246 (17.9) |
| Intravenous vasopressors | 1203 (17.3) |
| Intravenous antiarrhythmics | 530 (7.6) |
| Dialysis | 136 (2.0) |
| Pulmonary artery catheter | 326 (4.7) |
| Intra-aortic balloon pump | 104 (1.5) |
At hospital discharge, 48.1% of patients had mild to no neurological disability, 34.3% had moderate disability, 14.4% had severe disability, and 3.2% were in a coma or vegetative state. Most (55.3%) patients were discharged to either an inpatient rehabilitation or skilled nursing facility, and 4.8% went to hospice for comfort care. Of the 40% of patients who were discharged home, the majority (62%) did not receive any home health or nursing assistance.
Readmissions
Figure 2 depicts the cumulative incidence for all-cause readmission during the first year after discharge from an in-hospital cardiac arrest. Although 18.0% of patients died within the first 30 days after discharge, there were a total of 2005 readmission, yielding a 30-day mean cumulative incidence rate of 35 readmissions per 100 patients (95% confidence interval [CI], 33 to 37). By 1 year, there were a total of 8751 readmissions and 41.5% of patients had died (mean follow-up time of 248 ± 152 days), yielding a 1-year mean cumulative incidence rate of 185 readmissions per 100 patients (95% CI, 177 to 190). Notably, nearly half of patients were not readmitted during the first year, and 30% were readmitted more than once (Table 2).
Figure 2. Mean Cumulative Incidence for Any Readmission During Follow-up.
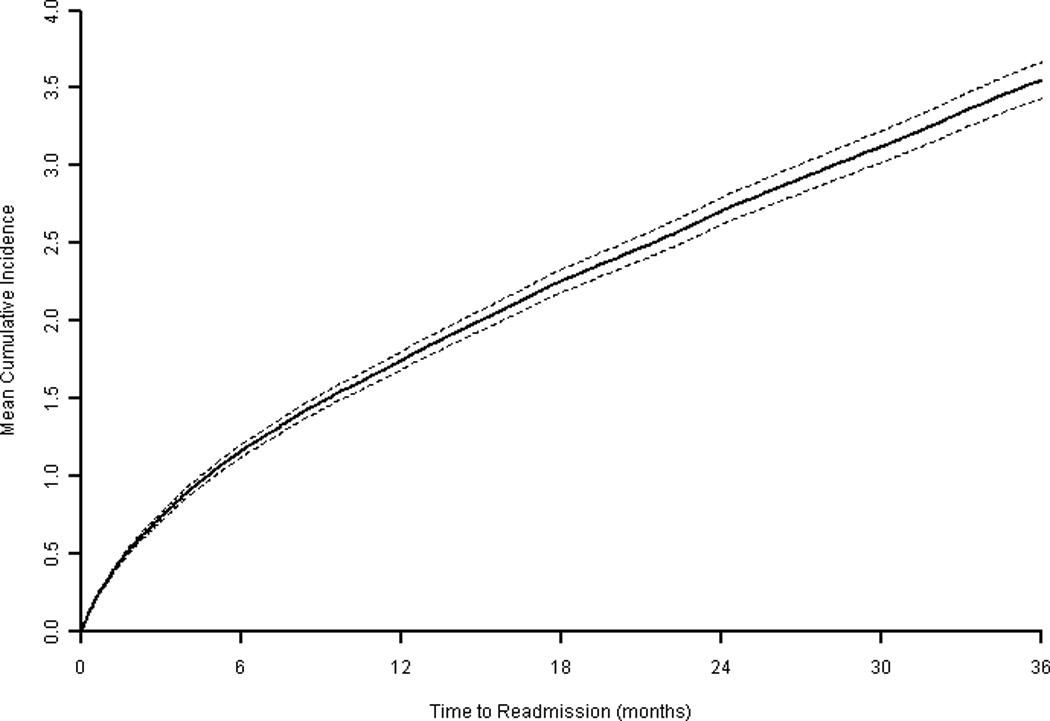
Cumulative incidence rate represented by solid line and 95% confidence intervals by dashed lines.
Table 2. Distribution of Readmission Frequency at 1-Year Follow-up.
Nearly half of those discharged alive after an in-hospital cardiac arrest were not readmitted during the first year, while another 30% were readmitted more than once.
| Number of Readmissions |
Patient N | % |
|---|---|---|
| 0 | 3182 | 45.6% |
| 1 | 1701 | 24.4% |
| 2 | 884 | 12.7% |
| 3 | 514 | 7.4% |
| 4 | 281 | 4.0% |
| 5 | 175 | 2.5% |
| >5 | 235 | 3.4% |
Table 3 summarizes the primary reasons for readmission. Of 2005 readmissions during the first 30 days of follow-up, cardiovascular disease was the predominant reason for readmission, comprising 720 (35.9%) of these hospitalizations. Another 43% of hospitalizations were due to pulmonary disease (n=343 [17.1%]), upper and lower gastrointestinal disease, including bleeding (n=265 [13.2%]), infections other than pneumonia (n=135 [6.7%]), and renal disease (n=118 [5.9%]). Notably, heart failure was the most frequent individual diagnosis related group, constituting 16.7% of all readmissions. Importantly, recurrent cardiac arrest as the principal reason for readmission was infrequent (11 [0.5%] readmissions). These category percentages were similar when we examined reasons for readmission at 1 year after hospital discharge (see Table 3).
Table 3. Principal Reasons for Readmission at 30 Days and 1 Year.
| 30 Day | 1 Year | |||
|---|---|---|---|---|
| n = 2005 | % | n = 8751 | % | |
| CARDIOVASCULAR | ||||
| Heart failure | 335 | 16.7 | 1374 | 15.7 |
| Coronary artery disease | 70 | 3.5 | 332 | 3.8 |
| Myocardial infarction | 59 | 2.9 | 207 | 2.4 |
| Chest pain | 38 | 1.9 | 138 | 1.6 |
| Syncope | 9 | 0.4 | 66 | 0.8 |
| Cardiac arrest | 11 | 0.5 | 40 | 0.5 |
| Other cardiac | 198 | 9.9 | 814 | 9.3 |
| PULMONARY | ||||
| Pneumonia | 88 | 4.4 | 439 | 5.0 |
| Acute Respiratory Failure | 83 | 4.1 | 277 | 3.2 |
| Chronic Obstructive Pulmonary Disease | 24 | 1.2 | 231 | 2.6 |
| Other Pulmonary | 148 | 7.4 | 476 | 5.4 |
| GASTROINTESTINAL | ||||
| Gastrointestinal bleed | 158 | 7.9 | 435 | 5.0 |
| PUD, Liver, and Intestinal diseases | 51 | 2.5 | 299 | 3.4 |
| Other Gastrointestinal | 56 | 2.8 | 280 | 3.2 |
| INFECTION | ||||
| Sepsis | 118 | 5.9 | 495 | 5.7 |
| Bacteremia and other infections without sepsis | 17 | 0.8 | 101 | 1.2 |
| RENAL DISEASE | 118 | 5.9 | 542 | 6.2 |
| MEDICAL / SURGICAL COMPLICATIONS | 127 | 6.3 | 492 | 5.6 |
| HEMATOLOGY / ONCOLOGY | ||||
| Malignant Cancer | 22 | 1.1 | 157 | 1.8 |
| Anemia | 5 | 0.2 | 34 | 0.4 |
| Other hematologic | 7 | 0.3 | 52 | 0.6 |
| Other cancers | 2 | 0.1 | 20 | 0.2 |
| NEUROLOGICAL | ||||
| Stroke | 39 | 1.9 | 209 | 2.4 |
| Other Neurological | 25 | 1.2 | 124 | 1.4 |
| ENDOCRINE | ||||
| Diabetes and complications | 32 | 1.6 | 171 | 2.0 |
| Other endocrine or immune-related | 11 | 0.5 | 49 | 0.6 |
| DEHYDRATION AND ELECTROLYTES | 38 | 1.9 | 185 | 2.1 |
| FRACTURE AND OTHER MUSCULOSKELETAL | 32 | 1.6 | 169 | 1.9 |
| INJURY OR POISONING | 18 | 0.9 | 159 | 1.8 |
| PSYCHIATRIC | 8 | 0.4 | 72 | 0.8 |
| ALL OTHER CAUSES | 58 | 2.9 | 312 | 3.6 |
Abbreviations: PUD, peptic ulcer disease
Inpatient Resource Use
The mean (± standard deviation) length of stay for the index hospitalization for in-hospital cardiac arrest was 19 ± 16 days, and the mean cost of that stay was $35,808 ± $38,230. In contrast, the mean cost for readmissions for the whole cohort (including those who were not admitted) was $7,741 ± $2323 at 30 days and $18,629 ± $9411 at 1 year. On average, a patient was hospitalized for 11 ± 22 days during the first year.
Inpatient resource use was substantially higher in younger than older patients, with 30-day adjusted costs of $6052 in patients 85 years or older, as compared with $7444 (adjusted cost ratio, 1.23; 95% confidence interval [CI], 1.06–1.42; P<0.001) and $8291 (adjusted cost ratio, 1.37; 95% CI, 1.19–1.59; P<0.001) for patients 75 to 84 years and 65 to 74 years of age, respectively (Table 4). Compared with whites (adjusted mean cost of $7413), black patients had higher 30-day adjusted inpatient resource use of $9044 (adjusted cost ratio, 1.22; 95% CI, 1.05–1.42; P<0.001). Patients with an initial cardiac arrest rhythm of ventricular fibrillation had lower adjusted inpatient resource use than those with an initial cardiac arrest rhythm of pulseless electrical activity. Similar patterns of inpatient costs were found for each subgroup when the follow-up was extended to 1 year after hospital discharge. In each instance, these differences in inpatient resource use were accompanied by parallel differences in readmission rates (e.g., those with higher inpatient resource use had higher cumulative readmission incidence rates; see Table 4)
Table 4. Long-Term Inpatient Resource Use, Overall and by Patient Subgroup.
Thirty-day and 1 year inpatient resource use for the overall cohort and pre-specified patient subgroups were determined from multivariable models and are summarized.
| Cumulative Readmission Incidence |
Adjusted Costs |
30-DAY Cost Ratio (95% CI) |
P | Cumulative Readmission Incidence |
Adjusted Costs |
1-YEAR Cost Ratio (95% CI) |
P | |
|---|---|---|---|---|---|---|---|---|
| ALL PATIENTS | 0.35 | $7,741* | 1.85 | $18,629* | ||||
| AGE GROUPS | ||||||||
| 65 to 74 | 0.32 | $8,291 | 1.37 (1.19–1.59) | <0.001 | 1.70 | $20,686 | 1.40 (1.24–1.60) | <0.001 |
| 75 to 84 | 0.33 | $7,444 | 1.23 (1.06–1.42) | <0.001 | 1.75 | $17,583 | 1.19 (1.06–1.34) | <0.001 |
| ≥ 85 | 0.36 | $6,052 | Reference | -- | 1.92 | $14,776 | Reference | -- |
| SEX | ||||||||
| Men | 0.31 | $7,706 | Reference | -- | 1.64 | $18,751 | Reference | -- |
| Women | 0.35 | $7,475 | 0.97 (0.87–1.06) | 0.28 | 1.87 | $18,188 | 0.97 (0.90–1.04) | 0.20 |
| RACE GROUPS | ||||||||
| White | 0.30 | $7,413 | Reference | -- | 1.64 | $17,687 | Reference | -- |
| Black | 0.47 | $9,044 | 1.22 (1.05–1.42) | <0.001 | 2.54 | $24,585 | 1.39 (1.24–1.54) | <0.001 |
| Other | 0.45 | $7,487 | 1.01 (0.77–1.30) | 0.50 | 2.41 | $21,932 | 1.24 (0.89–1.61) | 0.09 |
| INITIAL RHYTHM | ||||||||
| Pulseless electrical activity | 0.34 | $7,843 | Reference | -- | 1.81 | $19,785 | Reference | -- |
| Asystole | 0.37 | $8,627 | 1.10 (0.96–1.25) | 0.08 | 1.98 | $18,796 | 0.95 (0.86–1.04) | 0.11 |
| Ventricular fibrillation | 0.28 | $6,667 | 0.85 (0.73–0.96) | 0.008 | 1.49 | $17,015 | 0.86 (0.77–0.94) | <0.001 |
| Pulseless VT | 0.34 | $7,608 | 0.97 (0.82–1.16) | 0.36 | 1.81 | $18,994 | 0.96 (0.86–1.07) | 0.22 |
| NEUROLOGICAL STATUS | ||||||||
| Mild to no disability | 0.28 | $7,314 | Reference | -- | 1.52 | $17,980 | Reference | -- |
| Moderate disability | 0.37 | $7,533 | 1.03 (0.91–1.16) | 0.31 | 1.97 | $19,418 | 1.08 (1.00–1.18) | 0.03 |
| Severe disability | 0.38 | $9,581 | 1.31 (1.13–1.53) | <0.001 | 2.07 | $19,958 | 1.11 (1.00–1.25) | 0.03 |
| Coma or vegetative state | 0.36 | $4,096 | 0.56 (0.36–0.78) | <0.001 | 1.94 | $9,350 | 0.52 (0.37–0.69) | <.001 |
|
DISCHARGE DESTINATION |
||||||||
| Home, without assistance | 0.26 | $3,232 | Reference | -- | 1.39 | $12,460 | Reference | -- |
| Home, with home health | 0.31 | $3,361 | 1.04 (0.83–1.31) | 0.39 | 1.68 | $13,955 | 1.12 (0.98–1.28) | 0.04 |
| Skilled nursing care | 0.38 | $5,204 | 1.61 (1.34–2.01) | <0.001 | 2.04 | $15,949 | 1.28 (1.13–1.43) | <0.001 |
| Rehabilitation site | 0.36 | $28,603 | 8.85 (7.55–10.59) | <0.001 | 1.94 | $40,620 | 3.26 (2.96–3.61) | <0.001 |
| Hospice | 0.11 | $162 | 0.05 (0.01–0.10) | <0.001 | 0.62 | $374 | 0.03 (0.01–0.06) | <0.001 |
Costs for the whole cohort (All Patients) are crude costs. All subgroup costs were model adjusted.
Abbreviations: VT, ventricular tachycardia
At 1 year, patients discharged with moderate or severe neurological disability had much higher inpatient resource use as compared with patients with mild to no neurological deficits or in a coma or vegetative state. Compared with those who were able to be discharged home without any nursing assistance, patients who required home health nursing care, inpatient skilled nursing care, and inpatient rehabilitation after discharge had higher inpatient costs at 1 year. Not surprisingly, patients discharged to hospice care had minimal 1-year costs (adjusted costs, $374). Notably, there were no differences in inpatient resource use by sex. These subgroup patterns were similar when examining cost ratios at 30 days. Lastly, in contrast to follow-up inpatient costs, there were no cost differences for the index hospitalization by race, and initial hospitalization costs were higher for patients with coma or vegetative state (see Supplementary Appendix eTable 4).
Discussion
Among patients who survived to discharge after an in-hospital cardiac arrest, we found that readmissions occurred frequently, especially during the first 30 days (rate of 35 readmissions per 100 patients). On average, subsequent inpatient resource use was over $7800 during the first 30 days and nearly $19,000 during the first year. Cardiovascular disease was the most common reason for readmission, but this category comprised only one-third of all readmissions. There were important differences in readmission rates and inpatient costs, especially by age group, race, hospital disposition, and neurological status at discharge. Collectively, these findings provide important insights into the patterns of readmission and inpatient resource use by survivors of in-hospital cardiac arrest.
Since there are an estimated 200,000 in-hospital cardiac arrests annually in the U.S.,1 and because temporal trends suggest that survival rates have improved substantially over the past decade,14 there is growing interest in the morbidity and mortality of survivors of in-hospital cardiac arrest. Indeed, a recent study has found that the majority of hospitalized elderly patients who survive a cardiac arrest remain alive at 1 year.2 However, there has not been, to date, a systematic evaluation of readmission patterns and inpatient resource use of survivors of in-hospital cardiac arrest. Although one prior study quantified inpatient resource use to be nearly $63,000 per patient at a mean of 22 months of follow-up,15 that study was comprised of 28 survivors from one site, reported hospital charges (not actual payments), and included charges from both the index hospitalization and subsequent readmissions. Another study had found that 71% of patients who survived an in-hospital cardiac arrest were readmitted by 2 years. However, that study included only 79 survivors and did not examine cumulative rates of readmission nor quantify costs.16 By linking data from GWTG-Resuscitation to Medicare files, we were able to leverage rigorous data collection within a multicenter prospective registry with detailed information on inpatient utilization from a national insurance database. As a result, our study extends the findings of prior studies by providing, to date, the most representative and comprehensive estimates of long-term readmission and inpatient resource use for survivors of in-hospital cardiac arrest.
Our findings help put into context the notion that survivors of in-hospital cardiac arrest have extraordinarily high morbidity and mortality. In a recent study, we found that survivors of in-hospital cardiac arrest have a similar 3-year mortality rate as Medicare-matched patients hospitalized with heart failure.17 In this present study, we found that inpatient resource use during the first year for in-hospital cardiac arrest survivors was similar to 1-year costs for systolic heart failure patients with poor health status (e.g., EPHESUS trial: $18,476)18 and those with moderate to severe neurological disability after cardio-embolic stroke ($23,000).19 Therefore, although survivors of in-hospital cardiac arrest have significant morbidity and mortality after hospital discharge, these rates are not substantially different from those of other highly morbid cardiac conditions. Interestingly, rehospitalization for cardiac arrest was rare, occurring in <1% of readmissions.
Our study was also able to examine whether differences in inpatient resource use differed by important subgroups. Black patients who survive an in-hospital cardiac arrest are known to have lower survival rates after hospital discharge than white patients.2 We found that they also had higher rates of readmissions and subsequent inpatient resource use, which is consistent with their higher long-term mortality rate. We also found significant differences by age group, with fewer readmissions and lower inpatient resource use among more elderly survivors. Although the reasons for the lower rate are not altogether clear, it may be related to age differences in use of advanced directives (particularly concerning resuscitations) and decisions about palliative care after surviving a cardiac arrest. There was also a gradient of inpatient resource use by hospital disposition. Patients discharged home had the lowest rate of readmissions and inpatient resource use, whereas patients sent to rehabilitation centers had the highest, with 44% higher 1-year inpatient costs. Finally, there was a notable step-wise gradient in readmission rates and long-term inpatient resource use by discharge neurological status, with higher utilization among those with greater neurological disability at hospital discharge.
The cost data from this study provides important post-discharge information for the overall cohort and for specific subgroups – information that prior to our analysis has been missing from the literature. Although we did not conduct assessments of cost-effectiveness in this manuscript, prior cost-effectiveness studies (e.g., hypothermia in cardiac arrest survivors) have lacked reliable estimates of long-term costs among cardiac arrest survivors. As new technologies and treatment strategies become adopted (e.g., routine cardiac catheterization of cardiac arrest survivors, therapeutic hypothermia, implantable cardioverter-defibrillators) in survivors of in-hospital cardiac arrest, we believe the specific cost estimates from this study could be used to provide more precise estimates of their cost-effectiveness. Finally, our readmission and cost findings suggest a critical need for the development and testing of strategies which can reduce neurological disability during the acute resuscitation period and/or improve post-discharge recovery in these high-risk patients. If such strategies were found to be successful, they would not only reduce morbidity but also substantial downstream costs.
Our study should be interpreted in the context of the following potential limitations. First, GWTG-Resuscitation is a quality-improvement registry. Although it collects data from a diverse group of hospitals, our findings may not be generalizable to all U.S. hospitals, including non-Medicare (e.g., Veteran Administration) hospitals. Second, we restricted the analysis to fee-for-service Medicare beneficiaries who could be matched to Medicare files; therefore, readmission patterns and inpatient resource use in patients younger than 65 years and those with Medicare Advantage plans may differ. Third, our cost data for readmissions were based on Medicare payments to hospitals, which reimburse at lower rates than private insurers and may underestimate inpatient resource use for all patients. Fourth, we did not have cost data for other types of non-acute care, such as skilled nursing and outpatient rehabilitation, which would have underestimated the cost ratios for patients with neurological disability. Fifth, we did not have information on outpatient utilization, such as medications and clinic visits, and we therefore only examined inpatient resource use. However, as the vast majority of total resource use is comprised of inpatient hospitalizations, our findings likely parallel patterns for total resource use. Sixth, our findings were restricted to survivors of in-hospital cardiac arrest and therefore do not apply to those with out-of-hospital cardiac arrest. Seventh, we excluded patients for whom a GWTG-Resuscitation record could not be linked to a Medicare hospitalization. Nonetheless, excluded patients were similar to patients in the study cohort; therefore, their exclusion was unlikely to significantly bias our results. Finally, our study was based on observational data; therefore, while we were able to adjust for a number of confounders, we were unable to account for certain factors, such as left ventricular ejection fraction, which may have influenced readmission rates or inpatient resource use.
In conclusion, we found that elderly survivors of in-hospital cardiac arrest were frequently readmitted, with high costs for inpatient care during follow-up. Readmission rates and inpatient costs differed by patient age, race, hospital disposition and neurological status at discharge.
Supplementary Material
Acknowledgments
Funding/Support:
Dr. Chan is supported by a Career Development Grant Award (K23HL102224) from the National Heart Lung and Blood Institute.
Dr. Krumholz is supported by grant U01 HL105270-03 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute.
GWTG-Resuscitation is sponsored by the American Heart Association, which had no role in the study design, data analysis or manuscript preparation and revision.
Footnotes
Disclosures:
Dr. Chan has served as a consultant for the American Heart Association. Dr. Krumholz discloses that he is the recipient of a research grant from Medtronic, through Yale University, and is chair of a cardiac scientific advisory board for United Health. None of the other authors has any conflicts of interest or financial interests to disclose.
Authorship: Dr. Chan had full access to all of the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study Concept and design: Chan
Acquisition of Data: Chan, Curtis
Statistical Analysis: Li, Hammill
Analysis and interpretation of data: Chan, Nallamothu, Krumholz, Curtis, Li, Hammill, Spertus
Drafting of the manuscript: Chan
Critical revision of the manuscript for important intellectual content: Chan, Nallamothu, Krumholz, Curtis, Li, Hammill, Spertus
Study Supervision: Chan
References
- 1.Merchant RM, Yang L, Becker LB, Berg RA, Nadkarni V, Nichol G, Carr BG, Mitra N, Bradley SM, Abella BS, Groeneveld PW. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39:2401–2406. doi: 10.1097/CCM.0b013e3182257459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan PS, Nallamothu BK, Krumholz HK, Spertus JA, Li Y, Hammill BG, Curtis LH. Long-term outcomes of elderly survivors of in-hospital cardiac arrest. N Engl J Med. 2013;368:1019–1026. doi: 10.1056/NEJMoa1200657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G, Lane-Trultt T. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 4.Cummins RO, Chamberlain D, Hazinski MF, Nadkarni V, Kloeck W, Kramer E, Becker L, Robertson C, Koster R, Zaritsky A, Bossaert L, Ornato JP, Callanan V, Allen M, Steen P, Connolly B, Sanders A, Idris A, Cobbe S. Recommended guidelines for reviewing, reporting, conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style’. American Heart Association. Circulation. 1997;95:2213–2239. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 5.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 6.Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM, Meaney PA, Cen L, Nadkarni VM, Praestgaard AH, Berg RA. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299:785–792. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 7.Hammill BG, Hernandez AF, Peterson ED, Fonarow GC, Schulman KA, Curtis LH. Linking inpatient clinical registry data to Medicare claims data using indirect identifiers. Am Heart J. 2009;157:995–1000. doi: 10.1016/j.ahj.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–484. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 9.Heilbron DC. Zero-Altered And Other Regression Models For Count Data With Extra Zeros. Boimetrical Journal. 1994;36:531–547. [Google Scholar]
- 10.Blough DK, Ramsey SD. Using Generalized Linear Models to Assess Medical Care Costs. Health Services and Outcomes Research Methodology. 2000;1:185–202. [Google Scholar]
- 11.Shao J, Tu D. The jackknife and bootstrap. New York: Springer Verlag; 1995. [Google Scholar]
- 12.Raghunathan TESP, Van Hoeyk J. IVEware: Imputation and Variance Estimation Software - User Guide. Michigan: Survey Research Center, Institute for Social Research University of Michigan; 2002. [Google Scholar]
- 13.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing V, Austria. ISBN 3-900051-07-0. 2008 URL http://www.R-project.org.
- 14.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berger R, Kelley M. Survival after in-hospital cardiopulmonary arrest of noncritically ill patients. A prospective study. Chest. 1994;106:872–879. doi: 10.1378/chest.106.3.872. [DOI] [PubMed] [Google Scholar]
- 16.Herlitz J, Andreasson AC, Bang A, Aune S, Lindqvist J. Long-term prognosis among survivors after in-hospital cardiac arrest. Resuscitation. 2000;45:167–171. doi: 10.1016/s0300-9572(00)00187-8. [DOI] [PubMed] [Google Scholar]
- 17.Chan PS, Nallamothu BK, Krumholz HM, Spertus JA, Li Y, Hammill BG, Curtis LH. Long-term outcomes in elderly survivors of in-hospital cardiac arrest. N Engl J Med. 2013;368:1019–1026. doi: 10.1056/NEJMoa1200657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan PS, Soto G, Jones PG, Nallamothu BK, Zhang Z, Weintraub WS, Spertus JA. Patient Health Status and Costs in Heart Failure Insights From the Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS) Circulation. 2009;119:398–407. doi: 10.1161/CIRCULATIONAHA.108.820472. [DOI] [PubMed] [Google Scholar]
- 19.Chan PS, Vijan S, Morady F, Oral H. Cost-effectiveness of radiofrequency catheter ablation for atrial fibrillation. J Am Coll Cardiol. 2006;47:2513–2520. doi: 10.1016/j.jacc.2006.01.070. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.