Abstract
Objectives
Associations of objectively measured activity across the full range of levels with mortality in the aged population are uncertain. This study examines associations of objective measures of activity level with mortality risk in older men.
Design
Prospective cohort study
Setting
Six U.S. sites
Participants
2918 men age ≥71 years followed an average of 4.5 years
Measurements
Time awake spent in sedentary behavior (MET level ≤1.50), light activity (MET level 1.51–2.99) and at least moderate activity (MET level ≥3.00) measured using an activity monitor (SenseWearPro armband worn ≥5 days) and expressed as quartiles (Q). Deaths confirmed with death certificates; cause of death adjudicated by review of certificates and records.
Results
During follow-up, 409 (14%) men died. After multivariable adjustment, greater time spent in sedentary behavior (hazard ratio [HR] Q4 vs. Q1 1.51 [95% CI, 1.10–2.08]), less time spent in light activity (HR Q1 vs. Q4 1.54 [95% CI, 1.06–2.24]), and less time spent in at least moderate activity (HR Q1 vs. Q4 1.56 [95% CI, 1.09–2.25]), were similarly associated with increased mortality risk primarily due to higher risks of cardiovascular and non-cardiovascular, non-cancer death. The association of time spent in sedentary behavior with mortality varied by time spent at higher activity level. Greater time spent in sedentary behavior was associated with an increased risk of death among men spending ≥1.2 (median) hours/day in at least moderate activity (HR Q4 vs. Q1 2.09 [95% CI, 1.26–3.49]), but not among those spending less time (HR Q4 vs. Q1 1.02 [95% CI, 0.62–1.66]) (p=0.005 for interaction).
Conclusion
In older men exceeding current guidelines on physical activity, greater time spent in sedentary behavior is associated with increased mortality risk.
Keywords: physical activity, mortality, aging, men
INTRODUCTION
A typical 24-hour period is comprised of sleeping and a wide range of activities during the waking period including sedentary behavior, light intensity activity, moderate intensity activity and vigorous intensity activity. While activity intensity levels can be estimated by self-report, questionnaire-based assessments are subject to recall and reporting biases1 and often do not accurately capture light activity and sedentary behaviors.2 These limitations may be of most concern when estimating activity level of older adults.3;4
Activity level can be objectively measured using an accelerometer, a small electronic device that provides an objective record of the volume, intensity and frequency of activity between and within a 24 hour period with considerable precision.5 Studies using accelerometry data in participants in the 2003–2004 U.S. National Health and Nutrition Examination Survey (NHANES)have reported that older adults are most sedentary with 9 hours per day of sedentary time during waking hours among those ≥75 years6, and least active with average time in vigorous activity not different from zero among those ≥60 years.4
While a few prior studies have reported the relationship of objectively measured activity7;8with risk of death in older adults, the associations of objectively measured activity across the full range of levels with mortality risk in the aged population are uncertain. Specifically, it is uncertain whether objectively measured light activity is related to risk of death and if sedentary time is a risk factor for mortality among adults meeting public health guidelines on participation in physical activity (i.e. those spending ≥30 minutes of moderate activity on five days each week). To comprehensively assess associations of objective measures of activity level with mortality risk in older men, we measured time awake spent in sedentary behavior, light activity and at least moderate activity and time spent asleep using a portable multisensory device in a cohort of 2918 men ≥71 years enrolled in the Osteoporotic Fractures in Men (MrOS) study and followed them prospectively for an average of 4.5 years for all-cause and cause-specific mortality.
METHODS
Study Population
From 2000 to 2002, 5994 men aged ≥65 years were recruited from population-based listings in six regions of the United States for the baseline visit of MrOS.9;10Men with a history of bilateral hip replacement and men unable to walk without the assistance of another person were excluded. From 2007 to 2009, surviving participants were invited to participate in a third study visit. The cohort for this analysis was comprised of 2918 men with valid activity monitor data at the third examination (See Supplementary Appendix Figure 1). The institutional review board at each participating institution approved the study protocol and written informed consent was obtained from all participants.
Activity Monitor
Participants were instructed to wear the activity monitor (SenseWear Pro Armband [Body Media, Inc., Pittsburgh, PA]) at all times, including while sleeping, over the right triceps muscle for a typical 7-day period and to remove it only for brief periods for bathing and water activities. Data were sampled in 1-minute (min) epochs over 24-hour periods from a heat flux sensor, a galvanic skin response sensor, a skin temperature sensor, a near body temperature sensor, and a body movement sensor (bi-axial accelerometer). These data were used in proprietary algorithms (Innerview Professional 5.1 software) along with participant characteristics (age, height, weight, handedness, and smoking status) to estimate time(min/24 hours) spent sleeping and time (min/24 hours) awake spent in sedentary behavior (Metabolic Equivalent Task [MET] level ≤1.50), light activity (MET level 1.51–2.99) and at least moderate activity (MET level ≥3.00).11 METs were calculated as energy expenditure divided by the constant value of 1 kcal/kg/hour.12;13
A validation study comparing the SenseWear Pro Armband with the criterion method of doubly labeled water showed excellent levels of agreement for total energy expenditure in older adults.14 In addition, a validation study in patients with obstructive sleep apnea and controls15 showed excellent levels of agreement between time spent sleeping estimated by the SenseWear software and total sleep time as measured using overnight in-laboratory polysomnography. Men were required to have at least five 24-hour periods of data and wear the activity monitor at least 90% of the time to be considered as having valid data; this time period was selected to ensure that the activity monitor recorded time spent in daily activity that was representative of the participant’s usual life. All activity level measures used in the analyses reflected mean daily experience in order to obtain a representative characterization of usual activity pattern, and were averaged over all days to limit variability in the measures.
Other Measurements
Participants were asked about race/ethnicity, education, marital status, smoking status, health status and a physician diagnosis of selected medical conditions (see footnote Table 1). Depressive symptoms were evaluated using the Geriatric Depression Scale.16 Men were asked about their ability to perform five instrumental activities of daily living (IADL).17 Self-reported physical activity was assessed using the Physical Activity Scale for the Elderly (PASE).18 Tests of physical function included gait speed (time in seconds to walk 6 meters at usual pace expressed as m/s). Cognitive function was assessed with the Modified Mini-Mental State examination.19 Total body bone mineral density including total body fat was measured with dual-energy x-ray absorptiometry.20
Table 1.
Characteristics of 2918 Men by Quartile of Time Awake Spent in Sedentary Behavior
| Characteristic | Quartile of Time Awake Spent in Sedentary
Behaviora, min/24hrs |
|||||
|---|---|---|---|---|---|---|
| Overall (n=2918) |
Q1 (least sedentary) (n=729) |
Q2 (n=730) |
Q3 (n=727) |
Q4 (most sedentary) (n=732) |
p-valueb | |
| Age, years, mean (SD) | 79.0 (5.2) | 77.8 (4.7) | 78.9 (5.1) | 79.4 (5.1) | 80.0 (5.5) | <0.001 |
| Caucasian race, n (%) | 2637 (90.4) | 664 (91.1) | 664 (91.0) | 648 (89.1) | 661 (90.3) | 0.57 |
| College degree or higher, n (%) | 2315 (79.3) | 561 (77.0) | 586 (80.3) | 583 (80.2) | 585 (79.9) | 0.16 |
| Married, n (%) | 2289 (78.4) | 599 (82.2) | 558 (76.4) | 573 (78.8) | 559 (76.4) | 0.02 |
| Health status, excellent/good, n (%) | 2543 (87.2) | 653 (89.8) | 649 (88.9) | 632 (87.1) | 609 (83.2) | <0.001 |
| Current smoker, n (%) | 53 (1.8) | 12 (1.7) | 11 (1.5) | 11 (1.5) | 19 (2.6) | 0.45 |
| Selected medical conditionsc, n (%) | <0.001 | |||||
| 0–1 | 1618 (55.5) | 468 (64.2) | 428 (58.7) | 372 (51.2) | 350 (47.9) | |
| 2–3 | 1180 (40.5) | 245 (33.6) | 277 (38.0) | 313 (43.1) | 345 (47.2) | |
| 4+ | 118 (4.1) | 16 (2.2) | 24 (3.3) | 42 (5.8) | 36 (4.9) | |
| GDS score (0–15), mean (SD) | 1.7 (2.0) | 1.5 (2.0) | 1.6 (1.9) | 1.8 (2.0) | 2.0 (2.1) | <0.001 |
| 3MS score (0–100), mean (SD) | 92.7 (6.1) | 93.2 (5.5) | 92.7 (5.9) | 92.6 (6.4) | 92.3 (6.6) | 0.10 |
| IADLd impairments (0–5), mean (SD) | 0.2 (0.6) | 0.1 (0.5) | 0.2 (0.6) | 0.2 (0.6) | 0.4 (0.8) | <0.001 |
| Total percent body fat, mean (SD) | 26.6 (5.5) | 24.8 (5.4) | 26.5 (5.2) | 27.2 (5.5) | 27.9 (5.4) | <0.001 |
| PASE score, mean (SD) | 135.0 (67.4) | 159.5 (68.2) | 137.0 (66.5) | 126.9 (65.9) | 116.6 (61.3) | <0.001 |
| Gait speed, m/s, mean (SD) | 1.1 (0.2) | 1.2 (0.2) | 1.1 (0.2) | 1.1 (0.2) | 1.1 (0.2) | <0.001 |
| Time awake spent in light activitye, min/24hrs, mean (SD) | 67.7 (34.4) | 94.4 (37.4) | 69.1 (28.6) | 59.0 (27.0) | 48.5 (25.0) | <0.001 |
| Time awake spent in at least moderate activityf, min/24hrs, mean (SD) | 82.3 (60.5) | 140.0 (70.9) | 82.0 (44.9) | 62.1 (37.6) | 45.1 (32.4) | <0.001 |
| Time spent asleep, min/24hrs, mean (SD) | 392.8 (82.1) | 438.3 (75.8) | 421.1 (65.9) | 390.5 (59.4) | 321.8 (73.5) | <0.001 |
Abbreviations: GDS, Geriatric Depression Scale; 3MS, Modified Mini-Mental State examination; IADL, Instrumental Activities of Daily Living; PASE, Physical Activity Scale for the Elderly
Quartile cutpoints: 772.2, 844.7, 915.0 min/24hrs
time awake spent at Metabolic Equivalent Tasks (METs) ≤1.50, excluding time spent sleeping
Characteristics of participants were compared across quartiles using ANOVA for normally distributed continuous variables; Kruskal Wallis tests for skewed continuous variables and chi-square tests for homogeneity for categorical variables.
comorbidities include history of cardiovascular disease, self-reported hypertension, diabetes mellitus, chronic obstructive pulmonary disease, dementia, Parkinsonism, chronic kidney disease, liver disease, and non-skin (melanoma) cancer
activities include managing money, managing medications, shopping for groceries or clothes, performing housework/chores and meal preparation
time awake spent at METs 1.51 to 2.99
time awake spent at METs ≥ 3.00
Mortality
Participants were contacted every four months to ascertain vital status. During a mean (SD) follow-up of 4.5 (1.0) years after the third examination, over 99% of these contacts were completed. Deaths were confirmed with death certificates and cause of death was adjudicated due to cardiovascular disease(CVD), cancer or other cause by central physician review of death certificates and medical records. Cause of death was broadly categorized by ICD-9 codes as cardiovascular (codes 396.9–442, 966.71, 785.51), cancer (codes 141.9–208.0), and other causes (reported codes not in previous categories).
Statistical Analysis
The predictor variables of interest were time awake (min/24 hours) spent in sedentary behavior (MET level ≤1.50), light activity (MET level 1.51–2.99) and at least moderate activity (MET level ≥3.00). Characteristics of participants were compared across quartiles of time spent in sedentary behavior. Adjusted survival curves for each activity level measure stratified by quartiles were plotted.
Cox proportional hazards models were used to estimate the association of each activity level measure with all-cause and cause-specific mortality outcomes. The proportional hazards assumption for models was confirmed using Schoenfeld residuals.21 The hazard ratio (HR) and 95% confidence interval (CI) for each outcome was calculated across quartiles of time spent in sedentary behavior with quartile 1 (least sedentary) serving as the referent group, while the HR and 95% CI for outcomes was calculated across quartiles of time spent in light activity and quartiles of time spent in at least moderate activity) with quartile 4 (most active) serving as the referent group. Men who were lost to follow-up (n=26) were censored after date of last follow-up contact. In cause-specific mortality analyses, men who died of another cause were censored at the time of death.
Initial analyses were adjusted for age, race, site and season and then further adjusted for additional potential confounders selected for inclusion in the multivariable model because they were correlates of activity level measures or associated with mortality risk independent of age. Since studies in older adults have reported independent associations of self-reported physical activity22–28 and gait speed29 and inconsistent associations of objectively measured sleep duration30;31with risk of death in older adults, the PASE score, gait speed and time spent asleep were subsequently added to the multivariable model to determine whether an association was independent of self-reported activity, gait speed, and sleep duration. Multicollinearity of the PASE (and other covariates) with the activity monitor measures was examined and found to be at an acceptable level (variance inflation factors ≤2.5). Tests for trend were performed by including each activity level measure (ordinal variable, 4 levels) as an independent variable in the models.
We examined whether the associations differed by age group and tested for age *activity level measure interactions. Since unhealthy individuals who are at higher risk of death are also more likely to be sedentary and less active, sensitivity analyses were performed excluding 51 men who died during the first year of follow-up and excluding 1298 men with multiple (≥2) medical conditions. To determine if sedentary time was a risk factor for mortality among more active men, we stratified participants by time spent in light activity (<64 minutes [median] vs. ≥64 minutes) and time spent in at least moderate activity (<69 minutes [median] vs. ≥69 minutes). We also tested for the possibility of interactions between time spent in sedentary behavior and time spent at these higher activity levels for the prediction of risk of mortality.
All significance levels reported were two-sided. All analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
Among the 2918 men (mean age 79.0 years) in the cohort, activity monitor data were collected for an average (SD) of 5.1 (0.3) 24-hour periods. In a typical 24-hour period, men were sedentary while awake for 60.8% of the time, participated in light activities while awake for 4.9% of the time and participated in at least moderate activity while awake for 5.9% of the time (28.4% of time was spent sleeping). Of time spent in at least moderate activity, only 13% was spent in vigorous (MET level ≥6.00) activity. Median (interquartile range) was 845 (772–915) minutes for time awake spent in sedentary behavior, 64 (42–88) minutes for time awake spent in light activity and 69 (38–114) minutes for time awake spent in at least moderate activity. There were moderate inverse correlations between time spent in sedentary behavior and the other activity level variables(r=−0.53 for time spent in light activity and −0.63 for time spent in at least moderate activity); the correlation between time spent in light activity and time spent in at least moderate activity was 0.69. Characteristics of participants by quartile of time spent in sedentary behavior are shown in Table 1.
Activity Level Measures and All-Cause Mortality
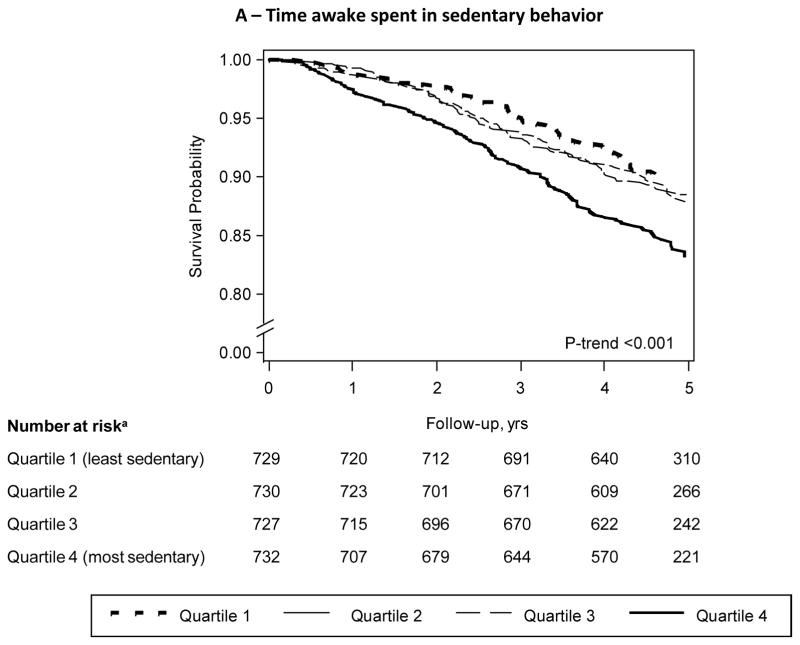
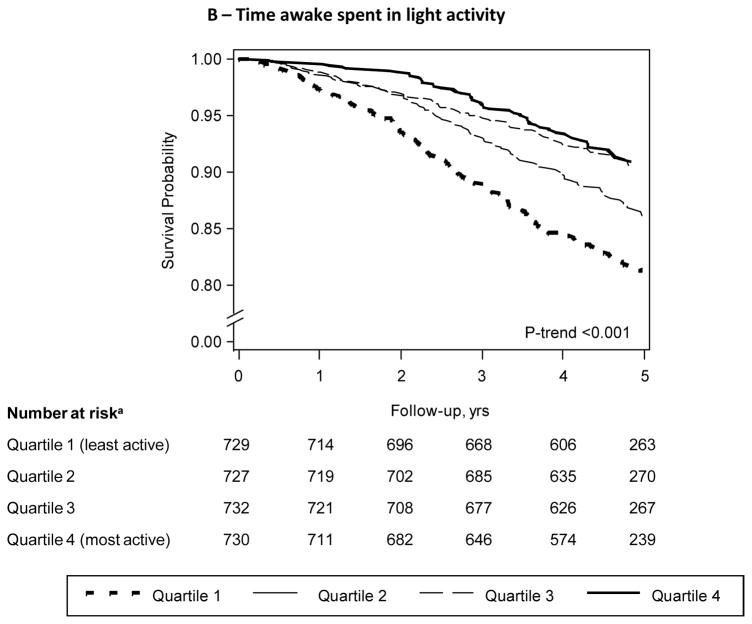
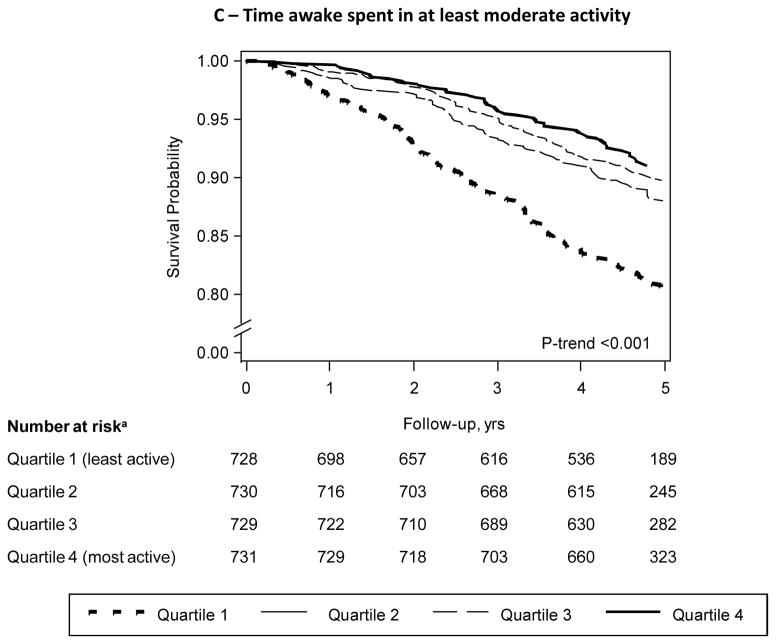
A total of 409 (14%) men died during an average(SD) follow-up of 4.5 (1.0) years. Men with greater time spent in sedentary behavior, those with less time spent in light activity and those with less time spent in at least moderate activity had a lower probability of survival (log rank test for trend <0.001 across quartiles of each activity level measure) (Figure 1a–c).
Figure 1.
Figure 1a–c. Cumulative Survival by Quartile of Activity Level Measure
Model adjusted for age, clinic, race, and season
aThe number at risk at 5 years is much smaller because not all participants had 5 years of follow-up time
Greater time spent in sedentary behavior was associated with a higher risk of death (Table 2). After adjustment for multiple confounders (age, race, site, season, education, marital status, health status, smoking, comorbidity burden, depressive symptoms, cognitive function, IADL impairments, percent body fat), men in quartile (Q) 4 (≥915 minutes [15.2 hours]) had over a 1.5-fold higher risk of all-cause mortality (HR 1.56, 95% CI 1.15–2.14) compared with men in Q1 (referent group, <772 minutes [12.7 hours]) (p-trend 0.01). Further adjustment for differences in self-reported activity, gait speed and time spent asleep did not attenuate this association (HR Q4 vs. Q1 1.79, 95% CI 1.19–2.70) (p-trend 0.02).
Table 2.
Association between Activity Level Measures and All-cause Mortality
| Relative Hazard (95% CI)
|
||||
|---|---|---|---|---|
| Activity Level Measure | Incidence rate per 1,000 person years (95% CI)a | Base modelb | Multivariable modelc | MV model + PASE + gait speed + time spent asleep |
| Time awake spent in sedentary behaviord, min/24hrs | ||||
| Q1 – least sedentary (<772.2) | 26.78 (18.49–35.07) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Q2 (772.2–844.6) | 29.21 (23.20–35.23) | 1.22 (0.90–1.67) | 1.26 (0.92–1.75) | 1.30 (0.93–1.81) |
| Q3 (844.7–914.9) | 28.64 (22.89–34.40) | 1.21 (0.89–1.65) | 1.12 (0.81–1.56) | 1.19 (0.83–1.70) |
| Q4 – most sedentary (≥915.0) | 43.95 (36.51–51.40) | 1.78 (1.33–2.38) | 1.56 (1.15–2.14) | 1.79 (1.19–2.70) |
| p-trend | <0.001 | 0.01 | 0.02 | |
| Time awake spent in light activitye, min/24hrs | ||||
| Q1 – least active (<42.4) | 47.96 (40.00–55.92) | 2.37 (1.72–3.28) | 1.70 (1.19–2.45) | 1.57 (1.08–2.29) |
| Q2 (42.4–63.9) | 31.98 (25.87–38.09) | 1.60 (1.15–2.24) | 1.42 (1.00–2.01) | 1.40 (0.98–1.99) |
| Q3 (64.0–88.3) | 23.44 (16.63–30.25) | 1.07 (0.75–1.54) | 1.06 (0.73–1.54) | 1.06 (0.73–1.54) |
| Q4 – most active (≥88.4) | 21.68 (14.94–28.42) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| p-trend | <0.001 | <0.001 | 0.006 | |
| Time awake spent in at least moderate activityf, min/24hrs | ||||
| Q1 – least active (<37.6) | 50.24 (42.21–58.28) | 2.52 (1.85–3.45) | 1.80 (1.27–2.54) | 1.58 (1.10–2.27) |
| Q2 (37.6–68.5) | 30.13 (23.88–36.69) | 1.42 (1.02–1.98) | 1.29 (0.92–1.83) | 1.19 (0.83–1.69) |
| Q3 (68.6–114.3) | 24.33 (18.46–30.19) | 1.18 (0.83–1.67) | 1.15 (0.81–1.65) | 1.12 (0.78–1.60) |
| Q4 – most active (≥114.4) | 21.23 (15.02–27.44) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| p-trend | <0.001 | <0.001 | 0.009 | |
Abbreviation: MV, Multivariable; PASE, Physical Activity Scale for the Elderly
adjusted for age
adjusted for age, race, site, and season
base model further adjusted for education, marital status, health status, smoking, comorbidity burden, depressive symptoms, cognitive function, number of Instrumental Activities of Daily Living (IADL) impairments, and percent body fat
time awake spent at Metabolic Equivalent Tasks (METs) ≤ 1.50
time awake spent at METs 1.51 to 2.99
time awake spent at METs ≥ 3.00
Less time spent in light activity and less time spent in at least moderate activity were also each associated with an increased risk of death. After adjustment for multiple potential confounders and accounting for self-reported activity, gait speed and time spent asleep, the HR (95% CI) of mortality was 1.57 (1.08–2.29) among men in Q1 (<42 minutes) compared with those in Q4 (≥88 minutes) of light activity (p-trend 0.006) and 1.58 (1.10–2.27) among men in Q1 (<38 minutes) compared with those in Q4 (≥114 minutes) of at least moderate activity (p-trend 0.009).
There was no evidence of an interaction between age(<80 vs. ≥80 years) and any activity level measure for prediction of risk of mortality. In addition, multivariable associations between each measure and mortality persisted when 51 men who died within the first year of follow-up were excluded from the analyses; multivariable HRs (95% CI) were 1.47 (1.04–1.68) for Q4 vs. Q1 of sedentary behavior, 1.49 (1.02–2.18) for Q1 vs. Q4 of light activity and 1.58 (1.10–2.27) for Q1 vs. Q4 of at least moderate activity. Excluding the 1298 men with multiple (≥2) co-morbid medical conditions from the analyses also did not substantially alter the results (data not shown), though the association between greater time spent in sedentary behavior and mortality was modestly attenuated and no longer significant.
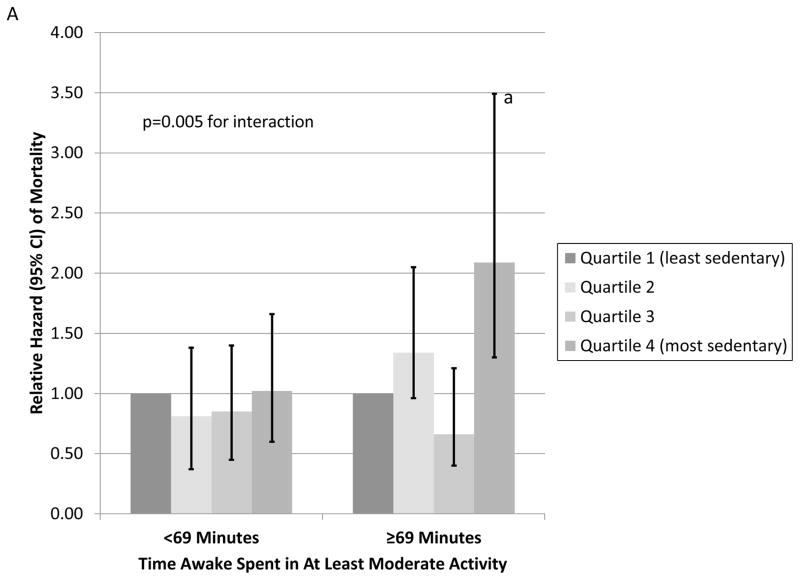
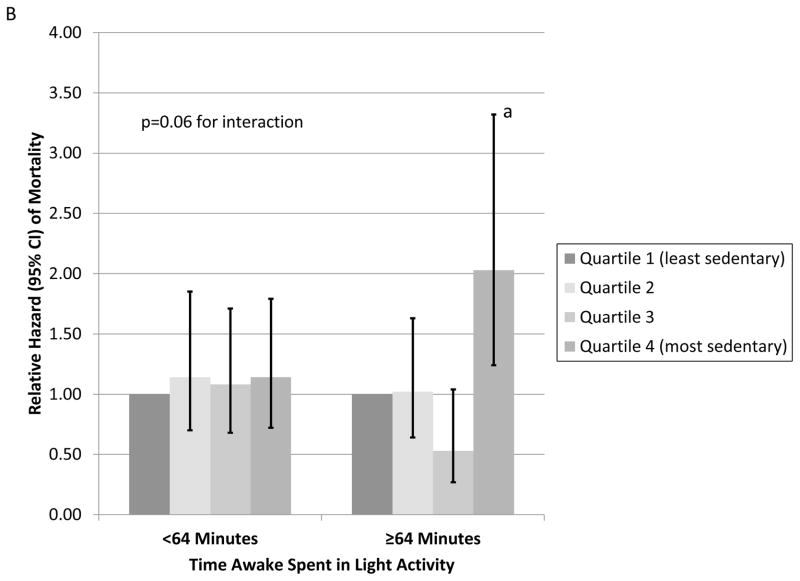
There was evidence that the association of time spent in sedentary behavior with mortality varied by time spent in light activity and time spent in at least moderate activity. For example, greater time spent in sedentary behavior was associated with an increased risk of death among men spending at least 69(median) minutes per day in at least moderate activity (multivariable HR Q4 vs. Q1 2.09 [95% CI, 1.26–3.49]), but not among those spending less time in at least moderate activity (multivariable HR Q4 vs. Q1 1.02 [95% CI, 0.62–1.66]) (p=0.005 for interaction) (Figure 2a). Similarly, greater time spent in sedentary behavior was associated with an increased risk of death among men spending at least 64 (median) minutes per day in light activity (multivariable HR Q4 vs. Q1 2.03 [95% CI, 1.24–3.32]), but not among those spending less time in light activity (HR Q4 vs. Q1 1.14 [95% CI, 0.72–1.79]) (p=0.06 for interaction) (Figure 2b).
Figure 2.
Figure 2a. Association between Time Awake Spent in Sedentary Behavior and Mortality Stratified by Time Awake Spent in at Least Moderate Activity
Models adjusted for age, race, site, and season, education, marital status, health status, smoking, comorbidity burden, depressive symptoms, cognitive function, number of Instrumental Activities of Daily Living (IADL) impairments, and percent body fat
Note: 69 minutes =median
ap<0.05, Q4 vs. Q1of time awake spent in sedentary behavior
Figure 2b. Association between Time Awake Spent in Sedentary Behavior and Mortality Stratified by Time Awake Spent in Light Activity
Models adjusted for age, race, site, and season, education, marital status, health status, smoking, comorbidity burden, depressive symptoms, cognitive function, number of Instrumental Activities of Daily Living (IADL) impairments, and percent body fat
Note: 64 minutes =median
ap<0.05, Q4 vs. Q1 of time awake spent in sedentary behavior
Activity Level Measures and Cause-Specific Mortality
Among the 409 deaths, 138 were attributed to CVD, 129 to cancer and 142 to non-CVD, non-cancer causes. The association between greater time spent in sedentary behavior and a higher risk of all-cause mortality appeared to be primarily related to increased risks of CVD and non-CVD non-cancer deaths among the most sedentary men(Table 3). Similar findings were apparent for time spent in at least moderate activity and cause-specific mortality. In contrast, there was some evidence that less time spent in light activity was associated with an increased risk of CVD death, cancer death and death due to other causes.
Table 3.
Association between Activity Level Measures and Cause-specific Mortality
| Relative Hazarda (95% CI) |
|||
|---|---|---|---|
| Activity Level Measure | Cardiovascular Death | Cancer Death | Non-CVD Non-cancer Death |
| Time awake spent in sedentary behaviorb, min/24hrs | |||
| Q1 – least sedentary (<772.2) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Q2 (772.2–844.6) | 1.59 (0.91–2.75) | 1.06 (0.62–1.80) | 1.17 (0.63–2.15) |
| Q3 (844.7–914.9) | 1.12 (0.63–2.00) | 0.84 (0.48–1.48) | 1.49 (0.84–2.64) |
| Q4 – most sedentary (≥915.0) | 1.71 (0.99–2.97) | 1.25 (0.74–2.10) | 1.82 (1.04–3.20) |
| p-trend | 0.16 | 0.52 | 0.02 |
| Time awake spent in light activityc, min/24hrs | |||
| Q1 – least active (<42.4) | 1.73 (0.90–3.34) | 1.71 (0.94–3.14) | 1.67 (0.89–3.13) |
| Q2 (42.4–63.9) | 1.92 (1.04–3.55) | 1.40 (0.78–2.49) | 1.03 (0.55–1.94) |
| Q3 (64.0–88.3) | 1.29 (0.67–2.49) | 0.92 (0.49–1.72) | 1.04 (0.54–1.99) |
| Q4 – most active (≥88.4) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| p-trend | 0.07 | 0.03 | 0.08 |
| Time awake spent in at least moderate activityd, min/24hrs | |||
| Q1 – least active (<37.6) | 2.86 (1.50–5.45) | 1.15 (0.65–2.06) | 1.80 (0.98–3.31) |
| Q2 (37.6–68.5) | 1.79 (0.94–3.42) | 1.01 (0.58–1.76) | 1.27 (0.69–2.34) |
| Q3 (68.6–114.3) | 1.60 (0.82–3.11) | 1.08 (0.62–1.87) | 0.90 (0.46–1.75) |
| Q4 – most active (≥ 114.4) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| p-trend | <0.001 | 0.70 | 0.02 |
Abbreviation: CVD, cardiovascular disease
model adjusted for age, race, site, season, education, marital status, health status, smoking, comorbidity burden, depressive symptoms, cognitive function, number of IADL impairments, and percent body fat
time awake spent at Metabolic Equivalent Tasks (METs) ≤ 1.50
time awake spent at METs 1.51 to 2.99
time awake spent at METs ≥ 3.00
DISCUSSION
Greater time spent in sedentary behavior, less time spent in light activity and less time spent in at least moderate activity during waking hours were each associated with a higher risk of death in this prospective study of older community-dwelling men. The association between greater time spent in sedentary behavior and increased mortality was most pronounced among more active men who were exceeding current recommendations on physical activity and public health in older adults. These findings suggest that physical activity guidelines should be updated to specifically encourage a reduction in sedentary time in addition to stressing participation in light and moderate activity in order to maximize longevity of aged populations.
Men in this study, on average, were sedentary while awake for 60% of the time during a 24-hour period, engaging in activities (e.g., sitting or reclining) that did not increase energy expenditure substantially above the resting level. A previous study of U.S. adults who wore an accelerometer while awake estimated that adults ≥70 years were sedentary for two-thirds of the time.6 Similarly, a prior study in older U.K. adults reported that half of the sample spent more than 80% of waking hours in sedentary behavior.32
Men spending ≥15.2 hours per day in sedentary behavior while awake compared with those spending <12.7 hours per day had a 1.5 to 1.7-fold higher risk of mortality during a follow-up of 4.5 years, even after accounting for differences in self-reported physical activity, gait speed and objectively measured sleep duration. Importantly, we found that the association of time spent in sedentary behavior with mortality depended on time spent at higher levels of activity. Among men participating in <69 minutes (1.2 hours) per day of moderate activity (and those participating in <64 minutes (1.1 hours)per day of light activity), time spent in sedentary behavior was not related to mortality suggesting that the amount of time spent in sedentary behavior does not influence longevity among less active older adults. However among more active men participating in ≥1.2 hours per day of at least moderate activity (and those participating in ≥1.1 hours per day of light activity), greater time spent in sedentary behavior conferred a 2-fold higher risk of death. This finding indicates that the relative benefit (at least in terms of mortality reduction) of physical activity among this group of men who met or exceeded current public health recommendations was least among the most sedentary individuals and supports the premise2;33 that too much sedentary time reduces the potential benefit of light or moderate activity in older adults. A previous study7 in 1906 adults with accelerometry data aged ≥50 years enrolled in NHANES reported that more sedentary time was associated with a higher risk of mortality during a follow-up of 2.8 years, even after accounting for time spent in at least moderate activity, but did not evaluate whether the association varied by time spent in moderate activity or time spent in light activity or take into account time spent asleep. In addition, prospective studies in adults34–38 using self-report instruments have found that sedentary behavior is associated with mortality, independent of physical activity level, but these instruments that may not differentiate sedentary behavior from light activity.
Less time spent in light activity and less time spent in at least moderate activity were each associated with a higher risk of death. These findings are in general agreement with results of a study8 of 302 older adults that reported that free living activity energy expenditure was associated with a lower risk of death, suggesting that any activity expenditure can help lower mortality risk. Our findings expand on these results by providing evidence that participation in usual daily (i.e., light) activity is associated with a reduction in risk of mortality.
Greater time spent in sedentary behavior and less time spent in at least moderate activity were each associated with higher risks of all-cause mortality primarily due to higher risks of CVD death and death due to non-CVD, non-cancer causes, while less time spent in light activity was associated with increased risks of CVD death, cancer death and death due to other causes. Previous studies36;38in middle aged adults have reported that self-reported sedentary behavior is associated with deaths due to CVD, cancer and other causes. Investigations in older adults22–25 have found consistent associations between self-reported physical activity and CVD death and inconsistently observed relationships between self-reported physical activity and cancer death.
Our results support current recommendations on physical activity and public health in older adults39–42 that suggest ≥30 minutes of moderate activity on five days each week to achieve health benefits. Our study with its objective measurements expands on the previous evidence for these recommendations that relied on reports of studies examining effects of self-reported physical activity on mortality.22–28 These guidelines also stress increasing moderate activity with less emphasis on attaining vigorous activity in agreement with our finding that older men spent very little time participating in vigorous activity. While our findings agree with the emphasis in current guidelines on participation in moderate activity, our results also suggest that future recommendations should stress reducing sedentary time and encourage participation in light activity. Incorporating participation in light activity into future guidelines is especially important in the aged population as many older adults may have difficulty maintaining recommended levels of moderate activity due to low levels of fitness, decreased functional capacity or existing disability.
This study has several strengths including the large well-characterized cohort with objective activity measures across the full range of levels, nearly complete follow-up, adjustment for several potential confounders, and ascertainment of cause-specific mortality. However, this study also has limitations. The cohort was comprised of predominantly healthy older men and results are not necessarily generalizable to other populations. Unhealthy individuals at increased risk of mortality are less likely to be active and more likely to be sedentary; thus, the possibility of residual confounding remains. However, associations remained after adjustment for health status and comorbidity burden and were not substantially altered when men who died within the first year of follow-up or men with multiple comorbidities were excluded from the analyses. Use of absolute MET ranges established in younger adults to define aerobic intensity categories may not be appropriate to use in older populations, but this limitation is mitigated by our evaluation of objectively measured activity across the full range of levels. Larger studies are needed to precisely quantify the independent effects of objective activity level measures on mortality risk. Finally, it is uncertain if associations will persist with longer follow-up.
In conclusion, greater time spent in sedentary behavior, less time spent in light activity and less time spent in at least moderate activity were each associated with an increased risk of mortality in older men. In particular, greater time in sedentary behavior was independently associated with higher mortality among active men meeting current guidelines about participation in physical activity in older adults. Efforts to encourage participation in both light and moderate activity and stress reduction of sedentary time may increase longevity of aged populations.
Supplementary Material
Acknowledgments
Source of Funding: The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), the National Center for Research Resources (NCRR), and NIH Roadmap for Medical Research under the following grant numbers: U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197, U01 AG027810, and UL1 TR000128.
Sponsor’s Role: The funding agencies had no direct role in the conduct of the study; the collection, management, analyses and interpretation of the data; or preparation or approval of the manuscript.
Footnotes
Meeting Presentation: Results were presented at the annual meeting of the Gerontological Society of America, November 2012, San Diego, CA.
Author Contributions:
Kristine Ensrud – Study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, and preparation of manuscript
Terri Blackwell – Analysis and interpretation of data, and critical review of manuscript
Jane Cauley – Study concept and design, acquisition of subjects and/or data, interpretation of data, and critical review of manuscript
Thuy-Tien Dam – Interpretation of data and critical review of manuscript
Peggy Cawthon – Interpretation of data and critical review of manuscript
John Schousboe – Interpretation of data and critical review of manuscript
Elizabeth Barrett-Connor – Study concept and design, acquisition of subjects and/or data, interpretation of data and critical review of manuscript
Katie Stone – Interpretation of data and critical review of manuscript
Douglas Bauer – Acquisition of subjects and/or data, interpretation of data and critical review of manuscript
James Shikany – Interpretation of data and critical review of manuscript
Dawn Mackey – Interpretation of data and critical review of manuscript
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper. Drs. Ensrud and Cauley have received grant support from the NIH (and supporting agencies) grant as listed under Funding Sources on the title page. Dr. Ensrud also serves as a consultant on a Data Monitoring Committee for Merck Sharpe & Dohme. Dr. Cawthon has received grant support from Merck and GlaskoSmithKline as well as personal fees from Eli Lilly. Dr. Schousboe has received personal fees from Merck, Inc. Dr. Barrett-Connor has received grant support from the NIH (and supporting agencies) grant as listed under Funding Sources on the title page.
References
- 1.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71:S1–14. [PubMed] [Google Scholar]
- 2.Pate RR, O’Neill JR, Lobelo F. The evolving definition of “sedentary”. Exerc Sport Sci Rev. 2008;36:173–178. doi: 10.1097/JES.0b013e3181877d1a. [DOI] [PubMed] [Google Scholar]
- 3.Matthews CE. Physical activity in the United States measured by accelerometer: comment. Med Sci Sports Exerc. 2008;40:1188. doi: 10.1249/MSS.0b013e31817057da. [DOI] [PubMed] [Google Scholar]
- 4.Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 5.Matthews CE, Hagstromer M, Pober DM, et al. Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc. 2012;44:S68–S76. doi: 10.1249/MSS.0b013e3182399e5b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koster A, Caserotti P, Patel KV, et al. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS One. 2012;7:e37696. doi: 10.1371/journal.pone.0037696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manini TM, Everhart JE, Patel KV, et al. Daily activity energy expenditure and mortality among older adults. JAMA. 2006;296:171–179. doi: 10.1001/jama.296.2.171. [DOI] [PubMed] [Google Scholar]
- 9.Blank JB, Cawthon PM, Carrion-Petersen ML, et al. Overview of recruitment for the osteoporotic fractures in men study (MrOS) Contemp Clin Trials. 2005;26:557–568. doi: 10.1016/j.cct.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 10.Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study--a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26:569–585. doi: 10.1016/j.cct.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 12.Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 14.Mackey DC, Manini TM, Schoeller DA, et al. Validation of an armband to measure daily energy expenditure in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:1108–1113. doi: 10.1093/gerona/glr101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharif MM, Bahammam AS. Sleep estimation using Body Media’s SenseWear armband in patients with obstructive sleep apnea. Ann Thorac Med. 2013;8:53–57. doi: 10.4103/1817-1737.105720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sheikh JI, Yesavage JA. Geriatric depression scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 1986;5:165–173. [Google Scholar]
- 17.Cawthon PM, Fink HA, Barrett-Connor E, et al. Alcohol use, physical performance, and functional limitations in older men. J Am Geriatr Soc. 2007;55:212–220. doi: 10.1111/j.1532-5415.2007.01062.x. [DOI] [PubMed] [Google Scholar]
- 18.Washburn RA, Smith KW, Jette AM, et al. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 19.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48:314–318. [PubMed] [Google Scholar]
- 20.Lee CG, Boyko EJ, Nielson CM, et al. Mortality risk in older men associated with changes in weight, lean mass, and fat mass. J Am Geriatr Soc. 2011;59:233–240. doi: 10.1111/j.1532-5415.2010.03245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika. 1982;69:239–241. [Google Scholar]
- 22.Gregg EW, Cauley JA, Stone K, et al. Relationship of changes in physical activity and mortality among older women. JAMA. 2003;289:2379–2386. doi: 10.1001/jama.289.18.2379. [DOI] [PubMed] [Google Scholar]
- 23.Kushi LH, Fee RM, Folsom AR, et al. Physical activity and mortality in postmenopausal women. JAMA. 1997;277:1287–1292. [PubMed] [Google Scholar]
- 24.Hakim AA, Petrovitch H, Burchfiel CM, et al. Effects of walking on mortality among nonsmoking retired men. N Engl J Med. 1998;338:94–99. doi: 10.1056/NEJM199801083380204. [DOI] [PubMed] [Google Scholar]
- 25.Bijnen FC, Caspersen CJ, Feskens EJ, et al. Physical activity and 10-year mortality from cardiovascular diseases and all causes: The Zutphen Elderly Study. Arch Intern Med. 1998;158:1499–1505. doi: 10.1001/archinte.158.14.1499. [DOI] [PubMed] [Google Scholar]
- 26.Morgan K, Clarke D. Customary physical activity and survival in later life: a study in Nottingham, UK. J Epidemiol Community Health. 1997;51:490–493. doi: 10.1136/jech.51.5.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaplan GA, Seeman TE, Cohen RD, et al. Mortality among the elderly in the Alameda County Study: behavioral and demographic risk factors. Am J Public Health. 1987;77:307–312. doi: 10.2105/ajph.77.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stessman J, Maaravi Y, Hammerman-Rozenberg R, et al. The effects of physical activity on mortality in the Jerusalem 70-Year-Olds Longitudinal Study. J Am Geriatr Soc. 2000;48:499–504. doi: 10.1111/j.1532-5415.2000.tb04995.x. [DOI] [PubMed] [Google Scholar]
- 29.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dew MA, Hoch CC, Buysse DJ, et al. Healthy older adults’ sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med. 2003;65:63–73. doi: 10.1097/01.psy.0000039756.23250.7c. [DOI] [PubMed] [Google Scholar]
- 31.Ensrud KE, Blackwell TL, Ancoli-Israel S, et al. Sleep disturbances and risk of frailty and mortality in older men. Sleep Med. 2012;13:1217–1225. doi: 10.1016/j.sleep.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Davis MG, Fox KR, Hillsdon M, et al. Objectively measured physical activity in a diverse sample of older urban UK adults. Med Sci Sports Exerc. 2011;43:647–654. doi: 10.1249/MSS.0b013e3181f36196. [DOI] [PubMed] [Google Scholar]
- 33.Owen N, Healy GN, Matthews CE, et al. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38:105–113. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dunstan DW, Barr EL, Healy GN, et al. Television viewing time and mortality: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Circulation. 2010;121:384–391. doi: 10.1161/CIRCULATIONAHA.109.894824. [DOI] [PubMed] [Google Scholar]
- 35.Katzmarzyk PT, Church TS, Craig CL, et al. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41:998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 36.Patel AV, Bernstein L, Deka A, et al. Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol. 2010;172:419–429. doi: 10.1093/aje/kwq155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Warren TY, Barry V, Hooker SP, et al. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med Sci Sports Exerc. 2010;42:879–885. doi: 10.1249/MSS.0b013e3181c3aa7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wijndaele K, Brage S, Besson H, et al. Television viewing time independently predicts all-cause and cardiovascular mortality: the EPIC Norfolk study. Int J Epidemiol. 2011;40:150–159. doi: 10.1093/ije/dyq105. [DOI] [PubMed] [Google Scholar]
- 39.Center for Disease Control and Prevention. [7-29-2013];How much physical activity do older adults need? 2011 Dec 1; http://www.cdc.gov/physicalactivity/everyone/guidelines/olderadults.html.
- 40.Davies S, Burns H, Jewell T, et al. Start active, stay active: a report on physical activity for health from the four home countries’. [10-10-2013];Chief Medical Officers. 2011 [Google Scholar]
- 41.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 42.World Health Organization. Physical activity and older adults. [7-29-2013];Recommended levels of physical activity for adults aged 65 and above. 2013 http://www.who.int/dietphysicalactivity/factsheet_olderadults/en/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.