Abstract
Objective
This study was conducted to compare the relative, clinical intraocular dose distribution for palladium-103 (103Pd) versus iodine-125 (125I) ophthalmic plaque radiation therapy.
Methods
Preoperative comparative radiation dosimetry was performed to evaluate 319 consecutive uveal melanomas treated between 2006 and 2012.
Results
There were 68 (21.3 %) anterior (iris and/or ciliary body) and 251 (78.7 %) choroidal melanomas examined in this study. According to AJCC staging, 7th edition, 146 (45.8 %) were T1, 126 (39.5 %) T2, 40 (12.5 %) T3, and 7 (2.2 %) T4. All were prescribed an equivalent tumor-apex dose. When compared to 125I, 103Pd was associated with a mean 41.9 % lower radiation dose to the opposite eye wall (p < 0.001), 12.7 % to the lens center (p < 0.001), 7.5 % to the optic disc (p = 0.008), and a 3.8 % decrease to the fovea (p = 0.034). However, subgroup analysis of smaller (T1-staged) tumors showed greater dose reductions to normal ocular structures compared to larger (T4-staged) tumors. Tumor and therefore plaque location also affected intraocular dose distribution. For example, palladium-103-related dose reductions to the fovea, optic nerve, and opposite eye wall were significantly greater for iris and ciliary body tumors compared to posterior choroidal melanomas (p < 0.001). After comparative dosimetry, 98.7 % (n = 315/319) were treated with 103Pd.
Conclusion
Preoperative comparative radiation dosimetry was performed for a large cohort of patients with uveal melanoma. It influenced radionuclide selection, offered an opportunity for radiation sparing of critical vision-related intraocular structures, and typically increased radiation within the tumors.
Keywords: Brachytherapy, Plaque, Palladium-103, Iodine-125, Choroidal melanoma
Introduction
Complications of plaque brachytherapy have been related to dose to normal ocular structures [1–5]. However, little has been written about methods to diminish unnecessary irradiation outside the targeted treatment volume [6–10, 5, 11].
In 1990, the first preclinical pilot studies used computer simulations and then thin layer dosimeter (TLD)-laden frozen eye bank eyes to compare 103Pd and 125I ocular dose distributions [8]. For an equivalent tumor target dose, the less energetic (21 keV) 103Pd-photons were more quickly absorbed than those from the (28 keV) 125I plaques within the eye and vitreous before it reached the episcleral dosimeters. In clinical practice, it was reasonable to assume that when outside the targeted volume (beneath the plaque), there would be relative 103Pd-related dose reductions to the macula, optic nerve, and lens. In 2009, the clinical results of 400 cases of choroidal melanoma treated by 103Pd ophthalmic plaque therapy demonstrated improved local control and visual acuity outcomes compared to other series using 125I [12].
In 2011, the American Association of Physicists in Medicine (AAPM) Task Group-129 (TG-129) examined the relative ocular dose distributions of 125I versus 103Pd plaque treatment for a single moderately sized T1 tumor and found relative dose advantages with the use of 103Pd [11]. In a second publication together with the American Brachytherapy Society (ABS), the AAPM TG-129 suggested that comparative preoperative dosimetry could improve clinical care [13]. Most recently, the ABS Ophthalmic Oncology Task Force guidelines reached consensus that a pretreatment comparison of available sources be employed prior to plaque therapy [14].
Since 2006, at The New York Eye Cancer Center and affiliated hospitals, we have routinely compared 125I to 103Pd prior to ophthalmic plaque brachytherapy. Utilizing data from those evaluations, we present the largest clinical case series of preoperative intraocular dosimetric comparisons for ophthalmic plaque brachytherapy for uveal melanoma.
Methods
Clinical evaluation and diagnosis
Preoperative comparative (103Pd versus 125I) dosimetry calculations were performed for 319 uveal melanoma patients treated between 2006 and 2012. Patients were diagnosed with uveal melanoma by clinical examination. A combination of ophthalmoscopy, fluorescein angiography, transillumination, and B-scan ultrasound were used to determine the tumor’s basal dimensions and apical height. Anterior uveal tumors (defined as iris and ciliary body melanomas) were assessed by slit-lamp biomicroscopy, gonioscopy, high-frequency ultrasound imaging and photography. Our methods of diagnosis are consistent with that described in the ABS/AAPM TG-129 report [13]. All tumors were T-staged according to the American Joint Committee on Cancer (AJCC) System, 7th edition [15–18].
Dosimetric calculations and treatment
Preoperative dosimetry calculations for 103Pd and 125I were performed to be comparable to the COMS protocol and followed the current recommendations of the American Association of Physicists in Medicine Task Group-43 (AAPM TG-43) [19, 13, 11, 20–22]. Thus, seeds were calculated as approximate isotropic point sources with no corrections for anisotropy. No attenuation was attributed to the acrylic fixative or for the gold plaque sidewalls. The backscatter effects from the plaque’s posterior wall were discounted. A 103Pd specific dose rate constant of 0.686 cGy/h/mCi was used. The radial dose function was obtained from published data [23–25]. The prescription point was the tumor’s apex, consistent with the 2003 and most current ABS recommendations [22, 14].
We chose to analyze four points along the central axis of the plaque: inner sclera, 5-mm axial depth, opposite retina, and the tumor’s apex. Due to their importance for visual acuity, additional intraocular locations included: the fovea, optic disc, and lens.
Statistical analysis
Comparison of the 103Pd and 125I ophthalmic plaque doses was computed using the Mann–Whitney U test. A confidence interval (CI) of 95 % was generated from the statistical analysis. In comparison of 103Pd and 125I ophthalmic plaque doses, a P value < 0.05 was considered statistically significant.
Results
Tumor characteristics
There were 319 uveal melanomas evaluated by comparative dosimetry between 2006 and 2012. They had a mean 4.0 mm apical height (range 1.8–14.2) and a mean 9.9 mm basal dimension (range 1.8–21). The majority were AJCC T1 and T2 stages at 45.8 % and 39.5 %, respectively (Table 1). This is comprised of iris or ciliary body (n = 68/319, 21.3 %), but majority were choroidal melanomas (n = 251/319, 78.7 %).
Table 1.
Melanoma characteristics and location
| Percentages (n)* | ||
|---|---|---|
| Tumor stage | T1 | 45.8 % (146) |
| T2 | 39.5 % (126) | |
| T3 | 12.5 % (40) | |
| T4 | 2.2 % (7) | |
| Tumor location | Anterior (iris and ciliary body) | 21.3 % (68) |
| Choroid | 78.7 % (251) |
n number of patients
Comparative dosimetry
Central axis dose
All treatment plans were analyzed for the relative dose deposition along the central axis of the plaque (inner sclera, 5 mm and opposite eye wall). By definition, the tumor’s apex received a mean equivalent dose for both radionuclides (Fig. 1). However, the use of 103Pd (versus 125I) was associated with a mean 10.4 % increase in dose to the inner scleral base (p = 0.040) and a 1.1 % increase at 5-mm axial depth (p = 0.031) for that equivalent tumor-apex dose. Therefore, the use of 103Pd was found to steepen the dose gradient within the tumor. Specifically, for an equivalent tumor-apex dose, the use of 103Pd increased the mean radiation dose within the tumor by mean 7.6 % (157.9 versus 146.7 Gy) compared to 125I.
Fig. 1.
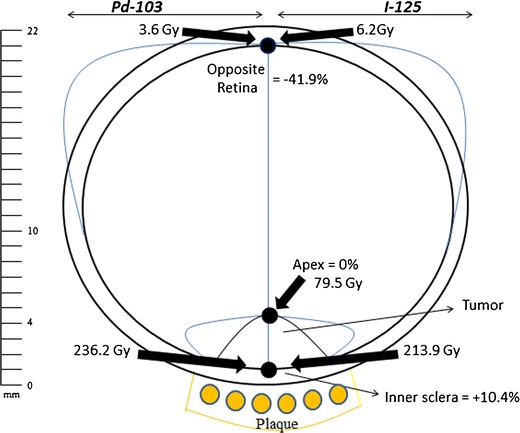
Dose gradient along the central axis of the plaque
Then as the lower energy 103Pd photons continue along the central axis across the eye, they were more rapidly absorbed (in the vitreous) before it reached the opposite eye wall (Fig. 1). At that data point, the use of 103Pd resulted in a 41.9 % reduction of radiation dose (p < 0.001).
Dose to critical intraocular structures
Vision retention is related to the function of certain critical radiosensitive intraocular structures. Therefore, we compared the radiation dose to the natural lens center, optic nerve, and fovea. Depending on the intraocular location of the tumor (and therefore the plaque), these critical structures can be located either within or outside the target volume [26]. In this series, the use of 103Pd (versus 125I) demonstrated overall mean reductions to these critical intraocular structures (Table 2). Specifically, the optic disc and fovea showed a mean 103Pd-related reduction of 7.5 % (p = 0.008) and 3.8 % (p = 0.034), respectively. The lens center showed a greater mean 103Pd-related radiation dose reduction of 12.7 % (p < 0.001).
Table 2.
Preoperative dosimetry for all melanomas, melanomas of the iris and ciliary body, and posterior choroidal melanomas
| All tumors 103Pd: mean dose, Gy | All tumors 125I: mean dose, Gy | Mean absolute dose difference between 103Pd and 125I, Gy | Mean 103Pd change relative to mean 125I dose, percent | P value | Anterior tumors 103Pd: mean dose, Gy | Anterior tumors 125I: mean dose, Gy | Mean absolute dose difference between 103Pd and 125I, Gy | Mean 103Pd change relative to mean 125I dose, percent | P value | Posterior Choroidal tumors 103Pd: mean dose, Gy | Posterior Choroidal tumors 125I: mean dose, Gy | Mean absolute dose difference between 103Pd and 125I, Gy | Mean 103Pd change relative to mean 125I dose, % | P value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N = 319 | N = 319 | N = 319 | N = 319 | N = 68 | N = 68 | N = 68 | N = 68 | N = 251 | N = 251 | N = 251 | N = 251 | ||||
| Inner sclera (beneath the plaque) | 236.2, CI 222.1–250.3 | 213.9, CI 204.0–223.8 | 22.3 | +10.4 % | 0.040 | 234.5, CI 196.6–272.4 | 215.2, CI 188.6–241.7 | 19.3 | +9.0 % | 0.575 | 236.7, CI 221.9–251.5 | 213.6, CI 203.1–224.1 | 27.1 | +10.8 % | 0.062 |
| 5-mm Depth | 64.8, CI 60.0–70.0 | 64.1, CI 60.3–67.9 | 0.7 | +1.1 % | 0.031 | 59.3, CI 45.6–72.3 | 58.9, CI 48.2–69.3 | 0.4 | +0.7 % | 0.024 | 66.4, CI 61.4–71.3 | 65.6, CI 61.6–69.5 | 0.8 | +1.2 % | 0.101 |
| Prescription point (apex of tumor) | 79.5, CI 78.6–80.4 | 79.5, CI 78.7–80.4 | 0.0 | 0.0 % | 1.000 | 81.2, CI 79.3–83.1 | 81.2, CI 79.3–83.1 | 0.0 | 0.0 % | 0.998 | 79.0, CI 78.0–80.0 | 79.0, CI 78.0–80.0 | 0.0 | 0.0 % | 1.000 |
| Opposite retina | 3.6, CI 3.0–4.2 | 6.2, CI 5.4–7.0 | 2.6 | −41.9 % | <0.001 | 3.1, CI 2.0–4.3 | 5.3, CI 3.9–6.7 | 2.2 | −41.5 % | <0.001 | 3.7, CI 3.0–4.4 | 6.5, CI 5.5–7.4 | 2.8 | −43.1 % | <0.001 |
| Lens center | 20.0, CI 17.5–22.4 | 22.9, CI 20.6–25.1 | 2.9 | −12.7 % | <0.001 | 42.9, CI 37.6–48.1 | 45.0, CI 40.2–49.8 | 2.1 | −4.7 % | 0.285 | 13.7, CI 11.5–15.9 | 17.8, CI 14.7–21.0 | 4.1 | −23.0 % | <0.001 |
| Optic disc | 28.4, CI 24.1–32.7 | 30.7, CI 26.7–34.6 | 2.3 | −7.5 % | 0.008 | 6.8, CI 1.4–12.3 | 8.5, CI 3.9–13.0 | 1.7 | −20.0 % | <0.001 | 34.3, CI 29.2–39.3 | 36.7, CI 32.1–41.3 | 2.4 | −6.5 % | 0.040 |
| Macula (fovea) | 37.9, CI 33.0–42.8 | 39.4, CI 34.8–44.0 | 1.5 | −3.8 % | 0.034 | 7.4, CI 1.4–13.4 | 8.9, CI 3.8–14.0 | 1.5 | −16.9 % | <0.001 | 46.2, CI 40.5–51.8 | 47.7, CI 42.5–52.9 | 1.5 | −3.1 % | 0.175 |
Gy Gray, CI 95 % confidence interval
Dose is given in Gray (1 Gy = 100 cGy = 100 Rad)
Comparing anterior versus posterior tumor location
The subgroups of 68 anterior (iris and ciliary body) and 251 choroidal melanomas had relatively equivalent mean apical heights (3.8 versus 4.1 mm, respectively). Thus, both groups generally resulted in 103Pd-related increased radiation dose to the subjacent inner sclera and to the 5-mm axial depth (Fig. 1). Similarly, the use of 103Pd reduced the radiation dose to the opposite retina by 41.5 % (p < 0.001) and 43.1 % (p < 0.001) for anterior and posterior melanomas, respectively.
However, this subgroup analysis (anterior versus posteriorly located tumors) also revealed that the tumors’ relative distance to the lens, fovea, and optic disc was markedly different (Fig. 2). Specifically, anterior tumors were in closer proximity to the natural lens and farther from the macular fovea and optic disc. Conversely, posterior tumors were in closer proximity to the fovea and optic disc. These differences were found to affect the relative dose distributions for 103Pd versus 125I plaques.
Fig. 2.
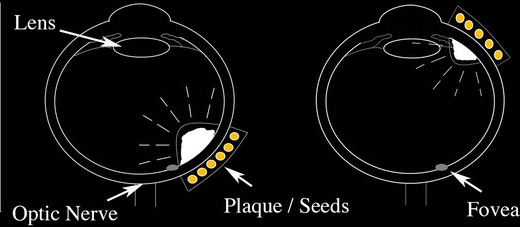
Tumor location affects distance to critical normal ocular structures
Specifically, in treatment of anterior tumors, 103Pd offered relative dose reductions of a mean 4.7 % (p = 0.285) to the relatively close lens. However, in treatment of posteriorly located melanomas, the use of 103Pd reduced the lens dose by 23.0 % (p < 0.001). Similarly, in evaluation of the fovea and optic disc, the subset of anteriorly located tumors revealed mean 103Pd-related dose reductions of 16.9 % (p < 0.001) to the fovea and 20.0 % (p < 0.001) to the optic disc. However, by comparative dosimetry for the subset of posteriorly located choroidal melanomas, mean103Pd-related dose reductions were 3.1 % (p = 0.175) to the fovea and 6.5 % (p = 0.040) to the optic nerve. This analysis revealed that 103Pd typically reduced the mean dose to the lens, fovea, and optic disc. However, the magnitude of that difference was dependent on distance.
AJCC T stage tumor comparison
Dosimetry of 103Pd versus 125I was also analyzed by AJCC T staging (Table 3). The most significant differences were noted between the relatively small T1 and the large T4 melanomas. For example, axial dosimetry for T1-staged tumors (n = 146) and T4-staged tumors (n = 7) revealed that 103Pd was associated with a mean increase in dose to the inner sclera of 4.5 % (p = 0.066) versus 32.2 % (p = 0.208), respectively. This shows that while all tumors received a higher mean scleral dose using 103Pd, the dose difference increased with tumor size. Similarly, the radiation dose to a 5-mm axial depth demonstrated a decrease of 6.6 % with 103Pd for the relatively short T1 tumors and an increase of 24.2 % for T4 tumors (Fig. 3).
Table 3.
Preoperative dosimetry for stages T1–T4 melanomas
| T1 tumors 103Pd: mean dose, Gy | T1 tumors 125I: mean dose, Gy | Mean absolute dose difference between 103Pd and 125I, Gy | Mean 103Pd change relative to mean 125I dose, percent | P value | T2 tumors 103Pd: mean dose, Gy | T2 tumors 125I: mean dose, Gy | Mean absolute dose difference between 103Pd and 125I, Gy | Mean 103Pd change relative to mean 125I dose, percent | P value | |
| N = 146 | N = 146 | N = 146 | N = 146 | N = 126 | N = 126 | N = 126 | N = 126 | |||
| Inner sclera (beneath the plaque) | 177.7, CI 156.9–198.5 | 170.0, CI 155.4–184.6 | 7.7 | +4.5 % | 0.066 | 233.5, CI 218.0–249.1 | 215.4, CI 203.8–227.0 | 18.1 | +8.4 % | 0.131 |
| 5-mm depth | 42.5, CI 35.3–49.7 | 45.5, CI 39.8–51.2 | 3.0 | −6.6 % | <0.001 | 65.4, CI 60.4–70.3 | 66.2, CI 61.8–70.5 | 0.8 | −1.2 % | 0.516 |
| Prescription point (apex of tumor) | 82.4, CI 81.1–83.7 | 82.4, CI 81.1–83.7 | 0.0 | 0.0 % | 0.999 | 79.8, CI 78.7–80.8 | 79.8, CI 78.7–80.8 | 0.0 | 0.0 % | 0.999 |
| Opposite retina | 1.9, CI 1.0–2.8 | 3.7, CI 2.5–4.9 | 1.7 | −45.9 % | <0.001 | 3.6, CI 2.9–4.3 | 6.8, CI 5.3–8.2 | 3.2 | −47.1 % | <0.001 |
| Lens center | 12.9, CI 9.3–16.5 | 15.7, CI 12.4–19.0 | 2.8 | −17.8 % | <0.001 | 21.8, CI 18.4–25.3 | 25.3, CI 22.0–28.6 | 3.5 | −13.8 % | 0.001 |
| Optic disc | 23.9, CI 17.5–30.3 | 26.4, CI 20.5–32.3 | 2.5 | −9.5 % | 0.039 | 29.6, CI 22.0–37.2 | 31.6, CI 24.6–38.6 | 2.0 | −6.3 % | 0.064 |
| Macula (fovea) | 32,8, CI 25.6–40.0 | 35.2, CI 28.4–42.0 | 2.4 | −6.8 % | 0.091 | 37.7, CI 29.8–45.6 | 39.0, CI 31.6–46.4 | 1.3 | −3.3 % | 0.142 |
| T3 tumors 103Pd: mean dose, Gy | T3 tumors 125I: mean dose, Gy | Mean absolute dose difference between 103Pd and 125I, Gy | Mean 103Pd change relative to mean 125I dose, percent | P value | T4 tumors 103Pd: mean dose, Gy | T4 tumors 125I: mean dose, Gy | Mean absolute dose difference between 103Pd and 125I, Gy | Mean 103Pd change relative to mean 125I dose, percent | P value | |
| N = 40 | N = 40 | N = 40 | N = 40 | N = 7 | N = 7 | N = 7 | N = 7 | |||
| Inner sclera (beneath the plaque) | 386.3, CI 337.7–434.8 | 321.2, CI 289.3–353.2 | 65.1 | +20.3 % | 0.051 | 647.8, CI 394.8–900.9 | 490.0, CI 330.5–649.5 | 157.8 | +32.2 % | 0.208 |
| 5-mm Depth | 118.5, CI 101.4–135.6 | 107.4, CI 94.3–120.5 | 11.1 | +10.3 % | 0.308 | 210.3, CI 127.9–292.8 | 169.3, CI 114.4–224.2 | 41.0 | +24.2 % | 0.401 |
| Prescription point (apex of tumor) | 70.8, CI 67.4–74.2 | 70.8, CI 67.4–74.2 | 0.0 | 0.0 % | 0.996 | 62.6, CI 51.0–74.3 | 62.6, CI 51.0–74.3 | 0.0 | 0.0 % | 0.952 |
| Opposite retina | 8.4, CI 4.5–12.5 | 12.0, CI 8.2–15.9 | 3.6 | −30.0 % | <0.001 | 11.5, CI 7.0–16.0 | 16.4, CI 11.1–21.7 | 4.9 | −29.9 % | 0.208 |
| Lens center | 31.9, CI 21.4–42.4 | 34.5, CI 25.5–43.5 | 2.6 | −7.5 % | 0.159 | 50.9, CI −1.7–103.5 | 49.2, CI 8.4–90.1 | 1.7 | +3.5 % | 0.998 |
| Optic disc | 37.3, CI 27.5–47.1 | 40.2, CI 30.9–49.5 | 2.9 | −7.2 % | 0.407 | 65.2, CI 35.1–95.3 | 63.2, CI 40.5–86.0 | 2.0 | +3.2 % | 0.912 |
| Macula (fovea) | 54.0, CI 37.6–70.3 | 53.6, CI 39.8–67.5 | 0.4 | +0.7 % | 0.582 | 56.6, CI −2.2–115.4 | 54.0, CI 7.6–100.4 | 2.6 | +4.8 % | 0.910 |
Dose is given in Gy = Gray (1 Gy = 100 cGy = 100 Rad), CI = 95 % confidence interval
Fig. 3.
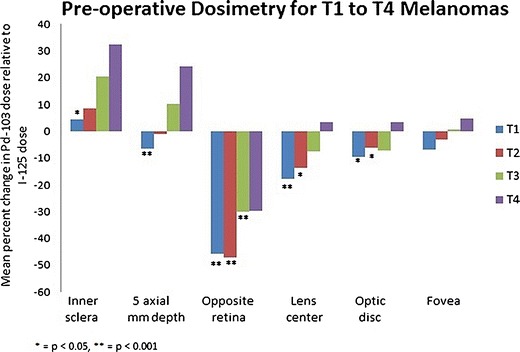
Mean percent change in dose when comparing 103Pd versus 125I
Once the radiation extended beyond the equivalent tumor-apex prescription dose, 103Pd radiation was absorbed by the vitreous before reaching the opposite eye wall. Dose to this data point was also affected by tumor height. For example, in treatment of taller tumors, there was less intervening vitreous or distance to the opposite eye wall. Thus, 103Pd-related mean dose reductions to the opposite eye wall were 45.9 % (p < 0.001) for T1 tumors versus 29.9 % (p = 0.208) for T4 tumors (Table 3).
However, all the important anatomical ocular structures (lens center, optic disc, and fovea) demonstrated mean dose reduction with 103Pd versus 125I for T1 to T3 tumors (Fig. 3). Here, comparative dosimetry revealed that the use of 103Pd decreased the mean dose to the opposite eye wall, while 103Pd increased the mean dose to the lens, optic disc, and fovea in T4-staged uveal melanomas (Fig. 3). Detailed subset analysis demonstrated that the use of 103Pd would increase the dose (for T4-staged tumors) to the lens and fovea in three eyes (n = 3/7, 43 %) and to the optic disc in two eyes (n = 2/7, 29 %). No eye with a tumor in the T4 subset exhibited a relative increase to all three ocular structures (optic disc, fovea, and lens) using 103Pd.
Patients treated with 125I plaques
There were 315 patients (98.7 %) who received 103Pd plaque therapy and four patients who received 125I plaque therapy. The four tumors treated with 125I had a mean 11.7 mm apical height (range 8.2 to 14.2) and a mean 16.1 mm basal dimension (range 13.9–17.9). The distance from the tumor edge to the macula and optic disk ranged from 0 to 3.4 mm and from 0 to 3.9 mm, respectively. Of these four tumors, two were T3 and two were T4 tumors. In those four 125I-treated eyes, the lens received an increased 125I dose of 12.6 % relative to that of 103Pd. However, it was the mean 125I-related dose reduction at the optic disc and fovea (10.5 and 16.0 %, respectively) that was the main reason for using 125I. Overall, three patients received lower optic disc dose due to the use of 125I and all four patients received lower fovea dose with 125I.
Discussion
Comparative clinical dosimetry was used to analyze intraocular dose distribution prior to radiation therapy for 319 uveal melanomas. Specifically, lower energy 103Pd was compared to relatively higher energy 125I seeds for ophthalmic plaque therapy. Evaluations along the central axis of the plaque revealed that the scleral dose was higher utilizing 103Pd. Therefore, with an equivalent planned apex prescription, the use of 103Pd increased the mean tumor dose. In addition, the opposite eye wall was both the farthest from the plaque and best represented organ dose. Here, the use of 103Pd was associated with an overall reduction of 41.9 % (p < 0.001). In comparison of critical targets for vision preservation, there were modest overall 103Pd-related dose reductions to the lens, optic disc, and fovea. While subset analysis of anteriorly located uveal melanomas revealed significantly greater 103Pd-related sparing of the optic disc and fovea, dosimetry for the posterior choroidal melanomas revealed more significant mean dose reductions to the lens.
Tumor size also influenced the intraocular dose distribution. In comparison of 103Pd versus 125I, increased T staging as per AJCC, 7th edition, was associated with relatively more tumor irradiation with 103Pd. For example, from T1 to T4, the mean percent increase in dose to the inner sclera rose from 4.5 % (p = 0.066), 8.4 % (p = 0.131), 20.3 % (p = 0.051), and 32.2 % (p = 0.208), respectively. Conversely, the mean percent decrease in dose to the opposite retina provided by 103Pd relative to 125I trended to diminish as the tumors get larger, T1 45.92 % (p < 0.001), T2 47.1 % (p < 0.001), T3 30.0 % (p < 0.001), and T4 29.9 % (p = 0.208). As their edges were more likely to be in close proximity to the lens center, optic disc, and fovea, higher T-staged (larger uveal melanomas) exhibited smaller percent differences between radionuclides. In these cases, it was not uncommon to find the calculated dose to these critical ocular structures beyond published tolerances. In addition, our decisions to use 103Pd were related to dose savings to the opposite eye wall in an effort to diminish organ dose.
The majority of tumors were treated with 103Pd, but 1.3 % tumors (n = 4/319) received 125I. In general, the decision to use 125I was influenced by the higher mean 103Pd dose at the optic disc (10.5 %) and fovea (16.0 %). The increased 103Pd dose at the optic disc and fovea was affected by the large tumor apical height and proximity of the optic disc and fovea to the tumor edge.
The limitations of this study include the following: it is from a single center, it was retrospective, and there was a small sample size of T4 tumors. Furthermore, the dosimetry calculations in this series assumed homogeneous water-equivalent tissues consistent with TG-43. The 2012 AAPM and ABS TG-129 recommended computing both homogenous and heterogeneous dose calculations as part of the preoperative plaque planning [13]. They noted that there can be large variations in doses between the two methods and that plaques often have heterogeneous material within that can affect dose calculations to normal intraocular structures [13]. Dosimetric calculations in this study also neglected anisotropy correction recommended by TG-43 to be in agreement with COMS practice [21, 23, 11]. As there are no universally accepted clinical dosimetry methods used at multiple ophthalmic brachytherapy centers, we present our findings as relatively equivalent to standard clinical practice during our period of recruitment. Though we recognize that different dosimetry methods may change the absolute numbers, there is no reason to believe they would change the dose distribution trends revealed by this work.
Conclusion
This study demonstrates that pretreatment comparative dosimetry can be used to evaluate the intraocular distribution of radiation and aid radionuclide selection. Our study revealed that when comparing 125I versus 103Pd plaque therapy for uveal melanoma, both tumor size and location affected the relative dose to critical normal intraocular structures. In 319 patients, the use of 103Pd resulted in a trend toward increased dose within the tumor target volume and decreased dose to most normal ocular structures.
Acknowledgments
This work was supported by The Eye Cancer Foundation (http://eyecancerfoundation.net).
Conflict of interest
Paul T. Finger, Di Zhou, Nina Kalach, Ekaterina Semenova, and Walter Choi declare they have no conflict of interest.
Ethical standards
Chart review, data collection, and analysis were collected in accordance with the ethical standards of The New York Eye Cancer Center committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, as well as the Health Insurance Portability and Accountability Act of 1996. All persons gave their informed consent prior to their inclusion in the study.
References
- 1.Finger PT. Radiation therapy for choroidal melanoma. Surv Ophthalmol. 1997;42(3):215–232. doi: 10.1016/S0039-6257(97)00088-X. [DOI] [PubMed] [Google Scholar]
- 2.Finger PT, Chin KJ, Yu GP, Palladium-103 for Choroidal Melanoma Study G Risk factors for radiation maculopathy after ophthalmic plaque radiation for choroidal melanoma. Am J Ophthalmol. 2010;149(4):608–615. doi: 10.1016/j.ajo.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 3.Finger PT, Chin KJ, Yu GP, Patel NS, Palladium-103 for Choroidal Melanoma Study G Risk factors for cataract after palladium-103 ophthalmic plaque radiation therapy. Int J Radiat Oncol Biol Phys. 2011;80(3):800–806. doi: 10.1016/j.ijrobp.2010.02.051. [DOI] [PubMed] [Google Scholar]
- 4.Finger PT. Tumour location affects the incidence of cataract and retinopathy after ophthalmic plaque radiation therapy. Br J Ophthalmol. 2000;84(9):1068–1070. doi: 10.1136/bjo.84.9.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yousef YA, Finger PT. Lack of radiation maculopathy after palladium-103 plaque radiotherapy for iris melanoma. Int J Radiat Oncol Biol Phys. 2012;83(4):1107–1112. doi: 10.1016/j.ijrobp.2011.09.033. [DOI] [PubMed] [Google Scholar]
- 6.Finger PT, Ho TK, Fastenberg DM, Hyman RA, Stroh EM, Packer S, Perry HD. Intraocular radiation blocking. Invest Ophthalmol Vis Sci. 1990;31(9):1724–1730. [PubMed] [Google Scholar]
- 7.Oliver SC, Leu MY, DeMarco JJ, Chow PE, Lee SP, McCannel TA. Attenuation of iodine 125 radiation with vitreous substitutes in the treatment of uveal melanoma. Arch Ophthalmol. 2010;128(7):888–893. doi: 10.1001/archophthalmol.2010.117. [DOI] [PubMed] [Google Scholar]
- 8.Finger PT, Moshfeghi DM, Ho TK. Palladium 103 ophthalmic plaque radiotherapy. Arch Ophthalmol. 1991;109(11):1610–1613. doi: 10.1001/archopht.1991.01080110148053. [DOI] [PubMed] [Google Scholar]
- 9.Finger PT, Lu D, Buffa A, DeBlasio DS, Bosworth JL. Palladium-103 versus iodine-125 for ophthalmic plaque radiotherapy. Int J Radiat Oncol Biol Phys. 1993;27(4):849–854. doi: 10.1016/0360-3016(93)90459-9. [DOI] [PubMed] [Google Scholar]
- 10.Semenova E, Finger PT. Palladium-103 radiation therapy for small choroidal melanoma. Ophthalmology. 2013;120(11):2353–2357. doi: 10.1016/j.ophtha.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 11.Rivard MJ, Chiu-Tsao ST, Finger PT, Meigooni AS, Melhus CS, Mourtada F, Napolitano ME, Rogers DWO, Thomson RM, Nath R. Comparison of dose calculation methods for brachytherapy of intraocular tumors. Med Phys. 2011;38(1):306–316. doi: 10.1118/1.3523614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finger PT, Chin KJ, Duvall G, Palladium-103 for Choroidal Melanoma Study G Palladium-103 ophthalmic plaque radiation therapy for choroidal melanoma: 400 treated patients. Ophthalmology. 2009;116(4):790–796. doi: 10.1016/j.ophtha.2008.12.027. [DOI] [PubMed] [Google Scholar]
- 13.Chiu-Tsao ST, Astrahan MA, Finger PT, Followill DS, Meigooni AS, Melhus CS, Mourtada F, Napolitano ME, Nath R, Rivard MJ, Rogers DW, Thomson RM. Dosimetry of (125)I and (103)Pd COMS eye plaques for intraocular tumors: report of task group 129 by the AAPM and ABS. Med Phys. 2012;39(10):6161–6184. doi: 10.1118/1.4749933. [DOI] [PubMed] [Google Scholar]
- 14.The American Brachytherapy Society Ophthalmic Oncology Task Force (submitted for review) The 2013 American Brachytherapy Society (ABS) guidelines for plaque brachytherapy of uveal melanoma and retinoblastoma. Brachytherapy [DOI] [PubMed]
- 15.Malignant Melanoma of the Uvea . In: AJCC cancer staging manual. 7. Stephen B, Edge DRB, Compton CC, Fritz AG, Greene FL, Trotti A III, editors. New York: Springer; 2009. pp. 547–559. [Google Scholar]
- 16.Kivela T, Kujala E. Prognostication in eye cancer: the latest tumor, node, metastasis classification and beyond. Eye. 2013;27(2):243–252. doi: 10.1038/eye.2012.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kujala E, Damato B, Coupland SE, Desjardins L, Bechrakis NE, Grange JD, Kivela T. Staging of ciliary body and choroidal melanomas based on anatomic extent. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31(22):2825–2831. doi: 10.1200/JCO.2012.45.2771. [DOI] [PubMed] [Google Scholar]
- 18.Shields CL, Kaliki S, Furuta M, Fulco E, Alarcon C, Shields JA. American joint committee on cancer classification of posterior uveal melanoma (tumor size category) predicts prognosis in 7731 patients. Ophthalmology. 2013;120(10):2066–2071. doi: 10.1016/j.ophtha.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 19.Astrahan MA, Szechter A, Finger PT. Design and dosimetric considerations of a modified COMS plaque: the reusable “seed-guide” insert. Med Phys. 2005;32(8):2706–2716. doi: 10.1118/1.1993828. [DOI] [PubMed] [Google Scholar]
- 20.Earle J, Kline RW, Robertson DM. Selection of iodine 125 for the collaborative ocular melanoma study. Arch Ophthalmol. 1987;105(6):763–764. doi: 10.1001/archopht.1987.01060060049030. [DOI] [PubMed] [Google Scholar]
- 21.Ray SK, Bhatnagar R, Hartsell WF, Desai GR. Review of eye plaque dosimetry based on AAPM task group 43 recommendations. American Association of Physicists in Medicine. Int J Radiat Oncol Biol Phys. 1998;41(3):701–706. doi: 10.1016/S0360-3016(97)00568-3. [DOI] [PubMed] [Google Scholar]
- 22.Nag S, Quivey JM, Earle JD, Followill D, Fontanesi J, Finger PT, American Brachytherapy Society The american brachytherapy society recommendations for brachytherapy of uveal melanomas. Int J Radiat Oncol Biol Phys. 2003;56(2):544–555. doi: 10.1016/S0360-3016(03)00006-3. [DOI] [PubMed] [Google Scholar]
- 23.Rivard MJ, Coursey BM, DeWerd LA, Hanson WF, Huq MS, Ibbott GS, Mitch MG, Nath R, Williamson JF. Update of AAPM task group no. 43 report: a revised AAPM protocol for brachytherapy dose calculations. Med Phys. 2004;31(3):633–674. doi: 10.1118/1.1646040. [DOI] [PubMed] [Google Scholar]
- 24.Beyer D, Nath R, Butler W, Merrick G, Blasko J, Nag S, Orton C. American brachytherapy society recommendations for clinical implementation of NIST-1999 standards for (103)palladium brachytherapy. The clinical research committee of the American Brachytherapy Society. Int J Radiat Oncol Biol Phys. 2000;47(2):273–275. doi: 10.1016/S0360-3016(00)00555-1. [DOI] [PubMed] [Google Scholar]
- 25.Vikram B. American Brachytherapy Society recommendations for clinical implementation of NIST-1999 standards for palladium-103 brachytherapy: in regard to Beyer et al. Int J Radiat Oncol Biol Phys. 2001;47:273–275. doi: 10.1016/s0360-3016(00)00796-3. [DOI] [PubMed] [Google Scholar]
- 26.Newman H, Chin KJ, Finger PT. Subfoveal choroidal melanoma: pretreatment characteristics and response to plaque radiation therapy. Arch Ophthalmol. 2011;129(7):892–898. doi: 10.1001/archophthalmol.2011.161. [DOI] [PubMed] [Google Scholar]


