Abstract
The role of the Toll-like receptor 4 (TLR4), a component of the innate immune system, in the development of burn-induced acute lung injury (ALI) has not been completely defined. Recent data suggested that an intact TLR4 plays a major role in the development of organ injury in sterile inflammation. We hypothesized that burn-induced ALI is a TLR4-dependent process. Male C57BL/6J (TLR4 wild-type [WT]) and C57BL/10ScN (TLR4 knockout [KO]) mice were subjected to a 30% total body surface area steam burn. Animals were killed at 6 and 24 h after the insult. Lung specimens were harvested for histological examination after hematoxylin-eosin staining. In addition, lung myeloperoxidase (MPO) and intercellular adhesion molecule 1 immunostaining was performed. Lung MPO was measured by an enzymatic assay. Total lung keratinocyte-derived chemoattractant (IL-8) content was measured by enzyme-linked immunosorbent assay. Western blot was performed to quantify phosphorylated IκBα, phosphorylated nuclear factor κB p65 (NF-κBp65), and high mobility group box 1 expression. Acute lung injury, characterized by thickening of the alveolar-capillary membrane, hyaline membrane formation, intraalveolar hemorrhage, and neutrophil infiltration, was seen in WT but not KO animals at 24 h. Myeloperoxidase and intercellular adhesion molecule 1 immunostaining of KO animals was also similar to sham but elevated in WT animals. In addition, a reduction in MPO enzymatic activity was observed in KO mice as well as a reduction in IL-8 levels compared with their WT counterparts. Burn-induced ALI develops within 24 h after the initial thermal insult in our model. Toll-like receptor 4 KO animals were clearly protected and had a much less severe lung injury. Our data suggest that burn-induced ALI is a TLR4-dependent process.
Keywords: TLR4, HMGB-1, burn, lung injury, neutrophil
INTRODUCTION
Toll-like receptors, a family of transmembrane receptor proteins, play a major role in innate immunity and are located in virtually every cell of the body. Since the time that Toll-like receptor 4 (TLR4) was originally described as the receptor for bacterial endotoxin, much has been discovered in its recognition of other endogenous damage-associated molecular patterns (DAMPs) involved in triggering the innate immune system after sterile injury (1, 2). Many injury models including bacterial endotoxemia (3), pulmonary contusion (4), hemorrhagic shock (5, 6), and, recently, burn (7) demonstrate the importance of the TLR4 receptor in progression of inflammation. There remains, however, a paucity of literature to support the involvement of TLR4 in the development of acute lung injury (ALI) after burn.
The synthesis of proinflammatory mediators after burn is a central component to ALI and multiple organ failure. TNF-α elevation is seen after burn (8), which stimulates further production of inflammatory mediators through activation of the NF-κB pathway. Similarly, ligand-binding of TLR4 receptors leads to an increase in NF-κB pathway activation and synthesis of proinflammatory mediators (9, 10).
We have demonstrated that ALI is a secondary consequence of cutaneous burn injury (11) and that it is a neutrophil-mediated process (Krzyzaniak et al, data submitted for publication). Increases in NF-κB pathway activation lead to increased expression of IL-8 and intercellular adhesion molecule 1 (ICAM-1) signaling neutrophil recruitment and translocation into the pulmonary parenchyma. Once in the lungs, neutrophils cause injury via release of granulated contents and generation of reactive oxygen species.
High mobility group box 1 (HMGB-1) has been shown to be elevated in both infectious and noninfectious injury and serves as an important endogenous signaling molecule that mediates late, continued inflammation (12). Its release occurs both actively and passively as a result of cell inflammation and damage. Within the paradigm of sterile injury, increases in HMGB-1 have been demonstrated in models of hemorrhagic shock (13) and femur fracture (14). There has been some evidence suggesting HMGB-1 release can happen early and mediate organ dysfunction (15); however, the predominant data show that it is a late mediator of continued inflammation. Interestingly, HMGB-1 has also been shown to act as a ligand for the TLR4 receptor (16).
We have recently demonstrated the importance of a functional TLR4 receptor in the development of intestinal injury and the breakdown of the intestinal epithelial barrier (7). In this study, we investigated the role of the TLR4 receptor in mediating ALI. We postulated that an intact TLR4 receptor is required for burn-induced ALI to occur.
MATERIALS AND METHODS
Burn model of injury
Male and female C57BL/6J (TLR4 wild-type [WT]) and C57BL/10ScN (TLR4 knockout [KO]) mice (originals from Jackson Laboratories, Sacramento, Calif) breeding pairs were raised and allowed access to food and water ad libitum. The number of animals used for each experiment is specifically stated in the figure legends, but in general was at least three animals per experiment per condition. All animals were anesthetized using inhaled isoflurane. The dorsal fur was removed using an electric clipper. Animals were then placed in a template estimating 30% total body surface area and subjected to a steam burn for 7 s as previously described (11, 17). After burn injury, animals received a subcutaneous injection of 1.4 mL normal saline with 100 µL of buprenorphine for pain control and resuscitation. Animals were recovered from anesthesia and returned to their cages. At 6 and 24 h after burn, animals were again anesthetized with inhaled isoflurane for euthanasia, and tissue procurement was performed. Before tissue collection, intracardiac cold saline flush was performed via the right ventricle to clear the circulatory system. Tissue collection from sham animals was performed in the same manner as the other groups. Experiments were approved by the University of California Animal Subjects Committee and are in accordance with guidelines established by the National Institutes of Health.
Histological evaluation
Lung samples taken 24 h after burn injury were preserved immediately at the time of collection in 10% formalin solution and submitted for paraffin blocking and hematoxylin-eosin staining by University of California, San Diego, Histology Core Services. Multiple 5-µm sections of lung (n ≥ 4 mice per experimental condition) were evaluated by a pathologist blinded to the experimental groups. Sections were scored according to the pulmonary injury scoring system previously used by our laboratory (18). Sections were rated on a scale from 0 to 3, ranging from normal to severe injury. Sections were analyzed based on the amount of intraalveolar hemorrhage, pulmonary congestion, edema, and infiltration of inflammatory cells to yield a maximum possible score of 12. Lung injury scores were averaged for each experimental condition, and images were taken at 20× and 60× magnification with light microscopy.
Immunoblot
Lung samples (n ≥ 5 animals per group) were immediately snap frozen with liquid nitrogen at the time of collection and stored at −80°C. Tissue protein extraction was performed by homogenizing tissue with Nuclear and Cytoplasmic Extraction Reagent (Pierce, Rockford, Ill) and Halt Phosphatase and Protease Inhibitor (Pierce). Samples were then centrifuged, and the supernatant was retained. The total protein concentration of each extract was determined using the bicinchoninic acid (BCA) protein assay according to a microplate procedure (Pierce). Absorbance was measured at 562 nm with a standard curve for albumin. Ten micrograms of protein were loaded into each sample well. Samples were separated using 6% to 18% Tris-glycine gel and transferred onto nitrocellulose membranes. After blocking with 5% bovine serum albumin, samples were exposed overnight to rabbit anti–phospho-IκBα, anti–phospho–nuclear factor κB p65 (NF-κB p65) antibody (1:500; Cell Signaling Technology, Danvers, Mass). A separate immunoblot was performed for HMGB-1 (Abcam, Cambridge, Mass) cytoplasmic content. The samples were then treated with anti–rabbit IgG horseradish peroxidase–linked antibody (1:2,000; Cell Signaling), followed by chemiluminescent detector solution (Pierce). β-Actin and lamin B loading control (1:500; Cell Signaling) were measured appropriately for each gel. Band pixel density was calculated using Un-Scan-It software (Silk Scientific, Orem, Utah). The relative band density was calculated by dividing the pixel density of the lane of interest by its pixel density of the loading control. The average relative band density of the sham animals was calculated, and the data are reported as relative band density/sham (±SEM).
Lung keratinocyte-derived chemoattractant content
Mouse keratinocyte-derived chemoattractant (KC) is a neutrophil chemoattractant present in mice with functions that are similar to that of human IL-8. Quantification of KC was conducted through a commercially available enzyme-linked immunosorbent assay (ELISA) from R&D Systems, Minneapolis, Minn. The total protein concentration of each extract was determined using the BCA protein assay according to a microplate procedure (Pierce). Absorbance was measured at 562 nm with a standard curve for albumin. Data are represented as picograms per milligram of lung tissue protein.
Immunohistochemistry
Formalin-preserved lung specimens were submitted for paraffin blocking by University of California, San Diego, Histology Core Services. After deparaffinization, lung slides were incubated in citrate antigen retrieval solution (Thermo Scientific, Fremont, Calif) for 20 min at 95°C and cooled to room temperature (n ≥ 5 animals per group). Sections were blocked for 2 h with 10% donkey serum albumin in phosphate-buffered saline (PBS) at room temperature. Next, slides were incubated overnight at 4°C with primary antibody for myeloperoxidase (MPO) (Thermo Scientific) or ICAM-1 (R&D Systems) diluted 1:100 in 1% bovine serum albumin in PBS. Sections were washed and incubated in 0.3% H2O2 to quench endogenous peroxidase activity for 15 min. Sections were washed again and incubated in anti–rabbit IgG horseradish peroxidase–linked antibody (Cell Signaling Technologies) diluted 1:400 in 1% bovine serum albumin in PBS for 1 h. Specific labeling was done with DAB substrate kit (Vector Laboratories, Burlingame, Calif). Specimens were then counterstained with hematoxylin. Direct comparison for ICAM-1 staining was performed with light microscopy. Ten random high-power fields were examined per animal to determine the number of cells staining positive for MPO.
MPO assay
Frozen lung specimens stored at −80°C were used to perform the enzymatic reaction. Approximately 5 mg of frozen lung tissue was dounce homogenized in 5% hexadecyl ammonium bromide solution, placed in a centrifuge, and spun at 14,000 revolutions per minute for 30 min at 4°C, and supernatant was removed. A standard curve was created using stock MPO enzyme 10 units/mL (Sigma, St Louis, Mo) and reconstituted with 0.5 mL of ddH2O. Samples were diluted 1:10 with 1× PBS solution. Ten microliters of stock standard curve dilutions and unknown samples were added to 90-µL substrate solution composed of 1:1 dilute hydrogen peroxide and DMB o-dianisidine (Sigma) for a total volume of 100 µL per well. Reaction was allowed to incubate at room temperature for 10 min. Absorbance was then measured on a plate reader at 450 nm. The total protein concentration of each extract was determined using the BCA protein assay according to a microplate procedure (Pierce). Absorbance was measured at 562 nm with a standard curve for albumin. Data are expressed as units of MPO per mg protein ± SEM.
Statistical analysis
Data are expressed as the mean ± SEM. The statistical significance among groups was determined using multiple univariate ANOVA with Bonferroni correction where appropriate. Statistical analysis of nonparametric data was done performing a Kruskal-Wallis test followed by post hoc Mann-Whitney U test for multiple comparisons. Statistical analysis was performed using SPSS software v11.5 (SPSS, Chicago, Ill) or KaleidaGraph Software version 4.04 (Synergy Software, Reading, Pa). Statistical significance was defined as P ≤ 0.05.
RESULTS
ALI is absent in TLR4 KO animals
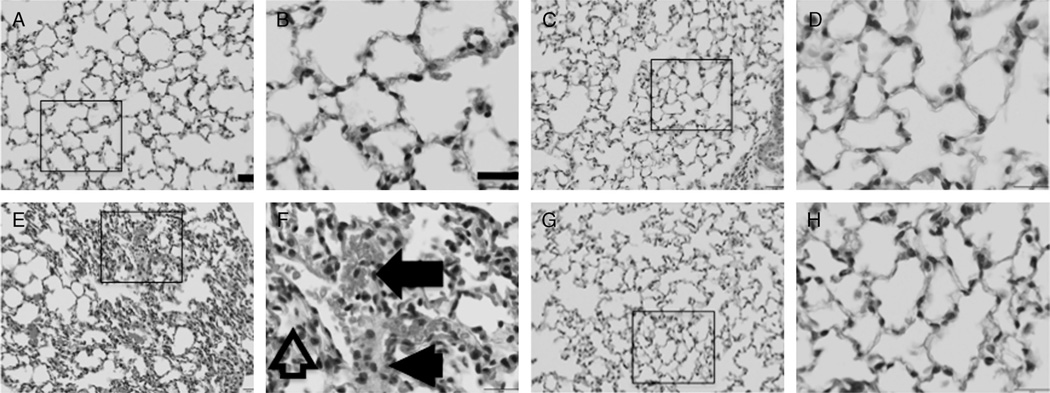
Lung histology was used to evaluate the severity of lung injury. Both TLR4 WT and TLR4 KO sham animals demonstrated no injury to the lungs (Fig. 1, A and B, and C and D, respectively). Lung injury was readily apparent in TLR4 WT animals 24 h after burn injury (Fig. 1, E and F). At a higher magnification (Fig. 1F), lung injury can be seen as thickening of the alveolar-capillary membrane (arrowhead), hyaline membrane formation (arrow outline), and intra-alveolar hemorrhage (arrow). However, lung specimens from TLR4 KO animals at 24 h demonstrated minimal injury similar to sham animals (Fig. 1, G and H). Lung injury scores were significantly more severe in the TLR4 WT animals 24 h after burn injury (Fig. 2).
Fig. 1. Lung histology and lung injury scoring.
Acute lung injury occurs in TLR4 WT but not TLR4 KO animals. Sections of lung were harvested 24 h after 30% total body surface area burn (n ≥ 3 animals per group), stained with hematoxylin and eosin, and compared with sham. All images are 20× and 60× magnification (left to right, respectively). A and B demonstrate normal lung appearance in TLR4 WT sham animals. Toll-like receptor 4 KO sham animals give similar histological appearance to TLR4 WT sham animals (C and D). Severe lung injury marked by thickening of the alveolar-capillary membrane (arrow head), hyaline membrane formation (arrow outline), and intra-alveolar hemorrhage (arrow) is seen in TLR4 WT animals at 24 h after burn (E and F). This injury pattern is not seen in TLR4 KO animals 24 h after burn with images that appear similar to sham (G and H). Black bar = 20 µm. At least four animals were used per group.
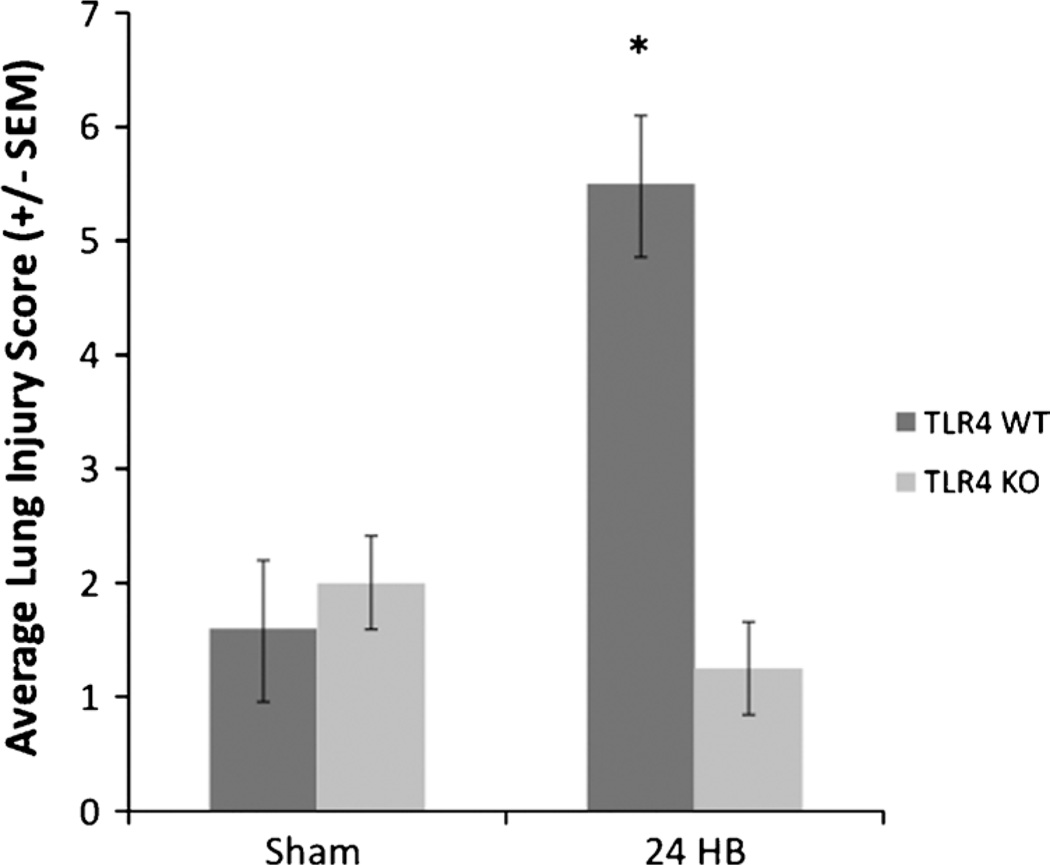
Fig. 2. Lung injury scores.
Lung injury scores were elevated in TLR4 WT animals 24 h after burn. Lung injury scoring was based on categories of inflammatory cell infiltration, pulmonary edema, congestion, and intra-alveolar hemorrhage graded on a scale from 0 = normal, 1 = mild, 2 = moderate, and 3 = severe injury, yielding a maximum possible score of 12. Sections were graded by a pathologist blinded to the study protocol. Lung injury scores were significantly elevated in the TLR4 WT animals 24 h after burn (*P < 0.03 compared with TLR4 WT sham, TLR4 KO sham, and TLR4 KO 24 h burn animals). Statistics were calculated by Kruskal-Wallis test followed by Mann-Whitney U test for multiple comparisons of nonparametric data. At least four animals were used per group.
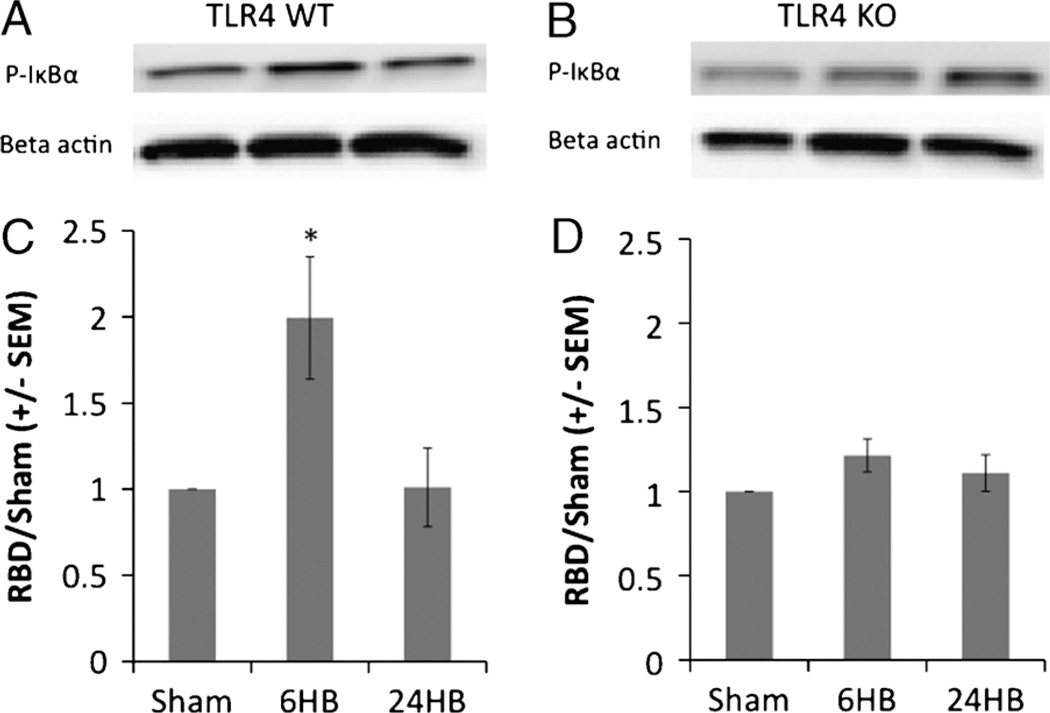
Activation of NF-κB pathway is absent in TLR4 KO animals
The NF-κB pathway is an important intracellular signaling mechanism associated with TLR4 activation. Before transcription of inflammatory cytokines begins, cleavage of the NF-κBp65 subunit from its inhibitor molecule, via phosphorylation, must occur. In this experiment, phosphorylation of IκBα within the cytoplasm significantly increased 6 h after burn in the TLR4 WT animals (Fig. 2, A and C). However, no alteration of P-IκBα levels occurred in the TLR4 KO animals (Fig. 3, B and D).
Fig. 3. Cytoplasmic phosphorylated IκBα levels.
P-IκBα levels are increased 6 h after burn in TLR4 WT animals. A and B demonstrate representative Western blots for cytoplasmic P-IκBα levels and β-actin loading control proteins. P-IκBα levels were significantly increased 6 h after burn in TLR4 WT animals (P < 0.05 compared with TLR4 WT sham) (C). No difference in P-IκBα levels was seen in TLR4 KO animals between time intervals (D). At least four animals were used per group.
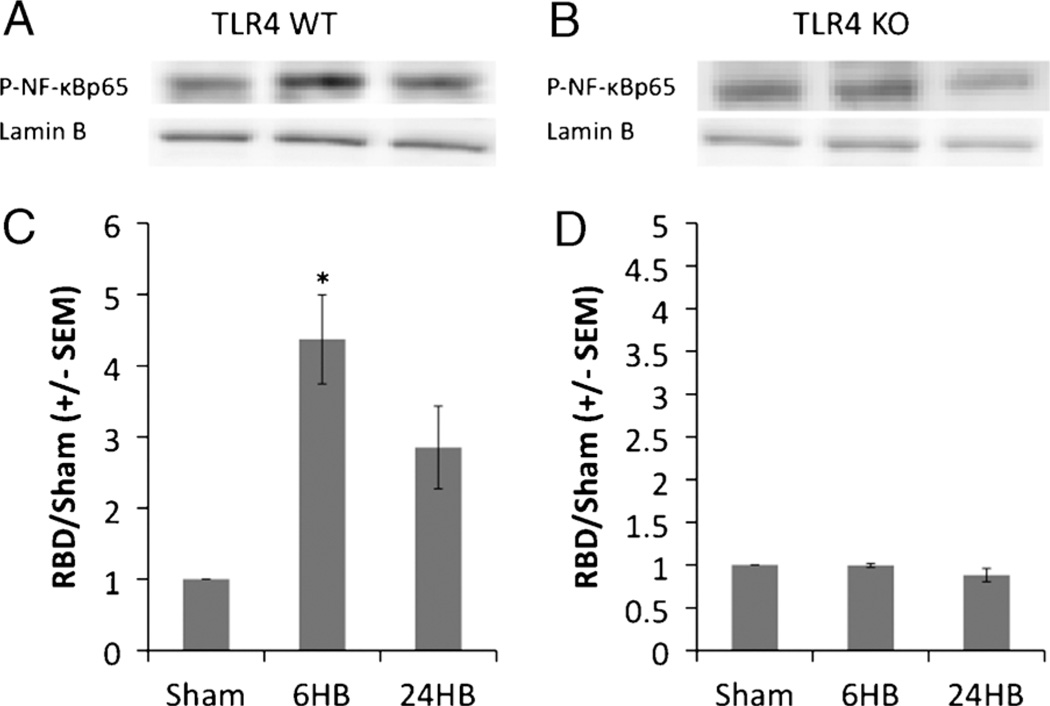
Once dissociated from its inhibitor molecule and phosphorylated, NF-κBp65 can freely move into the cell nucleus and initiate transcription of inflammatory mediators. Six hours after burn injury, nuclear P–NF-κBp65 levels significantly increased in TLR4 WT animals (Fig. 4, A and C). In TLR4 KO animals, nuclear P–NF-κBp65 levels were unchanged at the studied time points (Fig. 4, B and D).
Fig. 4. Nuclear phosphorylated NF-κBp65 levels.
P–NF-κBp65 levels are increased 6 h after burn in TLR4 WT animals. A and B demonstrate representative Western blots for nuclear P–NF-κBp65 levels and lamin B loading control proteins. P–NF-κBp65 levels were significantly increased 6 h after burn in TLR4 WT animals (P < 0.05 compared with TLR4 WT sham) (C). No difference in P–NF-κBp65 levels was seen in TLR4 KO animals between time intervals (D). At least four animals were used per group.
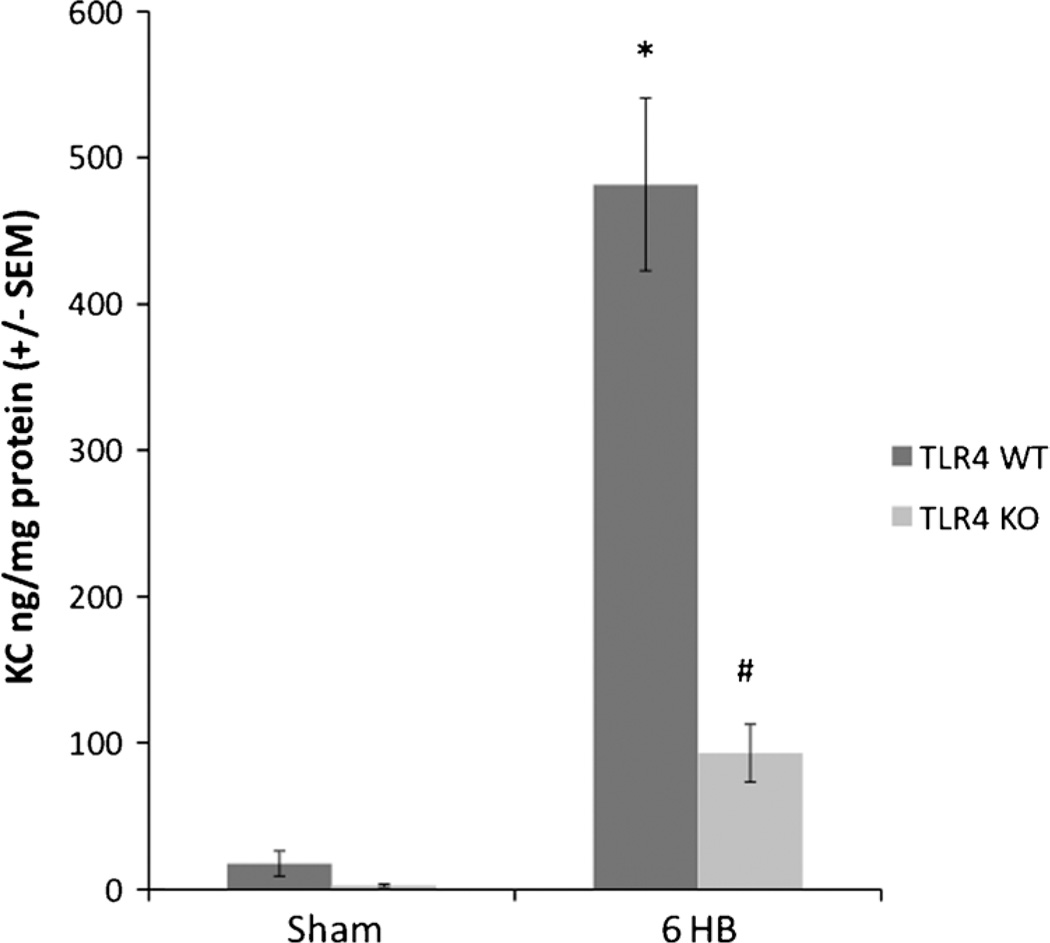
Lung KC levels are reduced in TLR4 KO animals
To assess the signal for neutrophil infiltration, expression of the murine analog to human IL-8, KC, was measured by ELISA (Fig. 5). Lung tissue KC levels were minimal in both TLR4 WT and TLR KO sham animals. Six hours after burn injury, lung tissue KC levels were significantly increased in TLR4 WT animals and TLR4 KO animals compared with sham. However, KC levels in the WT animals were markedly increased compared with the KO animals 6 h after burn injury.
Fig. 5. Mouse lung keratinocyte-derived chemokine.
Lung KC levels measured by ELISA were significantly more increased 6 h after burn in TLR4 WT than TLR4 KO. Lung KC levels were minimal in both sham animal groups. Keratinocyte-derived chemokine levels were significantly increased in TLR4WT animals 6 h after burn (*P < 0.001 compared with both TLR4 WT sham and TLR4 KO sham). Although TLR4 KO animals did show a significant increase in KC levels over both sham groups 6 h after burn (#P < 0.01), the KO deletion led to a significantly lower production of KC compared with TLR4 WT 6 h after burn (* = P < 0.001). At least four animals per group were used.
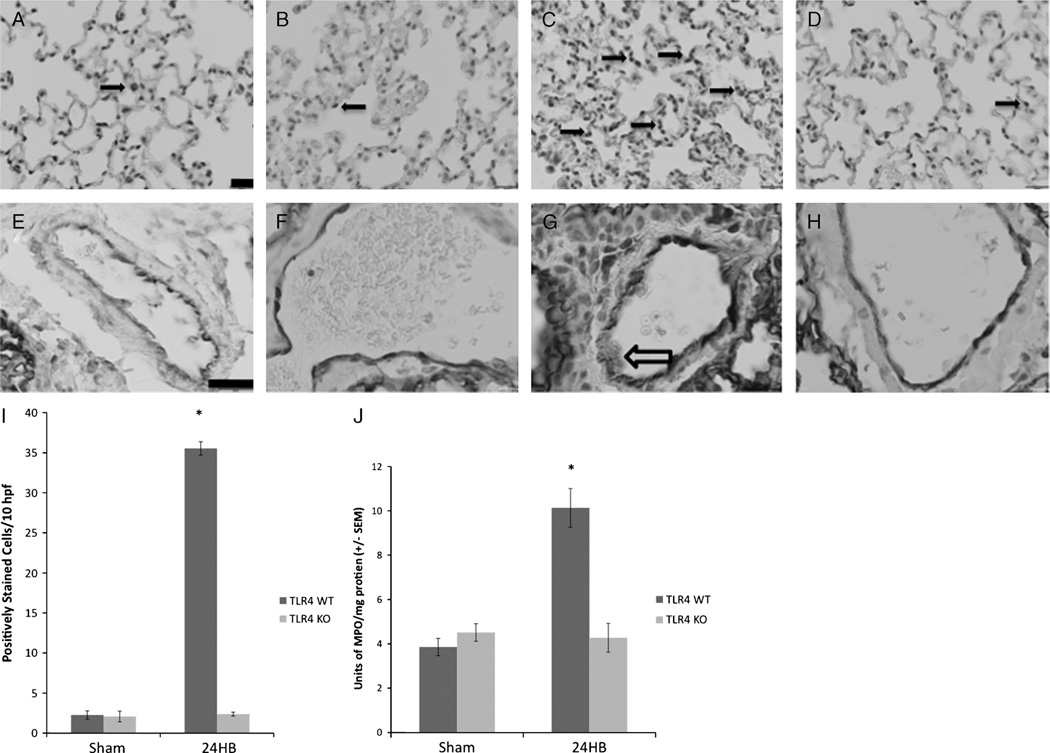
Neutrophil infiltration is not increased in TLR4 KO animals
Neutrophil infiltration into the lungs was visualized using immune staining (Fig. 6, A–D). Positively stained cells can rarely be seen in sham animals (Fig. 6A, arrow). Twenty-four hours after burn injury, a large increase in immune staining is seen in TLR4 WT but not in TLR4 KO animals (Fig. 6, C and D, respectively). Immune staining for ICAM-1 on the endothelium of pulmonary arterioles was also observed, providing the migration signal necessary for neutrophils to infiltrate into the lungs (Fig. 6, E–H). Again, immune staining is clearly increased (arrow outline) in the endothelium of TLR4 WT animals 24 h after burn but not in TLR4 WT sham, TLR4 KO sham, or TLR4 KO 24 h after burn.
Fig. 6. Lung MPO, ICAM-1 immune staining, and MPO assay.
Immune staining for MPO demonstrates few positively staining cells in sham animal groups (A and B, arrow) but increased in TLR4 WT animals (C) compared with TLR4 KO animals (D). Solid arrows indicate positively staining cells for MPO. Immune staining for ICAM-1 on the endothelial surface of pulmonary arterioles showed minimal staining in both TLR4 WT sham and TLR4 KO sham (E and F, respectively). Deposition of stain on the endothelial surface of pulmonary arterioles in TLR4 WT animals 24 h after burn was more intense than any other group (G, arrow outline). H shows a representative image of ICAM-1 immune staining seen in TLR4 KO animals 24 h after burn, showing similar staining pattern to both sham animal groups. Black bar = 20 µm. A–D, Original magnification ×20. E–H, Original magnification ×60. Myeloperoxidase positively staining cells were counted per 10 high-power fields per experimental group (I). Sections from TLR4 WT animals 24 h after burn had significantly more positively staining cells (*P > 0.05 compared with TLR4 WT sham, TLR4 KO sham, and TLR4 KO 24 h after burn). Enzymatic assay was used to measure MPO levels within pulmonary tissue (J). Myeloperoxidase enzymatic activity was significantly increased in TLR4 WT animals 24 h after burn (*P < 0.005 compared with TLR4 WT sham, TLR4 KO sham, and TLR4 KO animals 24 h after burn). At least four animals were used per group.
To assess the degree of neutrophil infiltration, positively staining cell counts per 10 high-power fields were performed for all groups (Fig. 6I). Toll-like receptor 4 WT animals demonstrated significantly higher positively immune-staining cell counts compared with both sham groups and TLR4 KO animals at 24 h. Myeloperoxidase enzyme activity was quantified within lung tissue extracts in both sham animals and 24 h after burn (Fig. 6J). Myeloperoxidase activity was significantly increased in TLR4 WT animals 24 h after burn compared with both TLR4 WT and TLR4 KO sham, as well as TLR4 KO animals 24 h after burn.
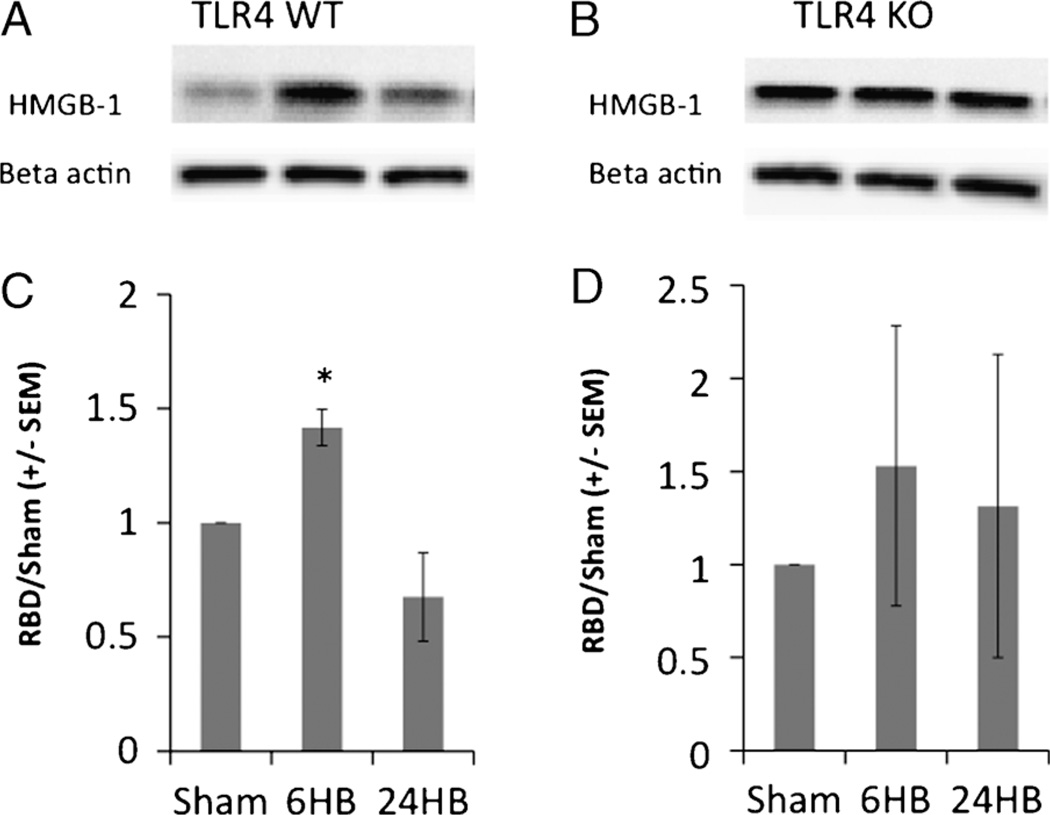
Cytoplasmic HMGB-1 is unchanged in burned TLR4 KO animals
High mobility group box protein 1 has been shown to mediate late inflammation after injury. This is accomplished by its movement out of the nucleus and into the cytoplasm and eventually its release into the systemic circulation. Six hours after burn injury, the cytoplasmic concentration of HMGB-1 is increased in TLR4 WT animals, followed by a decrease at 24 h (Fig. 7, A and C). In TLR4 KO animals, this is not observed (Fig. 7, B and D). The cytoplasmic concentration of HMGB-1 does not change in animals missing the functional TLR4. Secondary to the missing TLR4, cells may not be able to recognize the inflammatory stimulus that would otherwise cause the exportation of HMBG-1 from the cell nucleus.
Fig. 7. Western blot for HMGB-1.
High mobility group box 1 levels are increased 6 h after burn in TLR4 WT animals. A and B demonstrate representative Western blots for cytoplasmic HMGB-1 levels and β-actin loading control proteins. High mobility group box 1 levels were significantly increased 6 h after burn in TLR4 WT animals (P < 0.05 compared with TLR4 WT sham) (C). No difference in HMGB-1 levels was seen in TLR4 KO animals between time intervals (D). At least four animals were used per group.
DISCUSSION
Acute lung injury remains a major cause of morbidity and mortality in the critically ill patient, often leading to respiratory failure (19). The role of TLR4 in sterile lung injury has not yet been completely elucidated. Research has demonstrated that ALI occurs in several forms of sterile injury including pulmonary contusion (4), hemorrhagic shock (5, 6), and acute pancreatitis (20). However, its role in mediating ALI after burn has, to our knowledge, not been studied previously. This research provides an incremental step forward in the understanding of the role of TLR4 in sterile injury.
The present study demonstrates that ALI after burn is a TLR4-dependent process. The lack of injury evident by histology clearly shows that mice that are TLR4 deficient are protected against lung injury 24 h after burn. Acute lung injury in both sterile and nonsterile conditions is neutrophil mediated (21, 22). This study supports the role of the neutrophil in the development of ALI in animals with intact TLR4. However, mice that are genetically deficient of TLR4 neither produce the necessary inflammatory signals nor accumulate neutrophils within the lung tissue by some other mechanism.
Pulmonary complications after burns have been well documented and described over the past several decades (23). The family of Toll-like receptors recognizes specific molecular patterns, qualifying them as pattern-recognition receptors that can originate from invading pathogens or from damaged cells within the host (1). The prototypical pathogen-associated molecular pattern recognized by TLR4 is bacterial endotoxin. More recently, DAMPs have been well described, which can also mediate inflammation (2). Included in the category of DAMPs, heat shock proteins and HMGB-1, and likely many other unknown molecular patterns, are able to activate the innate immune system through TLR4 (2, 16). Although no clear link between TLR4-dependent lung injury and burn has been discovered, research favors the likelihood of a circulating factor acting as a DAMP that can effectively stimulate TLR4 and signal inflammation.
Although we focused on TLR4 in the present study, it should also be stated that other TLRs may have an important role in mediating the inflammatory response. We focused on TLR4 because of its known association and ability to recognized endogenous danger signals. The lack of injury and neutrophil infiltration seen in the present study supports a clear role for TLR4 in burn-induced ALI. Clearly, however, TLR4 is not the only member in the receptor family capable of mediating organ injury in sterile models of inflammation. For example, a role for TLR2 involvement has been shown in neutrophil-derived ALI following a hemorrhagic shock model (24). Inflammatory cells themselves harbor several TLRs, all playing an important function in the innate immune response and specifically in ALI (25).
The specific intracellular signaling mechanisms linking TLR4 to propagation of the inflammatory signals have been studied. However, some degree of uncertainty still remains between injury models and intracellular TLR4 signaling. Although we demonstrate in our study that burn-induced ALI activates the NF-κB pathway by upregulating phosphorylation of the p65 subunit through a TLR4-mediated process, the p65 subunit may not be the only member of the NF-κB family involved in sterile models of inflammation. Differences in specific subunit activation could explain why increases in p65 can be seen with TLR4 activation following endotoxemia but not necessarily with hemorrhagic shock (6, 26). The NF-κB proteins can be phosphorylated in several subunit combinations to mediate inflammation and are by no means limited to the p65 subunit (27).
It is conceivable that two possibilities exist to explain the inflammatory changes seen in TLR4 WT but not TLR4 KO animals. One possibility is that the burn injury itself mediates the lung injury seen at 24 h after the initial insult via release of an unknown factor from the damaged tissue. Although HMGB-1 has been documented to mediate ALI in severe infection models (15), it would appear less likely that HMGB-1 is mediating the lung injury seen in our burn model. Because the cytoplasmic concentration of HMGB-1 is elevated 6 h after injury, simultaneously with the activation of the NF-κB pathway, it is unlikely that enough time has elapsed for cellular release of HMGB-1 into the systemic circulation to activate TLR4 and the NF-κB pathway. Another possibility is that the inflammatory signal mediating lung injury originates from the gut. Consistent with previous experiments in our laboratory, an intact TLR4 is required for gut injury to occur (7). More recently, studies from our laboratory demonstrate that lung injury will not occur in the burn model if intestinal barrier injury is prevented (unpublished data). Although the current study does provide an incremental increase in understanding the mechanism behind the development of ALI, further definition of this process is needed to determine mechanisms of prevention in the critically ill patient.
In summary, we have demonstrated that ALI following cutaneous burn is TLR4-dependent process. Mice lacking a functional TLR4 were protected from histological abnormalities and neutrophil-mediated ALI 24 h after burn. Toll-like receptor 4 may be an important target to mitigate the innate inflammatory response after sterile injury. This could have implications in prevention of injury-induced end-organ dysfunction after trauma, burn, and sepsis.
ACKNOWLEDGMENTS
The authors thank Nicole Lopez, MD, Yan Ortiz Pomales, MD, Luiz Reys, MD, and Ann Marie Hageny for their contributions in completing this project.
No financial support was received for this study.
Footnotes
Presented in poster session at the 33rd annual meeting of the Shock Society, Portland, Oregon, June 12–15, 2010.
No competing financial interests exist.
REFERENCES
- 1.Xiang M, Fan J. Pattern recognition receptor-dependent mechanisms of acute lung injury. Mol Med. 2010;16:69–82. doi: 10.2119/molmed.2009.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lotze MT, Zeh HJ, Rubartelli A, Sparvero LJ, Amoscato AA, Washburn NR, Devera ME, Liang X, Tor M, Billiar T. The grateful dead: damage-associated molecular pattern molecules and reduction/oxidation regulate immunity. Immunol Rev. 2007;220:60–81. doi: 10.1111/j.1600-065X.2007.00579.x. [DOI] [PubMed] [Google Scholar]
- 3.Pastor CM, Pugin J, Kwak B, Chanson M, Mach F, Hadengue A, Frossard JL. Role of Toll-like receptor 4 on pancreatic and pulmonary injury in a mice model of acute pancreatitis associated with endotoxemia. Crit Care Med. 2004;32:1759–1763. doi: 10.1097/01.ccm.0000133020.47243.8e. [DOI] [PubMed] [Google Scholar]
- 4.Hoth JJ, Wells JD, Brownlee NA, Hiltbold EM, Meredith JW, McCall CE, Yoza BK. Toll-like receptor 4-dependent responses to lung injury in a murine model of pulmonary contusion. Shock. 2009;31:376–381. doi: 10.1097/SHK.0b013e3181862279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lv T, Shen X, Shi Y, Song Y. TLR4 is essential in acute lung injury induced by unresuscitated hemorrhagic shock. J Trauma. 2009;66:124–131. doi: 10.1097/TA.0b013e318181e555. [DOI] [PubMed] [Google Scholar]
- 6.Barsness KA, Arcaroli J, Harken AH, Abraham E, Banerjee A, Reznikov L, Mcintyre RC. Hemorrhage-induced acute lung injury is TLR-4 dependent. Am J Physiol Regul Integr Comp Physiol. 2004;287:R592–R599. doi: 10.1152/ajpregu.00412.2003. [DOI] [PubMed] [Google Scholar]
- 7.Peterson CY, Costantini TW, Loomis WH, Putnam JG, Wolf P, Bansal V, Eliceiri BP, Baird A, Coimbra R. Toll-like receptor-4 mediates intestinal barrier breakdown after thermal injury. Surg Infect. 2010;11:137–144. doi: 10.1089/sur.2009.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cannon JG, Friedberg JS, Gelfand JA, Tompkins RG, Burke JF, Dinarello CA. Circulating interleukin-1 beta and tumor necrosis factor-alpha concentrations after burn injury in humans. Crit Care Med. 1992;20:1414–1419. doi: 10.1097/00003246-199210000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Verstrepen L, Bekaert T, Chau TL, Tavernier J, Chariot A, Beyaert R. TLR-4, IL-1R and TNF-R signaling to NF-kappaB: variations on a common theme. Cell Mol Life Sci. 2008;65:2964–2978. doi: 10.1007/s00018-008-8064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chow JC, Young DW, Golenbock DT, Christ WJ, Gusovsky F. Toll-like receptor-4 mediates lipopolysaccharide-induced signal transduction. J Biol Chem. 1999;274:10689–10692. doi: 10.1074/jbc.274.16.10689. [DOI] [PubMed] [Google Scholar]
- 11.Costantini TW, Loomis WH, Putnam JG, Drusinsky D, Deree J, Choi S, Wolf P, Baird A, Eliceiri B, Bansal V, et al. Burn-induced gut barrier injury is attenuated by phosphodiesterase inhibition: effects on tight junction structural proteins. Shock. 2009;31:416–422. doi: 10.1097/SHK.0b013e3181863080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klune JR, Dhupar R, Cardinal J, Billiar TR, Tsung A. HMGB1: endogenous danger signaling. Mol Med. 2008;14:476–484. doi: 10.2119/2008-00034.Klune. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim JY, Park JS, Strassheim D, Douglas I, Diaz del Valle F, Asehnoune K, Mitra S, Kwak SH, Yamada S, Maruyama I, et al. HMGB1 contributes to the development of acute lung injury after hemorrhage. Am J Physiol Lung Cell Mol Physiol. 2005;288:L958–L965. doi: 10.1152/ajplung.00359.2004. [DOI] [PubMed] [Google Scholar]
- 14.Levy RM, Mollen KP, Prince JM, Kaczorowski DJ, Vallabhaneni R, Liu S, Tracey KJ, Lotze MT, Hackam DJ, Fink MP, et al. Systemic inflammation and remote organ injury following trauma require HMGB1. Am J Physiol Regul Integr Comp Physiol. 2007;293:R1538–R1544. doi: 10.1152/ajpregu.00272.2007. [DOI] [PubMed] [Google Scholar]
- 15.Abraham E, Arcaroli J, Carmody A, Wang H, Tracey KJ. HMG-1 as a mediator of acute lung inflammation. J Immunol. 2000;165:2950–2954. doi: 10.4049/jimmunol.165.6.2950. [DOI] [PubMed] [Google Scholar]
- 16.Yu M, Wang H, Ding A, Golenbock DT, Latz E, Czura CJ, Fenton MJ, Tracey KJ, Yang H. HMGB1 signals through Toll-like receptor (TLR) 4 and TLR2. Shock. 2006;26:174–179. doi: 10.1097/01.shk.0000225404.51320.82. [DOI] [PubMed] [Google Scholar]
- 17.Walker HL, Mason AD., Jr A standard animal burn. J Trauma. 1968;8:1049–1051. doi: 10.1097/00005373-196811000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Deree J, Martins J, de Campos T, Putnam JG, Loomis WH, Wolf P, Coimbra R. Pentoxifylline attenuates lung injury and modulates transcription factor activity in hemorrhagic shock. J Surg Res. 2007;143:99–108. doi: 10.1016/j.jss.2007.03.083. [DOI] [PubMed] [Google Scholar]
- 19.Bersten AD, Edibam C, Hunt T, Moran J. Incidence and mortality of acute lung injury and the acute respiratory distress syndrome in three Australian States. Am J Respir Crit Care Med. 2002;165:443–448. doi: 10.1164/ajrccm.165.4.2101124. [DOI] [PubMed] [Google Scholar]
- 20.Sharif R, Dawra R, Wasiluk K, Phillips P, Dudega V, Kurt-Jones E, Finberg R, Saluja A. Impact of Toll-like receptor 4 on the severity of acute pancreatitis and pancreatitis-associated lung injury in mice. Gut. 2009;58:813–819. doi: 10.1136/gut.2008.170423. [DOI] [PubMed] [Google Scholar]
- 21.Coimbra R, Loomis W, Melbostad H, Tobar M, Porcides RD, Hoyt DB. LPS-stimulated PMN activation and proinflammatory mediator synthesis is downregulated by phosphodiesterase inhibition: role of pentoxifylline. J Trauma. 2004;57:1157–1163. doi: 10.1097/01.ta.0000151261.28640.f7. [DOI] [PubMed] [Google Scholar]
- 22.Windsor AC, Mullen PG, Fowler AA, Sugerman HJ. Role of the neutrophil in adult respiratory distress syndrome. Br J Surg. 1993;80:10–17. doi: 10.1002/bjs.1800800106. [DOI] [PubMed] [Google Scholar]
- 23.Pruitt BA, Jr, Flemma RJ, DiVincenti FC, Foley FD, Mason AD, Jr, Young WG., Jr Pulmonary complications in burn patients. A comparative study of 697 patients. J Thorac Cardiovasc Surg. 1970;59:7–20. [PubMed] [Google Scholar]
- 24.Fan J. TLR cross-talk mechanism of hemorrhagic shock-primed pulmonary neutrophil infiltration. Open Crit Care Med J. 2010;2:1–8. doi: 10.2174/1874828700902010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lafferty EI, Qureshi ST, Schnare M. The role of Toll-like receptors in acute and chronic lung inflammation. J Inflamm. 2010;7:57. doi: 10.1186/1476-9255-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xie J, Lv R, Yu L, Huang W. Hydroxyethyl starch 130/0.4 exerts its anti-inflammatory effect in endotoxemic rats by inhibiting the TLR4/NF-kappaB signaling pathway. Ann Clin Lab Sci. 2010;40:240–246. [PubMed] [Google Scholar]
- 27.Viatour P, Merville MP, Bours V, Chariot A. Phosphorylation of NF-kappaB and IkappaB proteins: implications in cancer and inflammation. Trends Biochem Sci. 2005;30:43–52. doi: 10.1016/j.tibs.2004.11.009. [DOI] [PubMed] [Google Scholar]