Abstract
BACKGROUND
Despite long-standing guidelines from the American College of Obstetricians and Gynecologists that call for avoiding elective births prior to 39 weeks of gestation, elective deliveries make up almost one-third of US births occurring in weeks 36–38. Poor outcomes are more likely for infants born electively before 39 weeks than for those born at 39 weeks. The Perinatal Quality Collaborative of North Carolina (PQCNC) undertook the 39 Weeks Project in 2009–2010 with the aim of reducing the number of early-term elective deliveries in North Carolina hospitals.
METHODS
Participating hospitals (N = 33) provided retrospective data on all early-term deliveries and created new policies, or amended or enforced existing policies, to accomplish the project’s goals. Project activities included in-person learning sessions, regional meetings, webinars, electronic newsletters, a secure extranet Web site where participating hospitals could share relevant materials, and individual leadership consultations with hospital teams. Hospitals submitted monthly data to PQCNC, which provided ongoing training and data analysis.
RESULTS
Elective deliveries before 39 weeks of gestation decreased 45% over the project period, from 2% to 1.1% of all deliveries. The proportion of elective deliveries among all scheduled early-term deliveries also decreased, from 23.63% to 16.19%. There was an increase in the proportion of patients with documented evidence of medical indications for early delivery, from 62.4% to 88.2%.
LIMITATIONS
No data were collected to determine whether outcomes changed for patients whose deliveries were deferred. The project also depended on each hospital to code its own data.
CONCLUSIONS
The PQCNC’s 39 Weeks Project successfully decreased the rate of early-term elective deliveries in participating hospitals.
Three decades ago, the American College of Obstetricians and Gynecologists (ACOG) established 39 weeks as the minimal gestational age for non–medically indicated iatrogenic birth, and it has reiterated that guideline multiple times since then [1–6]. Despite the existence of this guideline, elective deliveries make up almost one-third of births in the United States occurring between 36 0/7 and 38 6/7 weeks of gestation. The Perinatal Quality Collaborative of North Carolina (PQCNC) is a voluntary, statewide organization that works with hospitals providing perinatal services in North Carolina and engages them in discrete initiatives for finite periods of time. PQCNC is funded by the North Carolina Division of Medical Assistance, the March of Dimes through its national office and its North Carolina chapter, and the Department of Pediatrics at the University of North Carolina (UNC) School of Medicine. In 2009–2010, PCQNC undertook the 39 Weeks Project, the stated goal of which was “to eliminate elective deliveries under 39 weeks’ gestation without documented pulmonary maturity studies in participating hospitals” [7].
Recent research has demonstrated the benefits of avoiding iatrogenic delivery prior to 39 weeks of gestation, including avoidance of adverse neonatal and maternal outcomes and decreased use of health resources (without worsening neonatal outcomes in low-risk pregnancies) [8–13]. The rate of elective deliveries before 39 weeks is one of the National Quality Forum’s measures [14] and one of The Joint Commission’s revised perinatal care measures [15]. Professional organizations, medical evidence, and regulatory agencies support inclusion of the rate of elective deliveries before 39 weeks as one component of a perinatal care quality improvement program.
At the outset of the study, data showed that in spite of existing guidelines and evidence, deliveries at participating hospitals were frequently scheduled for indications for which early delivery has no demonstrated benefit. This study documents the success among these hospitals in decreasing the rate of elective deliveries before 39 weeks of gestation, and it describes the successful strategies that led to this outcome.
Methods
The PQCNC leadership team included a neonatologist, a perinatologist, a quality improvement specialist, an obstetric nurse coordinator, a project manager, and a family support specialist; the input of these individuals to the project was equivalent to 2.5 full-time-equivalent staff members. An advisory board representing constituent organizations, health care providers, and consumers in North Carolina provided guidance to the leadership team. An expert panel of North Carolina obstetricians and nurse leaders also provided guidance and support for the project. This panel was selected from clinical leaders at hospitals that had already successfully undertaken quality improvement efforts to address late-preterm and early-term elective deliveries (36 0/7 to 38 6/7 weeks). The institutional review board (IRB) at the UNC School of Medicine reviewed this initiative and determined that it did not constitute human subjects research and therefore did not require IRB approval.
Hospital recruitment
All 88 hospitals in North Carolina with maternity services were invited to participate in this project. Participating hospitals agreed to collect and submit de-identified data to PQCNC and to create a project team that included physician, nurse, and administrative champions. Each team was encouraged to engage patients and families as advisers in their efforts. The only participation costs to hospitals were internal costs for data collection and submission.
Forty-one hospitals agreed to participate in the project; however, 3 of these hospitals joined the initiative late and submitted data retrospectively, and 5 other hospitals were unable to complete the project due to reductions in resources. The remaining 33 hospitals submitted 9 months of data on schedule and are represented in this analysis. These 33 hospitals, which perform approximately 60% of all deliveries in North Carolina, include most of the academic and tertiary centers in the state, as well as regional centers and rural community hospitals. Hospital delivery volumes ranged from 100 to more than 7,000 deliveries annually.
Project activities
Activities and tools included 3 in-person learning sessions, regional meetings, monthly webinars, a patient experience video, a weekly electronic newsletter, a secure extranet Web site for sharing relevant literature and materials from participating hospitals, and individual consultations with hospital teams. Learning sessions included didactic content from medical experts and patients, reports from participating teams about effective strategies, and time for teams to work individually on their hospital’s action plan. Regional meetings facilitated informal exchange of information among participating teams. Monthly webinars addressed data collection methodology, provided updates on data trends, and allowed discussion of challenges and successes.
Rather than prescribe a single course of action for all teams, PQCNC encouraged each team to develop its own action plan for decreasing the rate of elective deliveries before 39 weeks, so that each plan could reflect local needs and dynamics. Although PQCNC endorsed a statewide goal of eliminating elective deliveries before 39 weeks, each hospital team established site-specific goals based on its current performance and circumstances. During learning sessions, regional meetings, and webinars, PQCNC asked hospitals to share their strategies and practices for achieving the project’s goals.
Data collection
Each hospital was assigned a numeric code and submitted de-identified data for the period October 2009 through June 2010; data were submitted to PQCNC using a secure Web portal. Data elements included gestational age of the fetus at admission, use of amniocentesis, indication for delivery, mode of delivery, induction methods, birth weight, infant length of stay, neonatal complications, and maternal complications. Data were submitted for all planned deliveries—defined as scheduled cesarean sections and all inductions of labor—that occurred when the fetus’s gestational age was between 36 0/7 and 38 6/7 weeks. In addition, hospitals submitted overall totals for deliveries, scheduled cesarean sections, and inductions of labor for fetuses of all gestational ages.
The expert panel assigned each indication for delivery to 1 of 6 categories (A through F) based on their consensus regarding the appropriate management of patients with that indication; a seventh category (G) was created to capture other indications written in by the site (Table 1). The project aimed to reduce or eliminate category F, which includes deliveries explicitly identified in the chart as elective—that is, those with no indication for early delivery or with a primary indication of “repeat cesarean section.”
TABLE 1.
Indications for Scheduled Delivery, by Categorya
| Category | Description | Indications for scheduled delivery |
|---|---|---|
| A | Gestational age not a factor in delivery plan | Eclampsia, HELLP syndromeb, placenta previa with active bleeding, acute placental abruption, fetal demise, chorioamnionitis |
| B | Schedule delivery at 37–38 weeks of gestation if criteria are met (exclusive of hypertensive diseases) | Intrauterine growth restriction, oligohydramnios, isoimmunization, fetal hydrops, multiple gestation, cholestasis of pregnancy, third-trimester bleeding, placenta previa without current bleeding, decreased fetal movement, chronic placental abruption (symptom-free for more than 7 days), venous thromboembolism, fetal anomaly, nonreactive fetal nonstress test, biophysical profile score of 4 or less |
| C | Hypertensive disorders; schedule delivery at 37–38 weeks if criteria are met | Preeclampsia, pregnancy-induced hypertension, chronic hypertension |
| D | Schedule delivery before 39 weeks if amniocentesis indicates that lungs are mature | Poorly controlled diabetes, maternal drug use, prior classical cesarean section, long distance from hospital, previous myomectomy, prior precipitous labor, history of prior stillbirth, nonvertex presentation |
| E | Do not schedule delivery before 39 weeks in absence of other indications; consider earlier delivery only if amniocentesis indicates that lungs are mature | Well-controlled diabetes, genital herpes, lupus, fetus small for gestational age without evidence of placental insufficiency, coagulation defects, proteinuric renal disease, advanced cervical dilation, polyhydramnios, unstable lie of the fetus (sacrum posterior version), macrosomia |
| F | Elective; do not schedule delivery before 39 weeks; consider earlier delivery only if amniocentesis indicates that lungs are mature | Elective, repeat low transverse cesarean section, no indication |
| G | Other | All indications listed as “other” and written in by the individual site |
Categories of indications for scheduled delivery were devised by the Perinatal Quality Collaborative of North Carolina.
HELLP is an abbreviation for 3 features of the syndrome—H for hemolysis, EL for elevated liver enzyme levels, and LP for low platelet levels.
Data reporting
Hospitals received monthly reports from PQCNC. These reports included the number of scheduled deliveries occurring before 39 weeks of gestation; use of amniocentesis to determine fetal lung maturity; mode of delivery (cesarean section or vaginal delivery) for patients admitted for induction; number of cases with a primary indication of “elective,” which included cases with no documented indication or with “repeat low transverse cesarean section” as the primary indication; and the percentage of all indications that were supported by objective evidence using the standard definitions provided by the project’s expert panel.
Hospitals were also given in-depth quarterly reports that showed the distribution of primary indications for scheduled deliveries among the 7 categories for each institution as well as for the entire group of participating hospitals. Quarterly reports identified scheduled deliveries associated with maternal complications, neonatal complications, or both, and reports gave the percentage of cases in each category for which amniocentesis was performed. Hospitals were encouraged to use these data to revise their action plans and to enlist the support of key stakeholders within each institution. Local solutions were shared during monthly project telephone calls and during meetings that were held in response to specific inquiries. These solutions were collated but were not analyzed, so they are reported qualitatively.
Statistical analysis
Random effects models were used to assess the relationship between variables of interest while accounting for the many facilities with a random effect component. For binary variables, such as elective delivery or presence of neonatal complications, a generalized linear mixed model (PROC GLIMMIX, PROC NLMIXED) was used. For continuous variables, such as gestational age and birth weight, a linear mixed effects model (PROC MIXED) was used. All components of the analysis were performed using SAS 9.2 software (SAS Institute, Cary, North Carolina).
Results
Decrease in elective deliveries
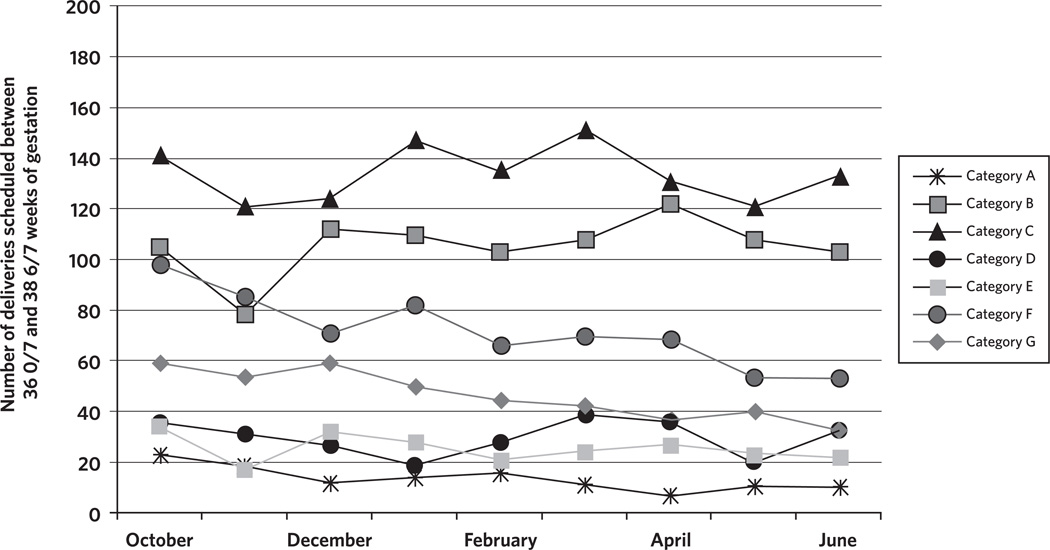
The 33 hospitals participating in the project collectively decreased early-term elective deliveries over the 9 months of the study from 2% to 1.1% of all deliveries; this represents an overall decline of 45% (Figure 1). Among all scheduled deliveries occurring between 36 0/7 and 38 6/7 weeks of gestation, the percentage of elective deliveries declined from 23.63% to 16.19%, which represents a decline of 31.5% (P = .002; Figure 2) Figure 3 shows monthly changes in the number of early-term deliveries by indication category (as defined in Table 1). Declines were noted in category F—the category for elective deliveries, which was the target for this project—and in category G, which included “other” indications for delivery.
FIGURE 1.
Rate of Early-Term Scheduled Deliveries as a Percentage of All Deliveries at Hospitals Participating in the 39 Weeks Project, October 2009 Through June 2010
FIGURE 2.
Percentage of All Early-Term Deliveries That Were Elective at Hospitals Participating in the 39 Weeks Project, October 2009 Through June 2010
FIGURE 3.
Total Number of Deliveries Scheduled Between 36 0/7 and 38 6/7 Weeks of Gestation, by Indication, at Hospitals Participating in the 39 Weeks Project of the Perinatal Quality Collaborative of North Carolina, October 2009 Through June 2010
Note. Categories A–G are defined in Table 1.
Repeat elective cesarean sections
The primary driver of elective early-term deliveries was the category of repeat elective cesarean sections, which represented 70.6% of elective early-term deliveries and 14.1% of all scheduled deliveries before 39 weeks of gestation (Figure 4). In comparison, elective inductions accounted for only 5.9% of early-term scheduled deliveries.
FIGURE 4.
Cesarean Sections as a Proportion of All Early-Term Scheduled Deliveries, All Medically Indicated Deliveries, and All Elective Deliveries at Hospitals Participating in the 39 Weeks Project of the Perinatal Quality Collaborative of North Carolina, October 2009 Through June 2010
Gestational age
Gestational age was greater for elective early-term deliveries than for early-term deliveries that were medically indicated (P<.001). The median gestational age for elective early-term deliveries was 38 5/7 weeks, whereas the median gestational age for medically indicated early-term deliveries was 37 6/7 weeks.
Evidence of medical indications for early delivery
There was a significant increase over time in the proportion of medically indicated, scheduled, early-term deliveries for which objective evidence of a medical indication was documented in the medical record (P<.001). In the first month of the project, 62.4% of primary medical indications for scheduled early-term deliveries were supported by objective evidence; by the end of the project, 88.2% of medical indications were supported by such evidence.
Neonatal complications
Among elective early-term deliveries, 8.4% were associated with a neonatal complication, and 4.1% resulted in admission to the newborn intensive care unit (NICU). In comparison, 17.3% of medically indicated, scheduled, early-term deliveries were associated with a neonatal complication, and 11.7% of such deliveries resulted in admission to the NICU.
Amniocentesis
The overall rate of amniocentesis was low across the study period but did increase by a statistically significant amount, from 6.9% at the start of the project to 8.4% by the end of the project (P = .05). There was no significant difference in use of amniocentesis between elective early-term scheduled deliveries compared with those that were medically indicated (P = .63).
Maternal complications
Overall, maternal complications occurred infrequently during the project. As expected, early-term deliveries that were medically indicated were associated with a higher rate of maternal complications (5.8%) compared with elective early-term deliveries (0.9%). The proportion of scheduled early-term deliveries with maternal complications did not change significantly over time (P = .14).
Hospital strategies
Hospital interventions varied across facilities and included changes to hospital policies, consensus agreements by members of the hospital’s obstetrics department, education of physicians and nurses, and a peer-review process for elective early-term deliveries. Some hospitals required that the departmental chair or a local perinatologist approve an early-term scheduled delivery unless there was a clear, documented indication. Hospitals became more rigorous in requiring information from providers who wished to schedule deliveries before 39 weeks of gestation, asking them to provide the medical indication for the delivery, supporting documentation, and the criteria used to establish gestational age.
Discussion
The 39 Weeks Project successfully decreased early-term elective deliveries over the 9-month period of the initiative. Rates of elective early-term deliveries and overall early-term births declined, without an increase in neonatal morbidity, suggesting that declines were accomplished by eliminating many elective early-term births, improving classification of early-term births that were medically indicated, and prolonging pregnancy in some women with complex births. Despite this success, elective deliveries still account for almost 17% of all deliveries occurring between 36 0/7 and 38 6/7 weeks of gestation in the participating hospitals.
Consistent with other published findings [16–18], many hospitals reported that a “hard stop” at the point of scheduling was the most effective method for reducing elective deliveries before 39 weeks of gestation. A “hard stop” occurs when the scheduler may not schedule a patient for delivery before 39 weeks of gestation without appropriate indications and supporting data. Several hospitals established a peer-review process specific to early-term elective deliveries or used an existing obstetric peer-review committee to ensure that specific feedback was given to any provider who performed an elective delivery before 39 weeks of gestation without an amniocentesis documenting lung maturity.
Given the impact of cesarean sections on the rate of scheduled deliveries before 39 weeks of gestation, we were not surprised to find that issues related to scheduling of surgery dominated the list of barriers noted by participating hospitals. Hospitals with dedicated obstetrical operating rooms could control the scheduling process more easily than could hospitals in which cesarean sections were performed in the hospital’s main operating rooms. Barriers also reflected lack of availability of 24-hour, dedicated obstetric anesthesia coverage.
One challenge to reducing the rate of early-term elective cesarean sections involved “block scheduling” of surgical time, in which all planned surgical procedures for the week are performed at a set time. Providers described performing a scheduled repeat cesarean section once the patient had completed 38 weeks of gestation in order to avoid scheduling cases too far into the 39th week of gestation, to avoid the possibility of an emergent cesarean delivery secondary to active labor. However, no PQCNC hospitals reported an increase in unscheduled cesarean sections as a result of prohibiting repeat elective cesarean sections before 39 weeks of gestation.
Research relevant to the PQCNC initiative and all materials from learning sessions and webinars were shared on an extranet Web site available to each hospital. PQCNC physician leaders facilitated discussions at several hospitals about the relevant medical issues, particularly when clinicians put up significant resistance to the implementation of changes. Inclusion of hospital administrators in hospital-based quality initiatives was also important, because it helped to defuse potential doctor-nurse conflicts around scheduling and to standardize processes across each institution.
Patient requests were perceived to be an important driver of early-term elective deliveries. The fact that many institutions across North Carolina participated in this initiative reduced providers’ fears that patients would abandon their practice and switch to a practice more willing to offer an early elective delivery. Physician champions noted that a hospital-wide standard prohibiting elective deliveries prior to 39 weeks of gestation helped prevent this scenario. Finally, hospitals found it easier to implement changes as part of a broader initiative; they were better able to influence provider groups that were resistant to policy changes by emphasizing that the hospital was attempting to adhere to standards set “by the state.”
The March of Dimes provided a brochure explaining the risks of elective early-term deliveries [19], which PQCNC distributed to childbirth education programs, provider offices, and triage patients who requested a scheduled delivery due to the discomforts of late pregnancy. Providers used the brochure to educate patients during early pregnancy about their policies, so that expectations would be clear well in advance of the patient’s due date.
This study found a significant increase in the provision of objective evidence supporting medical indications for early delivery, which suggests that providers improved their documentation, that only those deliveries that were truly medically necessary were performed, or both. Clear documentation tends to decrease legal risk for providers and hospital personnel. From a financial perspective, improved documentation for a delivery with complications may lead to a more appropriate diagnosis-related group (DRG) code and to increased reimbursement. Some deliveries should occur prior to 39 weeks of gestation, and accurate documentation of medical, fetal, and obstetrical complications can facilitate appropriate timing of scheduled early deliveries, as well as appropriate reimbursement. In 2011 the National Institute of Child Health and Human Development and the Society for Maternal-Fetal Medicine held a workshop to synthesize the available information about conditions that may necessitate medically indicated late-preterm or early-term births, and an article was subsequently published outlining what was learned about the optimal timing of delivery for specific conditions [20]. That information can help clinicians and hospitals avoid the problems that can arise when efforts to avoid elective early-term deliveries have the unintended consequence of preventing medically indicated early-term deliveries; these problems are highlighted in a 2012 article by Clark and colleagues [21].
The 1.5% absolute increase in the use of amniocentesis suggests that the 39 Weeks Project heightened attention to the ACOG guidelines stating that early-term elective deliveries should not be performed in the absence of test results indicating fetal lung maturity [1, 2]. However, amniocentesis was not performed on a substantial number of the women who did undergo early-term elective deliveries, and the observed change in use of amniocentesis was probably not clinically significant.
Demonstration of improved maternal and neonatal outcomes, with no increase in potentially avoidable complications, can help motivate the obstetric team to effect and sustain the changes necessary to avoid scheduled early elective deliveries. Obstacles include work/life balance, pressure from patients, concerns about complications that could potentially be avoided by earlier delivery, difficulty in scheduling, and lack of access to 24-hour anesthesia services in smaller hospitals.
Financial incentives and effective management of resources and costs may also motivate change. Community Care of North Carolina (CCNC), a care management plan for North Carolina’s Medicaid recipients, recently implemented a pregnancy “medical home” model [22]. To qualify as a pregnancy medical home and receive financial benefits, practices must agree to avoid elective deliveries prior to 39 weeks of gestation, in addition to meeting other requirements. The Joint Commission and the National Quality Forum now include the early-term elective delivery rate among their core measures for hospital accreditation, and this rate is included in publicly reported data [14, 15]. Numerous other states have adopted policies or launched multihospital initiatives to reduce the number of early-term elective deliveries [11, 16, 23–25]. Participating teams observed that challenges in scheduling medically indicated procedures were eased by eliminating elective early-term procedures. Similarly, other initiatives have reported decreased length of stay, improved patient throughput in labor and delivery, and decreased hospital costs [10, 11].
One strength of this initiative is its scope; participating facilities perform nearly 60% of deliveries in North Carolina. Also, the PQCNC data were collected specifically for each eligible case; we did not rely on administrative data sets or patient samples. An important limitation of the project is that no data were collected on patients whose babies were delivered after 39 weeks of gestation; we were therefore unable to determine whether outcomes changed for patients whose deliveries were deferred. Another limitation is that each hospital coded its own data. Also, fewer than half of the North Carolina hospitals with obstetrics services participated in this study; reasons for declining to participate were not collected, and participating and nonparticipating hospitals were not compared. Finally, successful strategies for preventing early-term elective deliveries at the hospital level were not collected in a formal manner.
Conclusion
This project demonstrates the ability of North Carolina hospitals and their obstetrics departments to work collaboratively and to effectively conduct an important quality improvement project with the potential for substantial improvements in neonatal outcomes, decreased use of health care resources, and improved care as a result of better documentation. Although the participating hospitals achieved a substantial collective decline in the rate of early-term elective deliveries, almost 17% of early-term deliveries were still elective by the end of the project. In a multistate trial with similar goals, Oshiro and colleagues [18] were able to reduce early-term deliveries from 27.8% of all deliveries to 4.8% of all deliveries over 12 months. Despite the successes achieved in the PQCNC 39 Week Project, there remain challenges: diminishing the rate of early-term elective births even further, sustaining the efforts of the participating hospitals, and spreading the successes of the project to hospitals that did not choose to participate.
Footnotes
Kate Berrien, RN, BSN, SM ______ Perinatal Quality Collaborative of North Carolina, Chapel Hill, North Carolina; and _______ Community Care of North Carolina, Raleigh, North Carolina.
Katherine Bryant, MSPH _____ Perinatal Quality Collaborative of North Carolina, Chapel Hill, North Carolina; and ______ Centers for Medicare & Medicaid Services, Baltimore, Maryland.
James Devente, MD ______ Perinatal Quality Collaborative of North Carolina, Chapel Hill, North Carolina; and ______ Brody School of Medicine, East Carolina University, Greenville, North Carolina.
Amanda French, RNC-OB, MSN, CNS _______ Perinatal Quality Collaborative of North Carolina, Chapel Hill, North Carolina; and _____ Duke University Health System, Durham, North Carolina.
Keith M. Cochran, MLT (ASCP), MS, PMP, LSSBB ______ Perinatal Quality Collaborative of North Carolina, Chapel Hill, North Carolina; and _______ Department of Pediatrics, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
Marty McCaffrey, MD _______ Perinatal Quality Collaborative of North Carolina, Chapel Hill, North Carolina; and _______ Department of Pediatrics, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
Beth Horton, MS ________ Department of Biostatistics, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
Nancy Chescheir, MD ______ Perinatal Quality Collaborative of North Carolina, Chapel Hill, North Carolina; and _______ Department of Obstetrics and Gynecology, School of Medicine, University of North Carolina at Chapel Hill, North Carolina.
Acknowledgment
Potential conflicts of interest. All authors have no relevant conflicts of interest.
References
- 1.American College of Obstetricians and Gynecologists (ACOG) Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 107: Induction of labor. Obstet Gynecol. 2009;114(2 Pt 1):386–397. doi: 10.1097/AOG.0b013e3181b48ef5. [DOI] [PubMed] [Google Scholar]
- 2.American College of Obstetricians and Gynecologists (ACOG) ACOG Practice Bulletin No. 97: Fetal lung maturity. Obstet Gynecol. 2008;112(3):717–726. doi: 10.1097/AOG.0b013e318188d1c2. [DOI] [PubMed] [Google Scholar]
- 3.American College of Obstetricians and Gynecologists (ACOG) ACOG Practice Bulletin No. 10: Induction of labor. Washington, DC: ACOG; 1999. [Google Scholar]
- 4.Committee on Educational Bulletins of the American College of Obstetricians and Gynecologists (ACOG) ACOG Educational Bulletin No. 230: Assessment of fetal lung maturity. Int J Gynaecol Obstet. 1997;56(2):191–198. [PubMed] [Google Scholar]
- 5.American College of Obstetricians and Gynecologists (ACOG) ACOG Committee Opinion No. 98. Fetal maturity assessment prior to repeat cesarean delivery. Washington, DC: ACOG; 1991. Committee on Obstetric Practice and the Society for Maternal-Fetal Medicine. [Google Scholar]
- 6.American College of Obstetricians and Gynecologists (ACOG) ACOG Committee Opinion No. 561: Nonmedically indicated early-term deliveries. Obstet Gynecol. 2013;121(4):911–915. doi: 10.1097/01.AOG.0000428649.57622.a7. [DOI] [PubMed] [Google Scholar]
- 7.Perinatal Quality Collaborative of North Carolina (PQCNC) Eliminating elective deliveries under 39 weeks gestation. [Accessed March 24, 2014];PQCNC Web site. doi: 10.18043/ncm.75.3.169. http://www.pqcnc.org/initiatives/39weeks. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin JA, Hamilton BE, Sutton PD, et al. Births: Final data for 2006. Natl Vital Stat Rep. 2009;57(7):1–102. [PubMed] [Google Scholar]
- 9.Zhang X, Joseph KS, Kramer MS. Decreased term and postterm birthweight in the United States: impact of labor induction. Am J Obstet Gynecol. 2010;203(2):124.e1–124.e7. doi: 10.1016/j.ajog.2010.03.044. [DOI] [PubMed] [Google Scholar]
- 10.Robinson CJ, Villers MS, Johnson DD, Simpson KN. Timing of elective repeat cesarean delivery at term and neonatal outcomes: a cost analysis. Am J Obstet Gynecol. 2010;202(6):632.e1–632.e6. doi: 10.1016/j.ajog.2010.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oshiro BT, Henry E, Wilson J, Branch DW, Varner MW Women and Newborn Clinical Integration Program. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113(4):804–811. doi: 10.1097/AOG.0b013e31819b5c8c. [DOI] [PubMed] [Google Scholar]
- 12.Hoffmire CA, Chess PR, Ben Saad T, Glantz JC. Elective delivery before 39 weeks: the risk of infant admission to the neonatal intensive care unit. Matern Child Health J. 2012;16(5):1053–1062. doi: 10.1007/s10995-011-0830-9. [DOI] [PubMed] [Google Scholar]
- 13.Yee W, Amin H, Wood S. Elective cesarean delivery, neonatal intensive care unit admission, and neonatal respiratory distress. Obstet Gynecol. 2008;111(4):823–828. doi: 10.1097/AOG.0b013e31816736e7. [DOI] [PubMed] [Google Scholar]
- 14.National Quality Forum (NQF) Measure 0469. PC-01 Elective Delivery. [Accessed April 28, 2013];NQF Web site. http://qualityforum.org/Qps/QpsTool.aspx. [Google Scholar]
- 15.The Joint Commission. Perinatal Care. [Accessed May 4, 2013];The Joint Commission Web site. 2014 Feb 21; http://www.jointcommission.org/perinatal_care/ [Google Scholar]
- 16.Clark SL, Miller DD, Belfort MA, Dildy GA, Frye DK, Meyers JA. Neonatal and maternal outcomes associated with elective term delivery. Am J Obstet Gynecol. 2009;200(2):156.e1–156.e4. doi: 10.1016/j.ajog.2008.08.068. [DOI] [PubMed] [Google Scholar]
- 17.Clark SL, Freye DR, Meyers JA, et al. Reduction in elective delivery at <39 weeks of gestation: comparative effectiveness of 3 approaches to change and the impact on neonatal intensive care admissions and stillbirth. Am J Obstet Gynecol. 2010;203(5):449.e1–449.e6. doi: 10.1016/j.ajog.2010.05.036. [DOI] [PubMed] [Google Scholar]
- 18.Oshiro BT, Kowalewski L, Sappenfield W, et al. A multistate quality improvement program to decrease elective deliveries before 39 weeks of gestation. Obstet Gynecol. 2013;121(5):1025–1031. doi: 10.1097/AOG.0b013e31828ca096. [DOI] [PubMed] [Google Scholar]
- 19.March of Dimes. Why the last weeks of pregnancy count: bilingual brochure. [Accessed March 4, 2012];March of Dimes Web site. https://www.marchofdimes.com/catalog/product.aspx?productid=5193&categoryid=&productcode=09-2428-09. [Google Scholar]
- 20.Spong CY, Mercer BM, D’alton M, Kilpartrick S, Blackwell S, Saade G. Timing of indicated late-preterm and early-term birth. Obstet Gynecol. 2011;118(2 Pt 1):3223–3233. doi: 10.1097/AOG.0b013e3182255999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark SL, Meyers JM, Perlin JB. Oversight of elective early term deliveries: avoiding unintended consequences. Am J Obstet Gynecol. 2012;206(5):387–389. doi: 10.1016/j.ajog.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 22.Community Care of North Carolina (CCNC) Pregnancy Medical Home Program. [Accessed May 4, 2013];CCNC Web site. https://www.communitycarenc.org/media/related-downloads/pregnancy-medical-home-brochure.pdf. [Google Scholar]
- 23.Ohnsorg T, Schiff J. Preventing elective induction before 39 Weeks. Minn Med. 2010;93(11):44–46. [PubMed] [Google Scholar]
- 24.Donovan EF, Lannon C, Ballit J, Rose B, Iams JD, Byczkowski T Ohio Perinatal Quality Collaborative Writing Committee. A statewide initiative to reduce inappropriate scheduled births at 36(0/7)– 38(6/7) weeks’ gestation. Am J Obstet Gynecol. 2010;202(3):243.e1–243.e8. doi: 10.1016/j.ajog.2010.01.044. [DOI] [PubMed] [Google Scholar]
- 25.Nicholl MC, Cattell MA. Getting evidence into obstetric practice: appropriate timing of elective caesarean section. Aust Health Rev. 2010;34(1):90–92. doi: 10.1071/AH09690. [DOI] [PubMed] [Google Scholar]