Abstract
Objective
Extracranial internal carotid artery (ICA) angioplasty and intracranial thrombectomy may be a safe and efficacious therapeutic option for recanalization of a subset of arterial occlusions termed tandem occlusions of Internal carotid artery and Middle cerebral artery (TIM).
Background
Approximately 25% of patients with middle cerebral artery (MCA) occlusion will have a concomitant ICA occlusion and 50% of patients with an ICA occlusion will have a proximal MCA occlusion. Cervical ICA occlusion with MCA embolic occlusion is associated with a low rate of recanalization and poor outcome after intravenous thrombolysis. We report our experience on acute ischemic stroke patients with TIM occlusion treated with extracranial ICA angioplasty/stenting and intracranial thrombectomy and/or standard intravenous thrombolysis.
Design/Methods
A retrospective analysis of 7 patients from our stroke database was done. 6 patients of the 7 patients were treated with extracranial ICA angioplasty and intracranial thrombectomy and/or intravenous thrombolysis. We examined early neurological improvement (defined by a reduction of National Institutes of Health Stroke Scale (NIHSS) > 8 points). We also evaluated the rate of successful recanalization based on thrombolysis in cerebral infarction (TICI) score of 2b or 3.
Results
All but one of the 6 treated patients achieved a TICI score of 2b or 3 signifying successful recanalization. In addition, treated patients had an early reduction of their NIHSS by greater than 8 points. The 1 patient who did not to achieve TICI 2b or 3 also failed to show early neurological improvement. Four of the treated patients had a follow up NIHSS at 90 days of 1 or less and mRS at 90 days of 0.
Conclusions
In cases of tandem occlusions of ICA and MCA, multimodal therapy consistent of intravenous thrombolysis and/or extracranial ICA stenting and intracranial thrombectomy to achieve recanalization may be a safe and efficacious therapeutic option for recanalization. Further prospective studies are warranted.
Introduction
C Miller Fisher objectively defined the symptoms of occlusive carotid artery disease in 1951 as causing ischemic symptoms on the ipsilateral eye and corresponding ipsilateral cerebral hemisphere (7). Since then there has been a plethora of studies and articles investigating the different types of occlusive carotid disease and their treatment modalities. In majority of cases the mechanism of stroke has been attributed to thrombus that forms over the atheroma within carotid arteries resulting in narrowing of the artery as a result of the atherosclerotic plaque itself with subsequent embolization and occlusion of more distal vessels as well (6- 8, 16-17, 19). Studies such as the NASCET and ACAS endarterectomy trials have elucidated that the ulceration of atherosclerotic plaques is the cause of thrombus formation that eventually leads to embolization into distal vessels causing ischemic strokes in patients who were symptomatic (5, 21). Over the years, various treatment modalities have emerged entailing treatment of acute ischemic stroke within the historic 3 to 4.5 hour window of time of symptom onset (10,25). Intravenous thrombolysis is the only FDA approved treatment modality that has been used widely in acute ischemic strokes albeit achieving complete recanalization in only 30-40% of patients who are treated (1,25). Lack of complete recanalization in patients using IV thrombolysis is partly due to a heterogeneous group of factors such as differences in time to treatment, size and location of arterial occlusion as well as the specific type of stroke subtype (4). Various studies have shed light into the effect of the location of arterial occlusion on clinical outcomes after an ischemic stroke. For instance, lower MCA recanalization rates with IV thrombolysis have been documented along with poor outcomes in a subtype of carotid occlusion often termed as a Tandem Internal carotid artery/Middle cerebral artery occlusion (TIM) (2, 14, 18). In fact, approximately 25% of patients with middle cerebral artery (MCA) occlusion will have a concomitant ICA occlusion and 50% of patients with an ICA occlusion will also have a proximal MCA occlusion (2-4). Such aforementioned patients with TIM occlusion have poor recanalization rate and response as quantified by clinical outcomes to intravenous thrombolysis (3). Kim et al investigated early recanalization rates and clinical outcomes in 104 patients with TIM occlusion and concluded lower early recanalization rates after administering IV tPA when compared to the controls (patients with isolated MCA occlusion) (15). The different response of recanalization in TIM occlusions when compared to isolated occlusions (such as MCA occlusions) can in part be secondary to differences in the hemodynamic flow conditions in addition to the actual degree of exposure to the thrombolytic agent that the tandem clots face in a TIM occlusion (16). In this report, we aimed to demonstrate our experience on acute ischemic stroke patients with TIM occlusion who were treated with a different treatment modality other than conventional intravenous thrombolysis; that which entailed extracranial ICA angioplasty/stenting and intracranial thrombectomy and/or standard intravenous thrombolysis.
Design/Methods
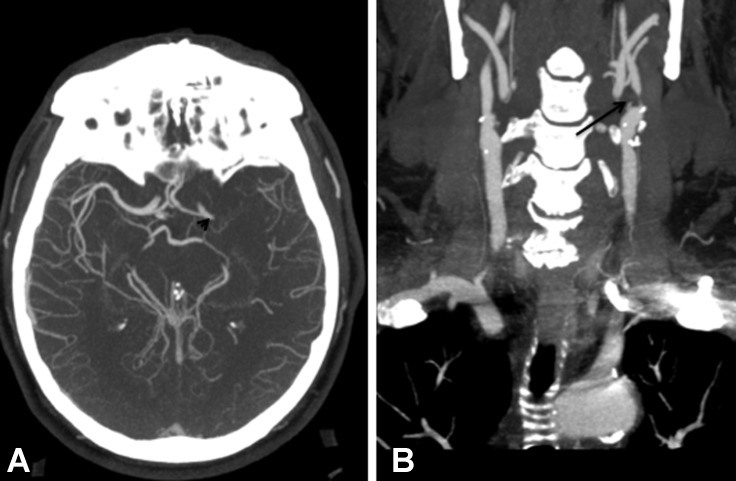
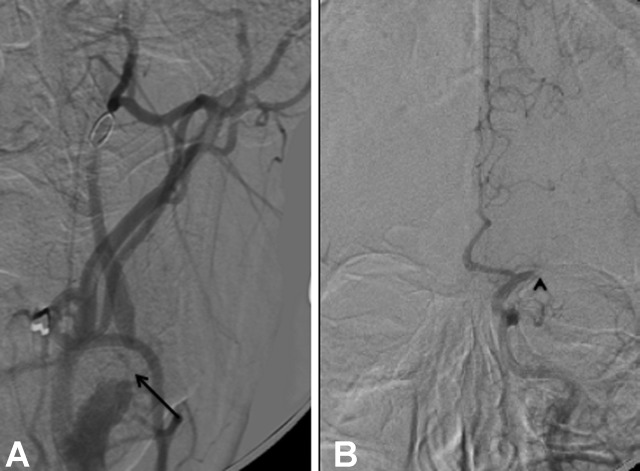
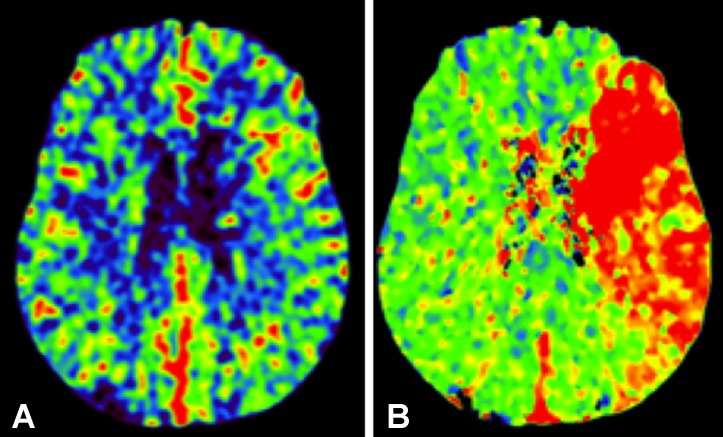
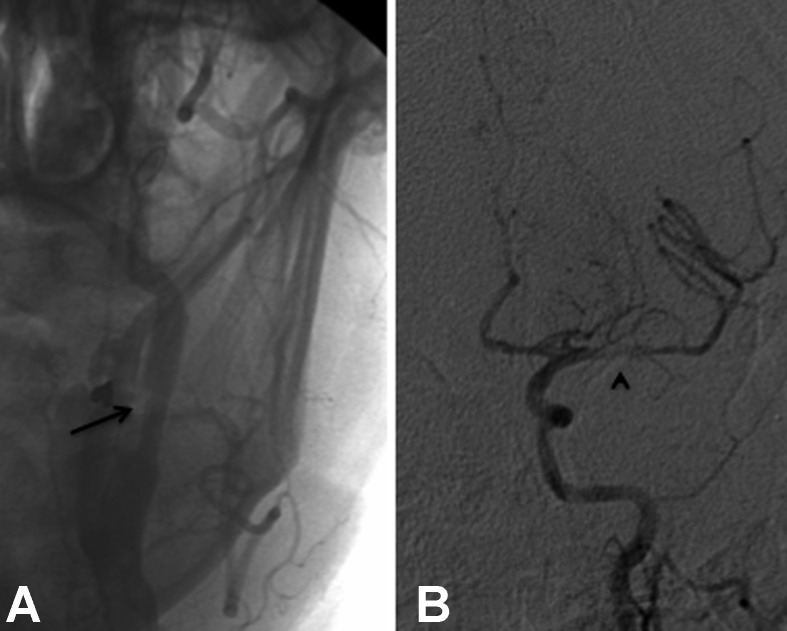
We performed a retrospective analysis of our stroke database at a university teaching hospital from July 2010 to August 2011. Our analysis was done after seeking institutional review board (IRB) approval. We retrospectively examined the first 7 patients that were found to have angiographically confirmed TIM occlusion (Figure 1). Several factors were taken into account when determining patient selection inclusion. We first determined angiographically the presence of adequate collateral flow arising from different arteries (from either ipsilateral or contralateral cerebral hemisphere) supplying the tissue that was within the vascular distribution of the occluded MCA prior to endovascular intervention. A CT perfusion was also obtained to determine and ensure the preservation of cerebral blood volume (CBV) in the area of MCA occlusion (Figure 2). This would allow us to objectively show if the tissue area was within the realm of salvagability or penumbra. During the endovascular procedure, the occluded internal carotid artery was first recanalized in 5 patients with either stenting and/or balloon angioplasty (Figure 3). By ensuring recanalization of the proximal occluded internal carotid artery, we augmented the reperfusion hemodynamics to the more distal MCA occlusion which ultimately contributed to faster reperfusion/recanalization of the MCA. In addition, a thrombectomy device was applied to the occluded MCA. Two of the five patients who underwent a combined ICA stening/angioplasty with thrombectomy from the MCA had contraindications to thrombolysis and hence tPA was not administered. Out of the 7 patients, 6 were treated with extracranial ICA angioplasty and intracranial thrombectomy and/or intravenous thrombolysis. Of the 6 patients treated, one failed to attain any degree of recanalization by both endovascular and through thrombolysis. This was thought to be as a consequence of a chronically occluded ICA. 1 of the 7 patients elected not to undergo treatment (refer tables for patient demographics and stroke outcome).
Figure (1): CT angiography of the head and neck showing (A) left MCA occlusion (arrowhead) and (B) ICA string sign (arrow).
Figure (2): Patient with example of tandem occlusion, (A) proximal ICA occlusion (arrow) and (B) MCA occlusion (arrowhead).
Figure (3): CT perfusion maps showing evidence of (A) preserved cerebral blood volume and (B) increased time to peak indicating big tissue at risk with small infarct territory.
We examined early neurological improvement post treatment, objectively defined for the purpose of our analysis to be a reduction of National Institutes of Health Stroke Scale (NIHSS) > 8 points at 24 hours. We also evaluated and objectified successful reperfusion based on the thrombolysis in cerebral infarction (TICI) score of 2b or 3.
Results
All but one of the patients treated with extracranial ICA angioplasty and intracranial thrombectomy with or without intravenous thrombolysis achieved a TICI score of 2b or 3 signifying successful reperfusion. In addition, patients who were treated also achieved a significant clinical improvement as defined by an early reduction of their NIHSS by greater than 8 points at 24 hours. It should be noted that 1 of the 6 patients who failed to achieve good reperfusion after the endovascular intervention did not achieve early neurological improvement. Four of the treated patients had a follow up 90 day NIHSS 1 or less. In addition, the modified Rankin Score (mRS) at 90 days was 0 for these aforementioned four patients who underwent treatment.
Discussion
Studies have shown symptomatic ICA occlusion to cause increased risk of additional strokes averaging to about 16 % at 2 years (9). Furthermore, data from different studies have shown that tandem occlusions involving ICA and MCA are often very highly symptomatic with only 20% cases showing good clinical outcomes after only intravenous thrombolysis (22). In fact, this marginal improvement in clinical outcome is reflected in both short and long term outcomes (22). Different intracranial vessels respond differently to intravenous thrombolysis in terms of recanalization rates as demonstrated by Linfante et al. who showed a 31% recanalization rate after using intravenous thrombolysis in patients with ICA occlusion compared to 88% in patients with MCA occlusion (18). We demonstrated that application of a multimodal therapy using endovascular modalities such as extracranial ICA stenting with intracranial thrombectomy with or without the use of intravenous thrombolysis is safe and efficacious (12). Various other studies have also shown similar beneficial effect in achieving good clinical outcomes after employing a multimodal extracranial ICA stenting with intracranial thrombectomy in TIM occlusions (12). None of the patients in our case series undergoing multimodal treatment developed hemorrhagic transformation or hypoperfusion related complications post procedure. The successful profile of this multimodal therapeutic option is highlighted via achieving a higher rate of reperfusion in addition to showing good clinical outcomes. Recently, Broderick et al presented a subgroup analysis of patients in the International Management of Stroke (IMS) 3 trial with a positive CTA showing a T-junction ICA occlusion and or T-junction ICA occlusion plus M1 occlusion. In this subset of patients, only 4 % had a good outcome, defined by mrs 0-2 at 90 days with IV tpa, whereas patients in the combined IV and IA endovascular group had 26% better outcomes.
However, Broderick et al also validated their findings during the 2013 International stroke conference that showed the subset of patients in IMS 3 with a Computed Tomographic Angiography (CTA) confirmed occlusion at baseline, showed a clinically significant difference when a combination of IV and IA tpa was administered compared to IV tpa alone, with statistical significance (p value) of 0.0114. Nevertheless it becomes important to note that the aforementioned role of combination IV and IA tpa versus IV tpa alone was nullified in the original IMS 3 paper due to the p value cut off being set at 0.01 for the purpose of the study, whereas the value attained during the study was only marginally higher at 0.0114.
In our cohort of patients, the percentage of a good outcome was better than that of IMS 3 due to faster rate of attaining recanalization from the time of symptom onset and due to the fact that we employed multiple therapeutic modalities in achieving recanalization, unlike a unimodal endovascular therapeutic modality that was used in the IMS 3 trial. The IMS 3 also noted that patients with a confirmed occlusion on the CTA had faster IV tpa to groin puncture time and faster groin puncture to IA tpa time (p value less than 0.01). This validates that health care providers would expedite the transfer of the patient to the endovascular catheter suite for initiating treatment once an occlusion is objectified on CTA.
A multimodal treatment option augments a higher degree of blood flow restoration, which may prevent the expansion of the ischemic penumbra into an infarct core (13, 23, 26). Since the size of ischemic core is known to correlate with clinical outcome, a multimodal endovascular approach may maximize the chances of favorable clinical outcomes if performed in a timely manner (22). This effect would not be as pronounced when a single modality treatment approach such as intravenous thrombolysis is applied to TIM occlusion (13). The application of endovascular therapies in treating TIM occlusions can also define radiographically the length of the occluded ICA with precision when compared to endarterectomy. In addition to providing better visualization of other diseased intracranial vascular structures, an endovascular approach also simultaneously allows better access to additional intracranial lesions (12). Studies have also shown the ability to navigate through an occluded proximal ICA after angioplasty to be an adjunct to intracranial intervention thereby increasing recanalization of an occluded intracranial artery when compared to the application of systemic intravenous thrombolysis alone (20,24). This concept of achieving an augmented ipsilateral hemispheric cerebral blood flow has shown to be positively correlated and associated with achieving MCA recanalization before systemic thrombolysis is administered (11). Therefore, an endovascular multimodality approach utilizing extracranial ICA angioplasty in the setting of TIM occlusions will result in greater proximal flow restoration that would ultimately lead to enhanced collateral supply resulting in superior distal hemodynamics leading to, in turn, higher distal recanalization rates (12).
Our study, despite showing positive results of a multimodal endovascular approach in treating TIM occlusion does have certain limitations. Primarily, the study is prone to selection bias owing to its retrospective nature. In addition, there were multiple thrombectomy techniques (techniques or devices) that were used to treat the tandem occlusions leading to a lack of standardization of techniques. Furthermore, the small number of patients that were analyzed limits the power of our retrospective analysis.
In conclusion, our experience with patients presenting with TIM occlusion undergoing endovascular multimodality approach highlights the reasonable efficacy, safety, and feasibility of this treatment in the short and long term clinical outcomes. Further prospective, randomized double blind studies in multicenter settings are needed to validate our findings.
Figure (4): Patient post treatment with (A) ICA stenting (arrow) and (B) thrombectomy of the MCA (arrowhead), showing an evidence of recanalization of both arteries.
Table (1): Patients demographic.
| Subject | Age | Race | CAD | HTN | Afib | HLD | Smoking | COPD | DM |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 65 | white | yes | yes | no | no | yes | no | no |
| 2 | 18 | hispanic | no | no | no | no | no | no | no |
| 3 | 55 | white | yes | yes | no | yes | no | no | no |
| 4 | 58 | white | yes | no | no | yes | yes | no | no |
| 5 | 62 | white | yes | yes | no | no | yes | no | yes |
| 6 | 53 | white | no | no | no | no | no | yes | yes |
| 7 | 69 | white | yes | yes | yes | yes | yes | no | no |
Table (2): Patient stroke outcome.
| Subject | Age | Gender | NIHSS | Endovascular treatment | t-PA | mRS at discharge | NIHSS 24 | recanalization at 24 hr | NIHSS 90 | mRS 90 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 65 | F | 20 | yes | no | 2 | 7 | TICI III | na | na |
| 2 | 18 | F | 15 | yes | yes | 0 | 1 | TICI III | 0 | 0 |
| 3 | 55 | M | 9 | yes | no | 1 | 2 | TICI III | 1 | 0 |
| 4 | 58 | M | 23 | yes | yes | 0 | 1 | TICI III | 0 | 0 |
| 5 | 62 | F | na | yes | yes | 0 | 0 | TICI IIb | 1 | 0 |
| 6 | 53 | M | 10 | attempt | no | 4 | 10 | TICI 0 | na | 4 |
| 7 | 69 | M | 15 | no | no | 4 | 15 | TICI I | na | 4 |
References
- Alexandrov A. Ultrasound identification and lysis of clots. Stroke. 2004;35:2722–2725. doi: 10.1161/01.STR.0000143321.37482.b3. [DOI] [PubMed] [Google Scholar]
- Christou I, Felberg R, Demchuk A, Burgin W, Malkoff M, Grotta J, et al. Intravenous tissue plasminogen activator and flow improvement in acute ischemic stroke patients with internal carotid artery occlusion. J Neuroimaging. 2002;12:119–123. doi: 10.1111/j.1552-6569.2002.tb00107.x. [DOI] [PubMed] [Google Scholar]
- Dababneh H, Guerrero W, Khanna A, Hoh B, Mocco J. Management of tandem occlusion stroke with endovascular therapy. Neurosurg Focus. 2012;32(5):E16. doi: 10.3171/2012.1.FOCUS11350. [DOI] [PubMed] [Google Scholar]
- El-Mitwalli A, Saad M, Christou I, Malkoff M, Alexandrov A. Clinical and sonographic patterns of tandem internal carotid artery/middle cerebral artery occlusion in tissue plasminogen activator-treated patients. Stroke. 2002;33:99–102. doi: 10.1161/hs0102.101892. [DOI] [PubMed] [Google Scholar]
- Executive Committee for the Asymptomatic Carotid Atherosclerosis Study Endarterectomy for asymptomatic carotid artery stenosis. JAMA. 1995;273:1421. [PubMed] [Google Scholar]
- Fisher CM. Concerning recurrent transient cerebral ischemic attacks. Can Med Assoc J. 1962;86:1091. [PMC free article] [PubMed] [Google Scholar]
- Fisher CM. Occlusion of the internal carotid artery. Arch Neurol Psychiatry. 1951;65(3):346. doi: 10.1001/archneurpsyc.1951.02320030083009. [DOI] [PubMed] [Google Scholar]
- Fisher CM, Karnes WE. Local embolism. J Neuropathol Exp Neurol. 1965;24:174. [Google Scholar]
- Grubb RL, Jr, Derdeyn CP, Fritsch SM, Carpenter DA, Yundt KD, Videen TO, et al. Importance of hemodynamic factors in the prognosis of symptomatic carotid occlusion. J Am Med Assoc. 1998;280:1055–1060. doi: 10.1001/jama.280.12.1055. [DOI] [PubMed] [Google Scholar]
- Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–1329. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- Jovin T, Gebel J, Yonas H, Horowitz M, Jungreis C, Grahovac S. Pretreatment ipsilateral regional cortical blood flow influences vessel recanalization in intra-arterial thrombolysis for MCA occlusion. AJNR Am J Neuroradiol. 2007;28(1):164–7. [PMC free article] [PubMed] [Google Scholar]
- Jovin TG, Gupta R, Uchino K, Jungreis C, Wechsler LR, Hammer MD, et al. Emergent Stenting of Extracranial Internal Carotid Artery Occlusion in Acute Stroke Has a High Revascularization Rate. Stroke. 2005;36:2426–2430. doi: 10.1161/01.STR.0000185924.22918.51. [DOI] [PubMed] [Google Scholar]
- Jovin TG, Yonas H, Gebel JM, Kanal E, Chang YF, Grahovac SZ, et al. The cortical ischemic core and not the consistently present penumbra is a determinant of clinical outcome in acute middle cerebral artery occlusion. Stroke. 2003;34:2426–2433. doi: 10.1161/01.STR.0000091232.81947.C9. [DOI] [PubMed] [Google Scholar]
- Kim YS, Garami Z, Mikulik R, Molina CA, Alexandrov AV. Early recanalization rates and clinical outcomes in patients with tandem internal carotid artery/middle cerebral artery occlusion and isolated middle cerebral artery occlusion. Stroke. 2005;36:869–871. doi: 10.1161/01.STR.0000160007.57787.4c. [DOI] [PubMed] [Google Scholar]
- Kim YS, Garami Z, Mikulik R, Molina CA, Alexandrov AV. Tandem Internal Carotid Artery/Middle Cerebral Artery Occlusion. An Independent Predictor of Poor Outcome After Systemic Thrombolysis Stroke. 2005;36(4):869–871. doi: 10.1161/01.STR.0000160007.57787.4c. [DOI] [PubMed] [Google Scholar]
- Kistler JP, Ropper AH, Heros RC. Therapy of ischemic cerebral vascular disease due to atherothrombosis. N Engl J Med. 1984;311(1):27. doi: 10.1056/NEJM198407053110105. [DOI] [PubMed] [Google Scholar]
- Kistler JP, Ropper AH, Heros RC. Therapy of ischemic cerebral vascular disease due to atherothrombosis. N Engl J Med. 1984;311(2):100. doi: 10.1056/NEJM198407123110206. [DOI] [PubMed] [Google Scholar]
- Linfante I, Linas RH, Selim M, Chaves C, Kumar S, Parker RA, et al. Clinical and vascular outcome in internal carotid artery versus middle cerebral artery occlusions after intravenous tissue plasminogen activator. Stroke. 2002;33:2066–71. doi: 10.1161/01.str.0000021001.18101.a5. [DOI] [PubMed] [Google Scholar]
- Mohr JP. Transient ischemic attacks and the prevention of strokes. N Engl J Med. 1978;299(2):93. doi: 10.1056/NEJM197807132990209. [DOI] [PubMed] [Google Scholar]
- Nesbit GM, Clark WM, O’Neill OR, Barnwell SL. Intracranial intraarterial thrombolysis facilitated by microcatheter navigation through an occluded cervical internal carotid artery. J Neurosurg. 1996;84:387–392. doi: 10.3171/jns.1996.84.3.0387. [DOI] [PubMed] [Google Scholar]
- North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325:445. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E. Tandem Internal Carotid Artery/Middle Cerebral Artery Occlusion. An Independent Predictor of Poor Outcome After Systemic Thrombolysis Stroke. 2006;37:2301–2305. doi: 10.1161/01.STR.0000237070.80133.1d. [DOI] [PubMed] [Google Scholar]
- Schlaug G, Benfield A, Baird AE, Siewert B, Lövblad KO, Parker RA, et al. The ischemic penumbra: operationally defined by diffusion and perfusion MRI. Neurology. 1999;53:1528–1537. doi: 10.1212/wnl.53.7.1528. [DOI] [PubMed] [Google Scholar]
- Spearman MP, Jungreis CA, Wechsler LR. Angioplasty of the occluded internal carotid artery. AJNR Am J Neuroradiol. 1995;16:1791–1796. [PMC free article] [PubMed] [Google Scholar]
- The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–1587. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- Wintermark M, Reichhart M, Thiran JP, Maeder P, Chalaron M, Schnyder P, et al. Prognostic accuracy of cerebral blood flow measurement by perfusion computed tomography, at the time of emergency room admission, in acute stroke patients. Ann Neurol. 2002;51:417–432. doi: 10.1002/ana.10136. [DOI] [PubMed] [Google Scholar]