Abstract
Importance
Non-suicidal and suicidal self-injury are very harmful behaviours and are associated with several psychiatric disorders. In the recently developed 5th version of the DSM, non-suicidal self-injury and suicidal behaviour disorder are for the first time introduced as conditions in their own right, instead of symptoms of other psychiatric disorders. It is unclear to what extent non-suicidal and suicidal self-injurious behaviours share the same underlying biological mechanisms and are influenced by the same environmental factors.
Objective
To determine the relative importance of genetic and environmental influences on the variation in non-suicidal self-injury and suicidal ideation and their covariation.
Design
Classical twin design, using population-based twin sample in which twins participated in semi-structured telephone interviews between 1996 and 2009 which primarily focused on psychiatric disorders.
Setting
General community.
Participants
10678 male and female Australian adult twins (mean age 32.8 years).
Main Outcome Measures
Lifetime presence of self-reported non-suicidal self-injury (NSSI) and suicidal ideation.
Results
The prevalence of NSSI and suicidal ideation was 4.7% and 26.5% and individuals that engaged in self-harm were much more likely to report suicidal ideation, OR(95%CIs)=8.4 (6.8–10.3). Results from a bivariate genetic model indicated that genetic factors explain a substantial part of the variance in both NSSI (37% for males and 59% for females) and suicidal ideation (41% and 55%, respectively), while residual influences (including nonshared environmental influences and measurement error) explain the remainder of the variance. Shared (family) environment did not seem to play a role. Moreover, both behaviours were strongly correlated (r=0.49 for males and 0.61 for females) and this correlation was largely explained by overlapping genetic influences (62% and 76% for males and females, respectively), whereas residual influences accounted for the remainder of the phenotypic correlation.
Conclusions and Relevance
Results indicated that the substantial correlation between NSSI and suicidal ideation is largely driven by overlapping genetic factors, suggesting that the two behaviours share similar biological underpinnings. Overlapping residual influences also explain part of the covariance between the two traits. Future research should further investigate which genetic and environmental influences underlie the vulnerability in NSSI and suicidal ideation.
Self-injurious behaviours are behaviours that are performed intentionally with the goal to injure oneself and include non-suicidal and suicidal behaviours (i.e., without versus with the intention to die)1. Lifetime prevalences in adult community samples are estimated 4–6% for non-suicidal self-injury (NSSI; including self-cutting, biting, or burning)2,3, while they are substantially higher in adolescent (14–47%)4–6 and clinical samples (21–61%)3,7. Lifetime prevalences for suicidal behaviours are estimated 9.2% for suicidal ideation, 3.1% for suicidal plans, and 2.7% for suicide attempts8. Non-suicidal and suicidal self-injurious behaviours are very impairing and associated with an increased risk of psychiatric disorders, such as depression and borderline personality disorder9–12. In the previous version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR)13, non-suicidal and suicidal self-injury were included only as symptoms of certain mental disorders. For instance, NSSI was included as a symptom of borderline personality disorder, although research indicates it also occurs in individuals without borderline14,15. In the recently developed 5th edition of the DSM16, NSSI and suicidal behaviour disorder are introduced as conditions in their own right. The American Psychiatric Association indicates that further research is needed to guide decisions for future editions of the DSM as to whether these conditions should be considered as formal disorders.
Currently, there is a debate about the relationship between NSSI and suicidal self-injury, with some researchers highlighting both behaviours are distinct17, whereas others are more cautious in clearly differentiating these two behaviours18. Numerous studies have noted that non-suicidal and suicidal self-injurious behaviours co-occur frequently14,19,20 and that NSSI longitudinally predicts increased risk of suicidal behaviours21–23. However, non-suicidal and suicidal self-injurious behaviours can also be distinguished from each other based on the following characteristics, see 24: intention (NSSI are not performed with the intention to die, suicidal behaviours are1,25), repetition (NSSI has a higher frequency than suicidal behaviours26,14), and lethality (NSSI includes methods of low lethality, such as burning, whereas suicidal behaviours include methods of higher lethality, such as overdose26). Moreover, studies have shown that suicidal self-injurious behaviours are associated with greater levels of psychological and psychosocial impairment compared to NSSI alone27,11 It is important to investigate whether non-suicidal and suicidal self-injury have the same underlying biological and environmental mechanisms to determine how distinct or similar both behaviours are. Clarifying this relationship is important for both research and treatment24.
Twin studies represent an adequate method to answer this question, as they determine the genetic and environmental influences on traits, but also the extent to which genetic and environmental factors are shared between traits. Studies on suicidal self-injury have found that 30–55% of the variance in suicide attempts and 43–56% in suicidal ideation could be attributed to genetic factors28–31. Studies on NSSI are very rare and findings are inconsistent. For instance, one study showed that thoughts of NSSI were moderately heritable (36%), whereas acts of NSSI were not heritable and solely explained by environmental influences32, although it needs to be noted that this study is limited by a small sample size of 483 twin pairs. Contrastingly, results from an unpublished study among female twins showed that more than half the variance in self-injury was explained by genes. Moreover, this study is –to our knowledge– the only study that has examined the overlapping genetic and environmental influences on NSSI and suicide attempts. Results showed that both behaviours shared a moderate amount of genetic and a very small amount of unique environmental risk31. However, because this study is unpublished, results should be interpreted with caution.
Using a large sample of male and female twins, the present study determined the relative importance of genetic and environmental influences on NSSI and suicidal ideation as well as on the covariance between both behaviours.
Methods
Participants
The study sample consisted of identical (monozygotic; MZ) and non-identical (dizygotic; DZ) twins from the Australian Twin Registry, a population-based twin registry. Between 1996 and 2009 the twins participated in various semi-structured telephone interviews focused on psychiatric disorders (see33–35). In each of these studies, twins completed the same items about NSSI and suicidal ideation. Verbal informed consent was obtained from all participants. Procedures were approved by the Human Studies Committee at Washington University and the Ethics Committee at Queensland Institute of Medical Research.
The combined sample comprised 10678 twins (4429 males and 6249 females), including 1154 female MZ, 693 male MZ, 932 female DZ, 594 male DZ, 1038 opposite sex DZ pairs, and 1856 single twins (single twins were retained as they increase precision of the threshold estimates). The participants’ age ranged from 19 to 75 years (M=32.76, SD=6.99). Zygosity was determined based on standard items about physical similarity, a procedure with high (at least 95%) concurrence with DNA typing36.
Measures
The interview was an adaption of the SSAGA (Semi-Structured Assessment for the Genetics of Alcoholism), which assesses psychiatric disorders in adults and has been shown to be reliable37. NSSI was assessed using the question “Other than when you tried to take your own life, did you ever hurt yourself on purpose, for example, by cutting or burning yourself?” and suicidal ideation was assessed using the question “Have you ever thought about taking your own life?”. Answers were coded with “yes” or “no”.
Data analysis
Descriptive statistics were calculated using SPSS 20.0. In accordance with standard twin analysis, genetic analyses employed maximum-likelihood modelling procedures using the statistical package Mx38. Measures were analyzed as raw dichotomous data, assuming that a normally distributed continuum of liability is cut in two at a certain threshold, yielding two observed categories. In maximum-likelihood modelling, the goodness-of-fit of a model is distributed as chi-square (χ2). By testing the change in chi-square (Δχ2) against the change in degrees of freedom (Δdf), we tested whether dropping or equating specific model parameters significantly worsens the model fit. We used the classical twin design, in which the variance in NSSI and suicidal ideation as well as the covariance between them is portioned into genetic (additive, A, and non-additive, D) and environmental (shared, C, and residual, E) influences. Additive genetic variance includes the influence of summed allelic effects on the liability of a trait, whereas non-additive variance includes dominance (allelic interactions within genes) and epistasis (interaction between multiple genes). Shared environmental variance results from environmental influences shared within twin pairs, making them more similar to each other (e.g., family environment), whereas residual environmental variance represents the variance due to unique experiences as well as measurement error.
Portioning of variance into genetic and environmental components can be achieved because MZ twins share 100% of their genes, whereas DZ twins share on average 50% of their segregating genes. Individual differences in phenotypes are the result of a combination of genetic and environmental influences. Structural equation modelling was used to determine which combination fits the observed data best. Moreover, by examining cross-twin cross-trait correlations, we partitioned the covariance between NSSI and suicidal ideation into genetic and environmental parts. Additional information on the classical twin design can be found elsewhere39,40.
A limitation of the classical twin design is that C and D are confounded and therefore cannot be tested simultaneously in a model with only twins reared together39. The choice of an ACE or ADE model depends on the pattern of MZ and DZ correlations. If the DZ correlation is greater than half the MZ correlation, C is estimated, but if the DZ correlation is smaller than half the MZ correlation, D is estimated41.
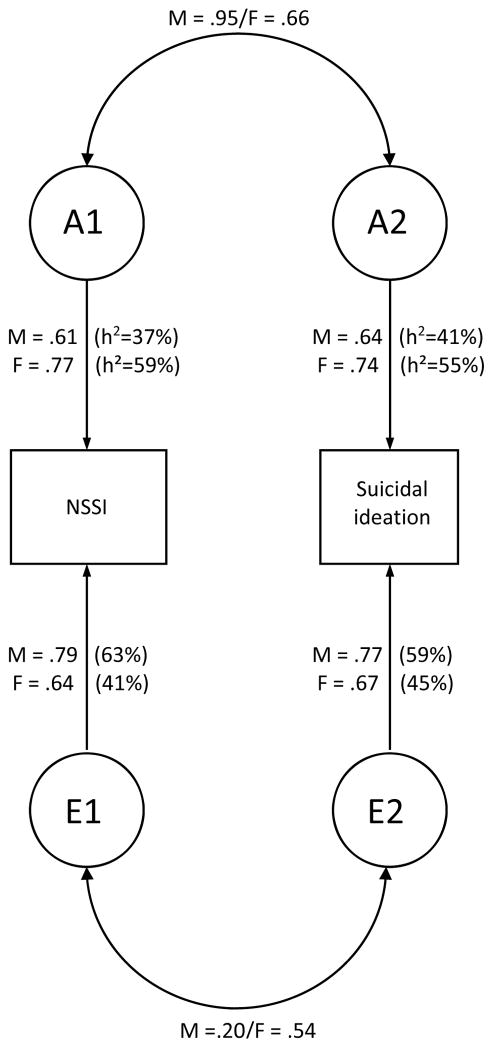
Prior to genetic modelling, we tested for the effects of age, sex, and zygosity on the thresholds of NSSI and suicidal ideation and then included these as fixed effects in the thresholds model as necessary. Subsequently, we fitted models to determine the relative influence of A, C or D, and E. We examined the significance of the genetic and environmental influences by testing whether dropping relevant parameters from the baseline model led to a significant decrease in model fit. For ease of interpretation, the bivariate model was transformed into a correlated factors model42 (see Figure 1).
Figure 1.
Correlated factor model. Graphical presentation of the parameter estimates and proportions of variance in non-suicidal self-injury (NSSI) and suicidal ideation accounted for by additive genetic (A) and residual environmental influences (E). h2 (heritability) is the percentage of variance accounted for by genetic factors. The double-headed arrows represent the genetic and residual correlations, indicating the degree to which the same genetic or residual (including non-shared environmental) factors are influencing the two traits. The residual correlation for males is significant at p=0.049, while all other estimates are significant at p < 0.001.
Results
Descriptive Statistics
Table 1 shows prevalences of and odds ratios (ORs) between NSSI and suicidal ideation for the overall sample as well as separately for males and females. The overall prevalence of NSSI and suicidal ideation was 4.7% and 26.5%. Individuals that engaged in self-harm were much more likely to report suicidal ideation, OR(95%CIs)=8.4 (6.8–10.3).
Table 1.
Frequencies (%) of and Odds Ratios (ORs) between lifetime non-suicidal self-injury (NSSI) and suicidal ideation
| Males | Females | Total | |
|---|---|---|---|
| NSSI (n=10674) | 206 (4.7%) | 300 (4.8%) | 506 (4.7%) |
| Suicidal ideation (n=10668) | 1175 (26.5%) | 1650 (26.4%) | 2825 (26.5%) |
| OR (95%CIs) (n=10664) | 5.97 (4.43–8.06) | 10.91 (8.23–14.47) | 8.39 (6.84–10.29) |
Note. ORs as obtained from Mplus6 accounting for sample nonindependence.
Preliminary Analyses
Before determining the variance components, the effects of sex, age, and zygosity, on the thresholds were tested using an α-level of 0.01. We did not find a significant age effect on suicidal ideation, but we did on NSSI (Δχ21=39.65, p<0.001), showing that younger participants reported lifetime NSSI more often. We did not find a significant sex effect on the thresholds for NSSI nor suicidal ideation, implying there were no differences in the prevalences between males and females. Moreover, levels of NSSI did not significantly differ between MZ and DZ twins in either sex, and neither did the level of suicidal ideation differ between MZ and DZ females. However, males from opposite-sex twin pairs showed a higher prevalence of suicidal ideation than same-sex male twins (Δχ21=9.10, p=0.003), so we did not equate this threshold with the threshold of same sex male pairs in subsequent modelling. We accounted for sex and age effects in subsequent modelling.
Table 2 displays polychoric twin pair correlations for each zygosity group. For both variables, the MZ twin pair correlations were higher than the DZ twin pair correlations, suggesting genetic influences on both traits. Given that the DZ twin pair correlations for both variables were less than half the MZ twin pair correlations, non-additive genetic influences could be expected for both NSSI and suicidal ideation. Therefore, D (and not C) was estimated in the univariate genetic models.
Table 2.
Polychoric twin pair correlations (95% confidence intervals) for lifetime non-suicidal self-injury (NSSI) and suicidal ideation for each zygosity group, estimated in Mx (corrected for age and sex effects)
| MZ females (1154 pairs) | MZ males (693 pairs) | DZ females (932 pairs) | DZ males (594 pairs) | DZ opposite-sex (1038 pairs) | |
|---|---|---|---|---|---|
| NSSI | 0.62 (0.47–0.75) | 0.49 (0.22–0.70) | 0.12 (−0.18–0.39) | −0.10 (−0.47–0.26) | 0.18 (−0.10–0.43) |
| Suicidal ideation | 0.59 (0.51–0.66) | 0.42 (0.29–0.54) | 0.14 (0.02–0.25) | 0.22 (0.08–0.35) | 0.14 (0.03–0.24) |
Genetic model fitting
Table 3 depicts the A, D, and E estimates as obtained from the univariate model. While the estimates of broad-sense heritability (H2; including additive and non-additive genetic influences) were significant for both males and females for either trait, the separate A and D estimates were not significant for NSSI, and for males the D estimate was not significant for suicidal ideation. It should be noted that separate A and D estimates should be treated with caution; A and D are highly confounded as they predict similar (but not identical) patterns of twin pair correlations. Therefore, when A and D are estimated simultaneously in one model, the estimates are imprecise and their relative magnitude can be biased depending on the extent of non-additive genetic effects (dominance and epistasis). However, broad-sense heritability is quite robustly estimated with a classical twin design using only twins reared together39,43. For this reason, we only estimated A and E in the bivariate model, where A will have captured both the additive and non-additive genetic influences.
Table 3.
Estimates (and 95% CIs) of the proportion of variance in non-suicidal self-injury (NSSI) and suicidal ideation
| NSSI | Suicidal Ideation | |||
|---|---|---|---|---|
|
| ||||
| Males | Females | Males | Females | |
|
| ||||
| A | 0.11 (0.00–0.61) | 0.19 (0.00–0.71) | 0.43 (0.33–0.53) | 0.13 (0.01–0.38) |
| D | 0.35 (0.00–0.67) | 0.43 (0.00–0.74) | 0.00 (0.00–0.38) | 0.45 (0.15–0.61) |
| H2 (A+D) | 0.46 (0.18–0.68) | 0.62 (0.47–0.74) | 0.43 (0.31–0.53) | 0.58 (0.50–0.66) |
| E | 0.54 (0.32–0.82) | 0.38 (0.26–0.53) | 0.57 (0.47–0.69) | 0.42 (0.34–0.50) |
Note. A = additive genetic influences, D = nonadditive genetic influences, E = residual environmental influences. H2 (A + D) represents broad-sense heritability (in bold).
Figure 1 depicts the parameter estimates of the bivariate model, separately for males and females. Specifically, the figure shows proportions of variance in NSSI and suicidal ideation accounted for by genetic (heritability, h2) and residual influences as well as the genetic and residual correlations. Parameter estimates could not be equated between males and females (Δχ23=15.84, p=0.001). To test the significance of each path in Figure 1, genetic and environmental parameters were dropped from the bivariate AE model (separately for males and females) and model fit was compared using an α-level of 0.05 (Table 4). Results showed that the genetic influences on NSSI (A=0.37 for males and 0.59 for females) and suicidal ideation (A=0.41 for males and 0.55 for females) were significant, see models 5 and 6 (Table 4). Moreover, the phenotypic correlation between NSSI and suicidal ideation (0.49 for males and 0.61 for females) as well as the genetic and residual correlations were significant, see models 2, 3, and 4, respectively (Table 4).
Table 4.
Goodness-of-fit statistics for bivariate models of non-suicidal self-injury (NSSI) and suicidal ideation
| Model | Males | Females | ||||||
|---|---|---|---|---|---|---|---|---|
| versus | Δdf | Δχ2 | p | versus | Δdf | Δχ2 | p | |
| 1 Full model | ||||||||
| 2 Test significance of phenotypic correlation between NSSI and suicidal ideation; Drop genetic and residual environmental cross-paths | 1 | 2 | 160.53 | < 0.001 | 1 | 2 | 352.71 | < 0.001 |
| 3 Test significance of the genetic correlation between NSSI and suicidal ideation; Drop genetic cross-path | 1 | 1 | 27.72 | < 0.001 | 1 | 1 | 58.76 | < 0.001 |
| 4 Test significance of the residual correlation between NSSI and suicidal ideation; Drop residual environmental cross-path | 1 | 1 | 3.87 | 0.049 | 1 | 1 | 28.81 | < 0.001 |
| 5 Test significance of the genetic influences on NSSI; Drop genetic influence on NSSI | 1 | 1 | 29.74 | < 0.001 | 1 | 1 | 77.19 | < 0.001 |
| 6 Test significance of the genetic influences on suicidal ideation; Drop genetic influence on suicidal ideation | 1 | 2 | 65.21 | < 0.001 | 1 | 2 | 165.90 | < 0.001 |
From the estimates in Figure 1, we calculated (see 44) the extent to which the phenotypic correlation could be attributed to genetic factors: For males this calculation is (0.61*0.95*0.64)/(0.61*0.95*0.64+0.79*0.20*0.77=0.76), showing that overlapping genetic factors accounted for 76% of the phenotypic correlation between NSSI and suicidal ideation, with the remaining 24% accounted for by correlated residual influences. For females, 62% of the phenotypic variance was due to common genetic factors, and 38% to residual influences.
Discussion
We examined genetic and environmental influences on NSSI and suicidal ideation as well as on the covariance between both behaviours using data from 10678 twins. Lifetime prevalences of NSSI and suicidal ideation were 4.7% and 26.5% and endorsing NSSI was related to an increased risk of suicidal ideation OR(95%CIs)=8.4 (6.8–10.3). Results of the genetic analyses showed that NSSI and suicidal ideation were moderately heritable. Moreover, both behaviours were highly correlated (r=0.49 for males, 0.61 for females) and the majority of the phenotypic correlations was due to overlapping genetic influences (76% for males, 62% for females), while overlapping residual influences (including non-shared environmental influences and measurement error) accounted for the remainder. This implies that NSSI and suicidal ideation are partly influenced by the same biological mechanisms.
These findings are consistent with prior findings of suicidal self-injury, indicating that approximately half of the variance in suicidality is explained by genes and the other half by residual environmental influences, whereas shared (family) environmental influences do not play a substantial role29–31. Previous twin studies on NSSI were based on a small sample size32 or only examined females31 and showed inconsistent results; Jang et al. (1996) did not find significant genetic influences on NSSI, while Durrett31 found that the variance in NSSI was largely accounted for by genetic factors, consistent with our findings.
Most importantly, we examined the overlap in genetic and environmental influences on NSSI and suicidal ideation. Consistent with previous studies21,22, we found a high phenotypic correlation between both behaviours. Furthermore, this comorbidity was largely driven by overlapping genetic factors and to a smaller degree by overlapping residual influences, which is in accordance with the findings from an unpublished study by Durret31.
More generally, our results are consistent with other studies that also found high phenotypic correlations between disorders from the same spectrum (e.g., depression and anxiety), as well as high genetic, considerably lower unique environmental, and very low/absent shared environmental correlations between these highly comorbid disorders45–48. On the other hand, disorders from different spectra show substantially lower phenotypic correlations and a much lower genetic correlation46,35.
Findings from these studies indicate that genetic influences that are overlapping between NSSI and suicidal ideation may also partly underlie vulnerability to other mental problems such as depression and anxiety. Liability to NSSI and suicidal ideation as well as other highly correlated disorders from the same spectrum may be influenced largely by the same underlying genetic/biological factors, but the exact disorder that develops among vulnerable individuals within the spectrum may be more dependent on unique environmental influences.
Future research should further investigate which genetic and environmental influences underlie vulnerability in NSSI and suicidal ideation. Previous research has identified some potential biological influences. For instance, meta-analyses of molecular genetic studies have shown that polymorphisms in the tryptophan hydroxylase gene (TPH)49 and the serotonin transporter gene promoter (5-HTTLPR)50, which both play important roles in serotonin functioning, are linked to suicidal self-injurious behaviours. Studies on the molecular underpinnings of NSSI are rare, but also implicate dysfunctions in the serotonin system51,52. Serotonin may play a role, because it is linked to impaired emotion regulation and impulsivity53, which are in turn associated with self-injurious behaviours54–56. Other studies point to a possible influence of endogenous opioids, which play a role in disordered pain and reward, for both suicide and NSSI57.
Previous studies have also identified some potential unique environmental influences. For instance, studies have shown that early traumatic childhood experiences (i.e., abuse and neglect)58–62, peer victimization and bullying63–66, and intimate partner violence and abuse67–70 are associated with an increased risk of self-injurious behaviours. Studies that directly compare NSSI and suicidal behaviours to investigate the differential effect of unique environmental contributions are however rare, although studies suggest that compared with NSSI, suicidal behaviours are associated with more stressful life events71 and greater sexual and emotional abuse72.
The present study is not without limitations, most of which are concerned with the classical twin design. For instance, one assumption of the classical twin design is that there are no effects of gene-environment correlation or interaction; not modelling these influences may lead to biased estimates. Another limitation is that C and D cannot be modelled simultaneously and that simultaneously estimating A and D influences leads to imprecise estimates. Lastly, an important limitation is that we only used single item responses to determine lifetime NSSI and suicidal ideation: This could have led to miss-estimation of the prevalences. However, the prevalence of NSSI in our sample (4.7%) is consistent with prevalences reported in previous adult population samples2,3. Furthermore, for a subsample of the individuals that endorsed the NSSI item (N=240), data were available regarding the specific self-injurious behaviours they had endorsed, showing that severer forms of self-injurious behaviours (e.g., cutting was endorsed 64%, burning 23%) were reported more frequently than moderate forms (e.g., scratching oneself, punching oneself, punching a hard object were endorsed about 10% each). Note that due to a lack of power we were unable to run analyses on this subgroup only. Our prevalence for suicidal ideation is relatively high potentially because the question did not distinguish between brief and sustained suicidal ideation. Given our crude assessment, it is likely that some of the non-shared environmental variance in and covariance between our measures is due to measurement error, which could have resulted in an overestimation of E and underestimation of A influences.
Despite these limitations, the present study made an important contribution to the current debate about the relationship between NSSI and suicidal ideation. We showed that both behaviours are substantially influenced by genetic and residual environmental factors. Furthermore, we found that the substantial correlation between NSSI and suicidal ideation is largely driven by overlapping genetic factors, suggesting that the two behaviours share similar biological underpinnings. Overlapping residual influences also explain part of the covariance between the two traits. An important goal for future research is to investigate which overlapping and specific genetic and environmental influences underlie the vulnerability in NSSI and suicidal ideation.
Acknowledgments
Supported by National Institutes of Health Grants AA07535, AA0758O, AA07728, AA10249, AA13320, AA13321, AA14041, AA11998, AA17688, DA012854, DA018267, DA018660, DA23668 and DA019951; by Grants from the Australian National Health and Medical Research Council (241944, 339462, 389927, 389875, 389891, 389892, 389938, 442915, 442981, 496739, 552485, 552498, and 628911). This research was further supported by the Centre for Research Excellence on Suicide Prevention (CRESP - Australia) and the Netherlands Organization for Health Research and Development, ZonMW 31160212 (NON, HEC).
We thank Anjali Henders, Richard Parker, Soad Hancock, Judith Moir, Sally Rodda, Pieta-Maree Shertock, Heather Park, Jill Wood, Pam Barton, Fran Husband, Adele Somerville,, David Smyth, Harry Beeby, and Daniel Park. Last, we thank the twins and their families for their participation.
Footnotes
Conflict of interest: The authors declare no conflict of interest.
The authors declare no conflict of interest.
KJHV had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The funding organisations played no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Nock MK. Self-Injury. Annu Rev Clin Psychol. 2010;6(1):339–363. doi: 10.1146/annurev.clinpsy.121208.131258. [DOI] [PubMed] [Google Scholar]
- 2.Klonsky ED. Non-suicidal self-injury in United States adults: prevalence, sociodemographics, topography and functions. Psychol Med. 2011;41(9):1981–1986. doi: 10.1017/S0033291710002497. [DOI] [PubMed] [Google Scholar]
- 3.Briere J, Gil E. Self-mutilation in clinical and general population samples: Prevalence, correlates, and functions. Am J Orthopsychiatry. 1998;68(4):609–620. doi: 10.1037/h0080369. [DOI] [PubMed] [Google Scholar]
- 4.Plener PL, Libal G, Keller F, Fegert JM, Muehlenkamp JJ. An international comparison of adolescent non-suicidal self-injury (NSSI) and suicide attempts: Germany and the USA. Psychol Med. 2009;39(9):1549–1558. doi: 10.1017/S0033291708005114. [DOI] [PubMed] [Google Scholar]
- 5.Lloyd-Richardson EE, Perrine N, Dierker L, Kelley ML. Characteristic and functions on non-suicidal self-injury in a community sample of adolescents. Psychol Med. 2007;37(8):1183–1192. doi: 10.1017/S003329170700027X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ross S, Heath N. A study of the frequency of self-mutilation in a community sample of adolescents. J Youth Adolescence. 2002;31(1):67–77. [Google Scholar]
- 7.DiClemente RJ, Ponton LE, Hartley D. Prevalence and correlates of cutting behavior: Risk for HIV transmission. J Am Acad Child Psy. 1991;30(5):735–739. [PubMed] [Google Scholar]
- 8.Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Brit J Psychiat. 2008;192(2):98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andover MS, Pepper CM, Ryabchenko KA, Orrico EG, Gibb BE. Self-mutilation and symptoms of depression, anxiety, and borderline personality disorder. Suicide Life Threat Behav. 2005;35(5):581–591. doi: 10.1521/suli.2005.35.5.581. [DOI] [PubMed] [Google Scholar]
- 10.Hankin BL, Abela JRZ. Nonsuicidal self-injury in adolescence: Prospective rates and risk factors in a 2 ½ year longitudinal study. Psychiatry Res. 2011;186(1):65–70. doi: 10.1016/j.psychres.2010.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jacobson CM, Muehlenkamp JJ, Miller AL, Turner JB. Psychiatric impairment among adolescents engaging in different types of deliberate self-harm. J Clin Child Adolesc Psychol. 2008;37(2):363–375. doi: 10.1080/15374410801955771. [DOI] [PubMed] [Google Scholar]
- 12.Brent DA, Perper JA, Moritz G, Allman C, Friend AMY, Roth C, et al. Psychiatric risk factors for adolescent suicide: A case-control study. J Am Acad Child Psy. 1993;32(3):521–529. doi: 10.1097/00004583-199305000-00006. [DOI] [PubMed] [Google Scholar]
- 13.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington: American Psychiatric Association; 2000. Text revision. [Google Scholar]
- 14.Nock MK, Joiner TE, Jr, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: Diagnostic correlates and relation to suicide attempts. Psychiatry Res. 2006;144(1):65–72. doi: 10.1016/j.psychres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 15.Selby EA, Bender TW, Gordon KH, Nock MK, Joiner TE., Jr Non-suicidal self-injury (NSSI) disorder: a preliminary study. J Pers Disord. 2012;3(2):167–175. doi: 10.1037/a0024405. [DOI] [PubMed] [Google Scholar]
- 16.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 17.Butler AM, Malone K. Attempted suicide v. non-suicidal self-injury: behaviour, syndrome or diagnosis? Br J Psych. 2013;202(5):324–325. doi: 10.1192/bjp.bp.112.113506. [DOI] [PubMed] [Google Scholar]
- 18.Kapur N, Cooper J, O’Connor RC, Hawton K. Non-suicidal self-injury v. attempted suicide: new diagnosis or false dichotomy? Br J Psych. 2013;202(5):326–328. doi: 10.1192/bjp.bp.112.116111. [DOI] [PubMed] [Google Scholar]
- 19.Fliege H, Kocalevent R-D, Walter OB, Beck S, Gratz KL, Gutierrez PM, et al. Three assessment tools for deliberate self-harm and suicide behavior: Evaluation and psychopathological correlates. J Psychosom Res. 2006;61(1):113–121. doi: 10.1016/j.jpsychores.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 20.Klonsky ED, May AM, Glenn CR. The relationship between nonsuicidal self-injury and attempted suicide: Converging evidence from four samples. J Abnorm Psychol. 2013;122(1):231–237. doi: 10.1037/a0030278. [DOI] [PubMed] [Google Scholar]
- 21.Asarnow JR, Porta G, Spirito A, Emslie G, Clarke G, Wagner KD, et al. Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: Findings from the TORDIA study. J Am Acad Child Psy. 2011;50(8):772–781. doi: 10.1016/j.jaac.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilkinson P, Kelvin R, Roberts C, Dubicka B, Goodyer I. Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT) Am J Psychiatry. 2011;168(5):495–501. doi: 10.1176/appi.ajp.2010.10050718. [DOI] [PubMed] [Google Scholar]
- 23.Prinstein MJ, Nock MK, Simon V, Aikins JW, Cheah CSL, Spirito A. Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. J Consult Clin Psych. 2008;76(1):92–103. doi: 10.1037/0022-006X.76.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamza CA, Stewart SL, Willoughby T. Examining the link between nonsuicidal self-injury and suicidal behavior: A review of the literature and an integrated model. Clin Psychol Rev. 2012;32(6):482–495. doi: 10.1016/j.cpr.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 25.Muehlenkamp JJ, Gutierrez PM. An investigation of differences between self-injurious behavior and suicide attempts in a sample of adolescents. Suicide and Life-Threatening Behavior. 2004;34(1):12–23. doi: 10.1521/suli.34.1.12.27769. [DOI] [PubMed] [Google Scholar]
- 26.Andover MS, Gibb BE. Non-suicidal self-injury, attempted suicide, and suicidal intent among psychiatric inpatients. Psychiatry Res. 2010;178(1):101–105. doi: 10.1016/j.psychres.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 27.Claes L, Muehlenkamp J, Vandereycken W, Hamelinck L, Martens H, Claes S. Comparison of non-suicidal self-injurious behavior and suicide attempts in patients admitted to a psychiatric crisis unit. Pers Indiv Differ. 2010;48(1):83–87. [Google Scholar]
- 28.Fu Q, Heath AC, Bucholz KK, Nelson EC, Glowinski AL, Goldberg J, et al. A twin study of genetic and environmental influences on suicidability in men. Psychol Med. 2002;32(1):11–24. doi: 10.1017/s0033291701004846. [DOI] [PubMed] [Google Scholar]
- 29.Glowinski AL, Bucholz KK, Nelson EC, Fu Q, Madden PAF, Reich W, et al. Suicide attempts in an adolescent female twin sample. J Am Acad Child Psy. 2001;40(11):1300–1307. doi: 10.1097/00004583-200111000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Statham DJ, Heath AC, Madden PA, Bucholz KK, Bierut L, Dinwiddie SH, et al. Suicidal behaviour: An epidemiological and genetic study. Psychol Med. 1998;28(4):839–855. doi: 10.1017/s0033291798006916. [DOI] [PubMed] [Google Scholar]
- 31.Durrett C. A behavior genetic study of self-harm, suicidality, and personality in African American and White women. unpublished dissertation retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2009-99240-047&site=ehost-live.
- 32.Jang KL, Livesley WJ, Vernon PA, Jackson DN. Heritability of personality disorder traits: a twin study. Acta Psychiatr Scand. 1996;94(6):438–444. doi: 10.1111/j.1600-0447.1996.tb09887.x. [DOI] [PubMed] [Google Scholar]
- 33.Heath AC, Whitfield JB, Martin NG, Pergadia ML, Goate AM, Lind PA, et al. A quantitative-trait genome-wide association study of alcoholism risk in the community: findings and implications. Biol Psychiatry. 2011;70(6):513–518. doi: 10.1016/j.biopsych.2011.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Knopik VS, Heath AC, Madden PA, Bucholz KK, Slutske WS, Nelson EC, et al. Genetic effects on alcohol dependence risk: re-evaluating the importance of psychiatric and other heritable risk factors. Psychol Med. 2004;34(8):1519–1530. doi: 10.1017/s0033291704002922. [DOI] [PubMed] [Google Scholar]
- 35.Lynskey MT, Agrawal A, Henders A, Nelson EC, Madden PA, Martin NG. An Australian twin study of cannabis and other illicit drug use and misuse, and other psychopathology. Twin Res Hum Genet. 2012;15(5):631–641. doi: 10.1017/thg.2012.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ooki S, Yamada K, Asaka A, Hayakawa K. Zygosity diagnosis of twins by questionnaire. Acta Genet Med Gemellol (Roma) 1990;39(1):109–115. doi: 10.1017/s0001566000005626. [DOI] [PubMed] [Google Scholar]
- 37.Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, Jr, et al. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol. 1994;55(2):149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- 38.Neale MC, Boker SM, Xie G, Maes HH. Mx: Statistical Modeling. 7. Richmond: Department of Psychiatry, Virginia Commonwealth University; 2006. [Google Scholar]
- 39.Posthuma D, Beem AL, de Geus EJ, van Baal GC, von Hjelmborg JB, Iachine I, et al. Theory and practice in quantitative genetics. Twin Res. 2003;6(5):361–376. doi: 10.1375/136905203770326367. [DOI] [PubMed] [Google Scholar]
- 40.Neale MC, Cardon LR. Methodology for genetic studies of twins and families. Boston: Kluwer; 1992. [Google Scholar]
- 41.Van Dongen J, Slagboom PE, Draisma HHM, Martin NG, Boomsma DI. The continuing value of twin studies in the omics era. Nat Rev Genet. 2012;13(9):640–653. doi: 10.1038/nrg3243. [DOI] [PubMed] [Google Scholar]
- 42.Loehlin J. The Cholesky approach: A cautionary note. Behav Genet. 1996;26(1):65–69. [Google Scholar]
- 43.Keller MC, Medland SE, Duncan LE. Are extended twin family designs worth the trouble? A comparison of the bias, precision, and accuracy of parameters estimated in four twin family models. Behav Genet. 2010;40(3):377–393. doi: 10.1007/s10519-009-9320-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Falconer DS, Mackay TFC. Introduction to Quantitative Genetics. 4. Harlow, Essex, UK: Longmans Green; 1996. [Google Scholar]
- 45.Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Major depression and generalized anxiety disorder: Same genes, (partly) different environments? Archives of General Psychiatry. 1992;49(9):716–722. doi: 10.1001/archpsyc.1992.01820090044008. [DOI] [PubMed] [Google Scholar]
- 46.Kendler KS, Prescott CA, Myers J, Neale MC. THe structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60(9):929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 47.Linker J, Gillespie NA, Maes H, Eaves L, Silberg JL. Suicidal ideation, depression, and conduct disorder in a sample of adolescent and young adult twins. Suicide Life Threat. 2012;42(4):426–436. doi: 10.1111/j.1943-278X.2012.00101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Young SE, Rhee SH, Stallings MC, Corley RP, Hewitt JK. Genetic and environmental vulnerabilities underlying adolescent substance use and problem use: General or specific? Behav Genet. 2006;36(4):603–615. doi: 10.1007/s10519-006-9066-7. [DOI] [PubMed] [Google Scholar]
- 49.Bellivier F, Chaste P, Malafosse A. Association between the TPH gene A218C polymorphism and suicidal behavior: A meta-analysis. Am J Med Genet B. 2004;124B(1):87–91. doi: 10.1002/ajmg.b.20015. [DOI] [PubMed] [Google Scholar]
- 50.Lin PY, Tsai G. Association between serotonin transporter gene promoter polymorphism and suicide: Results of a meta-analysis. Biol Psychiatry. 2004;55(10):1023–1030. doi: 10.1016/j.biopsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 51.Fikke LT, Melinder A, Landrø NI. The effects of acute tryptophan depletion on impulsivity and mood in adolescents engaging in non-suicidal self-injury. Hum Psychopharm Clin. 2013;28(1):61–71. doi: 10.1002/hup.2283. [DOI] [PubMed] [Google Scholar]
- 52.Crowell SE, Beauchaine TP, McCauley E, Smith CJ, Stevens AL, Sylvers P. Psychological, autonomic, and serotonergic correlates of parasuicide among adolescent girls. Dev Psychopathol. 2005;17(4):1105–1127. doi: 10.1017/s0954579405050522. [DOI] [PubMed] [Google Scholar]
- 53.Hariri AR, Holmes A. Genetics of emotional regulation: The role of the serotonin transporter in neural function. Trends Cogn Sci. 2006;10(4):182–191. doi: 10.1016/j.tics.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 54.Lynam DR, Miller JD, Miller DJ, Bornovalova MA, Lejuez CW. Testing the relations between impulsivity-related traits, suicidality, and nonsuicidal self-injury: A test of the incremental validity of the UPPS model. Pers Disord. 2011;2(2):151–160. doi: 10.1037/a0019978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gratz KL, Roemer L. The relationship between emotion dysregulation and deliberate self-harm among female undergraduate students at an urban commuter university. Cogn Behav Ther. 2008;37(1):14–25. doi: 10.1080/16506070701819524. [DOI] [PubMed] [Google Scholar]
- 56.Pisani A, Wyman P, Petrova M, Schmeelk-Cone K, Goldston D, Xia Y, et al. Emotion regulation difficulties, youth–adult relationships, and suicide attempts among high school students in underserved communities. J Youth Adolescence. 2013;42(6):807–820. doi: 10.1007/s10964-012-9884-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sher L, Stanley BH. The Role of Endogenous Opioids in the Pathophysiology of Self-Injurious and Suicidal Behavior. Arch Suicide Res. 2008;12(4):299–308. doi: 10.1080/13811110802324748. [DOI] [PubMed] [Google Scholar]
- 58.Joiner TE, Jr, Sachs-Ericsson NJ, Wingate LR, Brown JS, Anestis MD, Selby EA. Childhood physical and sexual abuse and lifetime number of suicide attempts: A persistent and theoretically important relationship. Behav Res Ther. 2007;45(3):539–547. doi: 10.1016/j.brat.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 59.Ystgaard M, Hestetun I, Loeb M, Mehlum L. Is there a specific relationship between childhood sexual and physical abuse and repeated suicidal behavior? Child Abuse Neglect. 2004;28(8):863–875. doi: 10.1016/j.chiabu.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 60.Gratz KL, Conrad SD, Roemer L. Risk factors for deliberate self-harm among college students. Am J Orthopsychiatry. 2002;72(1):128–140. doi: 10.1037//0002-9432.72.1.128. [DOI] [PubMed] [Google Scholar]
- 61.Gratz KL. Factors for deliberate self-harm among female college students: The role and interaction of childhood maltreatment, emotional inexpressivity, and affect intensity/reactivity. Am J Orthopsychiat. 2006;76(2):238–250. doi: 10.1037/0002-9432.76.2.238. [DOI] [PubMed] [Google Scholar]
- 62.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the adverse childhood experiences study. JAMA. 2001;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 63.Giletta M, Scholte RHJ, Engels RCME, Ciairano S, Prinstein MJ. Adolescent non-suicidal self-injury: A cross-national study of community samples from Italy, the Netherlands and the United States. Psychiatry Res. 2012;197(1–2):66–72. doi: 10.1016/j.psychres.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fisher HL, Moffitt TE, Houts RM, Belsky DW, Arseneault L, Caspi A. Bullying victimisation and risk of self harm in early adolescence: longitudinal cohort study. Brit Med J. 2012;344:e2683. doi: 10.1136/bmj.e2683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hinduja S, Patchin JW. Bullying, Cyberbullying, and Suicide. Arch Suicide Res. 2010;14(3):206–221. doi: 10.1080/13811118.2010.494133. [DOI] [PubMed] [Google Scholar]
- 66.Turner HA, Finkelhor D, Shattuck A, Hamby S. Recent victimization exposure and suicidal ideation in adolescents. Arch Pediatr Adolesc Med. 2012;166(12):1149–1154. doi: 10.1001/archpediatrics.2012.1549. [DOI] [PubMed] [Google Scholar]
- 67.Levesque C, Lafontaine M-F, Bureau J-F, Cloutier P, Dandurand C. The influence of romantic attachment and intimate partner violence on non-suicidal self-injury in young adults. J Youth Adolescence. 2010;39(5):474–483. doi: 10.1007/s10964-009-9471-3. [DOI] [PubMed] [Google Scholar]
- 68.Sansone RACJM. Self-inflicted bodily harm among victims of intimate-partner violence. Clin Psychol Psychot. 2007;14(5):352–357. [Google Scholar]
- 69.Kaslow NJ, Thompson MP, Meadows LA, Jacobs D, Chance S, Gibb B, et al. Factors that mediate and moderate the link between partner abuse and suicidal behavior in African American women. J Consult Clin Psych. 1998;66(3):533–540. doi: 10.1037//0022-006x.66.3.533. [DOI] [PubMed] [Google Scholar]
- 70.Pico-Alfonso MA, Garcia-Linares MI, Celda-Navarro N, Blasco-Ros C, Echeburua E, Martinez M. The impact of physical, psychological, and sexual intimate male partner violence on women’s mental health: Depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. J Womens Health. 2006;15(5):599–611. doi: 10.1089/jwh.2006.15.599. [DOI] [PubMed] [Google Scholar]
- 71.Baetens I, Claes L, Muehlenkamp J, Grietens H, Onghena P. Non-suicidal and suicidal self-injurious behavior among Flemish adolescents: A web-survey. Arch Suicide Res. 2011;15(1):56–67. doi: 10.1080/13811118.2011.540467. [DOI] [PubMed] [Google Scholar]
- 72.Whitlock J, Knox KL. The relationship between self-injurious behavior and suicide in a young adult population. Archives of Pediatrics & Adolescent Medicine. 2007;161(7):634–640. doi: 10.1001/archpedi.161.7.634. [DOI] [PubMed] [Google Scholar]