Abstract
AIM: To investigate the correlation of facet joint osteoarthritis (FJOA) at lumbar levels L4/L5 and L5/S1 and the Oswestry Disability Index (ODI).
METHODS: The study involved lumbar MRIs of 591 patients with a mean age of 47.3 years. The MRIs of the lumbar spine were performed on a 1.5 Tesla scanner (Magnetom® Avanto, Siemens AG, Erlangen, Germany) using a dedicated receive only spine coil. After initial blinding, each dataset was evaluated by 2 board certified radiologist with more than 5 years experience in musculoskeletal imaging. In total 2364 facet joints were graded. Degenerative changes of the facet joints were evaluated according to the 4-point scale as proposed by Weishaupt et al Functional status was assessed using the ODI. The index is scored from 0 to 100 and interpreted as follows: 0%-20%, minimal disability; 20%-40%, moderate disability; 40%-60%, severe disability; 60%-80%, crippled; 80%-100%, patients are bedbound. Spearman’s coefficient of rank correlation was used for statistical analysis, with significance set at P < 0.05.
RESULTS: In total 2364 facet joints at lumbar levels L4/5 and L5/S1 were analysed in 591 individuals. FJOA was present in 97% (L4/L5) and 98% (L5/S1). At level L4/5 (left/right) 17/15 (2.9%/2.5%) were described as grade 0, 146/147 (24.7%/24.9%) as grade 1, 290/302 (49.1%/51.1%) as grade 2 and 138/127 (23.4%/21.5%) as grade 3. At level L5/S1 (left/right) 10/11 (1.7%/1.9%) were described as grade 0, 136/136 (23.0%/23.0%) as grade 1, 318/325 (53.8%/55.0%) as grade 2 and 127/119 (21.5%/20.1%) as grade 3. Regarding the ODI scores, patients’ disability had a minimum of 0% and a maximum of 91.11% with an arithmetic mean of 32.77% ± 17.02%. The majority of patients (48.39%) had moderate functional disability (21%-40%). There was no significant correlation between FJOA and ODI on both sides of lumbar level L4/5 and on the left side of lumbar level L5/S1. A weak positive correlation was evaluated between ODI and FJOA on the right side of lumbar level L5/S1.
CONCLUSION: The missing correlation of FJOA and ODI confirms our clinical experience that imaging alone is an insufficient approach explaining low back pain. Clinical correlation is imperative for an adequate diagnostic advance in patients with low back pain.
Keywords: Spine, Facet joint osteoarthritis, Magnetic resonance imaging, Low back pain, Oswestry Disability Index
Core tip: Together with secondary disorders facet joint osteoarthritis (FJOA) sets a big burden on health care systems and economics of the western countries. Although FJOA is a common finding on lumbar magnetic resonance imaging (MRI), valid data with regard to correlation with clinical pain scores is missing. The presented study assesses the relationship between increasing grades of FJOA and the Oswestry Disability Score in a large cohort of lumbar MRIs. The results show a weak positive correlation between ODI and FJOA, proving the importance of an adequate clinical approach in patients with low back pain.
INTRODUCTION
Facet joint osteoarthritis (FJOA) is well known as a cause of low back and lower extremity pain[1-3]. Together with secondary disorders it sets a big burden on health care systems and economics of the western countries[4]. Due to its more precise demonstration of bony details computed tomography (CT) often is the preferred modality in the evaluation of FJOA. Weishaupt et al[5] evaluated the significance of magnetic resonance imaging (MRI) in comparison to CT using an established 4-point scale. They found that the interobserver agreement for grading FJOA was moderate for CT and MRI imaging whereas intraobserver agreement was good. Assumed differences of one grade are disregarded, interobserver agreement between both modalities becomes even excellent. In summary, the authors conclude that an additional CT scan is not required in the presence of an MRI examination. The Oswestry Disability Index (ODI) is the most commonly used measure to quantify disability for low back pain[6]. The patient questionnaire contains ten questions concerning the patient’s ability to cope with everyday life. The aim of the presented study was the assessment of a relationship between ODI scores and increasing grades of FJOA in a large cohort of lumbar MRIs.
MATERIALS AND METHODS
Study participants
Ethical committee approval was obtained for the study. The indications for MR imaging were suspected disc herniation and facet joint degeneration, respectively. The MRI scans of the lumbar spine were collected over a period of 12 mo in an outpatient setup. Each patient included in the study had a prior history of lower back pain without history of spinal surgery. Patients with proven disc herniation, spinal stenosis, scoliosis and evidence of vertebral fractures were also excluded from the study. Finally, the study involved lumbar MRIs of 591 patients (264 men and 327 women) with a mean age of 47.3 years (range 12-92 years).
Imaging technique
The MRIs of the lumbar spine were performed on a 1.5 Tesla scanner (Magnetom® Avanto, Siemens AG, Erlangen, Germany) using a dedicated receive only spine coil. The imaging protocol included sagittal T2-weighted fast spin-echo images (TR 2850, TE 102) with the following parameters: matrix 512, field of view 300 mm, slice thickness 4 mm, interslice gap 10%, number of excitations 2; axial T2-weighted fast spin-echo images (TR 3550, TE 90) with the following parameters: matrix 448; field of view 210 mm; slice thickness 4 mm; interslice gap 10%, number of excitations 2.
Image evaluation
After initial blinding each dataset was evaluated by two authors (Adel Maataoui and M Fawad Khan), both board certified radiologists with more than 5 years experience in musculoskeletal imaging, in consensus. Since degenerative changes occur most often and earlier in the two lowest motion segments[7], the readers were asked to grade the facet joints at lumbar levels L4/5 and L5/S1, respectively. In total 2364 facet joints were graded.
The facet joints were evaluated according to the 4-point (Grade 0 to Grade III) scale as proposed by Weishaupt et al[5]: A normal joint space (2-4 mm width) without evidence of osteophytes, hypertrophy of the articular process, subarticular bone erosions or subchondral cysts represented Grade I, while incremental existance of these parameters lead to a higher grade (Figure 1).
Figure 1.
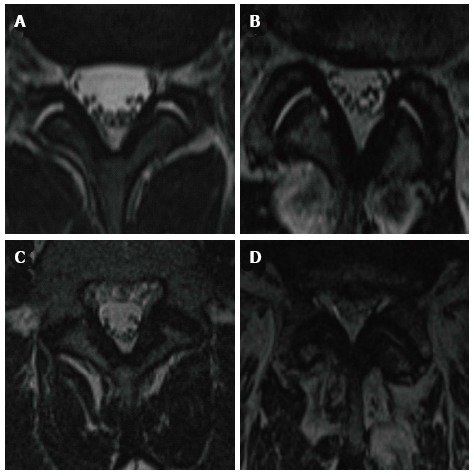
(A-D) Grading system of facet joint osteoarthritis in T2-weighted imaging according to Weishaupt et al[5]. Grade 0: Homogenous cartilage and normal (2-4 mm) joint space width; Grade I: Narrowing of the joint space and small osteophytes; Grade II: Narrowing of the joint space, moderate osteophytes and/or subchondral erosions; Grade III: Narrowing of the joint space, large osteophytes and subchondral erosion/cysts.
ODI
Functional status was assessed using the ODI. Before the examination the supervising physician filled the standardized questionnaire together with the patient. Among questions about the intensity of pain, ability of lifting, ability to care for oneself, ability to walk, ability to sit, ability to stand, social life, sleep quality, and ability to travel are prompted. The index is scored from 0 to 100 and interpreted as follows: 0%-20%, minimal disability; 20%-40 %, moderate disability; 40%-60%, severe disability; 60%-80%, crippled; 80%-100%, patients are bedbound. Due to ethical aspects the question about sexual function was excluded.
Statistical analysis
Statistical analysis was carried out using the BIAS software package (Epsilon publisher, Frankfurt a. M., Germany, http://www.bias-online.de). For statistical analysis Spearman’s coefficient of rank correlation and Student’s t-test were used. In all statistical analysis P < 0.05 was considered significant.
RESULTS
Grades of FJOA in the study population
In total 2364 facet joints at lumbar levels L4/5 and L5/S1 were analysed in 591 individuals. FJOA was present in 97% (L4/L5) and 98% (L5/S1). Table 1 summarizes the results.
Table 1.
Grades of facet joint arthritis for lumbar levels L4/5 and L5/S1 n (%)
| Lumbar level |
Grades |
|||
| 0 | I | II | III | |
| L4/5 left | 17 (2.9) | 146 (24.7) | 290 (49.1) | 138 (23.4) |
| L4/5 right | 15 (2.5) | 147 (24.9) | 302 (51.1) | 127 (21.5) |
| L5/S1 left | 10 (1.7) | 136 (23.0) | 318 (53.8) | 127 (21.5) |
| L5/S1 right | 11 (1.9) | 136 (23.0) | 325 (55.0) | 119 (20.1) |
At level L4/5 (left/right) 17/15 (2.9%/2.5%) were described as grade 0, 146/147 (24.7%/24.9%) as grade 1, 290/302 (49.1%/51.1%) as grade 2 and 138/127 (23.4%/21.5%) as grade 3.
At level L5/S1 (left/right) 10/11 (1.7%/1.9%) were described as grade 0, 136/136 (23.0%/23.0%) as grade 1, 318/325 (53.8%/55.0%) as grade 2 and 127/119 (21.5%/20.1%) as grade 3.
Function score as assessed by ODI
Regarding the ODI scores, patients’ disability had a minimum of 0% and a maximum of 91.11% with an arithmetic mean of 32.77% ± 17.02%. There was no statistical difference between the grade of disability in men (31.39% ± 16.72%) and women (33.89% ± 17.21%). The majority of patients (48.39%) had moderate functional disability (21%-40%).
The mean ODI scores for FJOA grade 0, 1, 2 and 3 on the left side of lumbar segment L4/5 were 29.02% ± 21.57%, 31.98% ± 17.16%, 33.24% ± 16.72% and 33.09% ± 17.00%, respectively. The mean ODI scores for FJOA grade 0, 1, 2 and 3 for the right side of lumbar segment L4/5 were 24.44% ± 21.20%, 32.00% ± 16.69%, 33.45% ± 16.93% and 33.04% ± 16.00%, respectively. Table 2 summarizes the results. For grade 0 to 2 of FJOA a discrete but continuous rise of ODI score was detectable. A statistically significant difference between the grade of disability (ODI score) and all grades of FJOA of both sides on lumbar level L5/S1 was not evident.
Table 2.
Oswestry Disability Index scores (%) in correlation to facet joint osteoarthritis (grade 0-III)
| Lumbar level |
Grade FJOA |
|||
| 0 | I | II | III | |
| L4/5 left | 29.02 ± 21.57 | 31.98 ± 17.16 | 33.24 ± 16.72 | 33.09 ± 17.00 |
| L4/5 right | 24.44 ± 21.20 | 32.00 ± 16.69 | 33.45 ± 16.93 | 33.04 ± 16.00 |
| L5/S1 left | 31.56 ± 17.05 | 31.85 ± 18.64 | 32.25 ± 15.75 | 35.17 ± 18.22 |
| L5/S1 right | 25.86 ± 12.81 | 31.26 ± 17.44 | 32.53 ± 16.38 | 35.80 ± 18.27 |
FJOA: Facet joint arthritis.
The mean ODI scores for FJOA grade 0, 1, 2 and 3 on the left side of lumbar segment L5/S1 were 31.56% ± 17.05%, 31.85% ± 18.64%, 32.25% ± 15.75% and 35.17% ± 18.22%, respectively. The mean ODI scores for FJOA grade 0, 1, 2 and 3 for the right side of lumbar segment L5/S1 were 25.86% ± 12.81%, 31.26% ± 17.44%, 32.53% ± 16.38% and 35.80% ± 18.27%, respectively. Table 2 summarizes the results. With increasing grade of FJOA a discrete but continuous rise of ODI score was detectable. A statistically significant difference between the grade of disability (ODI score) and the grade of FJOA of both sides on lumbar level L5/S1 was not evident.
Correlation of ODI and FJOA
There was no significant correlation between FJOA and ODI on both sides of lumbar level L4/5 and on the left side of lumbar level L5/S1: ODI and FJOA left: rho < 0.035, P < 0.371; ODI and FJOA right: rho < 0.052, P < 0.186; ODI and FJOA left: rho < 0.051, P < 0.196.
A weak positive correlation was evaluated between ODI and FJOA on the right side of lumbar level L5/S1: Rho < 0.084, P < 0.035.
DISCUSSION
Low back pain is a widely spread musculoskeletal disorder in all ages worldwide. The annual prevalence between 25% and 60% makes it a frequent cause of limitation of activity in people younger than 50 years. Furthermore, up to 85% of all people have back pain at some time in life[8]. Despite modern imaging modalities, such as magnetic resonance imaging, for a large proportion of patients with low back pain, it remains difficult to provide a specific diagnosis[9]. The fact that nearly all-lumbar structures are possible sources of low back pain, may serve as a possible explanation[10].
FJOA is a common imaging finding and has been suggested as a major cause of low back and lower extremity pain[1,2]. Since the facet joints are the only synovial joints in the spine with hyaline cartilage overlying subchondral bone, a synovial membrane and a joint capsule, they develop degenerative changes that are equivalent to other peripheral joints. Different studies reported contradicting results about the prevalence of FJOA at lumbar levels. Kalichman et al[11] reported that FJOA is more prevalent at L4/5 (45.1%) followed by L5/S1 (38.2%) and L3/4 (30.6%) whereas Abbas et al[12] describe a different descending order: L5/S1 (55%), L4/5 (27%) and L3/4 (16%). Additionally, Abbas et al[12] describe that FJOA is an age dependant phenomenon, which increases cephalocaudally, whereas they found no correlation of FJOA with sex or the Body mass index[12]. For the assessment of FJOA we applied the 4-point scale as proposed by Weishaupt et al[5]. Assuming that grade I changes already represent mild degenerative changes, nearly all patients in our study group showed degenerative alterations of the facet joints. Overall in our study population 97% (L4/5) and 98% (L5/S1) of the examined articulations revealed degenerative changes.
In their cross-sectional study Marchiori et al[13] correlated radiographic findings of spinal degeneration of the cervical spine with neck pain and disability in 700 patients[13]. They found that women report higher disability with increasing levels of degeneration while no relation was evident for men. The group of Ashraf et al[14] presents similar results. In 150 patients they classified degenerative changes of the lumbar spine on lateral radiographs according to the criteria of Kellgren and Lawrence[14]. Additionally, functional disability was measured using the ODI. They found no significant correlation between the morphological severity of osteoarthritis and ODI scores. A major limitation of the mentioned studies is the fact that degenerative changes of the cervical and lumbar spine were graded on plain film radiographs, which are because of superposition of limited diagnostic value. Additionally, severity of degeneration of intervertebral discs as well as of facet joints was taken into account for scoring. As already mentioned nearly all-lumbar structures are possible sources of low back pain, so that an isolated contemplation of anatomic structures (facet joint, intervertebral disc) and their degenerative changes with regard to clinical importance is necessary. Therefore in the presented study we correlated degenerative changes of the facet joints at lumbar levels L4/5 and L5/S1 with the ODI. The results of this study demonstrate that only for the right-sided facet joints of lumbar level L5/S1 there was a weak correlation between signs of degeneration and clinical disability scores as evaluated by ODI. Taking into account that a huge majority of patients of all ages show degenerative changes of facet joints in the lower motion segments of the lumbar spine, these results should be considered in the future evaluation of lumbar MRIs. In the presence of other degenerative changes like intervertebral disc degeneration, osteochondrosis or Morbus Baastrup the finding of FJOA shouldn’t be considered evidentiary as the cause of LBP. In fact, the presented results seem to prove that chronic LBP is a multifactorial disorder, which cannot be explained with a constricted view on one lumbar compartment.
MRI reliably detects age-dependent FJOA of the lumbar spine. Our data revealed no correlation between ODI and FJOA on both sides of lumbar level L4/5 and on the left side of lumbar level L5/S1, while only a weak positive correlation on the right side of lumbar level L5/S1 was evaluated. These findings support the demand, that clinical correlation of apparently explicit imaging findings is not an adjunct only but imperative for an adequate clinical approach in patients suffering from low back pain.
COMMENTS
Background
Facet joint osteoarthritis is well known as a cause of low back and lower extremity pain. Together with secondary disorders it sets a big burden on health care systems and economics of the western countries.
Research frontiers
Despite modern imaging modalities, such as magnetic resonance imaging, it remains difficult to provide a specific diagnosis for a large proportion of patients with low back pain. The fact that nearly all lumbar structures are possible sources of low back pain, may serve as a possible explanation.
Innovations and breakthroughs
The results of the presented study demonstrate that there exists only a weak correlation between signs of degeneration and clinical disability scores as evaluated by the Oswestry Disability Index. Taking into account that a huge majority of patients of all ages show degenerative changes of facet joints in the lower motion segments of the lumbar spine, these results should be considered in the future evaluation of lumbar MRIs.
Applications
With above mentioned innovations in mind, the presence of other degenerative changes like intervertebral disc degeneration, osteochondrosis or Morbus Baastrup the finding of facet joint osteoarthritis shouldn’t be considered evidentiary as the cause of low back pain.
Terminology
Since the facet joints are the only synovial joints in the spine with hyaline cartilage overlying subchondral bone, a synovial membrane and a joint capsule, they develop degenerative changes that are equivalent to other peripheral joints. The Oswestry Disability Index is the most commonly used measure to quantify disability for low back pain. The patient questionnaire contains ten questions concerning the patient’s ability to cope with everyday life.
Peer review
The manuscript is well written.
Footnotes
P- Reviewer: Razek AAKA, Teli MGA S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
References
- 1.Gellhorn AC, Katz JN, Suri P. Osteoarthritis of the spine: the facet joints. Nat Rev Rheumatol. 2013;9:216–224. doi: 10.1038/nrrheum.2012.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goode AP, Carey TS, Jordan JM. Low back pain and lumbar spine osteoarthritis: how are they related? Curr Rheumatol Rep. 2013;15:305. doi: 10.1007/s11926-012-0305-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suri P, Dharamsi AS, Gaviola G, Isaac Z. Are facet joint bone marrow lesions and other facet joint features associated with low back pain? A pilot study. PM R. 2013;5:194–200. doi: 10.1016/j.pmrj.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Collaborators USBoD. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weishaupt D, Zanetti M, Boos N, Hodler J. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol. 1999;28:215–219. doi: 10.1007/s002560050503. [DOI] [PubMed] [Google Scholar]
- 6.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 7.Laplante BL, DePalma MJ. Spine osteoarthritis. PM R. 2012;4:S28–S36. doi: 10.1016/j.pmrj.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Buchbinder R, Blyth FM, March LM, Brooks P, Woolf AD, Hoy DG. Placing the global burden of low back pain in context. Best Pract Res Clin Rheumatol. 2013;27:575–589. doi: 10.1016/j.berh.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Suri P, Boyko EJ, Goldberg J, Forsberg CW, Jarvik JG. Longitudinal associations between incident lumbar spine MRI findings and chronic low back pain or radicular symptoms: retrospective analysis of data from the longitudinal assessment of imaging and disability of the back (LAIDBACK) BMC Musculoskelet Disord. 2014;15:152. doi: 10.1186/1471-2474-15-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chou D, Samartzis D, Bellabarba C, Patel A, Luk KD, Kisser JM, Skelly AC. Degenerative magnetic resonance imaging changes in patients with chronic low back pain: a systematic review. Spine (Phila Pa 1976) 2011;36:S43–S53. doi: 10.1097/BRS.0b013e31822ef700. [DOI] [PubMed] [Google Scholar]
- 11.Kalichman L, Li L, Kim DH, Guermazi A, Berkin V, O’Donnell CJ, Hoffmann U, Cole R, Hunter DJ. Facet joint osteoarthritis and low back pain in the community-based population. Spine (Phila Pa 1976) 2008;33:2560–2565. doi: 10.1097/BRS.0b013e318184ef95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abbas J, Hamoud K, Peleg S, May H, Masharawi Y, Cohen H, Peled N, Hershkovitz I. Facet joints arthrosis in normal and stenotic lumbar spines. Spine (Phila Pa 1976) 2011;36:E1541–E1546. doi: 10.1097/BRS.0b013e318210c889. [DOI] [PubMed] [Google Scholar]
- 13.Marchiori DM, Henderson CN. A cross-sectional study correlating cervical radiographic degenerative findings to pain and disability. Spine (Phila Pa 1976) 1996;21:2747–2751. doi: 10.1097/00007632-199612010-00007. [DOI] [PubMed] [Google Scholar]
- 14.Ashraf A, Farahangiz S, Pakniat Jahromi B, Setayeshpour N, Naseri M. Correlation between Degree of Radiologic Signs of Osteoarthritis and Functional Status in Patients with Chronic Mechanical Low Back Pain. Malays J Med Sci. 2014;21:28–33. [PMC free article] [PubMed] [Google Scholar]


