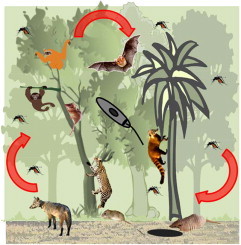
Graphical Abstract
Keywords: Leishmania spp, Reservoir, Wild mammals, Leishmaniasis
Highlights
-
•
Leishmania parasites are maintained by multiple hosts included in seven mammal orders.
-
•
Reservoir hosts are the assemblage of species responsible for Leishmania maintenance.
-
•
Mammal host–Leishmania interaction determines host competence to infect vectors.
-
•
Associate ecological and parasitological data are crucial to understand the wild cycle.
-
•
Prevention of human cases is dependent on a thorough knowledge of the wild cycle.
Abstract
The definition of a reservoir has changed significantly in the last century, making it necessary to study zoonosis from a broader perspective. One important example is that of Leishmania, zoonotic multi-host parasites maintained by several mammal species in nature. The magnitude of the health problem represented by leishmaniasis combined with the complexity of its epidemiology make it necessary to clarify all of the links in transmission net, including non-human mammalian hosts, to develop effective control strategies. Although some studies have described dozens of species infected with these parasites, only a minority have related their findings to the ecological scenario to indicate a possible role of that host in parasite maintenance and transmission. Currently, it is accepted that a reservoir may be one or a complex of species responsible for maintaining the parasite in nature. A reservoir system should be considered unique on a given spatiotemporal scale. In fact, the transmission of Leishmania species in the wild still represents an complex enzootic “puzzle”, as several links have not been identified. This review presents the mammalian species known to be infected with Leishmania spp. in the Americas, highlighting those that are able to maintain and act as a source of the parasite in nature (and are thus considered potential reservoirs). These host/reservoirs are presented separately in each of seven mammal orders – Marsupialia, Cingulata, Pilosa, Rodentia, Primata, Carnivora, and Chiroptera – responsible for maintaining Leishmania species in the wild.
1. Introduction
Upon their arrival in the Americas, humans began be exposed to parasite species that circulate in the extant fauna (Araújo et al., 2013). Even now, though to a lesser extent, we are still exposed to the wild environment, its wildlife and their parasites. Habitat fragmentation, global warming, non-sustainable exploratory activities, expansion of agriculture and eco-tourism are some factors that contribute to intensifying this contact (Aguirre and Tabor, 2008; Alexander et al., 2012; Jones et al., 2008). Human infection by parasites that circulate in the wild is especially probable for multi-host parasites, i.e., those capable of infecting a wide range of mammalian and vector host species (Woolhouse et al., 2001). This is the case for some Leishmania species, including L. infantum (=syn. L. chagasi), L. braziliensis, L. amazonensis and L. mexicana, the most important etiological agents of human leishmaniasis in the Americas (Alvar et al., 2012). These trypanosomatids are characterized by high genetic heterogeneity and biological eclecticism, as evidenced in varied orders of mammals that they are able to infect. As a result, these protozoa species have complex transmission cycles with region-specific epidemiological characteristics (Ashford, 1996; Rotureau, 2006).
Cases of human leishmaniasis, which may present distinct infection patterns, are caused by more than 20 species of heteroxenic flagellates of the genus Leishmania. These parasites circulate among mammals belonging to seven orders and, in the Americas, are transmitted by sandflies of the genus Lutzomyia (Diptera: Psychodidae) (Alvar et al., 2012). The classification into visceral and cutaneous forms, observed in human disease, cannot be applied to the infection in other mammals. Dogs infected with L. infantum present viscero-dermic disease, where parasite isolation is common even from intact skin (Madeira et al., 2009). Moreover, Leishmania species associated with human cutaneous infection have been observed in rodent viscera since the 1950s (Nery Guimarães, 1951; Roque et al., 2010). We thus challenge the classical concept of tissue tropism of Leishmania species. This term comes from the Greek “tropos”, a movement in a particular direction in response to an external stimulus. In Leishmania spp., however, the cells of the phagocytic mononuclear system represent the preferential niche. In ecological terms, the tissues where Leishmania species are found represent more favorable niches for permanent establishment (which may vary among mammalian hosts); preferential infection is not the result of a tropism for a given tissue.
Although the concepts and methods employed for the investigation of parasite reservoirs have changed significantly over time (Ashford, 1997; Haydon et al., 2002; Lainson et al., 1981a), most of the descriptions of Leishmania spp. reservoirs are still based on findings of natural infection, which do not provide information on the epidemiological importance of that host to parasite maintenance in the area. Considering the new definition of reservoirs, understanding the role of each mammalian host species in Leishmania transmission from secondary data demands a critical analysis of field and laboratory studies. Although knowledge of leishmaniasis has improved in recent decades (mainly concerning the cellular and molecular biology of the parasite, epidemiology and diagnosis of human infection), we still lack data on the transmission between their mammalian hosts and vectors. As a consequence, this disease presents an ongoing public-health problem and continues to expand its range (Alvar et al., 2012).
2. What defines a reservoir host?
As in any other host–parasite system, patterns of Leishmania infection in any mammalian host species are determined by host factors (species, concomitant infections/health, sex, age, behavioral patterns), parasite traits (generation time, dispersion strategies, molecular and biochemical characteristics of its sub-populations), exposure (inoculum size) and local environmental conditions (influenced, e.g., by stress and availability of natural resources) where the host–parasite encounter takes place (Chaves et al., 2007; De Tommasi et al., 2013). The influence of these factors shows that a given mammalian host species may not fill the same role in the transmission cycle in different localities and time periods (Desjeux, 2004; Mills and Childs, 1998). Furthermore, the competence to infect vectors (infectivity or transmissibility competence) is not homogeneously distributed in host populations, and transmission is assumed to be associated with only a minority of infected mammals in an ecological pattern known as the 20/80 rule (Miller and Huppert, 2013; Woolhouse et al., 1997). Parasite transmission nets are dynamic, thus it is likely that parasites are periodically extinguished in a particular host population and are re-introduced some time later (Mills and Childs, 1998).
Assuming that an infected mammal is a host, its importance in the transmission cycle will depend both on the dispersion strategy of the parasite and the peculiarities of this host–parasite interaction. The assemblage of these variables will determine the accessibility of the parasite to the external environment or to the intermediate host for transmission and thus for maintenance. These are the factors that determine the transmissibility competence of that host species; defining thus, its role as a reservoir host. Mainly based on studies by Ashford (1997) and Haydon et al. (2002), we consider a “reservoir” a system that includes one or more species of mammals that are responsible for maintaining the parasite in nature and should be considered as unique within a certain spatiotemporal scale (Jansen and Roque, 2010). Within this “reservoir system”, each host species plays a distinct role in transmission in a certain time and space. Transmissibility competence is thus a trait that alters over the course of infection in given individual host, such that one species or individual may assume different roles in the epidemiology of a parasite during its lifespan. Here, we consider “maintenance hosts” to be those mammals that can be infected and maintain the infection and “amplifier hosts” to be those mammals that, in addition to maintaining the infection, display a characteristic that favors transmission (more parasites in the blood and skin for longer periods). These conditions are interchangeable, and maintenance hosts may be converted into amplifier hosts according to the host's health conditions for example, immune suppression and concomitant parasitic infections (Botero et al., 2013). A schema of the reservoir system should include the ecology/biology of that host (life area and explored habitats), the local population structure and the relative abundance and interaction of the host species with other mammals (Miller and Huppert, 2013; Noireau et al., 2009).
Finally, a controversial point in the study of reservoirs is the assumption that a reservoir host must not show symptoms, as asymptomatic infection is usually associated with ancient host–parasite relationships (WHO, 1990). It is currently assumed, however, that not all ancient host–parasite interactions necessarily evolve into harmonic interactions because they may instead favor the transmissibility of the parasite. Transmission is crucial for parasite survival and is dependent on their reproductive strategy (Giorgio, 1995; Woolhouse et al., 2001). Indeed, virulence and pathogenicity may in some cases be considered fitness traits because both may improve parasite transmission and may, therefore, be positively selected.
3. Understanding the pattern of Leishmania spp. infection of mammalian hosts
Although they are enzootic parasites, there are few studies on the roles of different mammalian host species in the transmission of Leishmania spp. and “hosts” and “reservoirs” are usually treated as synonymous terms (WHO, 1990; Ashford, 1996). Studies considering long-lasting infection with these parasites in wild hosts are scarce (Raymond et al., 2003; Travi et al., 2002). Understanding the role played by different mammalian species in the transmission of Leishmania spp. in nature requires an epidemiological investigation that includes an infection follow-up and a representative sampling of the potential host species and mammalian populations in the area. Equally important is the adoption of a broad methodological approach that should include the diagnosis of infection by direct and indirect parasitological tests to evaluate transmissibility competence. Additionally, whenever possible, experimental studies on potential wild reservoirs must be performed to assist the interpretation of the data obtained in field investigations (Roque et al., 2010).
Direct examination and blood-culture techniques are less effective for the detection of Leishmania spp. in wild mammals. Even in dogs infected by L. infantum, its sensitivity varies among different studies and mostly depends on parasite load, examined tissue and technical experience (Ikeda-Garcia and Feitosa, 2006). On the other hand, specificity is always 100%. The gold-standard methods are the cultures of punctures or fragments of hematopoietic tissues, but the positive result does not necessarily reflect the competence of that host to transmit the parasite. This competence is defined by the accessibility of parasites to vectors, which is correlated with the origin of the cultured material. Positive skin or blood cultures and xenodiagnosis suggest transmissibility. Direct visualization of parasites in skin fragments has lower sensitivity, but in combination with the confirmation of the etiologic agent, this technique also confirms viability and thus therefore, its transmissibility. Positive cultures always demonstrate the presence of viable parasites, but positive obtained from internal organs (liver, spleen, bone marrow, and lymph nodes) do not necessarily indicate infectivity to the vector.
Serological tests, among which the most used are the immunofluorescence (IFAT) and immunoenzymatic (ELISA) assays, demonstrate infection. Sensitivity and specificity of these tests range from 90% to 100% and 80% to 100%, respectively for IFAT (Mettler et al., 2005) and from 80% to 99.5% and 81% to 100%, respectively for ELISA (Mancianti et al., 1995; Marcondes et al., 2011). A host that is positive in serological but negative in parasitological tests has been exposed to Leishmania infection (expected to still be infected), but are not necessarily important for the maintenance of the parasite in nature, i.e., are not necessarily reservoirs of the parasite. Molecular diagnosis by polymerase chain reaction (PCR) can be considered a parasitological assay, because it detects constitutive parts of the parasites (fragments of DNA). This technique may reach sensitivity and specificity values near 100%, but these values may vary depending on the examined tissue (Ashford et al., 1995; Lachaud et al., 2002; Troncarelli et al., 2009). Despite certainly demonstrating the presence of the parasite, it does not allow us to indicate the integrity of that parasite (Silva et al., 2005). Concerning the parasite transmissibility, only recently it was demonstrated that the parasite load, especially in the skin, can be related to the infectiousness during natural infection (Courtenay et al., 2014). Although PCR is considered extremely sensitive, its use as the gold standard for diagnosis or therapeutic cure of human leishmaniasis remains a matter of debate (Mendonca et al., 2004; Salam et al., 2010). In wild and synanthropic animals, diagnosis by PCR is still a challenge, lacking standardization of techniques and species–specific molecular targets.
4. Leishmania hosts and putative reservoirs
Studies of host–parasite interaction among wild mammals and Leishmania species are rare because of the complexity of performing long-term field-work and the difficulties of maintaining captivity colonies of wild species for experimental infection. Moreover, an essential aspect of this type of study is the accurate taxonomic identification of the mammalian hosts. Identification is not trivial for taxa (e.g. rodents and bats) that comprise a great diversity of species, including several whose taxonomic position is still debatable and can be identified only by karyotyping and/or molecular analysis. Our aim in this review was to re-interpret the available data on Leishmania reservoirs using an ecological approach and to consider the transmissibility potential from that species. We also added data on characterization of parasite in wild hosts from the Leishmania sp. collection of the Oswaldo Cruz Institute (CLIOC/Fiocruz: clioc.fiocruz.br). Our main difficulties in this review involved: (i) access to the full text of some articles, especially the older articles, published in languages other than English and in journals that are not broadly distributed; and (ii) in some cases, identification of Leishmania species, as the numerous taxonomic revisions have repeatedly changed the nomenclature of some species.
In this context, we discuss some of the wild and synanthropic species known to be infected with Leishmania spp., distinguishing between “parasite hosts” and “potential reservoirs”, with the latter designation used only when the authors demonstrated the retention of infection or the potential to transmit the parasite to vectors (positive xenodiagnosis or cultures from skin or blood). As already noted, Leishmania reservoirs show regional and temporal variation, and only a local study including ecological and parasitological analysis can determine whether these “potential reservoirs” may serve as reservoir in a given environment.
4.1. Order Didelphimorphia
The autochthonous American order Didelphimorphia is the only marsupial order recognized in the Americas. Mammals from this order have a wide distribution, mainly due to their remarkable adaptability to different ecological niches, particularly to environments with a high degree of human activity. The genus Didelphis is the most widely dispersed on the continent, occurring from southeastern Canada to southern Argentina (Austad, 1988). Didelphis spp. are nomadic, solitary (mainly males), and excellent climbers that are mainly found in holes in trees and foliage. These animals can colonize ceilings of houses and other shelters in domestic and peri-domestic areas, where they feed on human food garbage (Austad, 1988; Olifiers et al., 2005). Most likely due to its synanthropic character, this species is one of most studied regarding infection by Leishmania spp., although only a few of these studies included follow up on the natural or experimental infection (Travi et al., 1994, 1998b).
Didelphis marsupialis, a species distributed from Mexico to the Amazon region has been found to be infected with at least four Leishmania species (Arias et al., 1981; Corredor et al., 1989; Grimaldi et al., 1991) (Table 1). Its importance as a potential reservoir for L. infantum was demonstrated in a rural community from Colombia, where these animals were abundant, and displayed a high prevalence of positive cultures and high parasite loads (as observed in slide imprints), in the spleen (Corredor et al., 1989). Later studies also confirmed their importance elsewhere in Colombia and Venezuela (Quinnell and Courtenay, 2009; Travi et al., 1998a). Additionally, its importance as a reservoir was confirmed by the experimental infection by L. infantum of five specimens, which resulted in clinical signs suggestive of visceral leishmaniasis in one young female that presented amastigote parasites in the spleen, liver and lymph nodes. Parasites were re-isolated from all of these specimens, and three were also infective for Lu. longipalpis (Travi et al., 1998b).
Table 1.
Mammal host species described infected by different Leishmania species in the Americas.
| Order | Host species | Leishmania species | Infection pattern | Country | References |
|---|---|---|---|---|---|
| Didelphimorphia | Didelphis marsupialis | L. infantum | Potential reservoir | CO, VE | Corredor et al., 1989; apud Quinnell and Courtenay, 2009 |
| L. amazonensis | Parasite host | BR | Grimaldi et al., 1991 | ||
| L. guyanensis | Potential reservoir | BR; FG | Arias et al., 1981; Dedet et al., 1989 | ||
| L. forattinii | Parasite host | BR | IOCL 0067 | ||
| D. albiventris | L. infantum | Potential reservoir | BR | Sherlock et al., 1984; Sherlock, 1996 | |
| L. braziliensis | Parasite host | BR | Quaresma et al., 2011 | ||
| L. peruviana | Potential reservoir | PE | Llanos-Cuentas et al., 1999 | ||
| D. aurita | L. infantum | Parasite host | BR | Carreira et al., 2012 | |
| Philander opossum | L. amazonensis | Parasite host | BR | Lainson et al., 1981a | |
| Marmosa cinerea | L. amazonensis | Parasite host | BR | Arias et al., 1981 | |
| Marmosa sp | L. (Viannia) sp. | Parasite host | BR | Brandão-Filho et al., 2003 | |
| Micoreus paraguayanus | L. amazoensis | Parasite host | BR | Quintal et al., 2011 | |
| L. braziliensis | Parasite host | BR | Quintal et al., 2011 | ||
| Gracilinanus agilis | L. braziliensis | Parasite host | BR | Quaresma et al., 2011 | |
| Marmosops incanus | L. guyanensis | Parasite host | BR | Quaresma et al., 2011 | |
| Metachirus nudicaudatus | L. amazonensis | Parasite host | BR | Lainson et al., 1981a | |
| Monodelphis domestica | L. (Viannia) sp. | Parasite host | BR | Lima et al., 2013 | |
| Pilosa | Choloepus didactylus | L. guyanensis | Potential reservoir | FG; BR | Gentile et al., 1981; Lainson et al., 1981a |
| L. shawi | Parasite host | BR | Lainson et al., 1989 | ||
| C. hoffmanni | L. colombiensis | Parasite host | PN | Kreutzer et al., 1991 | |
| L. equatoriensis | Parasite host | EC | Grimaldi et al., 1992 | ||
| L. panamensis | Parasite host | PN | apud Ashford, 2000 | ||
| Bradypus tridactylus | L. shawi | Parasite host | BR | Lainson et al., 1989 | |
| Tamandua tetradactyla | L. guyanensis | Parasite host | BR | Lainson et al., 1981a | |
| L. amazonensis | Parasite host | EC | Mimori et al., 1989 | ||
| L. infantum | Parasite host | BR | Araújo et al., 2013 | ||
| Cingulata | Dasypus novemcinctus | L. naiffi | Potential reservoir | BR | Lainson and Shaw, 1989; Naiff et al., 1991 |
| L. guyanensis | Parasite host | BR | Lainson et al., 1979 | ||
| Rodentia | Proechimys species | L. amazonensis | Potential reservoir | BR; FG | Arias et al., 1981; Dedet et al., 1989 |
| L. guyanensis | Parasite host | BR; FG | Dedet et al., 1989; Lainson et al., 1981b | ||
| P. canicollis | L. infantum | Parasite host | CO | Travi et al., 1998a | |
| P. semispinosus | L. panamensis | Potential reservoir | CO | Travi et al., 2002 | |
| L. infantum | Parasite host | CO | Travi et al., 2002 | ||
| Thrichomys apereoides | L. braziliensis | Parasite host | BR | Quaresma et al., 2011 | |
| L. guyanensis | Parasite host | BR | Quaresma et al., 2011 | ||
| L. infantum | Parasite host | BR | Oliveira et al., 2005; Quaresma et al., 2011 | ||
| L. amazonensis | Parasite host | BR | Oliveira et al., 2005 | ||
| T. laurentius | L. infantum | Potential reservoir | BR | Roque et al., 2010 | |
| L. braziliensis | Potential reservoir | BR | Roque et al., 2010 | ||
| L. naiffi | Parasite host | BR | Cássia-Pires, unpublished data | ||
| L. shawi | Parasite host | BR | Cássia-Pires, unpublished data | ||
| T. inermis | L. shawi | Parasite host | BR | Cássia-Pires, unpublished data | |
| T. pachyurus | L. naiffi | Parasite host | BR | Cássia-Pires, unpublished data | |
| Nectomys squamipes | L. infantum | Parasite host | BR | Dantas-Torres and Brandao-Filho, 2006 | |
| L. braziliensis | Parasite host | BR | Peterson et al., 1988 | ||
| Rattus rattus | L. infantum | Parasite host | BR; VE | apud Quinnell and Courtenay, 2009 | |
| L. braziliensis | Potential reservoir | BR; VE | Vasconcelos et al., 1994; De Lima et al., 2002 | ||
| L. mexicana | Parasite host | VE | De Lima et al., 2002 | ||
| Clyomys laticeps | L. infantum | Parasite host | BR | Cássia-Pires, unpublished data | |
| Dasyprocta azarae | L. infantum | Parasite host | BR | Cássia-Pires, unpublished data | |
| Dasyprocta sp. | L. amazonensis | Parasite host | BR | Lainson et al., 1981b | |
| Rhipidomys mastacalis | L. infantum | Parasite host | BR | Quaresma et al., 2011 | |
| Coendu sp. | L. lainsoni | Parasite host | BR | IOCL 1058 | |
| L. hertigi/L. deanei | Parasite host | PN; BR | Herrer, 1971; Silva et al., 2013 | ||
| Coendu prehensilis | L. infantum | Parasite host | BO | Le Pont et al., 1989 | |
| Akodon arviculoides | L. braziliensis | Parasite host | BR | Forattini et al., 1972; Rocha et al., 1988 | |
| Akodon sp. | L. amazonensis | Parasite host | BO | Telleria et al., 1999 | |
| Necromys lasiurus | L. braziliensis | Potential reservoir | BR | Brandão-Filho et al., 2003; de Freitas et al., 2012 | |
| Sigmodon hispidus | L. braziliensis | Potential reservoir | VE | De Lima et al., 2002 | |
| L. mexicana | Potential reservoir | MX, VE | Van Wynsberghe et al., 2000; De Lima et al., 2002 | ||
| Holochilus scieurus | L. infantum | Parasite host | BR | Lima et al., 2013 | |
| H. scieurus | L. (Viannia) sp. | Parasite host | BR | Brandão-Filho et al., 2003 | |
| Cerradomys subflavus | L. (Viannia) sp. | Parasite host | BR | Lima et al., 2013 | |
| Mus musculus | L. braziliensis | Parasite host | BR | de Freitas et al., 2012 | |
| Oryzomys species | L. amazonensis | Parasite host | BO | Kerr et al., 2006 | |
| O. melanotis | L. amazonensis | Potential reservoir | MX | Van Wynsberghe et al., 2000 | |
| O. nigripes | L. braziliensis | Parasite host | BR | Forattini et al., 1972 | |
| Oligoryzomys sp. | L. amazonensis | Parasite host | BO | Telleria et al., 1999 | |
| Sciurus vulgaris | L. amazonensis | Parasite host | EC | Mimori et al., 1989 | |
| S. granatensis | L. equatorensis | Parasite host | EC | Grimaldi et al., 1992 | |
| Neotoma species | L. mexicana | Potential reservoir | US | Kerr et al., 1995; Raymond et al., 2003 | |
| Ototylomys phyllotis | L. mexicana | Potential reservoir | BE; MX | Ashford, 1996; Van Wynsberghe et al., 2000 | |
| Heteromys species | L. mexicana | Parasite host | BE; MX | Ashford, 1996; Van Wynsberghe et al., 2009 | |
| H. dermarestianus | L. panamensis | Parasite host | CR | Zeledon et al., 1977 | |
| Peromyscus yucatanicus | L. mexicana | Potential reservoir | MX | Van Wynsberghe et al., 2000 | |
| Nyctomys sumichrasti | L. mexicana | Parasite host | HN | Lainson and Strangways-Dixon, 1964 | |
| Reithrodontomys gracilis | L. mexicana | Parasite host | HN | Disney, 1968 | |
| Agouti paca | L. lainsoni | Potential reservoir | BR | Silveira et al., 1991 | |
| Phyllotis andinum | L. peruviana | Parasite host | PE | Llanos-Cuentas et al., 1999 | |
| Cavia porcellus | L. enriettii | Parasite host | BR | Machado et al., 1994 | |
| Carnivora | Cerdocyon thous | L. infantum | Potential reservoir | BR | Deane and Deane, 1955; Courtenay et al., 1996 |
| L. amazonesis | Parasite host | BR | apud Rotureau, 2006 | ||
| Speothos venaticus | L. infantum | Potential reservoir | BR | Figueiredo et al., 2008; Lima et al., 2009 | |
| Pseudalopex vetulus | L. infantum | Parasite host | BR | Curi et al., 2006; Luppi et al., 2008 | |
| Chrysocyon brachyurus | L. infantum | Parasite host | BR | Curi et al., 2006; Luppi et al., 2008 | |
| Puma concolor | L. infantum | Parasite host | BR | Dahroug et al., 2010 | |
| Panthera onca | L. infantum | Parasite host | BR | Dahroug et al., 2010 | |
| Nasua nasua | L. shawi | Parasite host | BR | Lainson et al., 1989 | |
| Potos flavus | L. guyanensis | Parasite host | FG | Pajot et al., 1982 | |
| L. amazonensis | Parasite host | EC | Kreutzer et al., 1991 | ||
| Conepatus chinga | L. amazonensis | Parasite host | BO | Telleria et al., 1999 | |
| L. braziliensis | Parasite host | BO | Buitrago et al., 2011 | ||
| Primata | Cebus apella | L. shawi | Potential reservoir | BR | Lainson et al., 1989 |
| Cebus xanthosternos | L. infantum | Parasite host | BR | Malta et al., 2010 | |
| Chiropotes satanas | L. shawi | Potential reservoir | BR | Lainson et al., 1989 | |
| Saguinus geoffroyi | L. amazonensis | Potential reservoir | PN | Herrer et al., 1973 | |
| Aotus trivirgatus | L. braziliensis | Potential reservoir | PN | Herrer and Christensen, 1976 | |
| Aotus azarai | L. (Viannia) sp. | Parasite host | AR | Acardi et al., 2013 | |
| Aotus nigriceps | L. infantum | Parasite host | BR | Malta et al., 2010 | |
| Callicebus nigrifrons | L. infantum | Parasite host | BR | Malta et al., 2010 | |
| Alouatta guariba | L. infantum | Parasite host | BR | Malta et al., 2010 | |
| Leonthopitecus crysomelas | L. infantum | Parasite host | BR | Malta et al., 2010 | |
| Pithecia irrorata | L. infantum | Parasite host | BR | Malta et al., 2010 | |
| Saguinus imperator | L. infantum | Parasite host | BR | Malta et al., 2010 | |
| Ateles paniscus | L. amazonensis | Parasite host | BR | Lima et al., 2012a | |
| Chiroptera | Carollia perspicillata | L. infantum | Potential reservoir | VE | De Lima et al., 2008 |
| Molossus molossus | L. infantum | Parasite host | BR | Savani et al., 2010 | |
| L. amazonensis | Parasite host | BR | Savani et al., 2010 | ||
| L. (Viannia) sp. | Parasite host | BR | Shapiro et al., 2013 | ||
| M. rufus | L. amazonensis | Parasite host | BR | Savani et al., 2010 | |
| Glossophaga soricina | L. infantum | Parasite host | BR | Savani et al., 2010 | |
| L. amazonensis | Parasite host | BR | Savani et al., 2010 | ||
| L. (Viannia) sp. | Parasite host | BR | Shapiro et al., 2013 | ||
| Nyctinomops laticaudatus | L. amazonensis | Parasite host | BR | Savani et al., 2010 | |
| Eumops glaucinus | L. amazonensis | Parasite host | BR | Savani et al., 2010 | |
| E. auripendulus | L. amazonensis | Parasite host | BR | Savani et al., 2010 | |
| Artibeus literatus | L. amazonensis | Parasite host | BR | Savani et al., 2010 | |
| Sturnira lilium | L. amazonensis | Parasite host | BR | Savani et al., 2010 | |
| Myotis nigricans | L. amazonensis | Parasite host | BR | Savani et al., 2010 |
Countries: AR – Argentine, BR – Brazil, CL – Chile, CO – Colombia, VE – Venezuela; FG – French Guiana; PE – Peru; PN – Panama; EC – Ecuador; BO – Bolivia; US – United States of America; BE – Belize; MX – Mexico; HN – Honduras; CR – Costa Rica.
IOC L*: Characterized Strains deposited in the Leishmania sp. Collection of the Oswaldo Cruz Institute (www.clioc.fiocruz.br). The number refers to the deposit number in CLIOC Catalogue.
Didelphis albiventris is abundant in central South America, from Colombia to northern Argentina, and is quite abundant in northeastern, central and southern Brazil. L. infantum isolation from this marsupial species was first described in Bahia, Brazil (Sherlock et al., 1984). Later, the same authors demonstrated its infectivity to vectors by xenodiagnosis (Sherlock, 1996), and others reported their natural infection detected by PCR (Humberg et al., 2012; Santiago et al., 2007). The other Leishmania species found infecting D. albiventris are L. braziliensis (Quaresma et al., 2011) and L. peruviana (Llanos-Cuentas et al., 1999) (Table 1).
L. infantum has also been detected in D. aurita (Carreira et al., 2012), and another study also strongly suggests such infection in the periphery of urban areas (Santiago et al., 2007). Although its role as a reservoir has not yet been demonstrated, it has strong potential to act as a reservoir due to the great phylogenetic proximity among the Didelphis species (Jansa et al., 2014). A unique study on a marsupial species able to explore distinct forest strata, the opossum Philander opossum, described its infection by L. amazonensis (Lainson et al., 1981a). The Leishmania species found infecting other marsupial species are described in Table 1 (Quintal et al., 2011).
Apart from the Didelphis species, which are proven as potential Leishmania reservoirs, other marsupial species are poorly studied. These ancient mammals are perhaps the very first Leishmania spp. hosts in the Americas, although their role in transmission net remains to be defined.
4.2. Order Pilosa
This order is composed of anteaters and sloths, which, along with armadillos (order Cingulata), compose the superorder Xenarthra (odd joints), previously known as Edentata (Moller-Krull et al., 2007). Together with the marsupials, these ancient Leishmania hosts are also native American fauna and present a peculiar blood–vessel structure that allows an extremely low metabolic rate, sparing energy (Bugge, 1979). Since the Tertiary Period, many representatives of this taxon have become extinct, and the extant genera constitute only a small proportion of the order. Mammals from this order have a long co-evolutionary history with trypanosomatids, including several Leishmania and Trypanosoma species, as well as the poorly studied genus Endotrypanum (Rotureau, 2006).
Sloths are arboreal inhabitants of tropical regions of Central and South America and are represented by two genera, Bradypus (Bradypodidae family) and Choloepus (Magalonichidae family). Sloths have reduced muscle mass and move slowly between trees by traveling directly through the arboreal strata, descending only weekly to defecate (Miranda and Costa, 2006). The two-toed sloth (Choloepus didactylus) is a potential reservoir of L. guyanensis, as demonstrated by the high rates of parasite isolation from intact skin (as well as viscera), which vary from 35% to 47% in French Guiana (Dedet et al., 1989; Gentile et al., 1981) and reach up to 46% in Brazil (Lainson et al., 1981a).
L. shawi was described infecting the two-toed sloth and the pale-throated sloth (Bradypus tridactylus), both in Brazil (Lainson et al., 1989). In Panama, L. colombiensis was isolated from the viscera of Hoffmann's two-toed sloth (Choloepus hoffmanni) (Kreutzer et al., 1991), while L. equatorensis was found infecting the same species in Ecuador (Grimaldi et al., 1992). Finally, L. panamensis, a species closely related to L. guyanensis, has been described in Choloepus hoffmanni from Panama (Ashford, 2000) (Table 1).
The anteaters constitute a single family (Myrmecophagidae) that are mainly arboreal, but that may also explore the terrestrial strata. The isolation of Leishmania was described in only one species, the lesser anteater Tamandua tetradactyla. L. guyanensis (Lainson et al., 1981a), L. amazonensis (Mimori et al., 1989), and L. infantum, this last in mixed infection with T. cruzi and T. rangeli (de Araujo et al., 2013), were found infecting the lesser anteater (Table 1).
The diversity of Leishmania species already known to infect sloths and anteaters suggests that these mammals may be important hosts for parasite species that are transmitted in the arboreal strata. In fact, most of the Leishmania species found infecting these hosts are transmitted by vectors associated with the arboreal strata, such as Lu. umbratilis and Lu. whitmani.
4.3. Order Cingulata
Armadillos, together with didelphid marsupials and Pilosa, are also among the oldest mammal groups from the Americas. They are also the most primitive of the xenarthrans. Members of the family Dasypodidae are the only surviving species in the order and are found from the southern United States to the Straits of Magellan (Miranda and Costa, 2006). So far, the nine-banded armadillo (Dasypus novemcinctus) is the only non-human host from which L. naiffi has been isolated (from blood, liver and spleen) (Lainson and Shaw, 1989; Naiff et al., 1991). L. guyanensis is another species already detected in D. novemcinctus from Brazil (Lainson et al., 1979). In some rural areas, armadillos are commonly observed invading chicken pens, searching for eggs, and frequenting peridomestic areas (personal observations), where it is possible that they can be a source of Leishmania infection for sandflies in this environment.
Armadillos, sloths and anteaters are hunted and eaten in some areas of South America, such as the Amazon. People commonly care for the young in their backyards after having killed the mothers during a hunt. The young are kept until they reach adulthood and we cannot exclude the possibility of they become sources of infection in the peridomestic environment.
4.4. Order Rodentia
Rodents are the most diverse and widespread order of mammals and include several cryptic species that can only be separated by karyotyping (Bonvicino et al., 2002). The first rodents (Hystricognathi – caviomorphs) arrived in the Americas (along with primates) from Africa approximately 45 million years ago. The second wave of rodent migration to the Americas (Sciurognathi – cricetids) was much more recent and included an initial establishment in North America (Flynn and Wyss, 1998). Since their arrival, rodents have diversified widely and may be found in desert, adapted to aquatic media, digging long and interconnected tunnels, and in forest canopies (Wilson and Reeder, 2005). This taxon is most likely the most studied in terms of infection by Leishmania spp. in both natural and experimental conditions; however, excepting a few studies, experimental infections have been conducted in laboratory mouse lineages, which are not representative of the wild Mus musculus.
After the Pilosa, Marsupialia and Cingulata, caviomorphs (sub-order Hystricognathi) are most likely the most ancient hosts of Leishmania spp. Moreover, their arrival in the Americas is related to the entry of some species from the sub-genus Leishmania into the continent (Thomaz-Soccol et al., 1993). Caviomorphs from the genus Proechimys were already found to be infected by various Leishmania species. These rodents are characterized by their longevity (more than 3 years in captivity) and high abundance in most localities where they are found in tropical forests of Central and South America (Ashford, 1996). Various Proechimys species have been identified as potential reservoirs of L. amazonensis in Brazil and French Guiana, as demonstrated by the frequent skin parasitism confirmed by tissue culture (Arias et al., 1981; Dedet et al., 1989). In French Guiana, for example, this infection was observed in two sympatric species, P. cuvieri and P. guyanensis (Rotureau, 2006). Other reports of natural infection in the skin of these rodents include: L. infantum in P. canicollis from Colombia (Travi et al., 1998a), and L. guyanensis in Proechimys sp. from French Guiana (Dedet et al., 1989), and Brazil (Lainson et al., 1981a) (Table 1).
P. semispinosus from Colombia experimentally infected with L. panamensis developed self resolving non-ulcerated lesions (from which parasites could be re-isolated, and which were demonstrated to be highly infective to vectors in the initial phase of infection (Travi et al., 2002). This host–parasite interaction exemplifies a temporal reservoir competence in one host species, passing from an amplifier host (in the beginning of infection) to a maintenance host, in which transmissibility competence is lower. In contrast, the same rodent species experimentally infected with L. infantum developed only subclinical infection and was not infective to vectors, although the authors re-isolated the parasites from the spleen of some rodents during necropsy (Travi et al., 2002). Other authors have detected no infection in laboratory-bred specimens of another species, P. guyannensis, after inoculation with promastigotes or amastigotes of L. infantum (Lainson et al., 2002). This difference may be due to many variables related to the host and the parasite, such as the intra-specific heterogeneity of both taxa and/or the size and route of the inoculum.
Considered monospecific until 2002, caviomorphs from the genus Thrichomys comprise at least five cryptic species distributed across different biomes in Brazil (Bonvicino et al., 2002). T. apereoides were found to be infected with L. braziliensis, L. guyanensis, L. infantum and L. amazonensis in leishmaniasis-endemic areas in Minas Gerais, Brazil (Oliveira et al., 2005; Quaresma et al., 2011). Recently, we also detected infection by various Leishmania species in these rodents: L. infantum, L. naiffi, L. braziliensis and L. shawi in T. laurentius, L. shawi in T. inermis and L. naiffi in T. pachyurus (Cássia-Pires et al., unpublished data). Moreover, T. laurentius experimentally infected with L. infantum and L. braziliensis were able to maintain the infection and parasite re-isolation was achieved up to 12 months after infection. Leishmania DNA was detected in all experimental groups and in all tissues sampled, independent of the Leishmania species inoculated (Roque et al., 2010).
In addition to Proechimys spp. and Thrichomys spp., L. infantum has been diagnosed in Clyomys laticeps, Dasyprocta azarae, Nectomys squamipes, Holochilus sciureus and Rhipidomys mastacalis from Brazil (Cássia-Pires et al., unpublished data; Dantas-Torres and Brandão-Filho, 2006; Quaresma et al., 2011; Lima et al., 2013; ) and Rattus rattus from Brazil and Venezuela (Quinnell and Courtenay, 2009). Natural infection of Coendu prehensilis, used as sentinels in Bolivia, has been parasitologically confirmed in the liver and spleen (Le Pont et al., 1989).
Regarding L. braziliensis, if we consider only studies that confirmed the identity of the etiological agent (not considering the ancient L. braziliensis sensu lato), the following rodent species have been described to be naturally infected: Akodon arviculoides, Mus musculus, Nectomys squamipes, Necromys (=Bolomys) lasiurus, Oryzomys nigripes, Rattus rattus and Sigmodon hispidus (Brandão-Filho et al., 2003; de Freitas et al., 2012; De Lima et al., 2002; Forattini et al., 1972; Peterson et al., 1988; Rocha et al., 1988; Vasconcelos et al., 1994). In other cases, the authors confirmed infection by the subgenus Leishmania (Viannia) sp. (Holochilus scieurus and Cerradomys subflavus) (Brandão-Filho et al., 2003; Lima et al., 2013) or tentatively identified the etiological agent through the biological pattern of in vitro growth (Rhipidomys leucodactylus and Proechimys guyannensis) (Lainson et al., 1981b).
Rodents are also usually considered as the main reservoirs of Leishmania from the L. mexicana complex (L. mexicana and L. amazonensis). L. amazonensis was described in rodents from the following genera: Akodon, Dasyprocta Oligoryzomys, Oryzomys, Proechimys, Thrichomys and Sciurus (Arias et al., 1981; Kerr et al., 2006; Lainson et al., 1981b; Mimori et al., 1989; Oliveira et al., 2005; Telleria et al., 1999). None of these studies, however, included follow-up of the infection or demonstrated competence to infect vectors.
L. mexicana has been isolated from various species of Neotoma, including a specimen of N. floridana with a large lesion in the ear from which the parasite could be isolated (Kerr et al., 1995; McHugh et al., 2003). This finding was informative, suggesting that this rodent species may be infective for the vector and an important reservoir of L. mexicana. Ototylomys phyllotis from Belize should be considered as a possible reservoir of L. mexicana because of its relative abundance, prevalence of infection and attraction to Lu. flaviscutellata, the most important vector in the region. Curiously, the same author failed to reproduce this infection under experimental conditions (Ashford, 1996), possibly due to factors occurring only in nature, such as stress and concomitant infections, which may be important for the establishment of Leishmania infection. This situation highlights the importance of the studies of naturally infected specimens and the difficulties of adopting potential reservoir hosts as alternative models for leishmaniasis studies. Moreover, these findings attest to the hazards of applying conclusions based solely on experimental models to natural systems.
The persistence of L. mexicana infection in wild rodents was demonstrated twice. The first such finding occurred in Mexico, where 29 naturally infected rodents were maintained in captivity and tested monthly for parasites for up to 2 years. In that study, the authors demonstrated persistent infection, including symptomatic infections, in Sigmodon hispidus, Oryzomys melanotis, Ototylomys phyllotis and Peromyscus yucatanicus, the latter two being the most important because of their high relative abundance in local fauna and longer life spans (Van Wynsberghe et al., 2000). Second, in the United States, during a 19-month mark–release–recapture study of Neotoma micropus, the authors reported the persistence of L. mexicana infection for up to 1 year (Raymond et al., 2003). Heteromys, Nyctomys and Reithrodontomys were also found infected with L. mexicana (Ashford, 1996; De Lima et al., 2002; Disney, 1968; Lainson and Strangways-Dixon, 1964; Van Wynsberghe et al., 2009).
Leishmania lainsoni was isolated from fragments of intact skin from pacas (Agouti paca) in the Brazilian state of Pará (Silveira et al., 1991) and from Coendu sp. (Table 1). Leishmania panamensis was isolated from naturally infected Heteromys dermarestianus from Costa Rica (Zeledon et al., 1977), while a squirrel Scirus granatensis was found to be infected with L. equatorensis in Ecuador (Grimaldi et al., 1992). Leishmania peruviana, a species suggested to be a synonym of L. braziliensis, was isolated from the Peruvian Phyllotis andinum (Llanos-Cuentas et al., 1999). Finally, L. hertigi/L. deanei and L. enriettii, species taxonomically more similar to Endotrypanum than to Leishmania have been described, respectively, in porcupines Coendu spp. (Herrer, 1971; Silva et al., 2013) and in the guinea pig Cavia porcellus (Machado et al., 1994).
Taken together, a broad diversity of Leishmania species naturally infect this mammal group, most likely reflecting the diversity of ecological niches occupied by the hosts. The differences observed among the rodent species include the forest strata they occupy and their reproductive strategies (seasonality, gestation time and number of offspring), and these traits should be considered evaluations of the importance of a rodent species as a Leishmania reservoir. Moreover, as expected for every host–parasite interaction, this heterogeneous mammalian taxon shows a spectrum of competence to maintain and transmit Leishmania from high susceptibility with high transmissibility competence to quick control of infection.
4.5. Order Carnivora
The mammals from this order also comprise a very heterogeneous group, including strict carnivores, such as ocelots (Leopardus pardalis) and tayras (Eira barbara) and species that supplement their diet with insects and fruits, such as coatis (Nasua nasua) and maned wolves (Chrysocyon brachyurus). Most have a large biomass and large range, important aspects of parasite dispersion (Rocha et al., 2013). Moreover, some species such as raccoons and tayras are found both on the ground and in the canopy, favoring the dispersion of parasites among forest strata. Unfortunately, carnivores require large ranges and, because of their potential to predate on livestock (mainly chickens and cattle), are heavily hunted, placing some carnivore species at risk of extinction (Silva and Adania, 2007).
Two carnivore species are closely linked to humans: dogs and cats. Dogs are the most important reservoirs of L. infantum throughout South America, although they can be infected with at least six other Leishmania species (Dantas-Torres, 2009). Recently, the importance of cats in Leishmania epidemiology has also been suggested (Pennisi et al., 2013). Among the wild carnivore hosts of L. infantum, the first description of infection was in the crab-eating fox Cerdocyon thous, although the authors inaccurately reported the host as Lycalopex vetulus (Courtenay et al., 1996; Deane and Deane, 1955). Since then, many studies have confirmed L. infantum infection in C. thous by parasitological, serological and/or molecular assays. Notably, these animals sometimes develop serious symptoms of the disease and present with amastigotes in intact skin, as also described in domestic dogs. Their prevalence of infection may range from 42% (by parasitological tests) to 78% (by serology) (Lainson et al., 1990; Quinnell and Courtenay, 2009; Silva et al., 2000). The vector infectivity was proven by xenodiagnosis, although the infection rate of vectors is reported to be lower than that observed for domestic dogs (Courtenay et al., 2002; Quinnell and Courtenay, 2009).
Apart from C. thous, another wild carnivore that is a potential reservoir of L. infantum is the bush dog Speothos venaticus. An individual kept in a zoo in Rio de Janeiro, Brazil, is the only wild canid, except for C. thous, from which L. infantum was isolated (Figueiredo et al., 2008). Infection in bush dogs was also confirmed by direct visualization, PCR and serology in two females with clinical signs of visceral leishmaniasis and maintained in other Brazilian zoos (Lima et al., 2009; Souza et al., 2010). Other wild canid species found to be infected, albeit only by PCR and/or serology, were the hoary fox Pseudalopex vetulus and the maned wolf Chrysocyon brachyurus (Curi et al., 2006; Luppi et al., 2008) (Table 1).
Some authors have investigated Leishmania infection in captive wild carnivores. Five of 15 wild canids belonging to the four native species mentioned earlier were found to be infected in a zoo in Belo Horizonte, Brazil. Of these, one bush dog and one hoary fox developed clinical signs of visceral leishmaniasis (Luppi et al., 2008). Among the wild felines, five pumas (Puma concolor) and one jaguar (Panthera onca) in a zoo from Cuiabá, Brazil, were PCR-positive in lymph-node puncture biopsy, L. infantum was specifically identified by the digestion of the amplified products with restriction enzymes (Dahroug et al., 2010). Later, the same authors demonstrated L. infantum infection in one lion, a non-native felid species, kept in the same zoo (Dahroug et al., 2011).
In addition to L. infantum, at least four other Leishmania species were found in wild carnivores: L. shawi in coatis Nasua nasua (Lainson et al., 1989); L. guyanensis in the kinkajou Potos flavus (Pajot et al., 1982); L. amazonensis in kinkajous, crab-eating foxes and skunks Conepatus chinga (Kreutzer et al., 1991; Rotureau, 2006; Telleria et al., 1999); and L. braziliensis in one Bolivian skunk (Buitrago et al., 2011) (Table 1).
Contrary to the numerous reports of infection in dogs and cats, much remains to study in terms of the putative roles of wild carnivores as Leishmania reservoirs. As in all host–parasite interactions, the infection patterns display regional and even individual peculiarities (Rocha et al., 2013). If we consider that in some biomes (“Pantanal or Chaco”, “Cerrado”, and “Pampa”) carnivore species are abundant and represent a huge biomass, any study of Leishmania reservoirs must include carnivores, including their Leishmania infection pattern, density and population structure in the area. Despite its inherent difficulties, the study of wild carnivores, especially in the areas where their relative abundance is high, is of fundamental importance to improve understanding of Leishmania ecology.
4.6. Order Primata
Nonhuman primates can be divided in two groups: the catarrhines (infraorder Catarrhini), from Africa, Europe and Asia (Old World Primates) and the platyrrhines (Platyrrhini) from the Americas (New World or Neotropical Primates). The main difference between them is that the catarrhines have upside-down nostrils on a long snout, while platyrrhines have laterally-faced nostrils on a shorter snout (Verona and Pissinatti, 2007). The different species of neotropical primates are included in the families Cebidae (tamarins) and Callitrichidae (marmosets), although some classifications also recognize three other families: Aotidae, Pithecidae and Atelidae. The neotropical primates occupy distinct arboreal strata and consume diverse diets, including species that feed on fruits, invertebrates and even small mammals (Verona and Pissinatti, 2007).
To date, few studies have described natural infection by Leishmania parasites in neotropical primates. Infection by L. shawi was described in the tufted capuchin monkey Cebus apella and the bearded saki Chiropotes satanas (Lainson et al., 1989), while infection by Leishmania (Viannia) sp. was recently demonstrated in four Argentinean owl monkeys Aotus azarai (Acardi et al., 2013). In Panamá, Geoffroy's tamarin Saguinus geoffroyi and the owl monkey Aotus trivirgatus were found to be infected with L. amazonensis and L. braziliensis, respectively (Herrer and Christensen, 1976; Herrer et al., 1973). In a Brazilian zoo, one black-fronted titi Callicebus nigrifrons from Belo Horizonte/MG presented with a fatal disease that resembled visceral leishmaniasis. Histological and immunohistochemical examinations, as well as a PCR specific for parasites from the L. donovani complex, confirmed infection with L. infantum (Malta et al., 2010). The other primate species that had PCR-positive blood samples in the same study were Alouatta guariba, Cebus xanthosternos, Leonthopitecus crysomelas, Aotus nigriceps, Pithecia irrorata and Saguinus imperator (Malta et al., 2010). In the zoo in Bauru/SP, Leishmania amazonensis was detected by PCR-RFLP in a spider monkey Ateles paniscus from the endemic Amazon region (Lima et al., 2012b) (Table 1).
Leishmania species that circulate in the Americas have been demonstrated to infect other neotropical primates, but only under experimental conditions. Most of these studies focused on the immune response to different drug treatments or on vaccine development. For many years, black-tufted marmosets Callithrix penicillata were used in experimental studies with L. braziliensis and L. amazonensis (Cuba et al., 1990; Cuba-Cuba and Marsden, 1993). Experimental infection of the common squirrel monkey Saimiri sciureus resulted in non-ulcerated skin lesions from which L. braziliensis and/or L. panamensis could be re-isolated (Pung et al., 1988). Owl monkeys Aotus trivirgatus developed localized cutaneous lesions after experimental infection with L. braziliensis, L. mexicana and L. panamensis (Christensen and de Vasquez, 1981; Lujan et al., 1986). Cebus apella developed skin lesions after experimental infection with L. lainsoni, L. amazonensis, L. braziliensis, L. mexicana and L. guyanensis (Garcez et al., 2002; Grimaldi, 2008). Conversely, Cebus nigrivittatus developed fatal disease when experimentally infected with L. infantum (Vouldoukis et al., 1986).
All neotropical primates are included in the list of the “Convention on International Trade in Endangered Species of Wild Fauna and Flora” (CITES), indicating that all are vulnerable to some degree (Verona and Pissinatti, 2007). For this reason, many species such as the golden lion tamarin Leonthopitecus rosalia are included in conservation programs. These programs often include exchange, translocation and re-introduction of animals without consideration of their parasite fauna, here including Leishmania and other trypanosomatids. Data from naturally infected primates demonstrate that these mammals may be involved in the maintenance of Leishmania in the wild, especially considering their ecology, species transmitted in the canopy. Taking into account the transmission cycle of these parasites, a lack of knowledge regarding the health status of the relocated primates may result in the introduction of infected mammals into a given area, promoting the establishment of new transmission cycles (Lisboa et al., 2006).
4.7. Order Chiroptera
Bats are nocturnal mammals and the only able to fly (sometimes associated with seasonal migration), an important trait that can result in the dissemination of parasite species. Their dispersion capacity is due to the ability to do true flapping flight (apparently evolved differently among bat lineages) and the sophisticated echolocation system that allows them to identify the environment (Jones and Teeling, 2006). Despite their known diversity, bats are still considered as a monophyletic group (Bishop, 2008; Bisson et al., 2009).
Bats are commonly infected with several trypanosomatid species, mainly from the Trypanosoma genus: T. cruzi, T. vespertilionis, and T. (Megatrypanum) sp., among others (Lima et al., 2012a). There is only one report of the isolation of Leishmania parasites (L. infantum) from the blood of a short-tailed fruit bat Carollia perspicillata in Venezuela (De Lima et al., 2008) (Table 1). Before that, Lampo et al. had demonstrated that bats could be sources of blood for Lutzomyia longipalpis in Venezuelan caves (Lampo et al., 2000).
In Brazil, two Leishmania species were identified in macerated fragments of spleen and liver from bats using a nested PCR followed by sequencing of the amplified products. Molossus molossus and Glossophaga soricina were found to be infected with L. infantum and L. amazonensis, and the latter was also found in Molossus rufus, Nyctinomops laticaudatus, Eumops glaucinus, E. auripendulus, Artibeus literatus, Sturnira lilium and Myotis nigricans (Savani et al., 2010). Recently, Leishmania (Viannia) sp. was detected in a skin lesion from Glossophaga soricina and blood from Molossus molossus (Shapiro et al., 2013) (Table 1). In this article, although the authors have described infection with L. braziliensis, PCR-RFLP using primers b1 and b2 (Schonian et al., 2003) does not allow for differentiation among other species from the same subgenus, such as L. guyanensis.
Bats should not be excluded as potential reservoirs of Leishmania sp. because of the lack of studies involving Leishmania and bats. Chiroptera represents 39% of the 560 mammal species reported in South American rainforests, it is the most common mammal group in terms of diversity and biomass (Emmons and Feer, 1997; Rotureau, 2006). These flying mammals are found in wild, domestic and synanthropic environments, being able to colonize different habitats in different ecotypes. Their refuges include hollow trees, the canopies of palm trees and ceilings of human houses and other rural buildings. Their high abundance and adaptability to peri-domestic environment reinforce the importance of investigating bats, already recognized as reservoirs of other trypanosomatids (Jansen and Roque, 2010), in the transmission cycles of Leishmania species.
5. Conclusions and perspectives
Many decades have passed since the description of Leishmania parasites, but their epidemiology is still not well understood in part because of the human-health focus of most studies. Only recently, influenced by the “one health” approach has the epidemiology of leishmaniasis started to be evaluated from a broader perspective (Palatnik-de-Sousa and Day, 2011).
In the case of human visceral leishmaniasis caused by L. infantum, the idea that dogs are the only reservoir of the parasite has led health authorities to direct the eradication of seropositive dogs on the basis that this action was the only way to control this zoonosis. In fact, several studies have demonstrated that dogs are epidemiologically important as reservoirs in different localities (reviewed by Lainson and Rangel, 2005; Dantas-Torres, 2009; Quinnell and Courtenay, 2009). Nevertheless, the participation of other infected mammals, rather than dogs, in the transmission cycle of L. infantum in urban areas, was already proposed for cats and opossums, for example (Pennisi et al., 2013; Santiago et al., 2007). The low effectiveness of dog culling program in Brazil is probably due to an assemblage of factors, most of them related to the lack of a structured surveillance system, and include the high interval between tests and between the positive result and dog elimination, the rapid replacement of susceptible dogs when an infected dog is euthanized, and the resistance of owners to euthanize their infected dogs (Costa et al., 2013; Grimaldi et al., 2012; Nunes et al., 2008). Some of these localities are very close to sylvatic areas, and the possibility that wild mammals may serve as a source of infection to vectors in peridomiciliary areas has been ignored. The putative participation of these mammals is an important additional factor to be considered in the proposition of measures to control this zoonosis. This review highlights species from distinct orders that may maintain and serve as a source of infection to phlebotomine sand fly vectors, providing a constant source of re-infection to a peri-domestic transmission system.
The reservoirs of the Leishmania species responsible for the cutaneous forms of human leishmaniasis are still unknown most likely because research has focused on the search for a specific reservoir host, as observed for dogs and L. infantum. These species may be maintained in the wild by a different strategy, as by a few “hot species” with high transmissibility competence or, most likely, through a reservoir system, an assemblage of mammals with distinct and transient degrees of transmissibility competence throughout infection. This hypothesis agrees with the reservoir definition proposed by Ashford (1997), almost 20 years ago. This system involves a tradeoff that could explain the evolutionary success of these parasite species: several individuals are infected, but each is competent for transmission for only a limited time, while retaining the infection for long periods of time. The sum of multiple short periods of infectivity in numerous infected mammals guarantees the maintenance and transmission of these Leishmania species.
All the links in the epidemiological chain must be clarified as a prerequisite for effective control strategies (Abdussalan, 1959; Palatnik-de-Sousa and Day, 2011; Shaw, 2007). We are still far from understanding the maintenance of different Leishmania species in nature. In this sense, the follow-up of naturally infected animals and experimental studies using potential reservoirs are essential to improving understanding of the mechanisms of maintenance of these parasites in their natural hosts. In the field, the studies should not be restricted to previously described infected hosts, but should be carried out using an integrated ecological approach to understand the role of each host species in the maintenance and amplification of Leishmania parasites. Priorities include the identification of the factors that influence the transmissibility competence of the individual mammalian hosts and understanding how environmental management could decrease infections in humans living close to sylvatic.
Over the last century, the scientific community has shown that different and several wild mammal species can become infected with Leishmania species. The focus must change to identify species that may serve as sources of infection to vectors and amplify enzootic foci, constituting a risk for human transmission. To this end, a paradigm shift in research and surveillance of wild reservoirs of Leishmania is urgently needed. This change will depend, among other factors, on understanding reservoir systems and acknowledging the importance of understanding the role each mammal species plays in maintaining these parasites in nature. The factors involved in the amplification of enzootic foci are temporally and regionally specific, and understanding some of these factors may support the development of effective and sustainable strategies for leishmaniasis surveillance.
Acknowledgements
AMJ is a “Cientista do Nosso Estado”, provided by FAPERJ and is financially supported by CNPq (“Bolsista de Produtividade, nível 1”, CNPq). ALRR is a “Jovem Cientista do Nosso Estado” provided by FAPERJ. The authors have declared that no competing interests exist.
References
- Abdussalan M. Significance of ecological studies of wild animal reservoir of zoonoses. Bull. World Health Organ. 1959;21:179–186. [PMC free article] [PubMed] [Google Scholar]
- Acardi S.A., Rago M.V., Liotta D.J., Fernandez-Duque E., Salomon O.D. Leishmania (Viannia) DNA detection by PCR-RFLP and sequencing in free-ranging owl monkeys (Aotus azarai azarai) from Formosa, Argentina. Vet. Parasitol. 2013;193:256–259. doi: 10.1016/j.vetpar.2012.12.012. [DOI] [PubMed] [Google Scholar]
- Aguirre A.A., Tabor G.M. Global factors driving emerging infectious diseases. Ann. N. Y. Acad. Sci. 2008;1149:1–3. doi: 10.1196/annals.1428.052. [DOI] [PubMed] [Google Scholar]
- Alexander K.A., Lewis B.L., Marathe M., Eubank S., Blackburn J.K. Modeling of wildlife-associated zoonoses: applications and caveats. Vector Borne Zoonotic Dis. 2012;12:1005–1018. doi: 10.1089/vbz.2012.0987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvar J., Velez I.D., Bern C., Herrero M., Desjeux P., Cano J. Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE. 2012;7:e35671. doi: 10.1371/journal.pone.0035671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araújo A., Reinhard K., Ferreira L.F., Pucu E., Chieffi P.P. Paleoparasitology: the origin of human parasites. Arq. Neuropsiquiatr. 2013;71:722–726. doi: 10.1590/0004-282X20130159. [DOI] [PubMed] [Google Scholar]
- Arias J.R., Naif R.D., Miles M.A., de Souza A.A. The opossum, Didelphis marsupialis (Marsupialia: didelphidae), as a reservoir host of Leishmania braziliensis guyanensis in the Amazon Basin of Brazil. Trans. R. Soc. Trop. Med. Hyg. 1981;75:537–541. doi: 10.1016/0035-9203(81)90194-2. [DOI] [PubMed] [Google Scholar]
- Ashford D.A., Bozza M., Freire M., Miranda J.C., Sherlock I., Eulalio C. Comparison of the polymerase chain reaction and serology for the detection of canine visceral leishmaniasis. Am. J. Trop. Med. Hyg. 1995;53:251–255. doi: 10.4269/ajtmh.1995.53.251. [DOI] [PubMed] [Google Scholar]
- Ashford R.W. Leishmaniasis reservoir and their significance in control. Clin. Dermatol. 1996;14:523–532. doi: 10.1016/0738-081x(96)00041-7. [DOI] [PubMed] [Google Scholar]
- Ashford R.W. What it takes to be a reservoir host. Belg. J. Zool. 1997;127:85–90. [Google Scholar]
- Ashford R.W. The leishmaniases as emerging and reemerging zoonoses. Int. J. Parasitol. 2000;30:1269–1281. doi: 10.1016/s0020-7519(00)00136-3. [DOI] [PubMed] [Google Scholar]
- Austad S.N. The adaptable opossum. Sci. Am. 1988;258:54–59. [Google Scholar]
- Bishop K.L. The evolution of flight in bats: narrowing the field of plausible hypotheses. Q. Rev. Biol. 2008;83:153–169. doi: 10.1086/587825. [DOI] [PubMed] [Google Scholar]
- Bisson I.A., Safi K., Holland R.A. Evidence for repeated independent evolution of migration in the largest family of bats. PLoS ONE. 2009;4:e7504. doi: 10.1371/journal.pone.0007504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonvicino C.R., Otazu I.B., D'Andrea P.S. Karyologic evidence of diversification of the genus Thrichomys (Rodentia, Echimyidae) Cytogenet. Genome Res. 2002;97:200–204. doi: 10.1159/000066613. [DOI] [PubMed] [Google Scholar]
- Botero A., Thompson C.K., Peacock C.S., Clode P.L., Nicholls P.K., Wayne A.F. Trypanosomes genetic diversity, polyparasitism and the population decline of the critically endangered Australian marsupial, the brush tailed bettong or woylie (Bettongia penicillata) Int. J. Parasitol. Parasite. Wildl. 2013;2:77–89. doi: 10.1016/j.ijppaw.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandão-Filho S.P., Brito M.E., Carvalho F.G., Ishikawa E.A., Cupolillo E., Floeter-Winter L. Wild and synanthropic hosts of Leishmania (Viannia) braziliensis in the endemic cutaneous leishmaniasis locality of Amaraji, Pernambuco State, Brazil. Trans. R. Soc. Trop. Med. Hyg. 2003;97:291–296. doi: 10.1016/s0035-9203(03)90146-5. [DOI] [PubMed] [Google Scholar]
- Bugge J. Cephalic arterial pattern in New World edentates and Old World pangolins with special reference to their phylogenetic relationships and taxonomy. Acta Anat. (Basel) 1979;105:37–46. doi: 10.1159/000145104. [DOI] [PubMed] [Google Scholar]
- Buitrago R., Cupolillo E., Bastrenta B., Le Pont F., Martinez E., Barnabe C. PCR-RFLP of ribosomal internal transcribed spacers highlights inter and intra-species variation among Leishmania strains native to La Paz, Bolivia. Infect. Genet. Evol. 2011;11:557–563. doi: 10.1016/j.meegid.2010.11.019. [DOI] [PubMed] [Google Scholar]
- Carreira J.C., da Silva A.V., de Pita P.D., Brazil R.P. Natural infection of Didelphis aurita (Mammalia: marsupialia) with Leishmania infantum in Brazil. Parasit. Vectors. 2012;5:111. doi: 10.1186/1756-3305-5-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaves L.F., Hernandez M.J., Dobson A.P., Pascual M. Sources and sinks: revisiting the criteria for identifying reservoirs for American cutaneous leishmaniasis. Trends Parasitol. 2007;23:311–316. doi: 10.1016/j.pt.2007.05.003. [DOI] [PubMed] [Google Scholar]
- Christensen H.A., de Vasquez A.M. Susceptibility of Aotus trivirgatus to Leishmania braziliensis and L. mexicana. Am. J. Trop. Med. Hyg. 1981;30:54–56. doi: 10.4269/ajtmh.1981.30.54. [DOI] [PubMed] [Google Scholar]
- Corredor A., Gallego J.F., Tesh R.B., Morales A., De Carrasquilla C.F., Young D.G. Epidemiology of visceral leishmaniasis in Colombia. Am. J. Trop. Med. Hyg. 1989;40:480–486. doi: 10.4269/ajtmh.1989.40.480. [DOI] [PubMed] [Google Scholar]
- Costa D.N., Codeço C.T., Silva M.A., Werneck G.L. Culling dogs in scenarios of imperfect control: realistic impact on the prevalence of canine visceral leishmaniasis. PLoS Negl. Trop. Dis. 2013;7:e2355. doi: 10.1371/journal.pntd.0002355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtenay O., Santana E.W., Johnson P.J., Vasconcelos I.A., Vasconcelos A.W. Visceral leishmaniasis in the hoary zorro Dusicyon vetulus: a case of mistaken identity. Trans. R. Soc. Trop. Med. Hyg. 1996;90:498–502. doi: 10.1016/s0035-9203(96)90293-x. [DOI] [PubMed] [Google Scholar]
- Courtenay O., Quinnell R.J., Garcez L.M., Shaw J.J., Dye C. Infectiousness in a cohort of Brazilian dogs: why culling fails to control visceral leishmaniasis in areas of high transmission. J. Infect. Dis. 2002;186:1314–1320. doi: 10.1086/344312. [DOI] [PubMed] [Google Scholar]
- Courtenay O., Carson C., Calvo-Bado L., Garcez L.M., Quinnell R.J. Heterogeneities in Leishmania infantum infection: using skin parasite burdens to identify highly infectious dogs. PLoS Negl. Trop. Dis. 2014;9:e2583. doi: 10.1371/journal.pntd.0002583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuba C.A., Ferreira V., Bampi M., Magalhaes A., Marsden P.D., Vexenat A. Experimental infection with Leishmania (Viannia) braziliensis and Leishmania (Leishmania) amazonensis in the marmoset, Callithrix penicillata (Primates: Callithricidae) Mem. Inst. Oswaldo Cruz. 1990;85:459–467. doi: 10.1590/s0074-02761990000400011. [DOI] [PubMed] [Google Scholar]
- Cuba-Cuba C.A., Marsden P.D. Marmosets in New World leishmaniasis research. Medicina (B Aires) 1993;53:419–423. [PubMed] [Google Scholar]
- Curi N.H., Miranda I., Talamoni S.A. Serologic evidence of Leishmania infection in free-ranging wild and domestic canids around a Brazilian National Park. Mem. Inst. Oswaldo Cruz. 2006;101:99–101. doi: 10.1590/s0074-02762006000100019. [DOI] [PubMed] [Google Scholar]
- de Araujo V.A., Boite M.C., Cupolillo E., Jansen A.M., Roque A.L. Mixed infection in the anteater Tamandua tetradactyla (Mammalia: pilosa) from Para State, Brazil: Trypanosoma cruzi, T. rangeli and Leishmania infantum. Parasitology. 2013;140:455–460. doi: 10.1017/S0031182012001886. [DOI] [PubMed] [Google Scholar]
- de Freitas T.P., D'Andrea P.S., de Paula D.A., Nakazato L., Dutra V., Bonvicino C.R. Natural infection of Leishmania (Viannia) braziliensis in Mus musculus captured in Mato Grosso, Brazil. Vector Borne Zoonotic Dis. 2012;12:81–83. doi: 10.1089/vbz.2010.0268. [DOI] [PubMed] [Google Scholar]
- Dahroug M.A., Almeida A.B., Sousa V.R., Dutra V., Turbino N.C., Nakazato L. Leishmania (Leishmania) chagasi in captive wild felids in Brazil. Trans. R. Soc. Trop. Med. Hyg. 2010;104:73–74. doi: 10.1016/j.trstmh.2009.08.003. [DOI] [PubMed] [Google Scholar]
- Dahroug M.A., Almeida A.B., Sousa V.R., Dutra V., Guimaraes L.D., Soares C.E. The first case report of Leishmania (leishmania) chagasi in Panthera leo in Brazil. Asian Pac. J. Trop. Biomed. 2011;1:249–250. doi: 10.1016/S2221-1691(11)60036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dantas-Torres F. Canine leishmaniosis in South America. Parasit. Vectors. 2009;2(Suppl. 1):S1. doi: 10.1186/1756-3305-2-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dantas-Torres F., Brandão-Filho S.P. Visceral leishmaniasis in Brazil: revisiting paradigms of epidemiology and control. Rev. Inst. Med. Trop. S. Paulo. 2006;48:151–156. doi: 10.1590/s0036-46652006000300007. [DOI] [PubMed] [Google Scholar]
- De Lima H., De Guglielmo Z., Rodriguez A., Convit J., Rodriguez N. Cotton rats (Sigmodon hispidus) and black rats (Rattus rattus) as possible reservoirs of Leishmania spp. in Lara State, Venezuela. Mem. Inst. Oswaldo Cruz. 2002;97:169–174. doi: 10.1590/s0074-02762002000200004. [DOI] [PubMed] [Google Scholar]
- De Lima H., Rodriguez N., Barrios M.A., Avila A., Canizales I., Gutierrez S. Isolation and molecular identification of Leishmania chagasi from a bat (Carollia perspicillata) in northeastern Venezuela. Mem. Inst. Oswaldo Cruz. 2008;103:412–414. doi: 10.1590/s0074-02762008000400018. [DOI] [PubMed] [Google Scholar]
- De Tommasi A.S., Otranto D., Dantas-Torres F., Capelli G., Breitschwerdt E.B., de Caprariis D. Are vector-borne pathogen co-infections complicating the clinical presentation in dogs? Parasit. Vectors. 2013;6:97. doi: 10.1186/1756-3305-6-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deane L.M., Deane M.P. Observações preliminares sobre a importância comparativa do homem, do cão e da raposa (Lycalopex vetulus) como reservatórios da Leishmania donovani em áreas endêmicas de Calazar, no Ceará. Hospital. 1955;48:79–98. [Google Scholar]
- Dedet J.P., Gay F., Chatenay G. Isolation of Leishmania species from wild mammals in French Guiana. Trans. R. Soc. Trop. Med. Hyg. 1989;83:613–615. doi: 10.1016/0035-9203(89)90374-x. [DOI] [PubMed] [Google Scholar]
- Desjeux P. Leishmaniasis: current situation and new perspectives. Comp. Immunol. Microbiol. Infect. Dis. 2004;27:305–318. doi: 10.1016/j.cimid.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Disney R.H.L. Observations on a zoonosis: leishmaniasis in British Honduras. J. Appl. Ecol. 1968;5:1–59. [Google Scholar]
- Emmons L.H., Feer F. University of Chicago Press; Chicago: 1997. Neotropical Rainforest Mammals. A Field Guide. [Google Scholar]
- Figueiredo F.B., Gremiao I.D., Pereira S.A., Fedulo L.P., Menezes R.C., Balthazar D.A. First report of natural infection of a bush dog (Speothos venaticus) with Leishmania (Leishmania) chagasi in Brazil. Trans. R. Soc. Trop. Med. Hyg. 2008;102:200–201. doi: 10.1016/j.trstmh.2007.10.001. [DOI] [PubMed] [Google Scholar]
- Flynn J.J., Wyss A.R. Recent advances in South American mammalian paleontology. Trends Ecol. Evol. 1998;13:449–455. doi: 10.1016/s0169-5347(98)01457-8. [DOI] [PubMed] [Google Scholar]
- Forattini O.P., Pattoli D.B.G., Rabello E.X., Ferreira O.A. Infecções naturais de mamíferos silvestres em área endêmica de leishmaniose tegumentar do Estado de São Paulo. Bras. Rev. Saude Publica. 1972;6:255–261. [PubMed] [Google Scholar]
- Garcez L.M., Goto H., Ramos P.K., Brigido M.C., Gomes P.A., Souza R.A. Leishmania (Leishmania) amazonensis-induced cutaneous leishmaniasis in the primate Cebus apella: a model for vaccine trials. Int. J. Parasitol. 2002;32:1755–1764. doi: 10.1016/s0020-7519(02)00138-8. [DOI] [PubMed] [Google Scholar]
- Gentile B., Le Pont F., Pajot F.X., Besnard R. Dermal leishmaniasis in French Guiana: the sloth (Choloepus didactylus) as a reservoir host. Trans. R. Soc. Trop. Med. Hyg. 1981;75:612–613. doi: 10.1016/0035-9203(81)90223-6. [DOI] [PubMed] [Google Scholar]
- Giorgio S. Moderna visão da evolução da virulência. Rev. Saude Publica. 1995;29:398–402. doi: 10.1590/s0034-89101995000500010. [DOI] [PubMed] [Google Scholar]
- Grimaldi G., Jr. The utility of rhesus monkey (Macaca mulatta) and other non-human primate models for preclinical testing of Leishmania candidate vaccines. Mem. Inst. Oswaldo Cruz. 2008;103:629–644. doi: 10.1590/s0074-02762008000700002. [DOI] [PubMed] [Google Scholar]
- Grimaldi G., Jr., Momen H., Naiff R.D., Mahon-Pratt D., Barrett T.V. Characterization and classification of leishmanial parasites from humans, wild mammals, and sand flies in the Amazon region of Brazil. Am. J. Trop. Med. Hyg. 1991;44:645–661. doi: 10.4269/ajtmh.1991.44.645. [DOI] [PubMed] [Google Scholar]
- Grimaldi G., Jr., Kreutzer R.D., Hashiguchi Y., Gomez E.A., Mimory T., Tesh R.B. Description of Leishmania equatorensis sp. n (Kinetoplastida: trypanosomatidae), a new parasite infecting arboreal mammals in Ecuador. Mem. Inst. Oswaldo Cruz. 1992;87:221–228. doi: 10.1590/s0074-02761992000200009. [DOI] [PubMed] [Google Scholar]
- Grimaldi G., Jr., Teva A., Santos C.B., Ferreira A.L., Falqueto A. The effect of removing potentially infectious dogs on the numbers of canine Leishmania infantum infections in an endemic area with high transmission rates. Am. J. Trop. Med. Hyg. 2012;86:966–971. doi: 10.4269/ajtmh.2012.12-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haydon D.T., Cleaveland S., Taylor L.H., Laurenson M.K. Identifying reservoirs of infection: a conceptual and practical challenge. Emerg. Infect. Dis. 2002;8:1468–1473. doi: 10.3201/eid0812.010317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrer A. Leishmania hertigi sp.n., from the tropical porcupine Coendou rothschildi Thomas. J. Parasitol. 1971;57:626–629. [PubMed] [Google Scholar]
- Herrer A., Christensen H.A. Epidemiological patterns of cutaneous leishmaniasis in Panama III. Endemic persistence of the disease. Am. J. Trop. Med. Hyg. 1976;25:54–58. doi: 10.4269/ajtmh.1976.25.54. [DOI] [PubMed] [Google Scholar]
- Herrer A., Christensen H.A., Beumer R.J. Reservoir host of cutaneous leishmaniasis among Panamanian forest mammals. Am. J. Trop. Med. Hyg. 1973;22:585. doi: 10.4269/ajtmh.1973.22.585. [DOI] [PubMed] [Google Scholar]
- Humberg R.M., Oshiro E.T., Cruz M.S., Ribolla P.E., Alonso D.P., Ferreira A.M. Leishmania chagasi in opossums (Didelphis albiventris) in an urban area endemic for visceral leishmaniasis, Campo Grande, Mato Grosso do Sul, Brazil. Am. J. Trop. Med. Hyg. 2012;87:470–472. doi: 10.4269/ajtmh.2012.11-0534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda-Garcia F.A., Feitosa M.M. Métodos de diagnóstico da leishmaniose visceral canina. Clin. Vet. 2006;62:32–38. [Google Scholar]
- Jansa S.A., Barker F.K., Voss R.S. The early diversification history of didelphid marsupials: a window into South America's “splendid isolation”. Evolution. 2014;68:684–695. doi: 10.1111/evo.12290. [DOI] [PubMed] [Google Scholar]
- Jansen A.M., Roque A.L.R. Domestic and Wild Mammalian Reservoirs. In: Telleria J., Tibyarenc M., editors. American Trypanosomiasis – Chagas Disease. Elsevier; London: 2010. pp. 249–276. [Google Scholar]
- Jones G., Teeling E.C. The evolution of echolocation in bats. Trends Ecol. Evol. 2006;21:149–156. doi: 10.1016/j.tree.2006.01.001. [DOI] [PubMed] [Google Scholar]
- Jones K.E., Patel N.G., Levy M.A., Storeygard A., Balk D., Gittleman J.L. Global trends in emerging infectious diseases. Nature. 2008;451:990–993. doi: 10.1038/nature06536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr S.F., McHugh C.P., Dronen N.O., Jr. Leishmaniasis in Texas: prevalence and seasonal transmission of Leishmania mexicana in Neotoma micropus. Am. J. Trop. Med. Hyg. 1995;53:73–77. [PubMed] [Google Scholar]
- Kerr S.F., Emmons L.H., Melby P.C., Liu C., Perez L.E., Villegas M. Leishmania amazonensis infections in Oryzomys acritus and Oryzomys nitidus from Bolivia. Am. J. Trop. Med. Hyg. 2006;75:1069–1073. [PubMed] [Google Scholar]
- Kreutzer R.D., Corredor A., Grimaldi G., Jr., Grogl M., Rowton E.D., Young D.G. Characterization of Leishmania colombiensis sp. n (Kinetoplastida: trypanosomatidae), a new parasite infecting humans, animals, and phlebotomine sand flies in Colombia and Panama. Am. J. Trop. Med. Hyg. 1991;44:662–675. doi: 10.4269/ajtmh.1991.44.662. [DOI] [PubMed] [Google Scholar]
- Lachaud L., Machergui-Hammami S., Chabbert E., Dereure J., Dedet J.P., Bastien P. Comparison of six PCR methods using peripheral blood for detection of canine visceral leishmaniasis. J. Clin. Microbiol. 2002;40:210–215. doi: 10.1128/JCM.40.1.210-215.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lainson R., Rangel E.F. Lutzomyia longipalpis and the eco-epidemiology of American visceral leishmaniasis, with particular reference to Brazil: a review. Mem. Inst. Oswaldo Cruz. 2005;100:811–827. doi: 10.1590/s0074-02762005000800001. [DOI] [PubMed] [Google Scholar]
- Lainson R., Shaw J.J. Leishmania (Viannia) naiffi sp. n., a parasite of the armadillo, Dasypus novemcinctus in Amazonian Brazil. Ann. Parasitol. Hum. Comp. 1989;64:3–9. doi: 10.1051/parasite/19896413. [DOI] [PubMed] [Google Scholar]
- Lainson R., Strangways-Dixon J. The epidemiology of dermal Leishmaniasis in British Honduras. Trans. R. Soc. Trop. Med. Hyg. 1964;58:136–153. doi: 10.1016/0035-9203(64)90003-3. [DOI] [PubMed] [Google Scholar]
- Lainson R., Shaw J.J., Ward R.D., Ready P.D., Naiff R.D. Leishmaniasis in Brazil: XIII. Isolation of Leishmania from armadillos (Dasypus novemcinctus), and observations on the epidemiology of cutaneous leishmaniasis in north Para State. Trans. R. Soc. Trop. Med. Hyg. 1979;73:239–242. doi: 10.1016/0035-9203(79)90225-6. [DOI] [PubMed] [Google Scholar]
- Lainson R., Shaw J.J., Povoa M. The importance of edentates (sloths and anteaters) as primary reservoirs of Leishmania braziliensis guyanensis, causative agent of “pianbois” in north Brazil. Trans. R. Soc. Trop. Med. Hyg. 1981;75:611–612. doi: 10.1016/0035-9203(81)90222-4. [DOI] [PubMed] [Google Scholar]
- Lainson R., Shaw J.J., Ready P.D., Miles M.A., Povoa M. Leishmaniasis in Brazil: XVI. Isolation and identification of Leishmania species from sandflies, wild mammals and man in north Para State, with particular reference to L. braziliensis guyanensis causative agent of “pian-bois. Trans. R. Soc. Trop. Med. Hyg. 1981;75:530–536. doi: 10.1016/0035-9203(81)90192-9. [DOI] [PubMed] [Google Scholar]
- Lainson R., Braga R.R., de Souza A.A., Povoa M.M., Ishikawa E.A., Silveira F.T. Leishmania (Viannia) shawi sp. n., a parasite of monkeys, sloths and procyonids in Amazonian Brazil. Ann. Parasitol. Hum. Comp. 1989;64:200–207. doi: 10.1051/parasite/1989643200. [DOI] [PubMed] [Google Scholar]
- Lainson R., Dye C., Shaw J.J., Macdonald D.W., Courtenay O., Souza A.A. Amazonian visceral leishmaniasis–distribution of the vector Lutzomyia longipalpis (Lutz & Neiva) in relation to the fox Cerdocyon thous (linn.) and the efficiency of this reservoir host as a source of infection. Mem. Inst. Oswaldo Cruz. 1990;85:135–137. doi: 10.1590/s0074-02761990000100027. [DOI] [PubMed] [Google Scholar]
- Lainson R., Ishikawa E.A., Silveira F.T. American visceral leishmaniasis: wild animal hosts. Trans. R. Soc. Trop. Med. Hyg. 2002;96:630–631. doi: 10.1016/s0035-9203(02)90333-0. [DOI] [PubMed] [Google Scholar]
- Lampo M., Feliciangeli M.D., Marquez L.M., Bastidas C., Lau P. A possible role of bats as a blood source for the Leishmania vector Lutzomyia longipalpis (Diptera: psychodidae) Am. J. Trop. Med. Hyg. 2000;62:718–719. doi: 10.4269/ajtmh.2000.62.718. [DOI] [PubMed] [Google Scholar]
- Le Pont F., Mouchet J., Desjeux P. Leishmaniasis in Bolivia. VII. Infection of sentinel porcupines (Coendou prehensilis, L.) by Leishmania (Le.) chagasi. Mem. Inst. Oswaldo Cruz. 1989;84:575. doi: 10.1590/s0074-02761989000400017. [DOI] [PubMed] [Google Scholar]
- Lima B.S., Dantas-Torres F., de Carvalho M.R., Marinho-Junior J.F., de Almeida E.L., Brito M.E. Small mammals as hosts of Leishmania spp. in a highly endemic area for zoonotic leishmaniasis in North-Eastern Brazil. Trans. R. Soc. Trop. Med. Hyg. 2013;107:592–597. doi: 10.1093/trstmh/trt062. [DOI] [PubMed] [Google Scholar]
- Lima L., Silva F.M., Neves L., Attias M., Takata C.S., Campaner M. Evolutionary insights from bat trypanosomes: morphological, developmental and phylogenetic evidence of a new species, Trypanosoma (Schizotrypanum) erneyi sp. nov., in African bats closely related to Trypanosoma (Schizotrypanum) cruzi and allied species. Protist. 2012;163:856–872. doi: 10.1016/j.protis.2011.12.003. [DOI] [PubMed] [Google Scholar]
- Lima V.M., Fattori K.R., Michelin A.F., Nogueira F.S., Souza L.O. Evidence of Leishmania spp. antibodies and DNA in bush dogs (Speothos venaticus) in Brazil. J. Zoo Wildl. Med. 2009;40:91–94. doi: 10.1638/2008-0043.1. [DOI] [PubMed] [Google Scholar]
- Lima V.M., Santiago M.E., Sanches L.C., Lima B.D. Molecular diagnosis of Leishmania amazonensis in a captive spider monkey in Bauru, Sao Paulo, Brazil. J. Zoo Wildl. Med. 2012;43:943–945. doi: 10.1638/2012-0059R1.1. [DOI] [PubMed] [Google Scholar]
- Lisboa C.V., Mangia R.H., Luz S.L., Kluczkovski A., Jr., Ferreira L.F., Ribeiro C.T. Stable infection of primates with Trypanosoma cruzi I and II. Parasitology. 2006;133:603–611. doi: 10.1017/S0031182006000722. [DOI] [PubMed] [Google Scholar]
- Llanos-Cuentas E.A., Roncal N., Villaseca P., Paz L., Ogusuku E., Perez J.E. Natural infections of Leishmania peruviana in animals in the Peruvian Andes. Trans. R. Soc. Trop. Med. Hyg. 1999;93:15–20. doi: 10.1016/s0035-9203(99)90163-3. [DOI] [PubMed] [Google Scholar]
- Lujan R., Chapman W.L., Jr., Hanson W.L., Dennis V.A. Leishmania braziliensis: development of primary and satellite lesions in the experimentally infected owl monkey, Aotus trivirgatus. Exp. Parasitol. 1986;61:348–358. doi: 10.1016/0014-4894(86)90190-6. [DOI] [PubMed] [Google Scholar]
- Luppi M.M., Malta M.C., Silva T.M., Silva F.L., Motta R.O., Miranda I. Visceral leishmaniasis in captive wild canids in Brazil. Vet. Parasitol. 2008;155:146–151. doi: 10.1016/j.vetpar.2008.04.024. [DOI] [PubMed] [Google Scholar]
- Machado M.I., Milder R.V., Pacheco R.S., Silva M., Braga R.R., Lainson R. Naturally acquired infections with Leishmania enriettii Muniz and Medina 1948 in guinea-pigs from São Paulo, Brazil. Parasitology. 1994;109(Pt 2):135–138. doi: 10.1017/s0031182000076241. [DOI] [PubMed] [Google Scholar]
- Madeira M.F., Figueiredo F.B., Pinto A.G., Nascimento L.D., Furtado M., Mouta-Confort E. Parasitological diagnosis of canine visceral leishmaniasis: is intact skin a good target? Res. Vet. Sci. 2009;87:260–262. doi: 10.1016/j.rvsc.2009.03.008. [DOI] [PubMed] [Google Scholar]
- Malta M.C., Tinoco H.P., Xavier M.N., Vieira A.L., Costa E.A., Santos R.L. Naturally acquired visceral leishmaniasis in non-human primates in Brazil. Vet. Parasitol. 2010;169:193–197. doi: 10.1016/j.vetpar.2009.12.016. [DOI] [PubMed] [Google Scholar]
- Mancianti F., Falcone M.L., Giannelli C., Poli A. Comparison between an enzyme-linked immunosorbent assay using a detergent-soluble Leishmania infantum antigen and indirect immunofluorescence for the diagnosis of canine leishmaniosis. Vet. Parasitol. 1995;59:13–21. doi: 10.1016/0304-4017(94)00738-x. [DOI] [PubMed] [Google Scholar]
- Marcondes M., Biondo A.W., Gomes A.A., Silva A.R., Vieira R.F., Camacho A.A. Validation of a Leishmania infantum ELISA rapid test for serological diagnosis of Leishmania chagasi in dogs. Vet. Parasitol. 2011;175:15–19. doi: 10.1016/j.vetpar.2010.09.036. [DOI] [PubMed] [Google Scholar]
- McHugh C.P., Thies M.L., Melby P.C., Yantis L.D., Jr., Raymond R.W., Villegas M.D. Short report: a disseminated infection of Leishmania mexicana in an eastern woodrat, Neotoma floridana, collected in Texas. Am. J. Trop. Med. Hyg. 2003;69:470–472. [PubMed] [Google Scholar]
- Mendonca M.G., de Brito M.E., Rodrigues E.H., Bandeira V., Jardim M.L., Abath F.G. Persistence of leishmania parasites in scars after clinical cure of American cutaneous leishmaniasis: is there a sterile cure? J. Infect. Dis. 2004;189:1018–1023. doi: 10.1086/382135. [DOI] [PubMed] [Google Scholar]
- Mettler M., Grimm F., Capelli G., Camp H., Deplazes P. Evaluation of enzyme-linked immunosorbent assays, an immunofluorescent-antibody test, and two rapid tests (immunochromatographic-dipstick and gel tests) for serological diagnosis of symptomatic and asymptomatic Leishmania infections in dogs. J. Clin. Microbiol. 2005;43:5515–5519. doi: 10.1128/JCM.43.11.5515-5519.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E., Huppert A. The effects of host diversity on vector-borne disease: the conditions under which diversity will amplify or dilute the disease risk. PLoS ONE. 2013;8:e80279. doi: 10.1371/journal.pone.0080279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills J.N., Childs J.E. Ecologic studies of rodent reservoirs: their relevance for human health. Emerg. Infect. Dis. 1998;4:529–537. doi: 10.3201/eid0404.980403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimori T., Grimaldi G., Jr., Kreutzer R.D., Gomez E.A., Mahon-Pratt D., Tesh R.B. Identification, using isoenzyme electrophoresis and monoclonal antibodies, of Leishmania isolated from humans and wild animals of Ecuador. Am. J. Trop. Med. Hyg. 1989;40:154–158. doi: 10.4269/ajtmh.1989.40.154. [DOI] [PubMed] [Google Scholar]
- Miranda F., Costa A.M. Xenarthra. In: Cubas Z.S., Silva J.C.R., Catão-Dias J.L., editors. Tratado de Animais Selvagens. 2006. pp. 402–414. Roca, São Paulo. [Google Scholar]
- Moller-Krull M., Delsuc F., Churakov G., Marker C., Superina M., Brosius J. Retroposed elements and their flanking regions resolve the evolutionary history of xenarthran mammals (armadillos, anteaters, and sloths) Mol. Biol. Evol. 2007;24:2573–2582. doi: 10.1093/molbev/msm201. [DOI] [PubMed] [Google Scholar]
- Naiff R.D., Freitas R.A., Naiff M.F., Arias J.R., Barrett T.V., Momen H. Epidemiological and nosological aspects of Leishmania naiffi Lainson & Shaw, 1989. Mem. Inst. Oswaldo Cruz. 1991;86:317–321. doi: 10.1590/s0074-02761991000300006. [DOI] [PubMed] [Google Scholar]
- Nery Guimarães F. Comportamento da Leishmania braziliensis Vianna, 1911 em hamsters (Cricetus [Mesocricetus] auratus) Hospital. 1951;40:25–46. [PubMed] [Google Scholar]
- Noireau F., Diosque P., Jansen A.M. Trypanosoma cruzi: adaptation to its vectors and its hosts. Vet. Res. 2009;40:26. doi: 10.1051/vetres/2009009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunes C.M., Lima V.M., Paula H.B., Perri S.H., Andrade A.M., Dias F.E. Dog culling and replacement in an area endemic for visceral leishmaniasis in Brazil. Vet. Parasitol. 2008;153:19–23. doi: 10.1016/j.vetpar.2008.01.005. [DOI] [PubMed] [Google Scholar]
- Olifiers N., Gentile R., Fiszon J.T. Relation between small-mammal species composition and anthropic variables in the Brazilian Atlantic Forest. Braz. J. Biol. 2005;65:495–501. doi: 10.1590/s1519-69842005000300015. [DOI] [PubMed] [Google Scholar]
- Oliveira F.S., Pirmez C., Pires M.Q., Brazil R.P., Pacheco R.S. PCR-based diagnosis for detection of Leishmania in skin and blood of rodents from an endemic area of cutaneous and visceral leishmaniasis in Brazil. Vet. Parasitol. 2005;129:219–227. doi: 10.1016/j.vetpar.2005.01.005. [DOI] [PubMed] [Google Scholar]
- Pajot F.X., Le Pont F., Gentile B., Besnard R. Epidemiology of leishmaniasis in French Guiana. Trans. R. Soc. Trop. Med. Hyg. 1982;76:112–113. doi: 10.1016/0035-9203(82)90033-5. [DOI] [PubMed] [Google Scholar]
- Palatnik-de-Sousa C.B., Day M.J. One Health: the global challenge of epidemic and endemic leishmaniasis. Parasit. Vectors. 2011;4:197. doi: 10.1186/1756-3305-4-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennisi M.G., Hartmann K., Lloret A., Addie D., Belak S., Boucraut-Baralon C. Leishmaniosis in cats: ABCD guidelines on prevention and management. J. Feline Med. Surg. 2013;15:638–642. doi: 10.1177/1098612X13489229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson N.E., Vexemat J.A., Rosa A.C.O.C., Lago P.R.L. Isolation of Leishmania (Viannia) braziliensis from the rodent Nectomys squamipes captured in Bahia, Brazil. Mem. Inst. Oswaldo Cruz. 1988;83(S1):28. [Google Scholar]
- Pung O.J., Hulsebos L.H., Kuhn R.E. Experimental American leishmaniasis and Chagas’ disease in the Brazilian squirrel monkey: cross immunity and electrocardiographic studies of monkeys infected with Leishmania braziliensis and Trypanosoma cruzi. Int. J. Parasitol. 1988;18:1053–1059. doi: 10.1016/0020-7519(88)90075-6. [DOI] [PubMed] [Google Scholar]
- Quaresma P.F., Rego F.D., Botelho H.A., da Silva S.R., Moura Junior A.J., Teixeira Neto R.G. Wild, synanthropic and domestic hosts of Leishmania in an endemic area of cutaneous leishmaniasis in Minas Gerais State, Brazil. Trans. R. Soc. Trop. Med. Hyg. 2011;105:579–585. doi: 10.1016/j.trstmh.2011.07.005. [DOI] [PubMed] [Google Scholar]
- Quinnell R.J., Courtenay O. Transmission, reservoir hosts and control of zoonotic visceral leishmaniasis. Parasitology. 2009;136:1915–1934. doi: 10.1017/S0031182009991156. [DOI] [PubMed] [Google Scholar]
- Quintal A.P., Ribeiro E.S., Rodrigues F.P., Rocha F.S., Floeter-Winter L.M., Nunes C.M. Leishmania spp. in Didelphis albiventris and Micoureus paraguayanus (Didelphimorphia: didelphidae) of Brazil. Vet. Parasitol. 2011;176:112–119. doi: 10.1016/j.vetpar.2010.11.011. [DOI] [PubMed] [Google Scholar]
- Raymond R.W., McHugh C.P., Witt L.R., Kerr S.F. Temporal and spatial distribution of Leishmania mexicana infections in a population of Neotoma micropus. Mem. Inst. Oswaldo Cruz. 2003;98:171–180. doi: 10.1590/s0074-02762003000200002. [DOI] [PubMed] [Google Scholar]
- Rocha F.L., Roque A.L., de Lima J.S., Cheida C.C., Lemos F.G., de Azevedo F.C. Trypanosoma cruzi infection in neotropical wild carnivores (Mammalia: carnivora): at the top of the T. cruzi transmission chain. PLoS ONE. 2013;8:e67463. doi: 10.1371/journal.pone.0067463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha N.M., Melo M.N., Baba E.H., Dias M., Michalick M.S., Da Costa C.A. Leishmania braziliensis braziliensis isolated from Akodon arviculoides captured in Caratinga, Minas Gerais, Brazil. Trans. R. Soc. Trop. Med. Hyg. 1988;82:68. [PubMed] [Google Scholar]
- Roque A.L., Cupolillo E., Marchevsky R.S., Jansen A.M. Thrichomys laurentius (Rodentia; Echimyidae) as a putative reservoir of Leishmania infantum and L. braziliensis: patterns of experimental infection. PLoS Negl. Trop. Dis. 2010;4:e589. doi: 10.1371/journal.pntd.0000589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotureau B. Ecology of the leishmania species in the Guianan ecoregion complex. Am. J. Trop. Med. Hyg. 2006;74:81–96. [PubMed] [Google Scholar]
- Salam M.A., Mondal D., Kabir M., Ekram A.R., Haque R. PCR for diagnosis and assessment of cure in kala-azar patients in Bangladesh. Acta Trop. 2010;113:52–55. doi: 10.1016/j.actatropica.2009.09.005. [DOI] [PubMed] [Google Scholar]
- Santiago M.E., Vasconcelos R.O., Fattori K.R., Munari D.P., Michelin A.F., Lima V.M. An investigation of Leishmania spp. in Didelphis spp. from urban and peri-urban areas in Bauru (Sao Paulo, Brazil) Vet. Parasitol. 2007;150:283–290. doi: 10.1016/j.vetpar.2007.09.026. [DOI] [PubMed] [Google Scholar]
- Savani E.S., de Almeida M.F., de Oliveira Camargo M.C., D'Auria S.R., Silva M.M., de Oliveira M.L. Detection of Leishmania (Leishmania) amazonensis and Leishmania (Leishmania) infantum chagasi in Brazilian bats. Vet. Parasitol. 2010;168:5–10. doi: 10.1016/j.vetpar.2009.10.019. [DOI] [PubMed] [Google Scholar]
- Schonian G., Nasereddin A., Dinse N., Schweynoch C., Schallig H.D., Presber W. PCR diagnosis and characterization of Leishmania in local and imported clinical samples. Diagn. Microbiol. Infect. Dis. 2003;47:349–358. doi: 10.1016/s0732-8893(03)00093-2. [DOI] [PubMed] [Google Scholar]
- Shapiro J.T., da Costa Lima Junior M.S., Dorval M.E., de Oliveira F.A., Cepa Matos M.F., Bordignon M.O. First record of Leishmania braziliensis presence detected in bats, Mato Grosso do Sul, southwest Brazil. Acta Trop. 2013;128:171–174. doi: 10.1016/j.actatropica.2013.07.004. [DOI] [PubMed] [Google Scholar]
- Shaw J. The leishmaniases–survival and expansion in a changing world. A mini-review. Mem. Inst. Oswaldo Cruz. 2007;102:541–547. doi: 10.1590/s0074-02762007000500001. [DOI] [PubMed] [Google Scholar]
- Sherlock I.A. Ecological interactions of visceral leishmaniasis in the state of Bahia, Brazil. Mem. Inst. Oswaldo Cruz. 1996;91:671–683. doi: 10.1590/s0074-02761996000600003. [DOI] [PubMed] [Google Scholar]
- Sherlock I.A., Miranda J.C., Sadigursky M., Grimaldi G., Jr. Natural infection of the opossum Didelphis albiventris (Marsupialia, Didelphidae) with Leishmania donovani, in Brazil. Mem. Inst. Oswaldo Cruz. 1984;79:511. doi: 10.1590/s0074-02761984000400020. [DOI] [PubMed] [Google Scholar]
- Silva D.A., Madeira M.F., Barbosa Filho C.J., Schubach E.Y., Barros J.H., Figueiredo F.B. Leishmania (Leishmania) hertigi in a porcupine (Coendou sp.) found in Brasilia, Federal District, Brazil. Rev. Bras. Parasitol. Vet. 2013;22:297–299. doi: 10.1590/S1984-29612013005000014. [DOI] [PubMed] [Google Scholar]
- Silva E.S., Pirmez C., Gontijo C.M., Fernandes O., Brazil R.P. Visceral leishmaniasis in the crab-eating fox (Cerdocyon thous) in south-east Brazil. Vet. Rec. 2000;147:421–422. doi: 10.1136/vr.147.15.421. [DOI] [PubMed] [Google Scholar]
- Silva E.S., Gontijo C.M., Melo M.N. Contribution of molecular techniques to the epidemiology of neotropical Leishmania species. Trends Parasitol. 2005;21:550–552. doi: 10.1016/j.pt.2005.09.008. [DOI] [PubMed] [Google Scholar]
- Silva J.C.R., Adania C.H. Carnivora – felidae (Onça, Suçuarana, Jaguatirica, Gato-do-mato) In: Cubas Z.S., Silva J.C.R., Catão-Dias J.L., editors. Tratado de Animais Selvagens. 2007. pp. 505–546. Roca, São Paulo. [Google Scholar]
- Silveira F.T., Lainson R., Shaw J.J., Braga R.R., Ishikawa E.E., Souza A.A. Cutaneous leishmaniasis in Amazonia: isolation of Leishmania (Viannia) lainsoni from the rodent Agouti paca (Rodentia: dasyproctidae), in the state of Para, Brazil. Rev. Inst. Med. Trop. Sao Paulo. 1991;33:18–22. doi: 10.1590/s0036-46651991000100004. [DOI] [PubMed] [Google Scholar]
- Souza N.P., Almeida A.B., Freitas T.P., Paz R.C., Dutra V., Nakazato L. Leishmania (Leishmania) infantum chagasi in wild canids kept in captivity in the State of Mato Grosso. Rev. Soc. Bras. Med. Trop. 2010;43:333–335. doi: 10.1590/s0037-86822010000300024. [DOI] [PubMed] [Google Scholar]
- Telleria J., Bosseno M.F., Tarifa T., Buitrago R., Martinez E., Torrez M. Putative reservoirs of Leishmania amazonensis in a Sub-Andean focus of Bolivia identified by kDNA-polymerase chain reaction. Mem. Inst. Oswaldo Cruz. 1999;94:5–6. doi: 10.1590/s0074-02761999000100002. [DOI] [PubMed] [Google Scholar]
- Thomaz-Soccol V., Lanotte G., Rioux J.A., Pratlong F., Martini-Dumas A., Serres E. Monophyletic origin of the genus Leishmania Ross, 1903. Ann. Parasitol. Hum. Comp. 1993;68:107–108. [PubMed] [Google Scholar]
- Travi B.L., Jaramillo C., Montoya J., Segura I., Zea A., Goncalves A. Didelphis marsupialis, an important reservoir of Trypanosoma (Schizotrypanum) cruzi and Leishmania (Leishmania) chagasi in Colombia. Am. J. Trop. Med. Hyg. 1994;50:557–565. doi: 10.4269/ajtmh.1994.50.557. [DOI] [PubMed] [Google Scholar]
- Travi B.L., Osorio Y., Becerra M.T., Adler G.H. Dynamics of Leishmania chagasi infection in small mammals of the undisturbed and degraded tropical dry forests of northern Colombia. Trans. R. Soc. Trop. Med. Hyg. 1998;92:275–278. doi: 10.1016/s0035-9203(98)91009-4. [DOI] [PubMed] [Google Scholar]
- Travi B.L., Osorio Y., Guarin N., Cadena H. Leishmania (Leishmania) chagasi: clinical and parasitological observations in experimentally infected Didelphis marsupialis, reservoir of New World visceral leishmaniasis. Exp. Parasitol. 1998;88:73–75. doi: 10.1006/expr.1998.4214. [DOI] [PubMed] [Google Scholar]
- Travi B.L., Arteaga L.T., Leon A.P., Adler G.H. Susceptibility of spiny rats (Proechimys semispinosus) to Leishmania (Viannia) panamensis and Leishmania (Leishmania) chagasi. Mem. Inst. Oswaldo Cruz. 2002;97:887–892. doi: 10.1590/s0074-02762002000600025. [DOI] [PubMed] [Google Scholar]
- Troncarelli M.Z., Camargo J.B., Machado J.G., Lucheis S.B., Langoni H. Leishmania spp. and/or Trypanosoma cruzi diagnosis in dogs from endemic and nonendemic areas for canine visceral leishmaniasis. Vet. Parasitol. 2009;164:118–123. doi: 10.1016/j.vetpar.2009.06.027. [DOI] [PubMed] [Google Scholar]
- Van Wynsberghe N.R., Canto-Lara S.B., Mian-Centeno A.G., Itza-Ortiz M.F., Andrade-Narvaez F.J. Retention of Leishmania (Leishmania) mexicana in naturally infected rodents from the State of Campeche, Mexico. Mem. Inst. Oswaldo Cruz. 2000;95:595–600. doi: 10.1590/s0074-02762000000500001. [DOI] [PubMed] [Google Scholar]
- Van Wynsberghe N.R., Canto-Lara S.B., Sosa-Bibiano E.I., Rivero-Cardenas N.A., Andrade-Narvaez F.J. Comparison of small mammal prevalence of Leishmania (Leishmania) mexicana in five foci of cutaneous leishmaniasis in the State of Campeche, Mexico. Rev. Inst. Med. Trop. Sao Paulo. 2009;51:87–94. doi: 10.1590/s0036-46652009000200006. [DOI] [PubMed] [Google Scholar]
- Vasconcelos I.A., Vasconcelos A.W., Fe Filho N.M., Queiroz R.G., Santana E.W., Bozza M. The identity of Leishmania isolated from sand flies and vertebrate hosts in a major focus of cutaneous leishmaniasis in Baturité, northeastern Brazil. Am. J. Trop. Med. Hyg. 1994;50:158–164. doi: 10.4269/ajtmh.1994.50.158. [DOI] [PubMed] [Google Scholar]
- Verona C.E.S., Pissinatti A. Primatas do novo mundo (Sagui, Macaco-prego, Macaco-aranha, Bugio) In: Cubas Z.S., Silva J.C.R., Catão-Dias J.L., editors. Tratado de Animais Selvagens. 2007. pp. 358–377. Roca, São Paulo. [Google Scholar]
- Vouldoukis I., Ogunkolade W., Strazielle L., Ploton I., Monjour L. Susceptibility of Cebus nigrivittatus to Leishmania infantum. J. Parasitol. 1986;72:472–473. [PubMed] [Google Scholar]
- WHO - World Health Organization, 1990. Control of the leishmaniasis. Technical report series 793. [PubMed]
- Wilson D.E., Reeder D.M. Johns Hopkins University Press; Baltimore, Maryland: 2005. Mammal Species of the World: A Taxonomic and Geographic Reference. [Google Scholar]
- Woolhouse M.E., Dye C., Etard J.F., Smith T., Charlwood J.D., Garnett G.P. Heterogeneities in the transmission of infectious agents: implications for the design of control programs. Proc. Natl Acad. Sci. U.S.A. 1997;94:338–342. doi: 10.1073/pnas.94.1.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolhouse M.E., Taylor L.H., Haydon D.T. Population biology of multihost pathogens. Science. 2001;292:1109–1112. doi: 10.1126/science.1059026. [DOI] [PubMed] [Google Scholar]
- Zeledon R., McPherson B., Ponce C. Isolation of Leishmania braziliensis from a wild rodent in Costa Rica. Am. J. Trop. Med. Hyg. 1977;26:1044–1045. doi: 10.4269/ajtmh.1977.26.1044. [DOI] [PubMed] [Google Scholar]


