Abstract
Objective
This study aims to develop a conceptual model of patient-defined SDM, and understand what leads patients to label a specific, decision-making process as shared.
Methods
Qualitative interviews were conducted with 23 primary care patients following a recent appointment. Patients were asked about the meaning of SDM and about specific decisions that they labeled as shared. Interviews were coded using qualitative content analysis.
Results
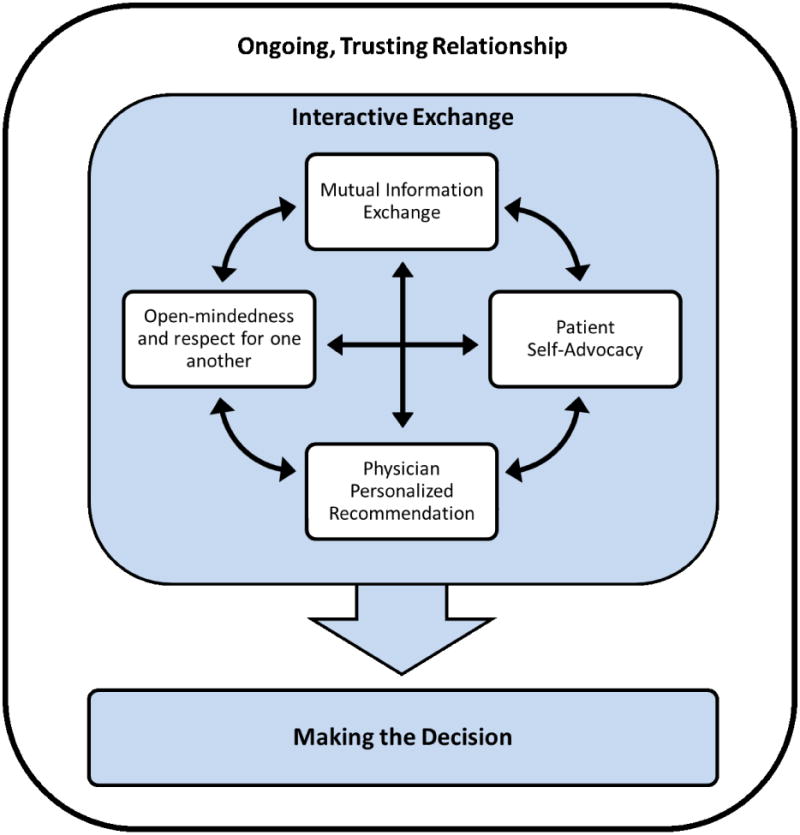
Patients' conceptual definition of SDM included four components of an interactive exchange prior to making the decision: both doctor and patient share information, both are open-minded and respectful, patient self-advocacy, and a personalized physician recommendation. Additionally, a long-term trusting relationship helps foster SDM. In contrast, when asked about a specific decision labeled as shared, patients described a range of interactions with the only commonality being that the two parties came to a mutually agreed-upon decision.
Conclusion
There is no one-size-fits all process that leads patients to label a decision as shared. Rather, the outcome of “agreement” may be more important than the actual decision-making process for patients to label a decision as shared.
Practice Implications
Studies are needed to better understand how longitudinal communication between patient and physicians and patient self-advocacy behaviors affect patient perceptions of SDM.
1. Introduction
Shared decision making (SDM) has been suggested as an optimal approach to making health care decisions [1], initially on ethical grounds and increasingly as a means to improve patient outcomes [2-4]. Clinicians are now routinely encouraged to employ a SDM process with patients (e.g. [5 6]). Despite this increased advocacy and attention, what exactly constitutes a shared decision making process is not always clear.
Among the academic literature, the most commonly cited definition of SDM is that developed by Charles and colleagues [7 8]. This definition includes four key characteristics, all of which must be present to be considered a shared decision: both the patient and clinician are involved in all phases; both parties share information; both parties express treatment preferences; and agreement is reached [7 9]. But other definitions exist (e.g. [3 10]) and the most common way of measuring patient perceptions of SDM is using a modification of the Degner et al. (1997) Control Preferences Scale [11 12]. This scale asks patients to rate their role in making a specific decision among five options: (1) I made the final decision, (2) I made the final decision after seriously considering my doctor's opinion, (3) My doctor and I shared the responsibility for deciding, (4) My doctor made the final decision but seriously considered my opinion, and (5) My doctor made the final decision. Option 3, while typically considered a shared decision, does not shed any light on how the decision making process actually occurred.
Understanding patient perceptions of SDM is important as a recent review found only patient-self reports of SDM to consistently have been associated with patient outcomes [12]. Furthermore, previous studies have found that patient perceptions of shared decisions differ from both observer ratings [13-16], and physician perceptions of SDM [17 18]. We know of only two studies that have directly explored the meaning of SDM to patients [19 20]. While these studies highlighted important differences between patient perceptions of SDM and published definitions of SDM, they were not designed to understand what needs to have happened in a specific decision-making context for a patient to label it as shared. Thus, in order to attain the benefits of patient-perceived SDM in practice, we need to have a better understanding of specifically what it is that patients label as shared.
The aims of this qualitative study are to: (1) develop a conceptual model of patient-defined SDM, and (2) understand what leads patients to label a specific, decision-making process as shared on the modified Control Preference Scale.
2. Methods
2.1 Study setting and participant recruitment
Participants were recruited from an academic and safety net health system in Virginia. The health system's electronic scheduling system was queried to identify adults aged 50 to 75 years with a non-follow-up primary care visit in the general internal medicine or family medicine out-patient clinic scheduled in the next month. The electronic medical record was queried to identify who among those were due for colorectal cancer screening as this study is part of a larger project exploring how receipt of patient-defined SDM affected colorectal cancer screening use and thus some of the interview questions (not used in this analysis) pertained to communication about colorectal cancer screening. These patients were mailed a letter of study introduction two weeks prior to their scheduled appointment. Within one week after their appointment, patients who had not declined participation were contacted via telephone by the first author. At that time, eligibility was confirmed and among those eligible and agreeing to participate, verbal consent was obtained. Patients were identified and recruited in batches of 5 to 7 and initial data analysis was begun after each batch of interviews. Recruitment in batches continued until theoretical saturation was achieved (i.e. when no new themes were identified during initial analyses) [21]. The study was approved by the Virginia Commonwealth University Internal Review Board.
2.2 Data collection
Study participation entailed completion of one telephone interview lasting approximately 45 minutes. The interviews were conducted by the first author using a semi-structured interview guide. Participants were first asked to recall and describe any decisions made in their most recent primary care appointment. They were then asked to indicate how each decision was made using the modified Control Preferences Scale [11], and to describe what during the visit led them to perceive that the decision was made this way. Finally, participants were asked about the meaning of SDM more broadly and about their perceptions of the patient and physician responsibilities in a SDM process. All interviews were audio-recorded.
2.3 Data analysis
Prior to analysis, all audio-recordings were transcribed. A qualitative content analysis approach was used to analyze interview data [22]. Coding and analysis occurred concurrently with subsequent interviews and proceeded in three steps: immersion, reduction, and interpretation [22]. During immersion, audio-recordings were listened to and transcripts read several times to identify emerging themes. The reduction step consisted of creating initial codes, developing a coding scheme, and coding the interviews using ATLAS.ti. Coding consisted of both a priori and inductive codes. The first author developed a preliminary coding scheme early in the analysis process and, in discussion with the coauthor, revised it using an iterative process as new relevant themes arose. When no new themes were found with subsequent interviews, recruitment stopped. The interpretation step consisted of reorganizing the data into categories that helped address the research questions and draw conclusions.
3. Results
3.1 Sample characteristics
Across the batches of recruitment, a total of 60 patients were identified as potentially eligible via health system records. Twenty-one patients could not be reached at the telephone number listed in their medical record, 14 declined participation, and two were ineligible due to not attending their scheduled appointment. In total, 23 patients were interviewed (Table 1). Patient participants were primarily female (61%) and white (74%). The mean participant age was 63 years (SD = 10.4).
Table 1. Sample characteristics (n=23).
| Characteristic | n (%) unless noted |
|---|---|
| Age in years, mean (SD) | 61.5 (7.5) |
| Female | 14 (61%) |
| Race | |
| African American | 6 (26%) |
| White | 17 (74%) |
| Clinic* | |
| General internal medicine | 21 (91%) |
| Family medicine | 2 (9%) |
| No. of decisions made, median (range) | 1 (0-3) |
Clinic refers to the type of practice that the patient attended for their recent primary care appointment.
3.2 Patients' conceptual definition of shared decision making
When asked about the meaning of shared decision making in general, respondents described two key phases of SDM: (1) an interactive exchange and (2) making the decision (Figure). Additionally, a theme emerged that spanned across the phases of SDM: the need for a trusting relationship with their physician that extends beyond any single encounter.
Figure. Patients' conceptual definition of SDM.
3.2.1 Phase 1: An interactive exchange
All patients described SDM as a collaborative process in which both the patient and physician are active participants. Patients described four interdependent components that make up the interactive exchange: a mutual exchange of information; open-mindedness and respect for one another; patient self-advocacy; and the physician making a personalized recommendation.
Mutual exchange of information
Patients nearly unanimously brought up the importance of a mutual exchange of information including “input from both sides,” in which the patient shares any relevant concerns or problems and the physician shares medical and treatment information. Patients described specific roles for both themselves and for physicians in the exchange of information.
First, patients are responsible to describe their symptoms and health concerns to their physician, so that their physician had the basic knowledge to begin forming a recommendation. For example, one patient said, “They can't read your mind. If you don't go in on your visit and tell them everything that's going on for whatever your problem happens to be, they can't really help you.” Many patients brought up the concept of “honesty,” noting the importance of being completely open with their physician, even if the topic is uncomfortable in order to reach the best possible decision. One patient described this with, “You (need to) be honest with the doctor. Just like a priest. You can tell the doctor everything. And you should, because they cannot treat you to your best advantage if they don't know everything.”
Patients acknowledged that physicians also have the responsibility to share information. Specifically, according to patients, physicians should share any relevant medical information and treatment options, taking the time to clearly explain in language that is understandable to patients. One patient described this, saying that it is important, “that your doctor tell you what's going' on, explain your options to you.” Another described the importance of the physician taking the time, “to explain what I had, to explain the medication. So, I knew exactly what it was for, how to use it.”
Open-mindedness and respect for one another
Many patients specifically described open-mindedness and respect for one another as an important component of SDM. Patients were clear in their beliefs that both physicians and patients bring their own specific expertise to the interaction. Acknowledging the physician's medical expertise, patients stated that they should listen and be-open minded about what the physician says.
I have to be very open and honest to her and I also have to be open-minded enough that if she recommends something that's a little unusual that I really need to seriously consider that because I know she's doing what she feels is best for me.
Likewise, patients stated that physicians should also listen to patients as they have unique knowledge about their own body and symptoms. This takes the form of an interactive conversation rather than the physician simply providing medical information. Patients described two ways that they understood physicians to be listening to them. First, when a physician makes time to talk with a patient on a more personal level, this helps the patient to be assured that the physician sees them as an individual person with unique circumstances and needs. Patients desired to see this type of open-mindedness throughout the visit, not only during the discussion about the particular decision at hand.
I think they just have to be very open and not rush and talk so fast and talk in ‘doctor-ese’ that you don't understand them-that if they can just look at you and-like you're a person and not patient number 93.
Second, patients wanted physicians to respect the expertise that they bring to the visit. To do this, physicians should carefully listen to patients, solicit their thoughts and concerns, and take time to answer questions before forming a recommendation.
The doctor has the training and the knowledge and everything, but I feel that the doctor needs to listen to the patient, listen to what they're saying. The doctor sees you for half hour, 15 minute appointments or whatever… you live with yourself.
Patient self-advocacy
Patients described a responsibility to advocate for themselves throughout the SDM process. This may consist of asking clarifying questions, guiding the conversation if the physician gets off track, sharing opinions, and speaking up if there are hesitations or disagreements. As one patient stated, “If you have a doubt, talk about it. Be prepared with questions. If it's something serious, have your questions down. Don't be afraid.” Like open-mindedness and respect, patients described the importance of these self-advocacy behaviors not only during the decision-making process, but also extending to all parts of the visit. By engaging in this way, patients viewed themselves as actively contributing to the formation of the best possible decision.
Personalized physician recommendation
Most patients seemed to take it for granted that physicians should provide a recommendation for action, whether for treatment or non-treatment, during the discussion. However, they had specific thoughts about how these recommendations should be made. First, patients wanted to feel confident that these recommendations were based on the individual patient and their unique situation, rather than relying only on what the physician typically recommends. Thus, patients reported that physicians should explain the reasoning for the particular recommendation both in general and for the individual patient. For example, one patient said they'd like physicians to “explain the reason for a certain procedure or an appointment with a specialist or whatever. It's helpful to me, and I think it would be for most patients, to understand why something is being suggested.” Another said, “I don't want doctors telling me what's best for me without me knowing that they understand what's best for me from my point of view.” Additionally, the words that physicians use to make the recommendations to patients affect patients' perceptions of SDM. Patients stated that they want physicians to make suggestions or give options, not demands or ultimatums.
3.2.3 Phase 2: Making the decision
In addition to the collaborative exchange between the patient and physician, patients said that a decision is made that is in the best interest of the patient. Patients generally described one of two perspectives about how the decision was made. About half of the patients (n=11) described decision making as mutual between the patient and physician. One patient described the decision-making process with, “You and your doctor talk over all the options and come up with a shared thought about what's the right way to do it.” Another said, “Well, for me that means that we thoroughly talk about any issues, concerns that I have and he has, and that we come to some agreement around treatment or non-treatment or whatever we're going to do.”
The other half of patients (n=12), however, stated that ultimately the patient always decides. These patients acknowledged that the patient has to take final responsibility, even if they shared in the communication process leading to the decision. One patient said, “It's a collaborative thing, but I mean I clearly feel that it's my decision. I also assume that my doctors share that assumption… but yeah I'm the decision maker.” Another patient described the distinction between a shared process and the final decision with,
I'm thinking sharing, that's the way it should be. I mean they can give you their opinion, but it's something that you've got to live with. I mean, I know you're going to them because they went to school for many years or whatever, but ultimately it's still your life and your body.
3.2.3 Trusting relationship built over time
Patients also pointed to the importance of a strong rapport when describing SDM. Prominent among this was the need for the patient to trust that the physician knows them and understands their health care needs and preferences. As described by patients, the building of this trust is not confined to the communication around a particular decision itself, but is built over time and extends beyond a single visit. As one patient stated,
I think you just have to find a doctor you trust, not because he's the best doctor out there and somebody else recommended him. That's nice, but what's the sense of having the best doctor out there if you don't have trust in him and you can't talk to them, you know?
A trusting relationship allows for both patient and physician to feel comfortable throughout the collaborative exchange to speak up if they are uncomfortable, and for a high quality, personalized decision to be made.
3.3 Specific decision-making processes labeled by patients as shared
Patients were also asked to describe any decisions that they made in their recent primary care appointment. A total of 33 unique decisions were described across the 23 interviews. The reported number of decisions made during the visit ranged from zero to three, with a median of one decision per visit. The context of the decisions was varied (Table 2). Of these 33 decisions, 15 (45%) were reported as being shared decisions on the modified Control Preference Scale [11] (option 3), 13 (40%) were reported as patient-led decisions (option 1 or 2), and 5 (15%) physician-led decisions (option 4 or 5).
Table 2. Decisions reported by patient participants (n=33).
| n (%) | |
|---|---|
| Clinical Context | |
| Medication changes | 11 (33%) |
| Diagnostic tests | 9 (27%) |
| Referrals to specialist | 5 (15%) |
| Cancer screening | 4 (12%) |
| Other | 4 (12%) |
| Modified Control Preference Scale | |
| Patient-led (Option 1 or 2) | 13 (40%) |
| Shared (Option 3) | 15 (45%) |
| Physician-led (Option 4 or 5) | 5 (15%) |
Across the 15 decisions that patients labeled as shared, the communication patients reported as having occurred varied greatly, ranging from extremely short and simple to lengthy discussions. In all of these patient-labeled shared decisions, patients stated that they and the physician ultimately came to a mutually agreed upon decision. Among these patient-labeled shared decisions, many were described as a straightforward process in which the physician made a recommendation or the patient brought in a request and both parties simply agreed. In these cases, little communication exchange was described and none of the components of the interactive exchange phase of the patients' conceptual definition of SDM were fully met. Despite this lack of interaction, these patients all felt that they came to a mutually agreed upon decision and thus regarded the decision as being shared. Below are two examples of patient descriptions of a decision labeled as shared, with either the physician or patient making an initial recommendation followed by simple agreement:
She just said if I hadn't had [a bone density scan] in three years, and I said, “Oh, I know it'd been longer than three years.” She said, “Well then I think you should have one,” and I said, “Fine. That's fine with me.” So that's a shared… She didn't say to me, you have to have this. I mean, you know, we discussed it, and we both agreed. So that's shared.
Well, I just I brought it up. I had been in my local pharmacy a couple months ago and I saw they were offering [the shingles vaccine] there… I'd had two scary incidents with shingles over the course of the last 20 years. I wanted to-I'm very interested in getting that preventive vaccine so I don't have another outbreak of it…He said, ‘I'll be happy to write that prescription for you.’ I said, ‘Good, let's give it a shot.’…I wanted to get it and he thought I needed it so it was a pretty mutual decision.
In other cases labeled as shared, patients described interactions that began with a physician recommendation followed by patient questions or hesitation, but ultimately ending in agreement between both parties. Patient descriptions of these interactive exchanges more closely resembled the conceptual model of patient-defined SDM as described in the Figure. For example, one patient described a decision, labeled as shared, with the following:
He said, given your history, I might like to consider medication [to lower cholesterol]… I felt that, at this point, I really don't want to take another medicine. I would like to try other methods before even considering going on medication… He listened to what I felt, my point of view or whatever. It wasn't a snap judgment, ‘Okay, your cholesterol is up and you're going to go on medication, and that's that.’ He listened and after discussion, and I said that I was reluctant to take medication at this time. He agreed, ‘Okay, we can wait and see how the other methods are working.
Despite these differences in the extent of the discussion, the only commonality found across the 15 decisions that patients labeled as shared was that the patient and physician ultimately came to a mutually agreed upon decision.
4. Discussion and conclusions
4.1 Discussion
When asked about the meaning of SDM in general, patients describe an interactive communication process that is similar to the commonly used definition of SDM developed by Charles and colleagues (1997, 1999). In particular, patients described two phases: an interactive exchange and making a decision. While patients use slightly different terms to describe the interactive exchange (mutual sharing of information, open-mindedness and respect for one another, patient self-advocacy, and a personalized physician recommendation) the overall process is quite comparable. On the other hand, when asked to describe what led them to label a recent, specific decision as being shared, they described a variety of communication processes ranging from those that contained no interactive exchange to those that contain an interactive exchange similar to that which would be labeled as SDM using currently accepted definitions. Across the wide range of decisions processes that patients labeled as shared, the only common element was that the processes ended in a decision that was mutually agreed upon by the patient and physician. Furthermore, in the cases labeled as shared decisions where patients agreed quickly with the physician's recommendation, very little communication process at all was described. Thus, while patient conceptual definitions of SDM center around interactive communication processes, patient perceptions of having participated in a shared decision appear more related to the outcome of a mutually agreed upon patient-physician decision rather than any specific communication process that led to this agreement.
These findings have implications for both the measurement of SDM as well as intervention design. Results from our patient interviews indicate that SDM, when measured by instruments such as the modified Control Preference Scale, likely do not reflect the patient's engagement in an interactive communication process, but rather the extent to which the patient felt that the outcome was shared. Thus, if the purpose of a study is to understand the extent to which the patient was engaged in an interactive exchange with the physician, the modified Control Preference Scale may not be an appropriate tool.
Our findings also have implications for the measurement of SDM beyond a patient's perspective. In these interviews, patients described their own role in the information exchange and decision-making as being as active as or more active than the physician role. However, many of the most commonly used measurement tools for SDM (including the OPTION scale [23]) focus solely on physician behaviors and thus may be missing important aspects of the interaction. Furthermore, similar to other recent qualitative studies [19 20], our findings point to the importance of relational factors between the patient and physician on patient perceptions of SDM. Patients emphasized the importance of relational factors beyond the current visit and described the importance of a trusting rapport between the patient and physician that is built over time. Thus, findings from this study provide support for recent calls for measuring SDM as part of a larger interaction and relationship rather than those focused solely on one discussion specific to a current decision [24].
In interviews, patients spoke of the importance of advocating for oneself in order to fully participate in a SDM process. Thus there may be a need for interventions that encourage patient self-advocacy such as asking questions, speaking up when uncomfortable, or asking for a second opinion. Past studies have shown that when patients are more active in their consultations, physicians both share more information [25] and adopt a more patient-centered style of communication [26]. Interventions to promote patient participation and self-advocacy could include communication training for either the patient or the physician. Patient interventions might include communication training that builds skills on assertiveness and question-asking. Physician interventions could provide training around creating a trusting environment that would allow patients to feel comfortable speaking up.
There are several potential explanations for our finding that patient reports of SDM about a specific, recent decision seem to be more about the outcome of agreement than the communication process experienced. First, if patients have an expectation that they will talk respectfully with their physician and come to agreement on a plan, and this expectation is met, patients are not likely to consider the process that led to the accomplished goal. This makes sense in light of communication theory, such as Expectancy Violations Theory [27], which posits that when a person's expectations of the interaction are violated, their focus changes from the original purpose of the interaction (agreement on a treatment plan) to thinking about the source of the discrepancy (or the communication process itself). Thus, unless a patient's implicit expectation is violated with extremely poor or disrespectful communication, the patient is not likely to think about the communication process itself, but rather stay focused on the goals of the consultation. Second, it is plausible that the wording of the choices themselves, led patients to think of an outcome rather than a process. In these interviews we used the modified Control Preference Scale, which asks patients to respond to the following question: “When it came to making the decision about <the specific topic>, which of these would you say would best describe how the decision was made?” The option that represents SDM is, “My doctor and I shared responsibility for deciding.” “Shared” in this context may be more about shared agreement rather than a detailed collaborative (shared) process.
Our qualitative findings suggest that aspects of the patient-physician relationship may influence perceptions about SDM. The length of the relationship and the patient's trust may be particularly important. Additionally, there may be differences in how patients perceive and experience SDM by the clinical context of the decision and other aspects of the health care system. Thus, we recommend that larger, quantitative studies be conducted to confirm the model put forth in this paper and also explore for any differences in patient definitions of SDM by characteristics of the patient, physician, and health care system, context of the decision, and relationship between the patient and physician.
Our study should be considered in light of several limitations. The time between a patient's scheduled appointment and the interview may influence the patient's ability to accurately recall the discussion with their physician. We worked to minimize any potential impact on our findings by contacting patients within one week of their scheduled appointment, but future studies should consider the use of interviews immediately after the medical appointment in order to obtain real time perceptions of the discussions. Second, we sampled patients who had recently attended a non-follow up primary care appointment. Thus, this sample may represent patients who are more active in their healthcare and perceptions of SDM may differ for those who take a less active approach. Finally, all of the patients in this sample were between the ages of 50 and 75. There is evidence that patient preferences for SDM differ by age, with older patients preferring to be less active in medical decision making [28-30] [29-31], but it is not clear whether perceptions of SDM may also be influenced by age. Our study was not designed to explore for a possible cohort effect by age. Future studies may want to explore how these and other decision and patient characteristics (e.g., level of education) might affect how patients perceive SDM both conceptually and regarding a specific, recent decision.
4.2 Conclusion
Patient reports of making a shared decision have been linked with improved patient outcomes [12]. However in order to foster the communication linked with these outcomes in practice, a clear understanding of what leads a patient to label a decision as shared is needed. This study makes an important contribution to the SDM literature by focusing specifically on the patient perspective of SDM. While SDM is often advocated on ethical grounds as a means to improve patient autonomy, the voice of the patient is notably lacking in most studies. The results presented here help to bridge this gap and allow for a better understanding of how patients conceptually define SDM as well what leads them to label a decision as shared. Conceptually, patients describe a SDM process similar to accepted models of SDM in the literature, but with a greater emphasis on open-mindedness and relational factors that are influenced by a relationship built over time. However, in the context of a specific, recent primary care decision, when agreement is reached about the decision, patients may label even relatively simple interactions as being shared decisions. Thus, it seems there is no one-size-fits all process that leads patients to label a decision as being shared. Rather, the outcome of “agreement” may be more important than the actual decision making process used to reach that agreement when patients label a recent decision as shared.
4.3 Practice implications
Our findings support the need for a more holistic approach to studying shared decision-making. SDM likely extends beyond the confines of a single encounter. Thus, measurement instruments and rigorously designed studies are needed to better understand how the longitudinal communication between patient and physicians affects both patient perceptions of SDM and patient outcomes. Furthermore, patients perceive themselves as having an active and important role in SDM. Interventions focused on improving patient self-advocacy may serve to improve quality decision-making between patients and clinicians.
Acknowledgments
Dr. Shay is supported by a post-doctoral fellowship, University of Texas School of Public Health Cancer Education and Career Development Program (National Cancer Institute/NIH Grant R25 CA57712). Financial support for this study was provided by a grant from the National Institute on Aging (1F31AG040923-01) and developmental projects award from the Center for Health Communications Research at the University of Michigan (5P50CA101451-09). The funding agreement ensured the authors' independence in designing the study, interpreting the data, writing, and publishing the report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Weston WW. Informed and shared decision-making: the crux of patient-centred care. Canadian Medical Association journal. 2001;165(4):438–39. [PMC free article] [PubMed] [Google Scholar]
- 2.Schofield T, Elwyn G, Edwards A, et al. Shared decision making. Patient Educ Couns. 2003;50(3):229–30. doi: 10.1016/s0738-3991(03)00170-8. [DOI] [PubMed] [Google Scholar]
- 3.Towle A, Godolphin W, Greenhalgh T, et al. Framework for teaching and learning informed shared decision making. Bmj. 1999;319(7212):766–71. doi: 10.1136/bmj.319.7212.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joosten EA, DeFuentes-Merillas L, de Weert GH, et al. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother Psychosom. 2008;77(4):219–26. doi: 10.1159/000126073. published Online First: Epub Date. [DOI] [PubMed] [Google Scholar]
- 5.Epstein RM, Street RL. NIH Publication No 07-6225. Bethesda, MD: National Cancer Institute; 2007. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. [Google Scholar]
- 6.Sheridan S, Harris R, Woolf S. Shared decision making about screening and chemoprevention. a suggested approach from the U.S. Preventive Services Task Force. American Journal of Preventive Medicine. 2004;26(1):56–66. doi: 10.1016/j.amepre.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 7.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango) Social science medicine. 1997;44(5):681–92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 8.Makoul G, Clayman M. An integrative model of shared decision making in medical encounters. Patient education and counseling. 2006;60(3):301–12. doi: 10.1016/j.pec.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 9.Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49(5):651–61. doi: 10.1016/s0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- 10.Elwyn G, Laitner S, Coulter A, et al. Implementing shared decision making in the NHS. BMJ. 2010;341:c5146. doi: 10.1136/bmj.c5146. [DOI] [PubMed] [Google Scholar]
- 11.Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. The Canadian journal of nursing research = Revue canadienne de recherche en sciences infirmieres. 1997;29(3):21–43. [PubMed] [Google Scholar]
- 12.Shay LA, Lafata JE. Where is the evidence? A systematic review of shared decision-making and patient outcomes. Under Review. 2013 doi: 10.1177/0272989X14551638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kasper J, Heesen C, Kpke S, et al. Patients' and observers' perceptions of involvement differ. Validation study on inter-relating measures for shared decision making. PLoS ONE. 2011;6(10):e26255–e55. doi: 10.1371/journal.pone.0026255. published Online First: Epub Date. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burton D, Blundell N, Jones M, et al. Shared decision-making in cardiology: do patients want it and do doctors provide it? Patient education and counseling. 2010;80(2):173–79. doi: 10.1016/j.pec.2009.10.013. published Online First: Epub Date. [DOI] [PubMed] [Google Scholar]
- 15.Flocke S, Stange K, Cooper G, et al. Patient-rated importance and receipt of information for colorectal cancer screening. Cancer epidemiology, biomarkers prevention. 2011;20(10):2168–73. doi: 10.1158/1055-9965.epi-11-0281. published Online First: Epub Date. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wunderlich T, Cooper G, Divine G, et al. Inconsistencies in patient perceptions and observer ratings of shared decision making: The case of colorectal cancer screening; Miami Special Issue: AACH Conference 2009; Miami, USA. 2010. pp. 358–63. published Online First: Epub Date. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janz N, Wren P, Copeland L, et al. Patient-physician concordance: preferences, perceptions, and factors influencing the breast cancer surgical decision. Journal of clinical oncology. 2004;22(15):3091–98. doi: 10.1200/JCO.2004.09.069. [DOI] [PubMed] [Google Scholar]
- 18.Fiks AG, Hughes CC, Gafen A, et al. Contrasting parents' and pediatricians' perspectives on shared decision-making in ADHD. Pediatrics. 2011;127(1):e188–96. doi: 10.1542/peds.2010-1510. published Online First: Epub Date. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Entwistle V, Prior M, Skea ZC, et al. Involvement in treatment decision-making: its meaning to people with diabetes and implications for conceptualisation. Social science & medicine (1982) 2008;66(2):362–75. doi: 10.1016/j.socscimed.2007.09.001. published Online First: Epub Date. [DOI] [PubMed] [Google Scholar]
- 20.Peek ME, Quinn MT, Gorawara-Bhat R, et al. How is shared decision-making defined among African-Americans with diabetes? International Conference on Communication in Healthcare - ICCH 2007. 2008;72(3):450–58. doi: 10.1016/j.pec.2008.05.018. published Online First: Epub Date. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Corbin J, A S. Basics of qualitative research: Techniques and procedures for developing grounded theory. Thosand Oaks, CA: Sage; 2008. [Google Scholar]
- 22.Forman J, Damschroder L. Qualitative content analysis. In: Siminoff LA, Ja L, editors. Empirical methods for bioethics: A primer. New York, NY: JAI Press; 2008. pp. 39–62. [Google Scholar]
- 23.Elwyn G, Edwards A, Wensing M, et al. Shared decision making: developing the OPTION scale for measuring patient involvement. Qual Saf Health Care. 2003;12(2):93–9. doi: 10.1136/qhc.12.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matthias MS, Salyers MP, Frankel RM. Re-thinking shared decision-making: context matters. Patient Educ Couns. 2013;91(2):176–9. doi: 10.1016/j.pec.2013.01.006. published Online First: Epub Date. [DOI] [PubMed] [Google Scholar]
- 25.Cegala D, Street R, Clinch CR. The impact of patient participation on physicians' information provision during a primary care medical interview. Health communication. 2007;21(2):177–85. doi: 10.1080/10410230701307824. [DOI] [PubMed] [Google Scholar]
- 26.Cegala DJ, Post DM. The impact of patients' participation on physicians' patient-centered communication. Patient Educ Couns. 2009;77(2):202–8. doi: 10.1016/j.pec.2009.03.025. published Online First: Epub Date. [DOI] [PubMed] [Google Scholar]
- 27.Burgoon JK, Jones SB. Nonverbal Expectancy Violations: Model Elaboration and Application to Immediacy Behaviors. Communication Monographs. 1988;55:58–79. [Google Scholar]
- 28.Frosch DL, Kaplan RM. Shared decision making in clinical medicine: past research and future directions. American Journal of Preventive Medicine. 1999;17(4):285–94. doi: 10.1016/s0749-3797(99)00097-5. [DOI] [PubMed] [Google Scholar]
- 29.Jung H, Baerveldt C, Olesen F, et al. Patient characteristics as predictors of primary health care preferences: a systematic literature analysis. Health expectations. 2003;6(2):160–81. doi: 10.1046/j.1369-6513.2003.00221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levinson W, Kao A, Kuby A, et al. Not all patients want to participate in decision making. A national study of public preferences. Journal of general internal medicine. 2005;20(6):531–35. doi: 10.1111/j.1525-1497.2005.04101.x. published Online First: Epub Date. [DOI] [PMC free article] [PubMed] [Google Scholar]


