Abstract
Aims
Sudden cardiac death (SCD) is among the most common causes of death in western countries including Germany. Whereas risk stratification and primary prevention is still insufficient, we also lack accurate incidence estimates. Current estimates vary widely (18.6–128/100 000/year), but data on SCD incidence in Germany are missing. Depending on SCD definitions, death needs to occur between 1 and 24 h after the onset of symptoms.
Methods and results
In the district of Aurich (190 000 inhabitants, Lower Saxony, Germany), emergency medical service (EMS) is provided by a district government operated single carrier and two hospitals. To evaluate all EMS calls in this district from 2002 to 2009, we obtained EMS protocols, medical records, and death certificates for data analysis and adjudication of SCD. We defined SCD according to the definition of the World Health Organization, considering patients with cardiac arrest within ≤1 h after the onset of symptoms. We also required cardiopulmonary resuscitation being performed by EMS personnel.
The overall mortality rate in the district of Aurich (1060/100 000/year) corresponded well with the average mortality rate in Germany (1030/100 000/year). During the observation period, we adjudicated 1212 SCD cases, equivalent to an annual rate of 151 SCD cases (81 cases/100 000/year). Rates remained remarkably stable over time, and affected a considerable number of individuals of working age (32/100 000/year).
Conclusion
Consistent with prior reports, the SCD incidence in a district of Germany is substantial. Despite an elaborate EMS system and advanced medical care, SCD rates remain stable and necessitate improved, individualized risk stratification.
Keywords: Sudden cardiac death, Germany, Resuscitation, Emergency medical service, Epidemiology, Cardiac arrest
What's new?
We report for the first time a systematic and conservative assessment of incidence of established sudden cardiac death (SCD) in Germany resulting in 81 cases of SCD per 100 000 per year.
34% of SCD occur before age 65.
Incidence of established SCD remains stable over an 8 year observation period.
Analysis of standardized and homogeneous emergency medical protocols provide important data on the epidemiology of SCD.
The clinical problem of SCD needs to be studied on a population level to improve risk stratification beyond the current low ejection fraction recommendation.
Introduction
The World Health Organization (WHO) defines sudden cardiac death (SCD) as death due to cardiac causes within 1h of the onset of symptoms in a person with known or unknown cardiovascular disease.1–3 Beyond the WHO definition of SCD, several other definitions are commonly used in scientific studies. Examples include definitions by the European Society of Cardiology and the American Heart Association, which consider SCD as death resulting from abrupt loss of heart function within minutes after the onset of symptoms. In addition, timing and circumstances of death have to be unexpected, and a past medical history of cardiac diseases is not required.4 Recently, a more unified definition for SCD ascertainment in community-based cohort studies and scientific investigations conducted in the general population has been recommended. Thereby, established SCD is an unexpected death without obvious extracardiac cause, occurring with a rapid witnessed collapse, or if unwitnessed, occurring within 1 h after the onset of symptoms. A probable SCD is an unexpected death without obvious extracardiac cause that occurred within 24 h. In any situation, death should not occur in the setting of a prior terminal condition, such as a malignancy not in remission or end-stage chronic obstructive lung disease.2 The International Classification of Diseases [ICD (German version)] defines SCD as ‘cardiac death as described, excluding myocardial infarction or conduction disturbance’.5
Cardiovascular diseases—including SCD—are the leading causes of death in Germany;6 yet, the incidence rate of SCD in Germany remains unknown.7,8 Prior studies in other countries have reported a widely varying SCD incidence rate, ranging from 18.6 to 128 cases/100 000 inhabitants/year.9–18
Here, we assessed the population-based incidence rate of SCD in Germany, applying the WHO definition and the most recent recommendation of the United States National Heart Lung and Blood Institute (NHLBI)/Heart Rhythm Society for established SCD using data from a well-characterized emergency medical service (EMS) registry operated in the district of Aurich, Lower Saxony, Germany.
Methods
We conducted our study in the district of Aurich, located in the Weser-Ems area in the northwest of Lower Saxony, Germany. The district covers an area of 1287 km2, and in 2009 was inhabited by 189 961 residents.19 Emergency medical care is provided exclusively by a single, central EMS carrier and two hospitals, all of which are owned and operated by the district government. Emergency medical service calls are dispatched centrally 24 h/day, 7 days a week. To reach all emergency patients district-wide within a maximum of 15 min, EMS operates 9 rescue service posts holding available 10 ambulances. Each ambulance is equipped with pre-hospital intensive care utilities, and is operated by two paramedics. For severe medical emergencies, two additional ambulances are staffed by trained emergency medicine physicians. All ambulances are equipped according to the German industry standard (DIN; paramedic-staffed ambulances: DIN EN 1798, Typ C; physician-staffed ambulances: DIN 75079).
Data for analysis were available from 1 January 2002 to 31 December 2009. We retrospectively included all patients who experienced pre-clinical SCD in the district of Aurich, and where EMS was called to the scene. We broadly screened all available EMS records for dispatch diagnoses compatible with SCD; keywords included ‘resuscitation’, ‘unconscious person’, ‘non-responsive person’, ‘collapse’, or similar paraphrases. We also used EMS claims data to identify resuscitation events that were not recognized by dispatch information. For all (100%) EMS operations suggestive of SCD by our screening approaches, we assessed the original EMS protocols and emergency medicine physician documentations. Only if a patient died at the scene, in addition we investigated the official death certificates (n = 56; 4.6%). In no case, death certificates were the only source of information. Hospital medical records were used occasionally to adjudicate SCD in the context of concomitant disease. No autopsy information was available for SCD adjudication. To stratify SCD patients in inhabitants and tourists, we searched for zip codes of residence. All patients with zip codes of residence from the district of Aurich or from one of the neighbouring districts (i.e. the districts of Wittmund, Leer, and Emden) were considered inhabitants. All those with different zip codes were considered tourists. All patient records were de-identified prior to analysis, and all study procedures conformed to the principles outlines in the declaration of Helsinki.
Based on the medical information and documentation, we adjudicated cases of established SCD. We included patients with both witnessed and unwitnessed events. In line with the WHO definition and NHLBI/Heart Rhythm Society 2010 recommendations of SCD, the onset of symptoms had to occur ≤1 h prior to the SCD event. We excluded patients without circulation for >1 h prior to the event. We further excluded patients with non-cardiac causes of death. Such non-cardiac events were assumed if resuscitation occurred in the context of major trauma including injuries obviously not compatible with life, or evident intoxications including smoke inhalation. We also excluded patients with known end-stage neoplastic diseases and other apparently moribund conditions. No age restrictions for inclusion were applied. All cases of established SCD based on our criteria were adjudicated independently by two physicians.
We calculated the annual incidence rate of SCD per 100 000 inhabitants. The count of inhabitants in the district of Aurich per year was derived from the annual official publication by the county government,19 and averaged over the observation period. For patients who experienced SCD, we describe baseline characteristics and compare differences by sex using a χ2 test or t-test as appropriate. We also present SCD incidence rates by age groups and describe the circadian and perennial distributions of SCD events. Poisson regression was used to formally compare perennial differences in SCD incidence by month. Statistical analyses were performed using SPSS (version16) and Microsoft Excel 2003.
Results
From 2002 to 2009, the mean mortality rate in the district of Aurich was 1060/100 000/year,19 which is well in accordance with the mean mortality rate in Germany during this period: 1030/100 000/year.6 The district of Aurich was also similar to the entire German population with respect to the age and sex distributions. Aurich was inhabited by 51.2% women and 48.8% men, whereas in Germany the proportions were 50.9% women and 49.1% men.5 Their age distributions by age groups were as follows in the district of Aurich vs. Germany: 0–20 years: 20.9 vs. 19.0%; 20–45 years: 29.1 vs. 31.9%; 45–65 years: 29.4 vs. 28.9%; >65 years: 20.6 vs. 20.2%.7 During the observation period, 228 592 EMS operations occurred. Applying our screening strategy, 5760 EMS operations were due to potential resuscitations. In 3487 of these operations, the patient was already responsive when EMS arrived at the scene, thus disproving SCD. In further 1061 EMS operations, death occurred due to clearly non-cardiac causes including overt suicide, surgical, or neurological emergencies. Finally, we identified 1212 EMS operations due to established SCD.
In 152 (12.5%) of all 1212 SCD cases, patients were declared dead at the scene without transport to one of the hospitals. All other patients were stabilized or transported under ongoing resuscitation conditions. Of these primarily successfully resuscitated patients, 887 (73.2%) were delivered to one of the district hospitals. The remaining 173 (14.3%) patients were transported to hospitals outside the district of Aurich, and were thus lost to follow-up. The latter were, however, included in our primary analysis by EMS records to calculate the incidence of SCD.
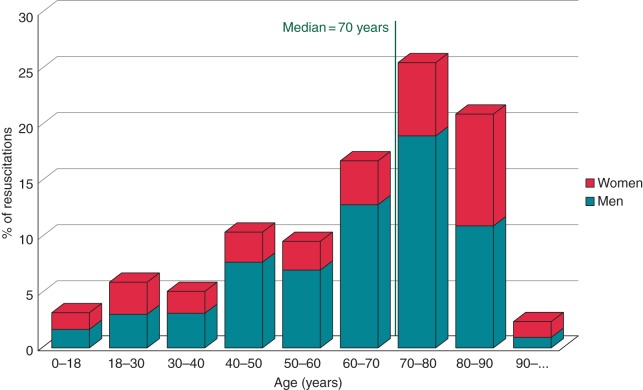
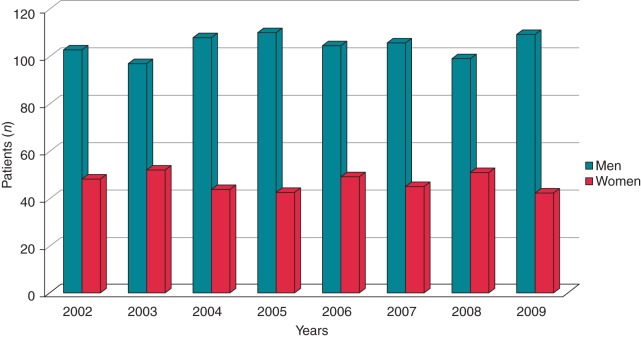
On average, we identified 151.5 SCD cases per year in the district of Aurich, corresponding to 81/100 000/year (Table 1). The incidence rate of SCD peaked in those of age 70–80 years; the median age at event was 69.5 years (Figure 1). In children and younger adults ≤35 years of age, the incidence of SCD was lower. This age group accounted for 113 (9.4%) SCD cases in the observation period. Incidence rates started to rise markedly after the age of 40 years. The annual incidence rate in those ≤35 years was 7.4/100 000/year. For patients 20–75 years of age (as used in the analysis of de Vreede-Swagemakers et al.9), it was 48/100 000/year (59% of SCD events in our cohort). In persons of usual employment age (15–65 years), we found an incidence rate of 32/100 000/year (39% of SCD events in our cohort). Sudden cardiac death occurred more frequently in men than in women: 836 (69%) men vs. 376 (31%) women (Figures 1 and 2). Only in the youngest (0–18 years) and oldest (>80 years) age groups, the rate of SCD was similar across sexes (Figure 1).
Table 1.
Sudden cardiac death incidence by year and sex
| SCD cases |
Men |
Women |
||||
|---|---|---|---|---|---|---|
| Year | n | n/100 000/year | n (%) | n/100 000/year | n (%) | n/100 000/year |
| 2002 | 151 | 79 | 103 (68%) | 54 | 48 (32%) | 25 |
| 2003 | 149 | 78 | 97 (65%) | 51 | 52 (35%) | 27 |
| 2004 | 152 | 80 | 108 (71%) | 57 | 44 (29%) | 23 |
| 2005 | 153 | 81 | 110 (72%) | 58 | 43 (28%) | 23 |
| 2006 | 154 | 81 | 105 (68%) | 55 | 49 (32%) | 26 |
| 2007 | 151 | 79 | 106 (70%) | 56 | 45 (30%) | 24 |
| 2008 | 150 | 79 | 99 (66%) | 52 | 51 (34%) | 27 |
| 2009 | 152 | 80 | 109 (72%) | 58 | 43 (28%) | 22 |
| 2002–09 | 151.5 | 81 | 104.6 (69%) | 55 | 46.9 (31%) | 25 |
Figure 1.
Age distribution of SCD cases from 2002 to 2009.
Figure 2.
Sex distribution of SCD cases from 2002 to 2009.
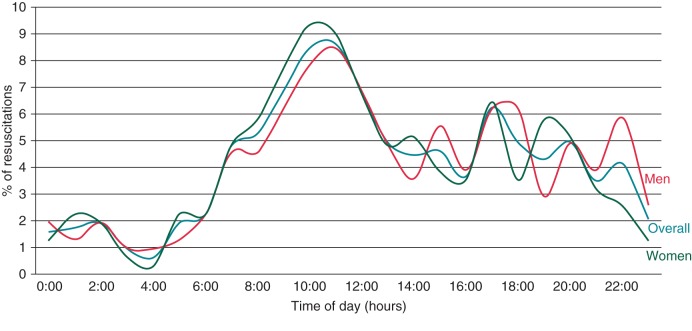
The district of Aurich is visited by tourists; per year, ∼7.5 million nights are spent by visitors, particularly during the summer months. Based on their zip code of residence, 8.5% of SCD patients (6.7/100 000/year) were tourists. To quantify the possible maximum confounding effect of tourists on the overall incidence of SCD, a sensitivity analysis revealed an annual SCD incidence of 74.3/100 000/year when restricted to county inhabitants only. The circadian distribution suggested the highest incidence of SCD between 8:00 a.m. and 12:00 p.m. for both men and women. The rate then slowly decreased until ∼12:00 a.m. The fewest SCD events were registered between 12:00 and 7:00 a.m., with a nadir around 4:00 a.m. (Figure 3). Perennially, most SCD events were observed in the months of August and September (see Supplementary material online, Figure S1). Yet, the differences in SCD incidence by month did not vary significantly (P = 0.09).
Figure 3.
Circadian distribution of SCD event, averaged from 2002 to 2009.
Discussion
In our study, we investigated the incidence of SCD in Germany, using data of well-characterized EMS and hospital medical records from the district of Aurich, Lower Saxony. Applying a conservative and consistent definition of established SCD and subsequent adjudication of all SCD cases, we report an SCD incidence rate of 81/100 000/year, which is largely in keeping with prior results from Europe and the USA. Even though the average overall annual mortality rates and the age and sex distributions, of the district of Aurich and Germany were similar, we assessed a circumscribed area of Germany.
Compared with other studies, our SCD incidence estimate is in the upper range of the published spectrum, yet with very stable annual rates for over 8 years (149–154 cases per year) (see Supplementary material online, Table S1). Analyses in the region of Maastricht9 and an US investigation17 suggested even higher incidence rates for SCD, whereat the underlying populations and the overall mortality rates were comparable. Importantly, the authors of the Maastricht study applied a different definition of SCD: patients were included who were seen alive within 24 h before the SCD event; analyses were then extended to medical information derived from the patients' family doctors. Patients <20 and >75 years were not included.9 Our definition of established SCD required an onset of symptoms ≤1 h prior to the event. As a critical difference, we required actually performed cardiopulmonary resuscitation measures as an indication of the acuteness of the index event. All ages were included.
Whereas studies from Ireland, Canada, or the USA might have an underlying population comparable with Germany and the Netherlands, their EMS systems are functioning differently.13,17,23 Studies in these countries reported SCD incidence rates between 50 and 60/100 000/year.11,14,16 Byrne et al. (Ireland) calculated the incidence of SCD based on emergency room and autopsy protocols. Consequently, patients declared dead out of hospital who did not undergo autopsy were excluded systematically, resulting in an underestimation of SCD.14 In our study, up to 12.5% of patients died at the scene and were not transported to the hospital but were included in the analysis for SCD incidence. This number seems to be low, given the high lethality of ventricular arrhythmias necessitating resuscitation.21,22 Yet, in the German EMS system it is a common practice to transport patients to the hospital once a normal rhythm has been restored, even if the outcome with respect to survival is likely to be fatal. Vaillancourt et al. evaluated questionnaires regarding resuscitations that were sent to EMS organizations and county governments in Canada. The incidence of SCD was calculated based on these questionnaires, but no information about missing questionnaires is provided.16 Since their methodology is distinctly different from ours, a direct comparison of the results appears unreliable. In the USA, Chugh et al.11 conducted a comparison between a prospective and a retrospective analysis of SCD cases. In the prospective analysis of protocols from EMS organizations, family doctors, and hospitals, the authors captured all available information about a patient, and subsequently adjudicated SCD. Using this approach, they found a SCD incidence rate of 53/100 000/year. In their retrospective analysis based on the interpretation of death certificates, the authors reported an incidence rate of 153/100 000/year. This three-fold difference highlights the importance of detailed patient information for the accurate estimation of SCD incidence.
To overcome the limitations of insufficient information of death certificates, we aimed to make use of as many more detailed sources as possible. Emergency medical service protocols with additional information and hospital medical records turned out to be most informative. Death certificates were only used in single cases (n = 56), when no other source of information besides EMS protocols was available. All clinical data adjudication was made by trained cardiologists to most accurately evaluate the presence of SCD. Despite methodological differences across studies, the adjudication of a specific SCD definition, such as in ‘established SCD’ used in our study, is likely to provide a most accurate estimate of SCD incidence and thereby reduces both over- and under-diagnosis. In addition, the geographical setting proved to be suitable for our evaluation: a well-defined geographical region, a single EMS carrier, and two district hospitals, all owned and operated by the district government, were an advantageous constellation making all EMS protocols and medical records available centrally and without major loss of follow-up. Further, all information was adjudicated by trained physicians.
Regarding the age distribution, we found the incidence of SCD to be highest from 70 to 80 years. This observation is explained most likely by a high prevalence of comorbidities predisposing to SCD in this age group. However, we also found a relevant proportion of SCD cases to be young: 7.4 SCD cases/100 000/year occurred below age 35 years. This observation is somewhat in contrast with other studies. Exemplarily, a Danish report by Winkel et al.23 only found 2.8/100 000/year. This discrepancy cannot be finally resolved by our study. Extensive and long past medical histories, and systematic autopsy information would be required to address the questions. Close to 40% of all SCD cases in our study occurred in individuals of working age (15–65 years). This high proportion is particularly relevant from a socioeconomic perspective. To reduce such a loss of work force in the future, further studies are warranted to improve prediction and prevention of SCD.
The circadian variation of SCD incidence showed a distribution similar to other studies, with a peak between 8:00 a.m. and 12:00 p.m.24–27 An explanation of this phenomenon in the context of our study remains open. Possible considerations include the sudden changes in heart rate, activity, and autonomic tone after wake up.28 Our definition of established SCD required SCD to occur within 1 h after the onset of symptoms. Therefore, we may have underestimated those cases occurring at night during sleep and recognized only in the morning limiting our observations on circadian incidence of SCD.
The perennial analysis suggested only slightly higher SCD rates during the summer. The county of Aurich is a touristic region with ∼7.5 million nights per year spent by visitors, particularly during summer. A slight increase of SCD incidence during the months of July through September might therefore be attributed to a higher percentage of visitors. Conversely, the numbers on county inhabitants experiencing SCD out of county are missing. Since other studies suggested a decrease of incidence during the summer,29 our results might be biased in this respect. Importantly, the perennial variation was not statistically significant.
Limitations
The strength of our investigation is the conservative and consistent definition of established SCD adjudicated by cardiologists based on emergency medical records from a well-defined area with homogeneous and standardized medical support and record systems. This strength is reflected by stable SCD incidence rates over a long time period of 8 years. However, several limitations need to be acknowledged. Most importantly, uncertainties remain regarding the incidence of SCD in patients who were found dead at the scene and in whom no EMS operation was initiated, as well as patients, in whom the onset of symptoms occurred >1 h before the initiation of the EMS operation. We also cannot exclude that among the 3487 individuals who were spontaneously responsive upon arrival of EMS personnel, there were single patients that experienced a rare event of spontaneous aborted SCD.
Yet, all of these circumstances, are pertinent to many other comparable studies,9,11,13–15,17,20,30 and result in an under- rather than an overestimation of the true incidence of SCD. Still, we acknowledge that single SCD cases might have been missed by our approach. Another limitation is the lack of information on long-term past medical history, systematic autopsy, or SCD cases without EMS involved. More general, we can only comment on the underlying population, which is primarily of German descent. It therefore remains unclear from our data, if the incidence of SCD is different in individuals of other ethnic backgrounds. Despite similarities in mortality rates and age and sex distributions, it remains to be shown, if the results from the district of Aurich can be extrapolated to the rest of Germany. Whereas there is no effect on our primary objective to assess the incidence of established SCD cases, we cannot comment on the outcome of the subgroup of patients not transported to one of the district hospitals.
Conclusion
In conclusion, our retrospective analysis of a well-defined EMS registry in the district of Aurich for the first time describes an incidence estimate for established SCD in a district of Germany. Unlike other recent investigations,15,20 we employed a systematic evaluation of original EMS protocols and medical records by trained cardiologists with a focus on established SCD cases to minimize under- or overestimation of incidence rates. Importantly, a considerable number (39%) of SCD events affect individuals of working age. Despite advances in medical care and a modern European EMS system, we observed stable incidence rates of SCD. A systematic assessment of the actual incidence of SCD in defined regions and countries might be a prerequisite for improved risk stratification and prevention of SCD. Prospective registries for representative regions of Europe that will include a range of variables for risk stratification including biomarkers and genetic information are warranted and will be important areas of future research.
Supplementary material
Funding
The work was supported partially by the German Federal Ministry of Education and Research (BMBF), the French Agence Nationale de la Recherche (ANR) [01KU0907], and the Deutsches Zentrum für Herz-Kreislauf-Forschung (DZHK). Funding to pay the Open Access publication charges for this article was provided by the DZHK (German Centre for Cardiovascular Research) and by the BMBF (German Ministry of Education and Research).
Acknowledgments
Conflict of interest: none declared.
References
- 1.Priori SG, Aliot E, Blomstrom-Lundqvist C, Bossaert L, Breithardt G, Brugada P, et al. Task force on sudden cardiac death of the European Society of Cardiology. Eur Heart J. 2001;22:1374–450. doi: 10.1053/euhj.2001.2824. [DOI] [PubMed] [Google Scholar]
- 2.Fishman GI, Chugh SS, Dimarco JP, Albert CM, Anderson ME, Bonow RO, et al. Sudden cardiac death prediction and prevention: report from a National Heart, Lung, and Blood Institute and Heart Rhythm Society Workshop. Circulation. 2010;122:2335–48. doi: 10.1161/CIRCULATIONAHA.110.976092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zaijia C, James TN, Kulbertus H, Maseri A, Oliver MF, Pobee JOM, et al. 1985. p. 726. Sudden cardiac death: report of a WHO scientific group [meeting held in Geneva from 24 to 27 October 1984]. World Health Organization technical report series.
- 4.Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, et al. American College of C, American Heart Association Task F, European Society of Cardiology Committee for Practice G, European Heart Rhythm A, Heart Rhythm S. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to develop guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death) developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Europace. 2006;8:746–837. doi: 10.1093/europace/eul108. [DOI] [PubMed] [Google Scholar]
- 5.Internationale Statistische Klassifikation der Krankheiten und Verwandter Gesundheitsprobleme, 10. Revision, German Modification. Deutsches Institut für Medizinische Dokumentation und Information http://www.dimdi.de/static/de/klassi/icd-10-gm/kodesuche/onlinefassungen/htmlgm2013/index.htm. 17 June 2013.
- 6.Todesursachen in Deutschland 2010. Federal Office of Statistics https://www.destatis.de/DE/Publikationen/Thematisch/Gesundheit/Todesursachen/Todesursachen2120400107004.pdf?__blob=publicationFile. 1 October 2013.
- 7.Myerburg RJ. Scientific gaps in the prediction and prevention of sudden cardiac death. J Cardiovasc Electrophysiol. 2002;13:709–23. doi: 10.1046/j.1540-8167.2002.00709.x. [DOI] [PubMed] [Google Scholar]
- 8.Muller D, Agrawal R, Arntz HR. How sudden is sudden cardiac death? Circulation. 2006;114:1146–50. doi: 10.1161/CIRCULATIONAHA.106.616318. [DOI] [PubMed] [Google Scholar]
- 9.de Vreede-Swagemakers JJ, Gorgels AP, Dubois-Arbouw WI, van Ree JW, Daemen MJ, Houben LG, et al. Out-of-hospital cardiac arrest in the 1990s: a population-based study in the Maastricht area on incidence, characteristics and survival. J Am Coll Cardiol. 1997;30:1500–5. doi: 10.1016/s0735-1097(97)00355-0. [DOI] [PubMed] [Google Scholar]
- 10.Rao BH, Sastry BK, Chugh SS, Kalavakolanu S, Christopher J, Shangula D, et al. Contribution of sudden cardiac death to total mortality in India—a population based study. Int J Cardiol. 2010;154:163–7. doi: 10.1016/j.ijcard.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 11.Chugh SS, Jui J, Gunson K, Stecker EC, John BT, Thompson B, et al. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol. 2004;44:1268–75. doi: 10.1016/j.jacc.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 12.Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–63. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 13.Tokashiki T, Muratani A, Kimura Y, Muratani H, Fukiyama K. Sudden death in the general population in Okinawa: incidence and causes of death. Jpn Circ J. 1999;63:37–42. doi: 10.1253/jcj.63.37. [DOI] [PubMed] [Google Scholar]
- 14.Byrne R, Constant O, Smyth Y, Callagy G, Nash P, Daly K, et al. Multiple source surveillance incidence and aetiology of out-of-hospital sudden cardiac death in a rural population in the West of Ireland. Eur Heart J. 2008;29:1418–23. doi: 10.1093/eurheartj/ehn155. [DOI] [PubMed] [Google Scholar]
- 15.Hua W, Zhang L-F, Wu Y-F, Liu X-Q, Guo D-S, Zhou H-L, et al. Incidence of sudden cardiac death in china: analysis of 4 regional populations. J Am Coll Cardiol. 2009;54:1110–8. doi: 10.1016/j.jacc.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 16.Vaillancourt C, Stiell IG. Cardiac arrest care and emergency medical services in Canada. Can J Cardiol. 2004;20:1081–90. [PubMed] [Google Scholar]
- 17.Bachman JW, McDonald GS, O'Brien PC. A study of out-of-hospital cardiac arrests in northeastern Minnesota. JAMA. 1986;256:477–83. [PubMed] [Google Scholar]
- 18.Becker LB, Smith DW, Rhodes KV. Incidence of cardiac arrest: a neglected factor in evaluating survival rates. Ann Emerg Med. 1993;22:86–91. doi: 10.1016/s0196-0644(05)80257-4. [DOI] [PubMed] [Google Scholar]
- 19. Wissenswertes rund um den Landkreis Aurich, Landkreis Aurich http://www.landkreis-aurich.de/daten_fakten.html. 17 June 2013.
- 20.Fragkouli K, Vougiouklakis T. Sudden cardiac death: an 11-year postmortem analysis in the region of Epirus, Greece. Pathol Res Pract. 2010;206:690–4. doi: 10.1016/j.prp.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 21.Atwood C, Eisenberg MS, Herlitz J, Rea TD. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation. 2005;67:75–80. doi: 10.1016/j.resuscitation.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 22.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Winkel BG, Holst AG, Theilade J, Kristensen IB, Thomsen JL, Ottesen GL, et al. Nationwide study of sudden cardiac death in persons aged 1–35 years. Eur Heart J. 2011;32:983–90. doi: 10.1093/eurheartj/ehq428. [DOI] [PubMed] [Google Scholar]
- 24.Muller JE, Ludmer PL, Willich SN, Tofler GH, Aylmer G, Klangos I, et al. Circadian variation in the frequency of sudden cardiac death. Circulation. 1987;75:131–8. doi: 10.1161/01.cir.75.1.131. [DOI] [PubMed] [Google Scholar]
- 25.Willich SN, Levy D, Rocco MB, Tofler GH, Stone PH, Muller JE. Circadian variation in the incidence of sudden cardiac death in the Framingham Heart Study population. Am J Cardiol. 1987;60:801–6. doi: 10.1016/0002-9149(87)91027-7. [DOI] [PubMed] [Google Scholar]
- 26.Arntz HR, Willich SN, Oeff M, Brüggemann T, Stern R, Heinzmann A, et al. Circadian variation of sudden cardiac death reflects age-related variability in ventricular fibrillation. Circulation. 1993;88:2284–9. doi: 10.1161/01.cir.88.5.2284. [DOI] [PubMed] [Google Scholar]
- 27.Willich SN, Goldberg RJ, Maclure M, Perriello L, Muller JE. Increased onset of sudden cardiac death in the first three hours after awakening. Am J Cardiol. 1992;70:65–8. doi: 10.1016/0002-9149(92)91391-g. [DOI] [PubMed] [Google Scholar]
- 28.Portaluppi F, Tiseo R, Smolensky MH, Hermida RC, Ayala DE, Fabbian F. Circadian rhythms and cardiovascular health. Sleep Med Rev. 2012;16:151–66. doi: 10.1016/j.smrv.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 29.Arntz H-R, Willich SN, Schreiber C, Brüggemann T, Stern R, Schultheiß H-P. Diurnal, weekly and seasonal variation of sudden death. Population-based analysis of 24061 consecutive cases. Eur Heart J. 2000;21:315–20. doi: 10.1053/euhj.1999.1739. [DOI] [PubMed] [Google Scholar]
- 30.Vaillancourt C, Charette M, Stiell IG, Phillips KR, Wells GA. Out-of-hospital cardiac arrest surveillance in Canada: a survey of national resources. Can J Emerg Med. 2010;12:119–27. doi: 10.1017/s1481803500012148. [DOI] [PubMed] [Google Scholar]