Abstract
Background
Sipuleucel-T is a US Food and Drug Administration–approved immunotherapy for asymptomatic or minimally symptomatic metastatic castration-resistant prostate cancer (mCRPC). Its mechanism of action is not fully understood. This prospective trial evaluated the direct immune effects of systemically administered sipuleucel-T on prostatic cancer tissue in the preoperative setting.
Methods
Patients with untreated localized prostate cancer were treated on an open-label Phase II study of sipuleucel-T prior to planned radical prostatectomy (RP). Immune infiltrates in RP specimens (posttreatment) and in paired pretreatment biopsies were evaluated by immunohistochemistry (IHC). Correlations between circulating immune response and IHC were assessed using Spearman rank order.
Results
Of the 42 enrolled patients, 37 were evaluable. Adverse events were primarily transient, mild-to-moderate and infusion related. Patients developed T cell proliferation and interferon-γ responses detectable in the blood following treatment. Furthermore, a greater-than-three-fold increase in infiltrating CD3+, CD4+ FOXP3-, and CD8+ T cells was observed in the RP tissues compared with the pretreatment biopsy (binomial proportions: all P < .001). This level of T cell infiltration was observed at the tumor interface, and was not seen in a control group consisting of 12 concurrent patients who did not receive any neoadjuvant treatment prior to RP. The majority of infiltrating T cells were PD-1+ and Ki-67+, consistent with activated T cells. Importantly, the magnitude of the circulating immune response did not directly correlate with T cell infiltration within the prostate based upon Spearman’s rank order correlation.
Conclusions
This study is the first to demonstrate a local immune effect from the administration of sipuleucel-T. Neoadjuvant sipuleucel-T elicits both a systemic antigen-specific T cell response and the recruitment of activated effector T cells into the prostate tumor microenvironment.
Introduction
Sipuleucel-T is an immunotherapy that improves overall survival (OS) in metastatic castration-resistant prostate cancer (mCRPC) (1,2). Sipuleucel-T is generated from autologous peripheral blood mononuclear cells (PBMC) that are cultured ex vivo with recombinant fusion protein (PA2024) composed of prostatic acid phosphatase (PAP) and granulocyte-monocyte colony stimulating factor (GM-CSF). While sipuleucel-T can generate systemic immune responses to PA2024 and PAP (3), the direct effect of this treatment on the tumor microenvironment is unknown.
To better understand the mechanism of action of sipuleucel-T, a multicenter phase 2 neoadjuvant trial administering sipuleucel-T to patients with localized prostate cancer, prior to their planned radical prostatectomy (RP), was undertaken (NeoACT, ClinicalTrials.gov identifier: NCT00715104). Immune infiltrates in RP specimens (posttreatment) as assessed by immunohistochemistry (IHC) were compared with those from paired pretreatment biopsies. Immune infiltrates were also assessed in prostate biopsy and RP specimens from control patients who did not receive any neoadjuvant treatment. We show that sipuleucel-T not only induces circulating T cell immune responses, but also T cell infiltration in the tumor microenvironment.
Methods
Study Design
This was a single-arm, multicenter phase II trial of neoadjuvant sipuleucel-T treatment in men with localized prostate cancer administered prior to planned RP. Eligible patients had a normal complete blood count, adequate hepatic and renal function, tissue available from a pretreatment prostate biopsy, and were negative for HIV, HTLV-1 and -2, and hepatitis B and C. All subjects gave written informed consent to participate in the protocol approved by the Institutional Review Boards (IRBs) of each participating institution. Subjects received sipuleucel-T at the standard two-week intervals for three planned doses prior to RP (Supplementary Figure 1, available online). Sipuleucel-T was started six to seven weeks prior to RP, allowing for a two- to three-week interval between the final infusion of sipuleucel-T and the RP. Following RP, patients were randomized to either receive or not receive a single booster of sipuleucel-T treatment at 12 weeks. This manuscript details the histologic results of neoadjuvant therapy with sipuleucel-T, the primary objective of this study, as well as the peripheral immune responses to sipuleucel-T observed in this clinical setting.
Control group: Prior to this study, the effect of systemically administered sipuleucel-T on localized prostate cancer deposits was unknown. Consequently, it was felt that randomization to a no-treatment arm was premature and would represent a major accrual challenge until any treatment effect was better characterized. However, it was felt to be critically important to have a negative control available, in order to provide confidence that changes observed in the prostates of treated patients represented a true treatment effect. A group of patients who underwent RP at the University of California San Francisco (UCSF) during the same time period, but who had not received any preoperative therapy, served as a reference group and were used as negative controls. These control patients were selected prior to undergoing any tissue analysis, based on a distribution of preoperative Cancer of the Prostate Risk Assessment (CAPRA) risk criteria (4), to provide an analogous mix of disease risk to the patients participating in the trial (five patients with CAPRA scores 0–2, four patients with CAPRA scores 3–5, and three patients with CAPRA scores 6–10). These patients were selected from the broader surgical population that routinely provides written consent for the use of their specimens for research (UCSF IRB approved protocol for human subjects research #11-05226).
Study Endpoints
The primary outcome measure was the change in the number of infiltrating CD3+ T cells/μm2 within the prostate tissue between the paired biopsy and RP specimens, as quantified by immunohistochemistry (IHC) and image analysis. Secondary endpoints included: 1) the difference in the number of infiltrating T cell subsets (cytotoxic CD8+, helper CD4+ FOXP3-, and regulatory CD4+ FOXP3+ T cells) between the biopsy and the RP, as quantified by IHC and image analysis, 2) changes from baseline to posttreatment of antigen-specific T cell responses in peripheral blood as measured by T cell proliferation and enzyme-linked immunospot (ELISPOT) assays, and 3) safety.
Systemic Immune Response Assays
T cell proliferation and ELISPOT assays were performed as previously described (Supplementary Methods, available online) (5).
Immunohistochemistry
Immunohistochemistry was performed using standard methods (Supplementary Methods, available online). Stained slides were then scanned with an automated microscope scanner (Aperio Scanscope XT, Aperio, Buffalo Grove, IL). For RP sections, tissue was designated into three distinct compartments: benign glands, tumor centers, and tumor interfaces. Five randomly selected fields (0.25mm2, original magnification 20×, 0.5 µm per pixel resolution) from each compartment were then captured from each slide with ImageScope software (Aperio). Tumor interfaces were defined as fields where malignant and benign glands were present. Automatic cell counts for single- and double-stained cells were determined for each field with color-specific algorithms in Axiovision software (Zeiss, Peabody, MA). The cell count for each compartment is reported as the mean for each of the five quantitated fields.
Statistical Analysis
This study was designed to detect activity within prostate tissue as measured by a change in the CD3+ T cell count/μm2 between the pretreatment biopsy and the RP tissue following sipuleucel-T infusions. Accrual of 30 patients was required to recognize a two-fold increase from baseline in at least 40% of the patient cohort, compared with only 15%. This assumed a power of 90% and a directional 5% statistical significance level based upon an exact binomial test.
One-way analysis of variance methods for repeated measures were used to test for overall differences in mean IHC results among the biopsy sample and three RP tissue compartments (Statistica v6.0, Statview, Cary, NC). Newman-Keuls post-hoc tests were performed to identify pairwise differences among the tissue types if there was an overall statistical difference (probability value < 0.05). Because patients were not randomized to treatment with sipuleucel-T, the treated and untreated cohorts were analyzed separately. Complete data were available for these analyses. For the analysis of the proliferation and ELISPOT assays, nonparametric methods were applied because of the frequency of zero measurements. For each immune response, the Wilcoxon matched pairs test was performed to compare the baseline distribution with each follow-up time point (pre-RP, weeks six and 12 post-RP). The Spearman rank order correlation was used and analyzed with a t test to evaluate the relationships between blood immune outcomes and between peripheral blood outcomes and tissue T cell components from the IHC analysis. No adjustment was made for multiple comparisons for these exploratory analyses. All statistical tests were two-sided, except for a test of a binomial proportion to compare the proportion of patients achieving a two- or three-fold increase in the RP specimen vs the pretreatment biopsy with a null hypothesis of 15% of the patients.
Results
Patients and Treatment
Between September 29, 2008 and June 6, 2011, a total of 42 patients were enrolled from five sites. Nineteen (45.2%) patients had low-risk disease, 14 (33.3%) had intermediate-risk disease, and nine (21.4%) had high-risk disease as defined by the CAPRA score prior to RP (Table 1). One patient withdrew consent prior to receiving any therapy, and was therefore excluded from the patients evaluated for immune responses (Supplementary Figure 2, available online). Of the 41 patients, 38 received all three pre-RP infusions of sipuleucel-T. Three patients received two infusions, but were unable to receive a third due to insufficient blood flow for leukapheresis (n = 1), error at the apheresis center (n = 1), and a patient failing to arrive for a treatment appointment (n = 1). Of the 41 patients who received sipuleucel-T, 37 underwent RP and were evaluable, three withdrew consent, and one was lost to follow up. Laparoscopic prostatectomy was performed in 29 patients, and retropubic RP was performed in eight patients. The 41 patients who received at least one leukapheresis procedure were considered in the assessment of safety. The 37 patients who underwent RP were evaluable for peripheral immune responses and immune infiltrates.
Table 1.
Baseline demographics and disease characteristics
| Characteristic | Patients, No. (%) |
|---|---|
| Patients enrolled | 42 (100.0) |
| Age, y | |
| Median | 61 |
| Range | 51–72 |
| Weight, lbs | |
| Median | 187 |
| Range | 147–309 |
| Race | |
| Caucasian | 41 (97.6) |
| Asian | 1 (2.4) |
| ECOG PS = 0 | 42 (100.0) |
| Gleason sum at baseline | |
| ≤6 | 10 (23.8) |
| 7 | 18 (42.9) |
| ≥8 | 14 (33.3) |
| Clinical stage | |
| T1B | 1 (2.4) |
| T1C | 21 (50.0) |
| T2A | 7 (16.7) |
| T2B | 2 (4.8) |
| T2C | 10 (23.8) |
| T3A | 1 (2.4) |
| Nodal status | |
| N0 | 16 (38.1) |
| NX | 26 (61.9) |
| Distant metastasis | |
| M0 | 17 (40.5) |
| MX | 25 (59.5) |
| PSA, ng/mL | |
| Median | 6 |
| Range | 1–92 |
| LDH (range), U/L | |
| Median | 156 |
| Range | 114–567 |
| Hemoglobin (range), g/dL | |
| Median | 15 |
| Range | 13–17 |
| Alk phos (range), U/L | |
| Median | 64 |
| Range | 34–154 |
| CAPRA Score | |
| 0–2 | 19 (45.2) |
| 3–5 | 14 (33.3) |
| 6–10 | 9 (21.4) |
* CAPRA = Cancer of the Prostate Risk Assessment; ECOG = Eastern Cooperative Oncology Group; LDH = lactic dehdrogenase; PSA = prostate-specific antigen.
Safety
Adverse events (AEs) prior to RP were reported in a total of 34/42 patients (81.0%), and most were Grade 1–2 and transient (Table 2) and consistent with other trials (2). Two serious AEs (SAEs) were reported prior to RP (B cell lymphoma [1/41] and infusion-related reaction [1/41]). The most frequent AEs (>10% of patients) that occurred within one day after infusion were Grade 1–2 fatigue, headache, and myalgia. There were only two treatment-related Grade 3 AEs that occurred prior to RP: arthralgia (1/41, 2.4%) and flu-like reaction (1/41, 2.4%). Sipuleucel-T did not appear to affect operative complications, procedure time, or estimated blood loss.
Table 2.
Adverse events*
| Adverse events | Total, No. (%) |
|---|---|
| Fatigue | 18 (42.9) |
| Paraesthesia oral | 10 (23.8) |
| Headache | 8 (19.0) |
| Citrate toxicity | 7 (16.7) |
| Chills | 5 (11.9) |
| Myalgia | 5 (11.9) |
| Nausea | 5 (11.9) |
| Contusion | 4 (9.5) |
| Diarrhea | 4 (9.5) |
| Muscle spasms | 4 (9.5) |
| Anxiety | 3 (7.1) |
| Arthralgia | 3 (7.1) |
| Paraesthesia | 3 (7.1) |
* Adverse events (AEs) that occurred from the first leukapheresis through prior to radical prostatectomy in less than 5% of patients are shown. Three grade 3–4 AEs (arthralgia, Infusion reaction, and B-cell lymphoma) were reported. There were no grade 5 AEs.
Clinical Efficacy
Downstaging was not observed at the time of RP relative to baseline. Six patients (16%) had downgrading of their Gleason Scores at RP relative to pretreatment biopsies, while eight had upgrading (22%). In the control group, one patient (8%) had downgrading of Gleason Score at RP relative to pretreatment biopsies, while two had upgrading (17%).
Systemic Immune Response
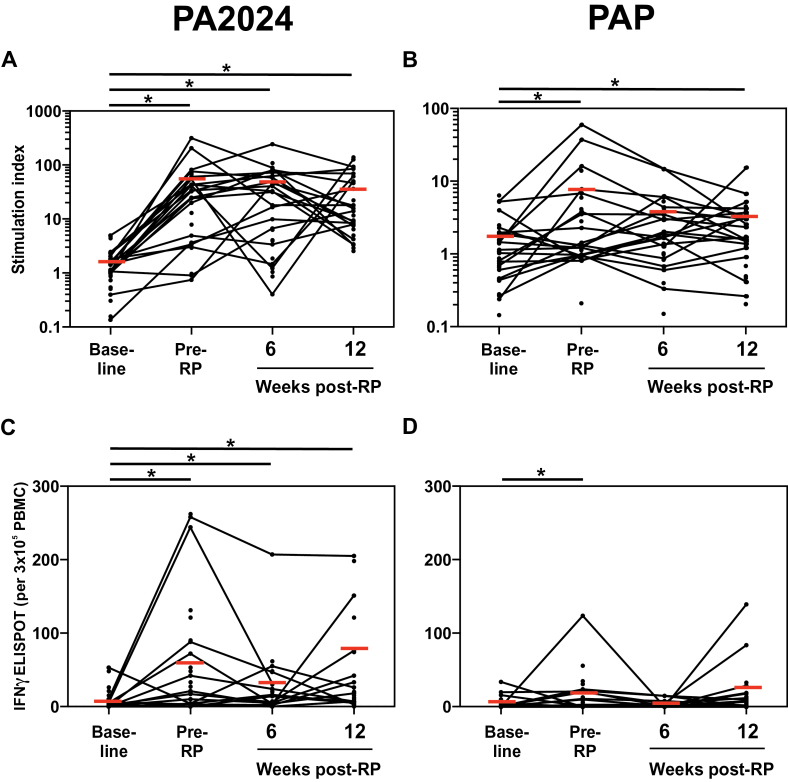
T cell proliferative responses to PA2024 were induced by treatment and persisted through week 12 post-RP (Figure 1A). T cell proliferation to PAP was also seen in some patients, though less frequently (Figure 1B). IFN-γ responses to PA2024, and to a lesser degree PAP, were also induced by treatment pre-RP (Figure 1, C and D).
Figure 1.
Antigen-specific circulating T cell responses following sipuleucel-T treatment. T cell proliferation to PA2024 (A) and PAP (B) were measured by 3H-thymidine incorporation in cultured PBMC. IFNγ responses to PA2024 (C) and prostatic acid phosphatase (D) were measured by enzyme-linked immunospot (ELISPOT) in cultured peripheral blood mononuclear cells. Each measure is shown at baseline, pre–radical prostatectomy (RP) (following sipuleucel-T infusions), six weeks post-RP, and 12 weeks post-RP. Horizontal bars represent the median values of patients with all four timepoints available. * Denotes two-sided P under .05, Wilcoxon matched pairs test for comparison with baseline. PA2024 = recombinant fusion protein; PAP = prostatic acid phosphatase; RP = radical prostatectomy.
Immune Response in Prostate Tissues
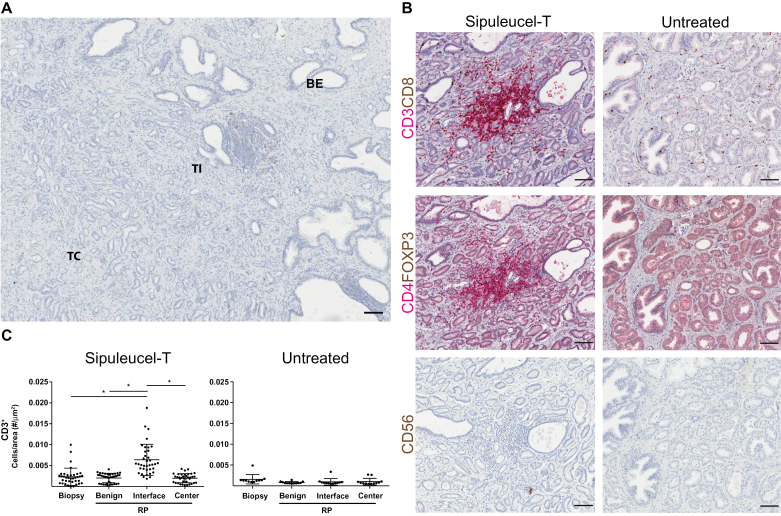
The frequencies of immune cells in the RP tissue were quantitated in three compartments: benign glands, tumor interface, and tumor center (Figure 2A). T cells were evident in the RP tissues of sipuleucel-T–treated patients and were concentrated primarily at the tumor interface (Figure 2B). Increased infiltration of CD3+ T cells was evident at the tumor interface (mean = 6.39 x 10–3/μm2, 95% confidence interval [CI] = 5.20 to 7.58 x 10–3/μm2) compared with the pretreatment biopsy (mean = 2.33 x 10–3/μm2, 95% CI = 1.66 to 2.99 x 10–3/μm2, P < .001) (Figure 2C). A greater-than-three-fold increase was seen in 57% (95% CI = 39% to 79%) of the patients treated with sipuleucel-T. This was statistically significantly higher than the null hypothesis of only a two-fold increase of 15% (P < .001). This increased infiltration by CD3+ T cells at the tumor interface (mean = 0.95 x 10–3/μm2) was not evident in the control group, who did not receive the neoadjuvant therapy.
Figure 2.
Frequency of intraprostatic T cells in biopsy and radical prostatectomy (RP) sections from patients treated with sipuleucel-T and untreated patients. A) Representative RP section with benign glands, tumor interface, and tumor center are depicted. B) Representative digital micrographs of immunohistochemistry-stained RP sections from patients treated with sipuleucel-T (left panels) and untreated patients (right panels) showing the tumor interface between benign and tumor tissue. Sections are stained for CD3 (red) /CD8 (brown) in the top panels, CD4 (red)/FOXP3 (brown) in the middle panels, and CD56 (brown) in the bottom panels. C) CD3+ T cells were quantitated by digital image analysis in prostate biopsies and in the RP sections. Cell frequencies in the RP sections were quantified in three compartments: benign glands, tumor interface, and tumor center. Means ± 95% confidence interval are shown with horizontal lines. * Denotes P under .05, analysis of variance (ANOVA) methods for repeated measures with post-hoc comparisons with the RP interface compartment. All ANOVA tests were two-sided. Scale bars = 100 μm. BE = benign glands; RP = radical prostatectomy; TC = tumor center; TI = tumor interface.
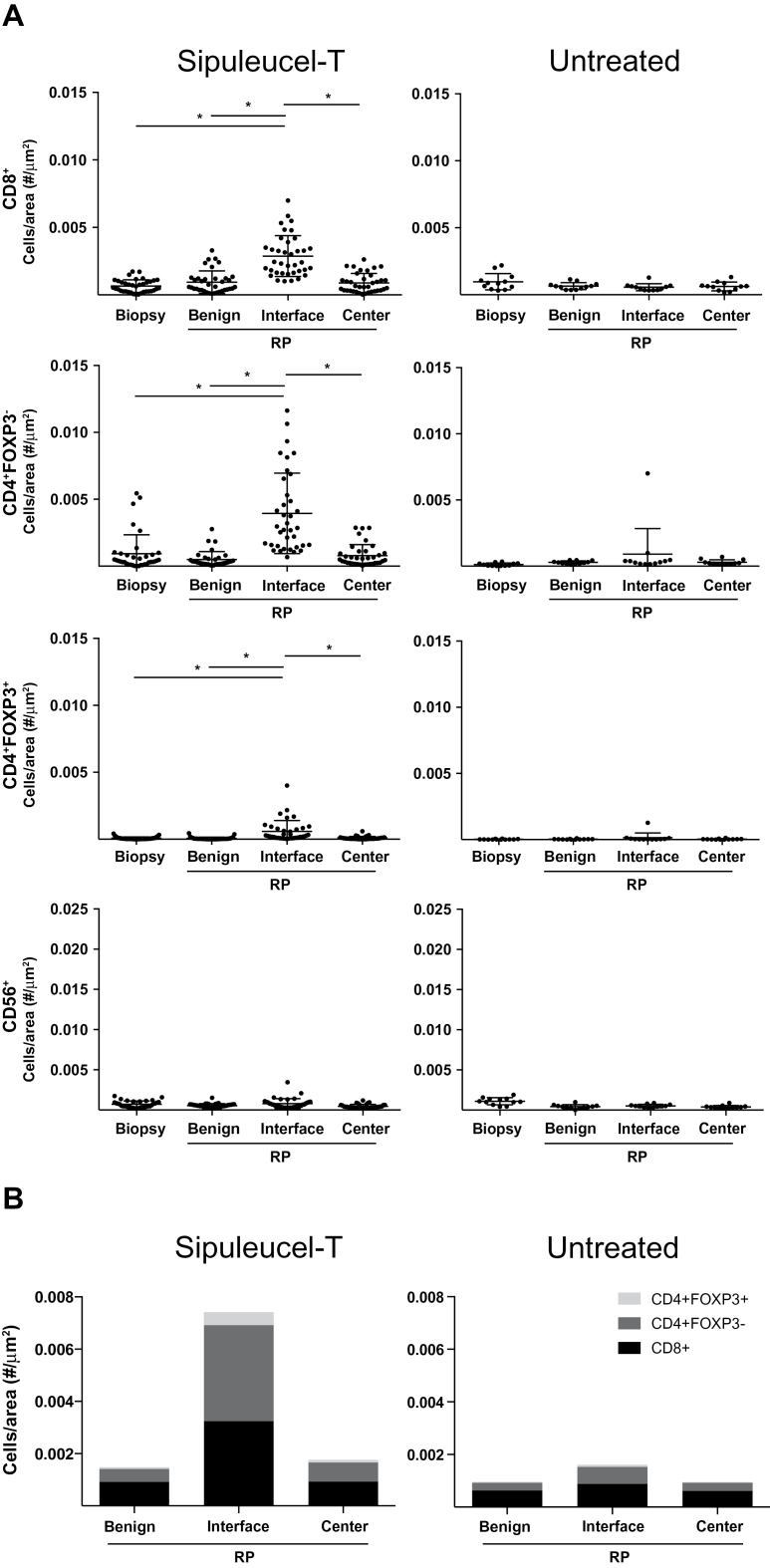
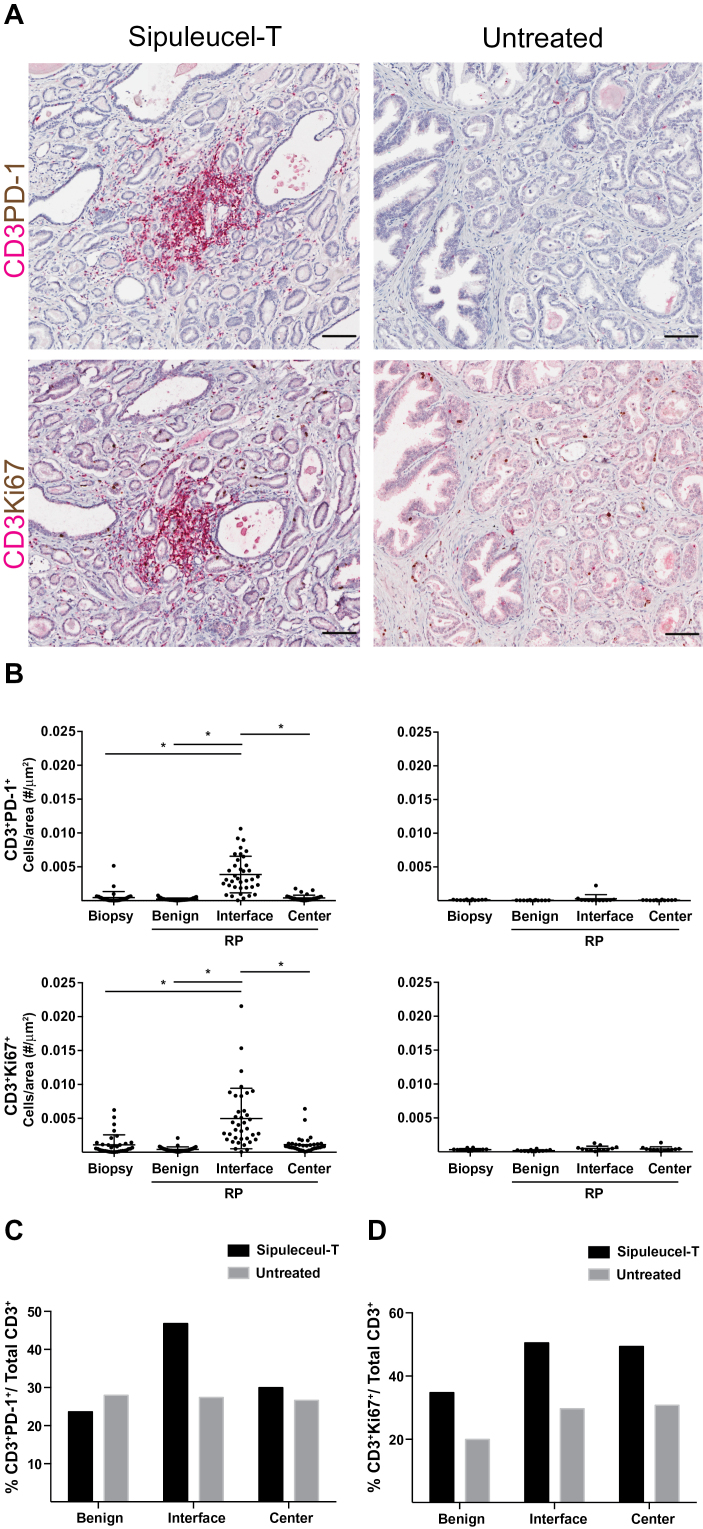
Effector CD4+ FOXP3- helper T cell numbers were increased at the tumor interface (mean = 3.95 x 10–3/μm2, 95% CI = 2.98 to 4.92 x 10–3/μm2) with treatment compared with the biopsy (mean = 0.93 x 10–3/μm2, 95% CI = 0.47 to 1.38 x 10–3/μm2, P < .001) (Figure 3A). CD8+ cytotoxic T cell numbers were also increased at the tumor interface (mean = 2.87 x 10–3/μm2, 95% CI = 2.39 to 3.36 x 10–3/μm2) compared with the biopsy (mean = 0.65 x 10–3/μm2, 95% CI = 0.50 to 0.80 x 10–3/μm2, P < .001). CD4+/FOXP3+ regulatory T cell (Tregs) numbers were also increased at the tumor interface. The majority of T cells at the interface were CD4+ helper T cells, with Tregs constituting only a small proportion of the T cells (Figure 3B, left panel). Nevertheless, the mean values among the four tissue compartments for CD3+ T cells, CD8+ T cells, CD4+ FoxP3- effector T cells, and CD4+/FOXP3+ Tregs were each statistically significantly different overall (all P < .0001, analysis of variance) with sipuleucel-T treatment (Figure 3B, left panel). Natural killer cell numbers were not increased in the RP specimens following sipuleucel-T treatment, indicating that the lymphocyte infiltration induced by sipuleucel-T was not because of nonspecific recruitment of immune cells to the prostate. Nearly half of CD3 T lymphocytes at the tumor interface of treated patients expressed PD-1 (Figure 4, A and B). Because PD-1 is expressed on both activated and exhausted T cells, we performed staining for Ki-67 as a marker of activated, proliferating T cells. In patients treated with sipuleucel-T, we found that the majority of CD3 T cells in interface and tumor centers were also Ki-67+ (Figure 4C). While T cells could rarely be found as clusters as seen with tertiary lymphoid structures (6), the increase of T cells was predominantly because of diffuse infiltration at the interface (Supplementary Figure 3A, available online). B cells were also increased at the tumor interface (Supplementary Figure 3B, available online). These lymphocytes were not consistently clustered at high endothelial venules (HEV), nor was there a difference in the density of HEV to account for the changes seen in the treated patients (Supplementary Figure 3, C and D, available online).
Figure 3.
Frequency of intraprostatic T cell subsets in biopsy and radical prostatectomy (RP) sections from patients treated with sipuleucel-T and untreated patients. A) Quantitation of CD8+cytotoxic T cells, effector CD4+ FOXP3- T cells, regulatory CD4+ FOXP3+ T cells, and CD56+ natural killer cells was performed using digital image analysis. Cell frequencies in the RP sections were again quantified in three compartments: benign glands, tumor interface, and tumor center. B) The relative composition of the mean T subset frequencies within the RP is presented. Means ± 95% confidence intervals are shown with horizontal bars. * Denotes P under .05, analysis of variance (ANOVA) methods for repeated measures with post-hoc comparisons with the RP interface compartment. All ANOVA tests were two-sided. RP = radical prostatectomy.
Figure 4.
Expression of programmed death 1(PD1) and Ki-67 on CD3+ T lymphocytes in biopsy and radical prostatectomy (RP) sections from patients treated with sipuleucel-T and untreated patients. A) Representative digital micrographs of immunohistochemistry-stained RP sections from sipuleucel-T–treated and –untreated control patients showing expression of PD1 and Ki-67 on CD3+ T lymphocytes at the tumor interface. Scale bars = 100 μm. B) Quantitation of PD1 and Ki-67 expression on CD3+ was performed using digital image analysis on the different tissue compartments. Means ± 95% confidence interval are shown with horizontal lines. The relative composition of the mean PD1+ (C) and Ki-67+ (D) T frequencies within the RP are presented. * P under .05, analysis of variance (ANOVA) methods for repeated measures with post-hoc comparisons with the RP interface compartment. Scale bars = 100 μm. All ANOVA tests were two-sided. RP = radical prostatectomy.
We examined whether there were any relationships between systemic immune responses and the magnitude of T cell infiltration in the tumors. We found no correlation between the pre-RP immune responses (proliferation or ELISPOT response to either PA2024 or PAP) and the CD3+, CD4+FOXP3-, and CD8+ T cell infiltration in any of the RP compartments (Spearman rank order correlations: P > .07 for all, data not shown). When the changes in immune responses from baseline to pre-RP were analyzed, however, there were statistically significant correlations between PAP IFNγ ELISPOT responses and CD3 infiltration in benign and tumor tissue (Spearman rank order correlations: t test P = .01 for each) (Table 3). There was also a statistically significant correlation between the change in PA2024 IFNγ ELISPOT and CD4 T cell infiltration at the interface (Table 3).
Table 3.
Correlations between the change in enzyme-linked immunospot (ELISPOT) response and frequency of T cells in the radical prostatectomy tissue (n = 27)
| Compartment | PA2024 ELISPOT change | PAP ELISPOT change | ||
|---|---|---|---|---|
| Spearman | P | Spearman | P | |
| correlation | correlation | |||
| CD3 benign | 0.16 | .44 | 0.48 | .01 |
| CD3 interface | 0.23 | .24 | 0.33 | .09 |
| CD3 center | 0.18 | .37 | 0.49 | .01 |
| CD4 benign | 0.03 | .90 | 0.02 | .92 |
| CD4 interface | 0.48 | .01 | 0 | .00 |
| CD4 center | 0.24 | .22 | 0.12 | .55 |
| CD8 benign | 0.22 | .27 | 0.22 | .28 |
| CD8 interface | 0.27 | .18 | 0.13 | .52 |
| CD8 center | 0.16 | .42 | 0.25 | .21 |
* Spearman rank order correlations were calculated between the change in ELISPOT response and the frequency of the specified T cells in the designated tissue compartment. Statistical significance was assessed using a two-sided t test. Change in ELISPOT = pre–radical prostatectomy ELISPOT – baseline ELISPOT. ELISPOT = enzyme-linked immunospot; PAP = prostatic acid phosphatase.
Discussion
Immunotherapy with sipuleucel-T is approved by the FDA for treatment of asymptomatic or minimally symptomatic metastatic CRPC. While the proposed mechanism of action of sipuleucel-T involves the induction of a T cell immune response targeting prostate cancer cells, the effects of sipuleucel-T at a tissue level have not been examined prior to this. This study demonstrates that neoadjuvant sipuleucel-T elicits both a systemic antigen-specific T cell response and results in the recruitment of activated effector T cells into the prostate tumor microenvironment.
These results demonstrate that neoadjuvant sipuleucel-T increases the frequency of CD3+ T cells within the prostate, particularly at the interface between benign and malignant glands. Quantitation of immune cells prior to treatment relied on stains from needle biopsies, which may be subject to sampling bias. Nevertheless, the recruitment of activated lymphocytes was not seen in the control cohort, which did not receive neoadjuvant therapy. It is not known if this recruitment of T cells also occurs in metastatic deposits of mCRPC patients treated with sipuleucel-T, or if this can account for the OS benefit that has been observed with sipuleucel-T in phase 3 mCRPC trials. However, infiltration of tumor tissues by T cells can be associated with improved clinical outcomes in many different malignancies (7,8). Specifically, recruitment of Th1 immune responses and effector/memory T cells represent favorable prognostic factors in the “immunoscore” that is being developed as a prognostic indicator for multiple malignancies (9,10). These findings are consistent with other immunotherapies, including anti-CTLA-4 and anti-PD-1 antibodies, that can also lead to enhanced recruitment of T cells to the tumor site (11,12). In this trial, digital microscopy was used in image analysis to enumerate the frequency of immune cells per unit area, rather than relying on more subjective grading (eg, 1+ to 4+). This approach allowed both the enumeration of immune cells within the prostate and the definition of the spatial compartments where these cells reside.
The concentration of immune cells at the tumor interface of prostate cancer patients treated with neoadjuvant sipuleucel-T is an intriguing observation. In the setting of colorectal cancer, infiltrating immune cells are typically localized to the tumor centers and the invasive margins, the latter of which would be analogous to the “tumor interfaces” described in this study (9,10). The concentration of immune cells at the tumor interface could potentially reflect the timing of treatments: The two to three weeks that separated the final sipuleucel-T infusion and the RP may have been insufficient to allow for migration into the tumor centers. Alternatively, components of the microenvironment may also preferentially position treatment-induced cells to specific locations within the prostate. These results also demonstrate the heterogeneous distribution of an immune infiltrate in the prostate. Indeed, the differences seen between biopsies and RPs could have been impacted by sampling error introduced by the biopsies. Nevertheless, the untreated cohort, which would have been subjected to the same sampling effect, did not have a similar change in T cell infiltration.
While other observational studies in prostate cancer have demonstrated that the presence of CD8 T cells in the tumor tissue may be prognostic of clinical outcome (13), our study shows that both CD8 and effector CD4 T cells were recruited to the tumor interface, which is a likely treatment effect. These cell types were preferentially recruited to prostate relative to Tregs. Our results do not, however, distinguish these effector T cells as Th1 or Th2 cells. CD8+ T cells present in the prostate have been previously shown to be oligoclonal and expressing PD-1, consistent with these cells being exhausted T cells (14). Neoadjuvant sipuleucel-T induced a statistically significant increase in the frequency of PD-1+ T cells at the tumor interface compared with the pretreatment biopsy (post-hoc test: P = .0001), but the presence of Ki-67 on the majority of the T cells indicated that they were not exhausted, but were proliferating perhaps to activation signals (eg, antigens) within the microenvironment.
In this study, correlation was observed between the immune responses seen in the RP tissues and peripheral immune responses measured at the time of resection by T cell proliferation or ELISPOT assays. This lack of correlation could reflect the limited number of patients with detectable systemic responses. Alternatively, antigen-specific T cells may have homed to the prostate tissues. The T cells recruited to the prostate could also be recognizing other antigens resulting from a cascading immune response that recognizes other antigens, referred to as epitope spreading. In any event, this observation raises issues as to the utility of using circulating immune responses from a single time-point measurement as a biomarker reflecting complex biological processes at the site of tumor deposits. In contrast, when induced changes in the circulating immune response between baseline and the time of surgery were considered, there were correlations with the magnitude of T cell infiltrates in the prostate, although these correlations were not consistent across all measures. These observations suggest that a more dynamic marker reflecting change over time in peripheral blood analytes might more accurately reflect changes at the level of tissue infiltrates. Future studies in larger cohorts assessing immune responses to such antigens and to a broader panel of prostate antigens may help further define the relevant circulating markers that correlate with responses within the tissue.
Assessing for the expression of immunologic cues that recruit immune cells within the tumor microenvironment could potentially help to identify patients who might respond to sipuleucel-T and perhaps other immunotherapies. Indeed, gene expression signatures associated with immune and/or clinical responses in other diseases that are being developed include different chemokines that contribute to T cell localization (15–17).
Because we are administering a treatment prior to planned definitive surgery, the time window between sipuleucel-T treatment and RP was narrow, which represents a potential limitation of our study. Evolution of the immune cell infiltration over time was not captured by our study. The tumor microenvironment in primary tumors is different from metastasis, so immune cell recruitment could be different in the advanced disease setting.
Nevertheless, these results also provide further rationale for combination trials using sipuleucel-T with other treatments that can augment T cell immunity, such as ipilimumab and cytokines, including IL-7 and IL-15. Moreover, the expression of PD-1 on the intraprostatic T cells induced by sipuleucel-T would also argue for combining this treatment with PD-1/PD-L1–targeting therapies (18). Finally, our results demonstrate how neoadjuvant trials with immunotherapies can provide opportunities for evaluating human immune responses in situ. Such an approach could be applied to other prostate cancer immunotherapies (19–21).
Funding
This study was sponsored by Dendreon Corporation. LF was also supported by the Peter Michael Foundation and a UCSF REAC Shared Equipment Grant. LF and SC were also supported by NIH 1R01 CA163012.
Supplementary Material
This paper was presented in part at the 2012 Genitourinary Cancers Symposium, 2012 ASCO Annual Meeting, 2012 European Society for Medical Oncology Annual Meeting, and 2012 Society for Immunotherapy of Cancer Annual Meeting.
We thank the patients and their families at the participating study sites, the clinical investigators on the study, and the contributions of Dendreon personnel in the conduct of these clinical studies. All authors contributed to the analysis and interpretation of the data, writing and editing of the manuscript, and approved the final version for submission. The study sponsor was involved in the design of the study as well as collection of the clinical data.
References
- 1. Small EJ, Schellhammer PF, Higano CS, et al. Placebo-controlled phase III trial of immunologic therapy with sipuleucel-T (APC8015) in patients with metastatic, asymptomatic hormone refractory prostate cancer. J Clin Oncol. 2006;24(19):3089–3094. [DOI] [PubMed] [Google Scholar]
- 2. Kantoff PW, Higano CS, Shore ND, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363(5):411–422. [DOI] [PubMed] [Google Scholar]
- 3. Sheikh NA, Petrylak D, Kantoff PW, et al. Sipuleucel-T immune parameters correlate with survival: an analysis of the randomized phase 3 clinical trials in men with castration-resistant prostate cancer. Cancer Immunol Immunother. 2013;62(1):137–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cooperberg MR, Pasta DJ, Elkin EP, et al. The University of California, San Francisco Cancer of the Prostate Risk Assessment score: a straightforward and reliable preoperative predictor of disease recurrence after radical prostatectomy. J Urol. 2005;173(6):1938–1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fong L, Brockstedt D, Benike C, et al. Dendritic cell-based xenoantigen vaccination for prostate cancer immunotherapy. J Immunol. 2001;167(12):7150–7156. [DOI] [PubMed] [Google Scholar]
- 6. Goc J, Fridman WH, Sautes-Fridman C, et al. Characteristics of tertiary lymphoid structures in primary cancers. Oncoimmunology. 2013;2(12):e26836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pages F, Kirilovsky A, Mlecnik B, et al. In situ cytotoxic and memory T cells predict outcome in patients with early-stage colorectal cancer. J Clin Oncol. 2009;27(35):5944–5951. [DOI] [PubMed] [Google Scholar]
- 8. Pages F, Berger A, Camus M, et al. Effector memory T cells, early metastasis, and survival in colorectal cancer. N Engl J Med. 2005;353(25):2654–2666. [DOI] [PubMed] [Google Scholar]
- 9. Ascierto PA, Capone M, Urba WJ, et al. The additional facet of immunoscore: immunoprofiling as a possible predictive tool for cancer treatment. J Transl Med. 2013;11:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Galon J, Pages F, Marincola FM, et al. Cancer classification using the Immunoscore: a worldwide task force. J Transl Med. 2012;10:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Huang RR, Jalil J, Economou JS, et al. CTLA4 blockade induces frequent tumor infiltration by activated lymphocytes regardless of clinical responses in humans. Clin Cancer Res. 2011;17(12):4101–4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Peng W, Liu C, Xu C, et al. PD-1 blockade enhances T-cell migration to tumors by elevating IFN-gamma inducible chemokines. Cancer Res. 2012;72(20):5209–5218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Karja V, Aaltomaa S, Lipponen P, et al. Tumour-infiltrating lymphocytes: A prognostic factor of PSA-free survival in patients with local prostate carcinoma treated by radical prostatectomy. Anticancer Res. 2005;25(6C):4435–4438. [PubMed] [Google Scholar]
- 14. Sfanos KS, Bruno TC, Meeker AK, et al. Human prostate-infiltrating CD8+ T lymphocytes are oligoclonal and PD-1+. Prostate. 2009;69(15):1694–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harlin H, Meng Y, Peterson AC, et al. Chemokine expression in melanoma metastases associated with CD8+ T-cell recruitment. Cancer Res. 2009;69(7):3077–3085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Messina JL, Fenstermacher DA, Eschrich S, et al. 12-Chemokine gene signature identifies lymph node-like structures in melanoma: potential for patient selection for immunotherapy? Sci Rep. 2012;2:765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ulloa-Montoya F, Louahed J, Dizier B, et al. Predictive gene signature in MAGE-A3 antigen-specific cancer immunotherapy. J Clin Oncol. 2013;31(19):2388–2395. [DOI] [PubMed] [Google Scholar]
- 18. Topalian SL, Drake CG, Pardoll DM. Targeting the PD-1/B7-H1(PD-L1) pathway to activate anti-tumor immunity. Curr Opin Immunol. 2012;24(2):207–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Small EJ, Tchekmedyian NS, Rini BI, et al. A pilot trial of CTLA-4 blockade with human anti-CTLA-4 in patients with hormone-refractory prostate cancer. Clin Cancer Res. 2007;13(6):1810–1815. [DOI] [PubMed] [Google Scholar]
- 20. McNeel DG, Dunphy EJ, Davies JG, et al. Safety and immunological efficacy of a DNA vaccine encoding prostatic acid phosphatase in patients with stage D0 prostate cancer. J Clin Oncol. 2009;27(25):4047–4054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kantoff PW, Schuetz TJ, Blumenstein BA, et al. Overall survival analysis of a phase II randomized controlled trial of a Poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J Clin Oncol. 2010;28(7):1099–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.