Abstract
Background
Anxiety and depression are recognised co-morbidities associated with COPD and have been related to poor health outcomes. Therapies to relieve anxiety and depression are currently not detailed in clinical guidelines.
Methods
A systematic review of psychological interventions for anxiety and depression in adults with COPD was conducted. Meta-analysis utilising the random effects model was undertaken for 4 studies that employed the same psychological intervention type, Cognitive Behavioural Therapy (CBT).
Results
Seven studies met the inclusion criteria. Four studies used CBT. Included studies utilised psychotherapy, uncertainty management and minimal psychological therapy. 70% of participants were male. Many studies had poor methodological quality. The meta-analysis showed a small decrease in symptoms for both anxiety (SMD −0.49, 95% CI −1.04, 0.06, P=0.08, n=193) and depression (SMD −0.37, 95% CI −0.86, 0.11, P=0.13, n=193). No change occurred when sensitivity analyses were conducted.
Conclusion
Anxiety and depression in COPD patients are known to impact on health outcomes. Effective psychological interventions such as CBT may assist people with COPD in reducing psychological burden. There remains a need for well-designed studies to provide substantive evidence for the use of psychological interventions in this patient population.
Introduction
Chronic obstructive pulmonary disease (COPD) is a major public health issue causing significant disability and mortality worldwide. With an estimated 64 million people affected globally, the WHO predicts that COPD prevalence will continue to increase, becoming the world's third major cause of death by 2030.1 In addition, people with chronic diseases such as COPD have comorbid and often multiple conditions that impact on treatment, disease progression and ultimately a patient's quality of life.2–4
The complex nature of COPD, along with multiple morbidities, contributes to significant health, social and economic costs for the individual, community and health services. 5 In people with COPD, comorbid anxiety and depression are often related to worse health outcomes, including higher rates of exacerbations, hospitalisation, readmissions and length of stay and reduced survival rates after emergency treatment.6 7 The prevalence of depression and anxiety has been found to be significantly higher in patients with COPD than in the general population, with studies estimating 40% and 36% for depression and anxiety rates, respectively.7 Although the precise mechanisms behind the high frequency of psychological disorders in COPD are not well understood, there appears to exist a complex inter-relationship between the patient's physiological and psychological states.4 8
Psychological dysfunction occurs both as a complication of COPD and as a symptom of this chronic disease.9 Depression has been proven to contribute to adverse immunological effects as well as to the characteristic systemic inflammation found in COPD.10 For people with COPD fear of having difficulty in breathing, coupled with continual physical distress and a prolonged loss of function are factors than can stimulate and provoke anxiety.11 Anxiety symptoms such as hyperventilation can, in turn, exacerbate dyspnoea.12 13 In both scenarios, the interactions may cause a worsening of the COPD patient's health status and quality of life, highlighting the importance of establishing evidence-based therapies to treat these mental health conditions.
The current treatment of COPD focuses on the minimisation of physical symptoms and may have limited attention to psychological symptoms despite the high prevalence of psychological dysfunction.14 15 Some studies suggest that the underdiagnosis and undertreatment of psychological disorders in COPD are still evident due to the ongoing complexity and inter-relationship of the physical and psychological pathologies.13 16 17 Therapeutic modalities such as pulmonary rehabilitation are often seen as evidence based interventions for COPD and its associated psychological comorbidities.8 18
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) treatment guidelines recommend treatment for these psychological morbidities, yet empirical evidence is lacking for their universal implementation.5 12 Furthermore, psychological interventions that are either stand-alone or part of a pulmonary rehabilitation are usually reported in terms of improved respiratory function and quality of life with limited reporting of specific mental health outcomes.19–21 There is no current review of psychological interventions for people with COPD to determine the evidence base for therapeutic interventions that may need to be incorporated into the COPD patient's clinical care and practice guidelines. The aim of this review was to assess the effectiveness of psychological interventions used to reduce clinical anxiety and depression in people with COPD.
Methods
Search strategy
After the development of a review protocol in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines,22 a comprehensive literature search of databases was conducted to identify relevant studies. The following electronic databases were searched from April to September 2013: PsychInfo, Cochrane, JBI, Medline, Pubmed, CINAHL, Embase, Sciencedirect, Google Scholar, Scopus and databases for theses and dissertations. Anticipating a paucity of studies on the review topic, a broad search strategy was employed to detect as many studies as possible. The database searches comprised the following combination of search terms to capture the target population: ‘chronic obstructive pulmonary disease’ OR ‘COPD’ OR ‘pulmonary disease’ OR ‘respiratory disease’. Symptoms of anxiety and depression terms included: ‘mental disorders’ OR ‘mental health’ OR ‘depression’ OR ‘anxiety’ OR ‘co-morbid psychological distress’ OR ‘psychological morbidity’ OR ‘stress’ OR ‘adjustment’ OR ‘coping’ OR ‘anxiety disorder’ OR ‘depressive disorder’ OR ‘psychopathology’. Intervention search terms comprised: ‘psychological interventions’ OR ‘psychosocial interventions’ OR ‘cognitive behavioural therapy’ OR ‘psychotherapy’ OR ‘supportive therapy’ OR ‘behavioural interventions’ OR ‘health education’ OR ‘counselling’ OR ‘self-care’ OR ‘self-management’ OR ‘pulmonary rehabilitation’ OR ‘relaxation’ OR ‘mindfulness’ OR ‘group therapy’ OR ‘visual imagery’ OR ‘behaviour management’ OR ‘psychodynamic therapies’ OR ‘psycho-educational therapies’. Indexed and free terms were used, with the search strategy being adapted to each database while maintaining the highest possible consistency in search logic. Search limits where applicable included English language, abstracts and humans and, in addition, reference lists of appropriate reviews and related articles were scanned for potential inclusion studies.
Eligibility criteria
Studies for inclusion in this review were required to be in the English language, published between the years 2000 and 2013, and meet participant, intervention, comparator and outcome (PICO) criteria. We included studies that were experimental or quasi-experimental of controlled comparative design. Participants were defined as adults (men and women aged 18 years and above) with a confirmed diagnosis of COPD, treated for symptoms of anxiety and depression. The primary COPD diagnosis and severity of the disease was to be determined by spirometry as defined by the GOLD standard.5 In the absence of spirometry confirmed COPD, studies that provided sufficient clinical documentation of COPD were also considered. Studies including individuals with psychiatric illnesses other than anxiety and/or depression, or other physical comorbidities were excluded.
For the purpose of this review, the following definition of psychological intervention was applied: ‘therapeutic actions that aim to address and modify behaviour, mood, emotional state and cognition in order to reduce symptoms of depression and anxiety’.23 Psychological interventions had to consist of a structured interaction between the patient and a healthcare facilitator trained in psychological techniques, where the intervention was centred primarily on evidence-based psychological practice.23 24 The delivery mode of the intervention included either individual or group sessions, both hospital ward and outpatient setting, and any length of time for follow-up. Mixed therapy interventions with a psychological component were only included if the independent effect of the psychological component could be determined. Studies that compared psychological interventions with inactive or active controls, such as usual care or an alternative intervention, were included.
The primary outcomes of interest for this review were evidence of reduction in symptoms of depression and/or anxiety following the administration of the psychological intervention. This outcome was measured by changes from baseline anxiety and depression scores to post-treatment scores, employing validated psychological assessment instruments.
Study selection and data extraction
Publication titles and abstracts were screened for eligibility by two independent reviewers (SS, SMS). Abstracts identified through the independent review process as potentially relevant articles were retrieved in full text. Full-text articles were subsequently reviewed independently (SS, SMS) using the predetermined inclusion and exclusion criteria. Any discrepancies and disagreements were resolved by discussion and a third party arbiter. Data were captured with the use of a standardised extraction form including bibliographical data, study type, participant information (sample size, patient health status and psychological morbidity), intervention (type, duration, frequency and delivery mode), control/comparison group and outcome data (baseline, post-treatment and follow-up measures).
Quality assessment
The quality of included studies was assessed by two reviewers independently (SS, SMS) and was included as part of the data extraction process and comprised assessment on risk bias and methodological quality. Assessment of risk bias was evaluated in the standard risk of bias domains: selection bias, performance bias, attrition bias, reporting bias and other sources of bias. The Critical Appraisal Skills Programme (CASP) checklists for risk of bias evaluation were used.25 The methodological quality of full-text articles was assessed employing checklists from the Scottish Intercollegiate Guidelines Network (SIGN).26
Data analysis
The Standardized Mean Difference (SMD) and corresponding 95% CI were calculated for continuous data that measured the same outcome utilising different assessment scales. The SMD is a useful indicator of an intervention's effect size, relative to the variability present in the study.27 Individual trial SMDs were calculated by subtracting the post-treatment mean of the control group from the post-treatment mean of the intervention group, divided by the pooled SD. In studies where there were several post-treatment follow-ups, the last follow-up measurements were used. Missing SDs that were not retrievable from the original authors were imputed from previously published analyses.28 29 Studies with imputed SDs or means were excluded from any meta-analyses. Revman V.4.2.2 software was used to perform meta-analyses of the four CBT studies. The random effects model was selected in view of the fact that the studies were not functionally equivalent and the true effect could not be assumed to be the same across studies. 27 30 Negative SMDs indicate an improvement in anxiety and depression symptoms, favouring the intervention. Typically, effect sizes of 0.20–0.30 are considered small, 0.50 medium and ≥0.80 large, based on Cohen's parameters.31
Results
Electronic database and secondary reference searches yielded 2117 records with 1738 remaining after removal of duplicates. From the initial title screenings, 214 potentially relevant articles were identified and these abstracts were subsequently reviewed. Of these, 168 abstracts were excluded as they failed to meet the predetermined inclusion criteria. Forty-six (46) publications were retrieved in full text for further assessment. Following a consensus meeting of the review authors, seven studies met the inclusion criteria as psychological interventions.
Overview of included studies
Studies included in this review were randomised controlled trials (RCT). The studies used a variety of psychological interventions over differing periods of time. Anxiety and depression outcome measures also varied between studies. Table 1 presents a summary of the characteristics of the included studies and baseline measurements.
Table 1.
Characteristics of included studies and baseline measurements
| First author, year, location and reference | Study design | Sample size (n) | Sex (% men) | Mean age | COPD severity (GOLD stage) | Anxiety outcomes measure | Depression outcomes measure | Baseline mean anxiety score | Baseline mean depression score |
|---|---|---|---|---|---|---|---|---|---|
| Psychological interventions | |||||||||
| de Godoy, 2003, Brazil32 | RCT | I=14 | I=85.7 | I=62.1 (SD 14.9) | Mild to severe (stage 1–3) | BAI | BDI | I=12.9 (SD 6.9) | I=13.7 (SD 8.9) |
| C=16 | C=62.5 | C=58.8 (SD 11.8) | C=10.9 (SD 9.8) | C=14.9 (SD 11.5) | |||||
| Hynninen, 2010, Norway33 | RCT | I=25 | I=56 | I=59.3 (SD 7.6) | Moderate to severe (stage 2–3) | BAI | BDI-II | I=17.5 (SD 7.3) | I=20.7 (SD 8.6) |
| C=26 | C=42.3 | C=62.6 (SD 9.9) | C=17.5 (SD 9.5) | C=20.5 (SD 9.7) | |||||
| Jiang, 2012, China34 | RCT | I=49 | I=71.4 | I=65.2 (SD 8.96) | Moderate to severe (stage 2–3) | SSAI, STAI | HADS-D | I=43.69 (SD 7.13), 42.91 (SD 6.78) |
I=7.16 (SD 3.02) |
| C=47 | C=68.1 | C=64.7 (SD 8.05) | C=42.83 (SD 7.25), 42.46 (SD 7.04) |
C=7.08 (SD 2.92) | |||||
| Kunik, 2001, USA 35 | RCT | I=21 | I=83 | I=71.3 (SD 5.9) | Moderate to severe (stage 2–3) | BAI | GDS | I=15.3 (SD 9.2) | I=11.5 (SD 7.3) |
| C=27 | C=83 | C=71.3 (SD 5.9) | C=10.0 (SD 6.8) | C=7.7 (SD 5.4) | |||||
| Kunik, 2008, USA36 | RCT | I=118 | I=96.6 | I=66.1 (SD 10.1) | Moderate to severe (stage 2–3) | BAI | BDI-II | I=22.67 (SD 14.22) | I=23.44 (SD 12.49) |
| C=120 | C=95.8 | C=66.5 (SD 10.4) | C=23.05 (SD 13.86) | C=21.12 (SD 12.09) | |||||
| Lamers, 2010, the Netherlands10 | RCT | I=96 | I=61.5 | I=70.5 (SD 6.3) | COPD severity not reported | SCL-A | BDI | I=20.6 (SD 6.2) | I=17.1 (SD 6.5) |
| C=91 | C=58.2 | C=71.5 (SD 7.1) | C=20.4 (SD 7.3) | C=18.3 (SD 7.2) | |||||
| Livermore, 2010, Australia37 | RCT | I=21 | I=43 | I=73.2 (SD 6.4) | Moderate to severe (stage 2–3) | HADS-A | HADS-D | I=5.2 (SD 2.9) | I=3.9 (SD 2.1) |
| C=20 | C=45 | C=73.5 (SD 8.1) | C=5.9 (SD 2.7) | C=4.1 (SD 2.8) | |||||
BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; BDI-II, Beck Depression Inventory 1996 revision; C, Control group; COPD, chronic obstructive pulmonary disease; GDS, Geriatric Depression Scale; GOLD, Global initiative for chronic Obstructive Lung Disease; HADS-A, Hospital Anxiety and Depression Scale—Anxiety subscale; HADS-D, Hospital Anxiety and Depression Scale—Depression subscale; I, Intervention group; RCT, randomised controlled trial; SCL-A, Anxiety subscale of the Symptom Checklist-90; SSAI, Speilberger's State Anxiety Inventory; STAI, State-Trait Anxiety Inventory.
Sample size, age and gender
The seven included studies totalled 691 participants. Sample sizes ranged from 30 to 238, with a mean sample size of 98.7. In all, 74.1% of participants were men, and the mean age ranged from 58.8 to 73.5 years.
Assessment of COPD diagnosis and severity
Six studies confirmed the diagnosis and assessed COPD severity by spirometry, utilising the GOLD criteria to determine the stage of severity.32–37 Of these, two studies also required confirmation by clinical records32 or the physician's referral.37 One study10 did not report COPD severity; in this study, COPD diagnosis was confirmed by a general practitioner. The majority of participants recruited in the included studies were classified between moderate and severe33–37 (GOLD stages 2–3), and one study included participants in the mild to severe range32 (GOLD stage 1–3).
Assessment of anxiety and depression
Anxiety and depression outcomes were assessed by various instruments as shown in table 1. According to the corresponding cut-off scores for each assessment scale,38 39 the baseline mean scores for anxiety suggested that participants had mild to moderate anxiety in five studies10 32–35; one study indicated moderate to severe anxiety,36 and one study was indicative of normal or non-clinically significant anxiety.37 Utilising the guidelines for each depression assessment instrument,40 41 the baseline mean scores indicated that one study was within normal ranges,37 two studies had normal to mild depression scores,34 35 two studies were in the mild to moderate range,10 32 and two studies were in the moderate to severe depression range.33 36
Sample selection and study design
Participants in the included studies were primarily recruited from hospital outpatient pulmonary clinics; one study recruited patients from general practices10 and another from a university respiratory research department. 32 With the exception of one study,10 the trials were conducted in outpatient settings and based in a diverse range of countries. All seven study designs were described as RCT. All studies compared a psychological intervention with an inactive control, such as standard care or education. Only three of the seven studies required participants to have clinically significant symptoms of anxiety or depression to be included in the study.10 33 36 The majority of studies excluded participants with more severe psychological disorders such as panic disorder or major depression. Five studies specified moderate to severe COPD severity as criteria for inclusion,33–37 while two studies included all levels of severity.10 32
Overview of interventions
Table 2 outlines the characteristics of the psychological interventions reported in the included studies.
Table 2.
Characteristics of psychological interventions
| First author, year, reference | Sampling and setting | Intervention | Control group | Intervention components | Number of sessions | Session duration (min) | Frequency | Delivered by | Delivery method | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|
| Psychological interventions | ||||||||||
| de Godoy, 200332 | Patients with COPD referred from the University Department of Respiratory Diseases to attend an outpatient pulmonary rehabilitation group | Psychotherapy integrated into the pulmonary rehabilitation program | Pulmonary rehabilitation program without psychotherapy | Addressing patients’ psychosocial needs, social, marital, work, health, interpersonal philosophy, habits. Cognitive and logotherapy techniques were used |
12 | Not reported | Once per week over 12 weeks | Not reported | Not reported | Assumed to be after 12 weeks |
| Hynninen, 201033 | Patients with COPD recruited from an outpatient pulmonary clinic at a University hospital and by newspaper advertisement | CBT | Enhanced standard care | Psychoeducation/awareness, relaxation, cognitive therapy, behavioural activation, fear-based exposure, sleep management skills | 7 | 120 | Once per week over 7 weeks | Masters-level psychology student, sessions videotaped and monitored by a specialist in clinical psychology | Group session of 4–6 participants | 2 months and 8 months |
| Jiang, 201234 | Han Chinese COPD outpatients recruited at Xiangya Hospital of Central South University | Uncertainty management | Standard care | Cognitive coping strategies on uncertainty regarding exacerbations delivered on audio CD, self-help manual on behavioural strategies, COPD education, management skills, instructional booklet and cards, four telephone contacts delivered by nurses in first 4 weeks where one cognitive coping skill was practised over the phone | 4 | 35 | Once per week over 4 weeks | Intervention nurses | Individual—by phone call | 10 months |
| Kunik, 200135 | Patients with COPD recruited from an academically affiliated Veterans Affairs Hospital and local newspaper | CBT | COPD education | Education on role of psychological distress in chronic illness, components of anxiety, cognitive behaviour skills in coping such as relaxation, diaphragmatic breathing, posture, exposure to anxiety provoking situations. Provision of workbooks and audiotapes to review skills and practice exercises | 1 | 120 | Once only | Board-certified geropsychiatrist | Group session | 1 call per week for 6 weeks post-treatment |
| Kunik, 200836 | Patients with COPD identified and recruited through an administrative database at the attended medical centre and flyer and advertisement methods | CBT | COPD education | Psycho-education/awareness on physiological, cognitive and behavioural symptoms of anxiety and depression, relaxation, cognitive therapy, problem solving, sleep management, increasing pleasurable activity, decreasing anxiety-related avoidance | 8 | 60 | Once over week over 8 weeks | Psychology interns and post-doctoral fellows with experience in CBT | Group sessions of up to 10 patients | 4, 8 and 12 weeks |
| Lamers, 201010 | Patients with COPD recruited from general practices. Home setting | Minimal psychological intervention | Usual care | Nurse-led intervention addressing the patient's feelings, cognitions and behaviours, patient diary keeping, awareness of mood relation to behaviour, self-management training to alter behaviour, action plans | 4 (average) tailored to individual patients | 60 | Varied number of sessions over a period of at most 3 months | Nurses trained by a GP, psychologist and psychiatrist | Individual | 3 months |
| Livermore, 201037 | Patients with COPD identified in the respiratory medicine department outpatient clinic of the teaching hospital | CBT | Routine care | Psycho-education, awareness of stress response on breathing, cycle of panic anxiety, cognitive challenging of negative thoughts, pursed lip breathing, activity planning, pacing and problem solving | 4 | 60 | Once per week over 4 weeks | Experienced clinical psychologist | Individual | 6, 12 and 18 months |
CBT, cognitive behaviour therapy; COPD, chronic obstructive pulmonary disease; GP, general practitioner; PR, pulmonary rehabilitation.
Among the seven included studies, four compared the effectiveness of CBT with standard care or education,33 35–37 while three employed other psychological therapies: psychotherapy, uncertainty management and minimal psychological intervention, in comparison to standard care. 10 32 34 Among the CBT studies, there was consistency in the intervention components; however, there was significant variability in relation to the number of sessions, frequency, delivery mode and follow-up. The number of intervention sessions for all studies ranged between 1 and 12 sessions. The intervention duration ranged from 1 day to 3 months and follow-up periods varied between 1 and 18 months. A wide range of healthcare professionals including psychologists, psychiatrists and nurses administered the psychological interventions. Three trials administered the intervention individually10 34 37 and three were administered in group sessions.33 35 36 Across all studies, there was high diversity in the psychological intervention type, duration, follow-up periods and delivery methods.
Quality assessment
The assessment for risk of bias was completed for all included studies. The majority of studies had low risk in the randomisation process, with the exception of one study,32 where the risk was unclear as randomisation was not described. Allocation concealment methods were only reported by two studies.33 37 Blinding of participants and personnel was an identified weakness in six of the seven studies.10 32 34–37 Incomplete outcome data were identified in three studies.10 36 37 Selective reporting was not found as all a priori analyses were reported.
Effects of psychological interventions on anxiety and depression
A summary of outcomes and individual SMDs for each study is shown in table 3. Overall, the individually calculated SMDs appear to suggest that the treatment effect direction favours psychological interventions for anxiety and depression; however, it is critical to note that the SMD values represent the separate effects of each study, and it is not possible to assert conclusions about the interventions’ summary effect.30 The size of the separate treatment effects and their significance are varied, with most values found within the small to medium effect range, and only one large effect size estimated for anxiety in the Jiang 2012 study.34
Table 3.
Effect of psychological interventions for COPD on symptoms of anxiety and depression at post-treatment
| First author, | Post-treatment mean (SD) |
|||||
|---|---|---|---|---|---|---|
| year, reference | Comparison | Outcome | Intervention | Control | SMD (95% CI) | Outcomes summary |
| de Godoy, 200332 | PR with Psychotherapy vs PR without Psychotherapy | Anxiety (BAI) | 4.2 (3.8) | 9.2 (8.6) | −0.73 (−1.48 to 0.01) | Intervention group showed significant reduction in anxiety and depression levels; however, it did not modify physical performance |
| Depression (BDI) | 5.0 (4.5) | 12.3 (11.8) | −0.08 (−1.54 to −0.05) | |||
| Hynninen, 201033 | CBT vs Enhanced standard care | Anxiety (BAI) | 11.0 (6.1) | 18.7 (10.1) | −0.53 (−1.08 to 0.03) | CBT intervention group significantly reduced symptoms of anxiety and depression. No significant changes in control group |
| Depression (BDI-II) | 13.4 (5.9) | 19.7 (8.9) | −0.54 (−1.10 to 0.02) | |||
| Jiang, 201234 | Uncertainty management vs Standard care | Anxiety (SSAI, STAI) | 31.53 (5.74), 31.37 (5.19) |
41.25 (6.86), 40.95 (7.15) |
−1.54 (−1.99, −1.09), −1.54 (−1.99 to −1.09) |
Compared to the control group, the intervention group showed significant improvement in anxiety and depression scores and QoL |
| Depression (HADS-D) | 5.64 (2.24) | 6.62 (2.47) | −0.17 (−0.56 to 0.22) | |||
| Kunik, 200135 | CBT vs COPD education | Anxiety (BAI) | 12.6 (8.7) | 11.9 (7.6) | 0.07 (−0.50 to 0.64) | CBT intervention group showed decreased depression and anxiety scores compared to control group. No change in physical functioning |
| Depression (GDS) | 9.4 (6.5) | 8.8 (7.6) | 0.08 (−0.49 to 0.65) | |||
| Kunik, 200836 | CBT vs COPD education | Anxiety (BAI) | 15.89 (14.87) | 17.46 (14.54) | −0.11 (−0.46 to 0.25) | Both intervention and control groups significantly improved anxiety and depression and QoL, with no significant difference between intervention groups |
| Depression (BDI-II) | 14.19 (13.69) | 14.54 (13.47) | −0.03 (−0.38 to 0.33) | |||
| Lamers, 201010 | Minimal psychological intervention vs Usual care | Anxiety (SCL-A) | 19.85 (0.87) | 23.54 (0.84) | −0.12 (−0.46 to 0.23) | Intervention group showed lower symptoms of anxiety and depression compared to control group. Intervention group also improved QoL measures |
| Depression (BDI) | 15.04 (1.00) | 17.96 (0.96) | −0.29 (−0.64 to 0.06) | |||
| Livermore, 201037 | CBT vs Routine care | Anxiety (HADS-A) | 3.6 (2.9) | 7.9 (4.1) | −0.71 (−1.35 to −0.08) | CBT intervention group reduced anxiety symptoms and panic attacks compared to control group |
| Depression (HADS-D) | 2.9 (2.6) | 6.3 (4.6) | −0.63 (−1.25 to 0.00) | |||
BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; BDI-II, Beck Depression Inventory 1996 revision; CBT, cognitive behaviour therapy; COPD, chronic obstructive pulmonary disease; GDS, Geriatric Depression Scale; GOLD, Global initiative for chronic Obstructive Lung Disease; HADS-A, Hospital Anxiety and Depression Scale—Anxiety subscale; HADS-D, Hospital Anxiety and Depression Scale—Depression subscale; PMR, Progressive Muscle Relaxation; PR, Pulmonary Rehabilitation; QoL, Quality of Life; SCL-A, Anxiety subscale of the Symptom Checklist-90; SMD, Standardized Mean Difference; SSAI, Speilberger's State Anxiety Inventory; STAI, State-Trait Anxiety Inventory.
The meta-analyses of the four CBT studies for anxiety and depression are shown in figures 1 and 2, respectively. The CBT studies favoured the direction of the intervention, showing small improvements in symptoms of anxiety (SMD −0.49, 95% CI −1.04 to 0.06, p=0.08, n=193) and depression (SMD −0.37, 95% CI −0.86 to 0.11, p=0.13, n=193). Statistically significant heterogeneity was found in both analyses (I2=80% and 74%) and the treatment direction showed no change when sensitivity analyses were conducted by the systematic removal of each study.
Figure 1.
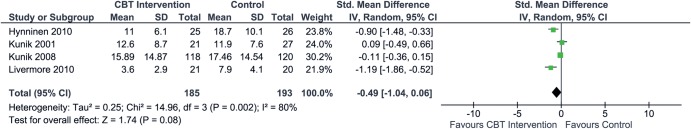
Effects of cognitive behaviour therapy (CBT) interventions on symptoms of anxiety in chronic obstructive pulmonary disease (COPD). Random effects model used. SMD, Standardised Mean Difference.
Figure 2.
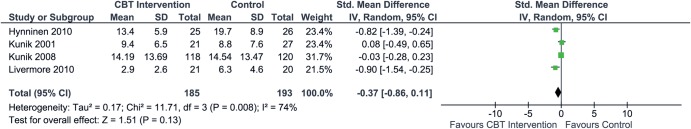
Effects of cognitive behaviour therapy (CBT) interventions on symptoms of depression in chronic obstructive pulmonary disease (COPD). Random effects model used. SMD, Standardised Mean Difference.
Discussion
This review of psychological interventions for people with COPD identified a number of studies that report a variety of interventions. The outcomes from these studies suggest that the psychological interventions understudy resulted in positive outcomes for participants in most cases. Four studies of cognitive behavioural therapy (CBT)33 35–37 reported improvements in the psychological status and quality of life.
The comparison of 8 weeks of 1 h education sessions with 8 weeks of 1 h CBT in Kunik et al's36 study resulted in an improvement in the quality of life scores and the psychological indices; however, no difference between groups was found at either 8 or 44 weeks. This finding may suggest face-to-face delivery by a health professional of information or techniques may play a role in the success of an intervention. Moreover, De Godoy's study32 suggests that the addition of psychotherapy to pulmonary rehabilitation may be useful in improving COPD patients’ psychological status, although the sample size was small and the reported results have wide SDs, which is suggestive of imprecision. Education, psychotherapy and CBT require few resources apart from a quiet environment and may be more easily adapted to home environments for people with COPD. For this reason, there is a need for well-designed studies that are appropriately powered to confirm the interventions that improve psychological outcomes and to identify the most suitable setting for the delivery of these interventions.
People with different levels of depressive symptoms may respond differently to interventions; however, participants reported similar levels of depressive symptoms at baseline in all but one study where levels were within normal limits37 Mean scores for other studies are close to the mild/moderate cut-off point and, assuming a normal distribution, this suggests that a substantial number of participants reported a moderate level of depressive symptoms. The magnitude of change in depressive symptoms was modest, although it was consistently positive in all studies regardless of the intervention.
Four of the seven studies used a usual care or standard care control group. When examining the effects of a behavioural or psychological intervention, it is important to use an active control group to control for the effects of attention given to participants. This is a limitation of this research, especially when self-report instruments are used, and highlights the issue when an intervention that has multiple sessions with patients is compared to usual care where patients often have a reduced interaction with health professionals. It is interesting to note that results for CBT and COPD education were not significantly different, suggesting that COPD education may have a positive effect on depressive symptoms.36 Studies reported in this review were conducted in six different countries, and it is not possible to tease out the cultural differences; however, this issue cannot be ignored.
From a clinical perspective, this review found that participants had high baseline scores for anxiety and depression, which may suggest the need for anxiety and depression screening within routine COPD assessment, and for the incorporation of proven psychological interventions as part of standard care. An assessment of the impact of psychological screening on patients, their care and its delivery within the health service needs to be considered along with an economic evaluation. Owing to the proportion of male participants with COPD (74.1%) identified in this review, from a gender perspective, the generalisation of the findings is limited. Other limitations associated with this review include the small number of trials identified (n=7), significant heterogeneity (due to the intervention modes, frequency of delivery, participants), risk of bias and the potential for an overestimation of effect. Furthermore, the short duration of the included studies may contribute to the difficulty in interpreting the long-term benefits of psychological interventions. There is a need for further research to address these limitations to enable consideration for the implementation of evidence-based psychological techniques and interventions in clinical care guidelines for this chronic disease population.
Conclusion
This review and meta-analysis report that there is potential for psychological interventions to reduce anxiety and depression in people with COPD. Limitations identified through this review were the small sample sizes of studies, heterogeneity of interventions and outcome measures. Psychological interventions such as cognitive behavioural therapy, psychotherapy and other minimal psychological interventions require further research through well-designed and appropriately powered studies before inclusion in COPD guidelines or clinical care. This review found high levels of psychological morbidity being reported and this highlights the potential for future studies to examine screening for psychological morbidity in this patient population. Furthermore, research is required to determine the most appropriate setting for the delivery of effective psychological interventions to ensure maximum benefit to patients with COPD.
Footnotes
Contributors: All authors were involved in the study design and data interpretation and contributed to the writing of the manuscript.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.World Health Organization. Global burden of disease. Secondary Global burden of disease 01/06/2013 2004. http://www.who.int/healthinfo/global_burden_disease/publications/en/index.html
- 2.Marinho P, Castro C, Raposo C et al. . Depressive symptoms, inflammatory markers and body composition in elderly with and without chronic obstructive pulmonary disease (COPD). Arch Gerentol Geriatr 2012;54:453–8. [DOI] [PubMed] [Google Scholar]
- 3.Kuhl K, Schurmann W, Rief W. Mental disorders and quality of life in COPD patients and their spouses. Int J Chron Obstruct Pulmon Dis 2008;3:727–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J 2009;33:1165–85. [DOI] [PubMed] [Google Scholar]
- 5.Global Initiative for Chronic Obstructive Lung Disease. Management and prevention of chronic obstructive pulmonary disease. Secondary management and prevention of chronic obstructive pulmonary disease 2010.
- 6.Dahlén I, Janson C. Anxiety and depression are related to the outcome of emergency treatment in patients with obstructive pulmonary disease. Chest 2002;122:1633–7. [DOI] [PubMed] [Google Scholar]
- 7.Yohannes A, Baldwin R, Connolly M. Mood disorders in elderly patients with chronic obstructive pulmonary disease. Rev Clin Gerentology 2000;10:193–202. [Google Scholar]
- 8.Burgess A, Kunik M, Stanley M. Chronic obstructive pulmonary disease: assessing and treating psychological issues in patients with COPD. Geriatrics 2005;60:18–21. [PubMed] [Google Scholar]
- 9.Hynninen M, Pallesen S, Nordhus I. Factors affecting health status in COPD patients with co-morbid anxiety or depression. Int J Chron Obstruct Pulmon Dis 2007;2:323–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Lamers F, Jonkers CC, Bosma H et al. . Improving quality of life in depressed COPD patients: effectiveness of a minimal psychological intervention. COPD 2010;7:315–22. [DOI] [PubMed] [Google Scholar]
- 11.Rose C, Wallace L, Dickson R et al. . The most effective psychologically-based treatments to reduce anxiety and panic in patients with chronic obstructive pulmonary disease (COPD): a systematic review. Patient Educ Couns 2002;47:311–18. [DOI] [PubMed] [Google Scholar]
- 12.Cafarella PA, Effing TW, Usmani ZA et al. . Treatments for anxiety and depression in patients with chronic obstructive pulmonary disease: a literature review. Respirology 2012;17:627–38. [DOI] [PubMed] [Google Scholar]
- 13.Cully J, Graham D, Stanley M et al. . Quality of life in patients with chronic obstructive pulmonary disease and comorbid anxiety or depression. Psychosomatics 2006;47:312–19. [DOI] [PubMed] [Google Scholar]
- 14.Jacobs J, Lisdonk Evd, Smeele I et al. . Management of patients with asthma and COPD: monitoring quality of life and the relationship to subsequent GP interventions. Fam Pract 2001;18:574–80. [DOI] [PubMed] [Google Scholar]
- 15.Stanley MA, Veazey C, Hopko D et al. . Anxiety and depression in chronic obstructive pulmonary disease: a new intervention and case report. Cogn Behav Pract 2005;12:424–36. [Google Scholar]
- 16.Kim H, Kunik M, Molinari V et al. . Functional impairment in COPD patients: the impact of anxiety and depression. Psychosomatics 2000;41:465–71. [DOI] [PubMed] [Google Scholar]
- 17.Laurin C, Moullec G, Bacon S et al. . The impact of psychological distress on exacerbation rates in COPD. Ther Adv Respir Dis 2011;5:3–18. [DOI] [PubMed] [Google Scholar]
- 18.Lacasse Y, Goldstein R, Lasserson T et al. . Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2006;18:1–7. [DOI] [PubMed] [Google Scholar]
- 19.Baraniak A, Sheffield D. The efficacy of psychologically based interventions to improve anxiety, depression and quality of life in COPD: a systematic review and meta-analysis. Patient Educ Couns 2011;83:29–36. [DOI] [PubMed] [Google Scholar]
- 20.Norweg A, Whiteson J, Malgady R et al. . The effectiveness of different combinations of pulmonary rehabilitation program components: a randomized controlled trial. Chest 2005;128:663–72. [DOI] [PubMed] [Google Scholar]
- 21.Putman-Casdorph H, McCrone S. Chronic obstructive pulmonary disease, anxiety, and depression: state of the science. Heart Lung 2009;38:34–47. [DOI] [PubMed] [Google Scholar]
- 22.Liberati A, Altman DG, Tetzlaff J et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Psychological Association. Presidential task force on evidence-based practice in psychology 2005 policy statement. Secondary Presidential task force on evidence-based practice in psychology 2005 policy statement 2005.
- 24.Pai A, Drotar D, Zebracki K et al. . A meta-analysis of the effects of psychological interventions in pediatric oncology on outcomes of psychological distress and adjustment. J Pediatr Psychol 2006;31:978–88. [DOI] [PubMed] [Google Scholar]
- 25.Critical Appraisal Skills Programme. Critical Appraisal Skills Programme: Making sense of evidence. Secondary Critical Appraisal Skills Programme: Making sense of evidence 2013. http://www.casp-uk.net/
- 26.Scottish Intercollegiate Guidelines Network. Critical appraisal: Notes and checklists. Secondary Critical appraisal: Notes and checklists 2014. http://www.sign.ac.uk/methodology/checklists.html
- 27.Deeks J, Higgins J, Altman D. Chapter 9: analysing data and undertaking meta-analyses. In: Higgins J, Green S, eds. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons Ltd. 2008:243–93. [Google Scholar]
- 28.Coventry PA, Bower P, Keyworth C et al. . The effect of complex interventions on depression and anxiety in chronic obstructive pulmonary disease: systematic review and meta-analysis. PLoS ONE 2013;8:e60532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coventry PA, Gellatly JL. Improving outcomes for COPD patients with mild-to-moderate anxiety and depression: a systematic review of cognitive behavioural therapy. Br J Health Psychol 2008;13:381–400. [DOI] [PubMed] [Google Scholar]
- 30.Borenstein M, Hedges LV, Higgins JPT. Introduction to meta-analysis. Hoboken, NJ: John Wiley & Sons, 2009. [Google Scholar]
- 31.Cohen J. Statistical power analysis for the behavioral sciences. 2nd edn: Lawrence Erlbaum Associates, 1988. [Google Scholar]
- 32.de Godoy DV, de Godoy RF. A randomized controlled trial of the effect of psychotherapy on anxiety and depression in chronic obstructive pulmonary disease. Arch Phys Med Rehabil 2003;84:1154–7. [DOI] [PubMed] [Google Scholar]
- 33.Hynninen M, Bjerke N, Pallesen S et al. . A randomized controlled trial of cognitive behavioral therapy for anxiety and depression in COPD. Respir Med 2010;104:986–94. [DOI] [PubMed] [Google Scholar]
- 34.Jiang X, He G. Effects of an uncertainty management intervention on uncertainty, anxiety, depression, and quality of life of chronic obstructive pulmonary disease outpatients. Res Nurs Health 2012;35:409–18. [DOI] [PubMed] [Google Scholar]
- 35.Kunik ME, Braun U, Stanley MA et al. . One session cognitive behavioural therapy for elderly patients with chronic obstructive pulmonary disease. Psychol Med 2001;31:717–23. [DOI] [PubMed] [Google Scholar]
- 36.Kunik ME, Veazey C, Cully JA et al. . COPD education and cognitive behavioral therapy group treatment for clinically significant symptoms of depression and anxiety in COPD patients: a randomized controlled trial. Psychol Med 2008;38:385–96. [DOI] [PubMed] [Google Scholar]
- 37.Livermore N, Sharpe L, McKenzie D. Prevention of panic attacks and panic disorder in COPD. Eur Respir J 2010; 35:557–63. [DOI] [PubMed] [Google Scholar]
- 38.Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S467–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spielberger C, Gorsuch R, Lushene R et al. . Manual for the state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press, 1983. [Google Scholar]
- 40.Smarr KL, Keefer AL. Measures of Depression and Depressive Symptoms Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthrtitis Care and Research (Hoboken) 2011;63(Suppl 11):S454–66. [DOI] [PubMed] [Google Scholar]
- 41.Beck A, Steer R, Garbin M. Psychometric properties of the Beck Depression Inventory twenty-five years of evaluation. Clin Psychol Rev 1988;8:77–100. [Google Scholar]


