Abstract
A posterior rectus sheath hernia is an abdominal wall hernia that is rarely encountered. Owing to its rarity, it can be easily overlooked in the setting of a patient presenting with abdominal pain. We report a case of a posterior rectus sheath hernia that caused intermittent small bowel obstruction. The unusual aspects of this case are that the defect was large, measuring 6 cm in the transverse diameter, and that it contained small bowel within a large portion of the rectus sheath. Because the defect was large and affected nearly the entire posterior rectus sheath, it was difficult to discern on computed tomography until a small bowel obstruction developed. In this case, a limited awareness of this clinical entity contributed to the delay in diagnosis.
Keywords: CT, abdomen, hernia, rectus sheath, small bowel obstruction, abdominal pain
CASE REPORT
History
A 51-year-old African-American female with a prior history of a remote partial hysterectomy but an otherwise unremarkable surgical history presented to the emergency department with abdominal pain for approximately 24 hours. The medical records from this remote hysterectomy were not available for review. She reported a long history of intermittent abdominal pain over the span of several years which had been treated conservatively.
Imaging Findings
A supine abdominal radiograph was performed that showed several mildly dilated loops of small bowel (Fig. 1). Abdominal computed tomography (CT) with enteric contrast showed dilatation of multiple jejunal loops and a focal transition point in the right side of the pelvis that was consistent with a small bowel obstruction (Fig. 2). She was observed for one day while undergoing conservative treatment and then discharged the following day after her symptoms resolved. She was admitted to the emergency department several months later with abdominal pain that was similar in character to her prior admission. This time, the abdominal CT without enteric contrast was reported as normal (Fig. 3). She was again managed conservatively and discharged after her symptoms resolved.
Figure 1.
51 year old female with a posterior rectus sheath hernia.
FINDINGS: Supine abdominal radiograph shows a dilated loop of bowel in the upper abdomen (arrow), a nonspecific finding.
TECHNIQUE: Supine abdominal radiograph.
Figure 2.
51 year old female with a posterior rectus sheath hernia.
FINDINGS: Axial multidetector CT of the abdomen (a), sagittal reconstruction (b), and magnified axial view (c) with intravenous and oral contrast show multiple dilated loops of small bowel consistent with a small bowel obstruction. In retrospect, these small bowel loops extend through a large defect in the posterior rectus sheath (arrows).
TECHNIQUE: GE Lightspeed VCT. Axial CT with sagittal reconstruction, 654 mA, 120 kV, 5 mm axial mm slices, 3 mm sagittal reconstructions, Oral contrast-Omnipaque 240 50 ml + 850 ml water, IV contrast-Isovue-370 100 ml
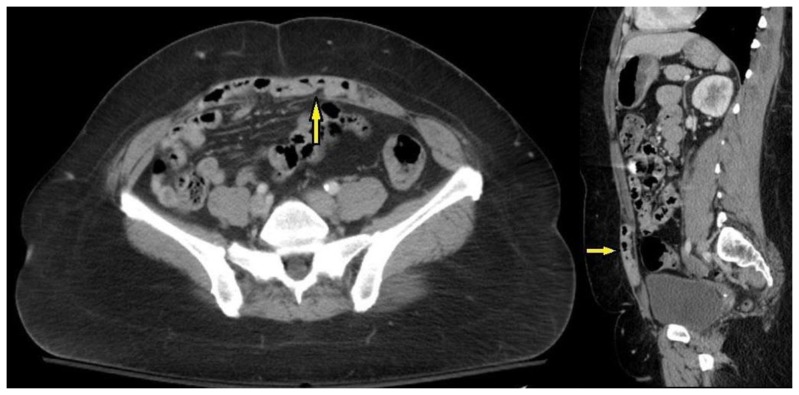
Figure 3.
51 year old female with a posterior rectus sheath hernia.
FINDINGS: Axial multidetector CT of the abdomen (a), sagittal reconstruction (b), and magnified axial view (c) with intravenous contrast only were read as normal. In retrospect, a large posterior rectus sheath defect contains multiple loops of small bowel (arrows) although no small bowel obstruction is present.
TECHNIQUE: GE Lightspeed VCT. Axial CT with sagittal reconstruction, 704 mA, 120 kV, 3 mm axial slices, 5 mm sagittal reconstructions, Oral contrast-none, IV contrast-Isovue-370 100 ml.
After two months, the patient presented with severe abdominal pain and emesis. An abdominal CT with enteric contrast during this admission showed multiple dilated loops of small bowel and re-demonstration of a transition point in the bowel that localized inferior to a defect in the posterior rectus sheath that measured 6 cm in transverse diameter (Fig. 4).
Figure 4.
51 year old female with a posterior rectus sheath hernia.
FINDINGS: Axial multidetector CT of the abdomen (a), sagittal reconstruction (b), and magnified axial view (c) with intravenous and oral contrast show multiple dilated loops of small bowel consistent with a small bowel obstruction. The small bowel loops herniate through a large defect in the posterior rectus sheath fascia and abut the anterior abdominal wall (arrows).
TECHNIQUE: GE Lightspeed VCT. Axial CT with sagittal reconstruction, 654 mA, 120 kV, 3 mm axial slices, 5 mm sagittal reconstructions, Oral contrast-Omnipaque 240 50 ml + 850 ml water, IV contrast-Isovue-370 100 ml.
Management and Follow-Up
Her symptoms did not improve with conservative treatment and an exploratory laparotomy confirmed the presence of several centimeters of strangulated small bowel within the posterior rectus sheath defect. The ischemic small bowel was resected followed by primary closure of the posterior rectus sheath defect. No intra-operative photographs were taken at the time of surgery. The patient had an uneventful post-operative recovery and approximately 18 months later she has not experienced a recurrent small bowel obstruction.
DISCUSSION
Etiology and Demographics
A posterior rectus sheath hernia is an extremely rare hernia of the anterior abdominal wall. Since the first description of a posterior rectus sheath hernia by Lopez in 1937, only nine cases have been reported. The age ranged from 25–83 with a mean of 50 years and 62% female patients[1]. Of the nine previously reported cases, the largest defect in the posterior rectus sheath measured 2 cm [1]. The majority of reported posterior rectus sheath hernias are either post-traumatic or post-surgical but a congenital defect of the posterior rectus sheath has accounted for a few cases. Rectus muscle and sheath differentiation begins in the human fetus at approximately 6 weeks, with formation of the anterior sheath first. The posterior rectus sheath develops from fascial laminae arising from the internal oblique and transversus abdominis muscles by 8–9 weeks [2].
A hernia of the posterior rectus sheath is rare because the sheath is comprised of strong connective tissue that forms a barrier to the herniation of abdominal contents. The weakest location of the posterior rectus sheath is inferior to the arcuate line, where the posterior rectus sheath is primarily composed of transversalis fascia [1]. The arcuate line is located at approximately one third of the distance between the umbilicus and the pubic crest. The posterior rectus sheath superior to the arcuate line is stronger because it is formed by the aponeurosis of the transversus abdominis muscle and the posterior aponeurosis of the internal oblique muscle [1, 3].
The largest reported posterior rectus sheath hernia prior to this case measured about 2 cm in the transverse diameter [1, 3, 4]. The unique findings in our patient are the large size of the defect, which measured 6 cm in transverse diameter, the involvement of the entire diameter of the infra-umbilical abdominal wall, and that small bowel filled nearly the entire hernia. These have not been typical features in previously reported cases. The patient had a remote history of cesarean section. However, the hernia defect was higher than the site of surgery, making it likely that this hernia was due to a congenital defect in the posterior rectus sheath.
Clinical and Imaging Findings
Abdominal wall hernias are a common surgical problem in the United States with more than one million abdominal wall hernia repairs performed annually [5, 6]. These defects often involve protrusion of abdominal contents through the abdominal wall fascia or musculature. They can be difficult to diagnose clinically since symptoms are frequently nonspecific or difficult to localize. Increased utilization of cross-sectional imaging, particularly CT, has dramatically improved diagnosis and subsequent management of patients with other types of abdominal wall hernias such as incisional, inguinal, femoral, and umbilical [4, 7].
Treatment and Prognosis
Diagnosis of a posterior rectus sheath hernia may be delayed owing to its rarity and lack of familiarity by clinicians, surgeons, and radiologists. Only three cases of rectus sheath hernias diagnosed by computed tomography have been reported [3]. The treatment of a posterior rectus sheath hernia is surgical with primary closure being preferred over prosthetic repair since the latter has an increased risk of intestinal strangulation [1]. The most devastating complication of an abdominal wall hernia is incarceration of small bowel that can result in an obstruction and potentially bowel strangulation if left untreated.
Differential Diagnosis
A lack of familiarity and the unusual anterior abdominal wall anatomy resulted in delayed diagnosis of the posterior rectus sheath hernia until it caused a small bowel obstruction, which was evident on the CT examination when bowel ischemia became irreversible. The differential diagnosis of this case would be a small bowel obstruction related to another cause such as an adhesion or obstructing mass, an abdominal wall hernia in another location, or an ileus.
TEACHING POINT
A posterior rectus sheath hernia is a rare but important diagnosis that can cause small bowel obstruction and should be considered in patients with unexplained intermittent abdominal pain. CT shows a defect in the posterior rectus sheath with bowel protruding anteriorly and abutting the rectus musculature.
Table 1.
Summary table of posterior rectus sheath hernia
| Etiology | Most often related to prior surgery or adhesions. Rarely caused by a congenital defect of the posterior rectus sheath |
| Incidence | Unknown (not described in the current literature). 9 previously reported cases since 1937 |
| Gender Ratio | 62% female, 38% male in previously reported cases |
| Age Predilection | 25–83 years, mean 50 years in previously reported cases |
| Risk Factors | Prior surgery, congenital defect of posterior rectus sheath |
| Treatment | Surgical: primary closure |
| Prognosis | Excellent after surgery. Without surgery prognosis varies but patients are at risk for small bowel obstruction and bowel ischemia |
| Findings on Imaging | X-ray-nonspecific findings; may be normal or may show dilated loops of bowel. CT shows a defect of the posterior rectus sheath and bowel protruding anteriorly through the defect. CT can also show dilated loops of bowel if there is an obstruction |
Table 2.
Differential diagnosis table for posterior rectus sheath hernia
| Diagnosis | X-Ray | CT |
|---|---|---|
| Posterior Rectus Sheath Hernia | Nonspecific; can be normal or show dilated loops of bowel | Defect of the posterior rectus sheath with bowel protruding anteriorly through the defect. Dilated loops of bowel can be seen if there is an obstruction |
| Small Bowel Obstruction Due to Adhesion | Dilated loops of bowel | Dilated loops of bowel and a hypodense band across the bowel at a transition point |
| Small Bowel Obstruction Due to Mass | Dilated loops of small bowel | Dilated loops of small bowel. A soft tissue mass or focal bowel wall thickening may be seen with heterogeneous enhancement |
| Small Bowel Obstruction Due to Another Type of Abdominal Hernia | Dilated loops of bowel; can be nonspecific | Dilated loops of bowel. Abdominal contents (typically fat and bowel) protruding into a defect in the abdominal wall. |
| Ileus | Dilated loops of small and/or large bowel | Dilated loops of small and/or large bowel without a visualized transition point, mass, or adhesion. |
ABBREVIATIONS
- CT
Computed Tomography
REFERENCES
- 1.Losanoff JE, Basson MD, Gruber SA. Spontaneous hernia through the posterior rectus abdominis sheath: case report and review of the published literature 1937–2008. Hernia. 2009;13:555–558. doi: 10.1007/s10029-009-0481-6. [DOI] [PubMed] [Google Scholar]
- 2.Yang JD, Hwang HP, Kim JH, et al. Development of the rectus abdominis and its sheath in the human fetus. Yonsei Med J. 2012;53:1028–1035. doi: 10.3349/ymj.2012.53.5.1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Felfel M, El Khoury M, Marboeuf Y, Strohl D, Menu Y. Incarcerated hernia through the posterior rectus sheath. AJR Am J Roentgenol. 2005;185:1185–1186. doi: 10.2214/AJR.04.0637. [DOI] [PubMed] [Google Scholar]
- 4.Whitson BA, Ose KJ. Spontaneous posterior rectus sheath hernia: a new clinical entity? Hernia. 2007;11:445–447. doi: 10.1007/s10029-007-0204-9. [DOI] [PubMed] [Google Scholar]
- 5.Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003;83:1045–1051. v–vi. doi: 10.1016/S0039-6109(03)00132-4. [DOI] [PubMed] [Google Scholar]
- 6.Rutkow IM, Robbins AW. Demographic, classificatory, and socioeconomic aspects of hernia repair in the United States. Surg Clin North Am. 1993;73:413–426. doi: 10.1016/s0039-6109(16)46027-5. [DOI] [PubMed] [Google Scholar]
- 7.Miller PA, Mezwa DG, Feczko PJ, Jafri ZH, Madrazo BL. Imaging of abdominal hernias. Radiographics. 1995;15:333–347. doi: 10.1148/radiographics.15.2.7761639. [DOI] [PubMed] [Google Scholar]